Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Understanding Comorbidity Between Non-Suicidal Self-Injury and Depressive Symptoms in a Clinical Sample of Adolescents: A Network Analysis
Authors Niu S , Yin X, Pan B, Chen H, Dai C, Tong C, Chen F, Feng X
Received 6 October 2023
Accepted for publication 25 December 2023
Published 4 January 2024 Volume 2024:20 Pages 1—17
DOI https://doi.org/10.2147/NDT.S443454
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Shan Niu,1,* Xiaoxiao Yin,1,* Bing Pan,2 Haotian Chen,1 Chunxiao Dai,3 Chunnan Tong,4 Fang Chen,2 Xiuqin Feng1
1Nursing Department, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, Zhejiang, People’s Republic of China; 2Department of Psychiatry, Second Affiliated Hospital, Zhejiang University School of Medicine, Zhejiang University, Hangzhou, Zhejiang, People’s Republic of China; 3Department of Clinical Psychology, Affiliated Hangzhou First People’s Hospital Zhejiang University School of Medicine, Hangzhou, Zhejiang, People’s Republic of China; 4Department of Psychiatry, The Second Hospital of Jinhua, Jinhua, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiuqin Feng
Nursing Department, The Second Affiliated Hospital of Zhejiang University School of Medicine, No. 88 Jiefang Road, Hangzhou, Zhejiang, People’s Republic of China
, Email [email protected]
Background: Non-suicidal self-injury (NSSI) and depression often co-occur among adolescents with more severe clinical symptoms. This study examined the network structures of NSSI and depressive symptoms in adolescents.
Methods: Participants were recruited in the psychiatric outpatient clinics of three tertiary hospitals between April 10 and July 10, 2023. All participants been already found with self-injury behaviors in outpatient when enrolled. NSSI diagnostic criteria and Patient Health Questionnaire-9 (PHQ-9) were utilized to collect NSSI and depressive symptoms separately. We performed a network analysis to visualize the correlation between each symptom and to identify core and bridging symptoms in comorbidities.
Results: A total of 248 patients were enrolled in the study, with a mean age of 15.48 (SD = 1.62). Based on the PHQ-9 scores and grades, our results showed that the incidence of depression in adolescents with non-suicidal self-injury behavior was relatively high (N=235, 94.76%), with the majority having severe depression. The network analysis revealed that nodes D-6 “feeling bad, failing or letting yourself or your family down”, D-1 “little interest or pleasure” and D-4 “feeling tired” were the most vital and most central symptoms. The most crucial bridging symptom is the node NSSI-8 “frequent thinking about self-injury”, which connects the NSSI to the depression comorbid network.
Conclusion: This study offers a significant symptom-level conceptualization of the association between NSSI and depressive symptoms in a clinical sample of adolescents, which not only enhances our understanding of the comorbid but also identifies potential treatment targets to prevent and treat comorbidity between adolescent NSSI and depression.
Keywords: non-suicidal self-injury, depression, comorbidity network, bridge symptoms, network analysis
Introduction
Non-suicidal self-injury (NSSI) is the deliberate and socially unacceptable destruction of one’s body tissue without suicidal intent, including cutting, scratching, burning, scalding, banging limbs/head, and hair pulling.1 It has been reported that NSSI typically occurs during adolescence.2 The prevalence of NSSI is over 17.2% in adolescents and 5.5% in adults.3 Adolescence is a significant period for brain development, in which neuroplasticity may be a risk and vulnerability to mental health attacks.4 Previous research has shown that self-injury not only repeatedly inflicts painful physical injuries on adolescents, but also affects their cognitive and affective neurodevelopmental trajectories and maladaptive coping loops later in life.5–8
According to research, multiple factors are associated with an increased risk of NSSI in adolescents, including psychosocial, biological, and family environmental factors. Among these risk factors, depressive symptoms typically play a mediating role in this process. For example, Adolescent depressive symptoms mediate the correlation between parental rejection and NSSI,9 nightmares and NSSI,10 deviant peer affiliation and NSSI,11 neuroticism and NSSI,12 cyber victimization and NSSI,13 and so on. A longitudinal study suggests that depression and NSSI may be intertwined in a cycle of reciprocal associations over time.14 Depression was a predictor of risk for NSSI, and NSSI also predicted more depression in the future.15,16 Therefore, understanding the relationship between adolescent NSSI and depression can provide a clearer understanding of the occurrence and development process of NSSI.
Depression and non-suicidal self-injury often co-occur, coincide with more severe clinical symptoms. Zhang et al17 found in a nationwide multi-center combined cohort study of adolescent depression that the detection rate of NSSI in adolescents with depression was as high as 76.06%. The detection rate of depression among NSSI patients was as high as 81.3%.18 It has been reported that compared to simple depression, comorbidity will characterize more severe clinical phenotypes in adolescents, aggravate the psychological and disease burden of patients, and increase the risk of suicide.19 Previous research on comorbidity of NSSI and depression in adolescents had focused on correlates, such as introversion, intermediate defenses,20 youthfulness, and impulsivity,21 but the specific symptoms underlying this correlation are still unclear.
The correlation between levels of disease symptoms can provide substantial insights into the potential coexistence structure between NSSI and depression. In the previous literature, studies had either focused on counting recognized symptoms to determine diagnosis and comorbidity prevalence, or had viewed symptoms as indicators of underlying dimensions, with correlations between symptoms viewed as by-products of dimensional commonality, thereby ignored the role of symptom-level correlations in comorbidities.22 Network theory of psychopathology is an alternative approach to conceptualizing comorbidity, which posits that mental disorders are dynamic networks formed through the interaction between symptoms, where specific symptoms may be more central and interrelated than others, thereby maintaining symptom clusters and maintaining the onset of the disease,23 which are referred to as core symptoms. In network theory, symptoms constitute mental disorders rather than reaction mental disorders.24 Cramer et al25 discussed the methodological problems in current research on comorbidity and conceptualize comorbidity between psychiatric disorders as a direct relationship between the various symptoms of a psychiatric disorder, arguing that a network approach may help to answer the key question of accurately describing comorbidity. Thus, NSSI and depression can be conceptualized as two syndromes with multi-index notations. The coexisting patients have high disease severity, which may be the structural pattern of symptom coexistence and broader pain response.
A commonly used network model in estimating psychological network is the pairwise Markov random filed (PMRF).26 A PMRA is a network in which nodes represent variables (symptoms), connected by undirected edges between two variables (relationships between these symptoms), which can encode the pattern of symptom-symptom interaction and provide a new understanding of mental health and comorbidities.24 In this model, statistical methods such as node centrality can be used to reflect the importance of nodes in the network. A node with high centrality can be considered as a central symptom in the network, and changing it will affect more other nodes in the model. For example, many studies have explored the symptom network of depression and stated that the core symptoms of depression are low mood, loss of pleasure, pessimism.27,28 In a comorbidity network, symptoms that connect two mental disorders are called “bridge symptoms” (ie, one disorder activates the other), and can also be calculated using the statistical indicator ‘bridge strength’. That is, the symptoms of mental disorders can spread. They will not stop at the border of a DSM diagnosis.22 The specific symptoms of one disorder also put one at risk factor for other disorders, thereby producing diagnostic comorbidity.29 For example, negative emotions, frequent thinking, separation anxiety, loneliness, and impulsivity may be bridge symptoms between NSSI and borderline personality disorder transmission;30 guilt, irritability, and sadness as Bridges Connecting Depression and Anxiety to Suicide.31 According to research,29 removing nodes (symptoms) based on bridge statistics was more effective than eliminating nodes with high traditional centrality statistics in preventing comorbidity. By deactivating bridge nodes, the spread of comorbidity can be prevented.
In summary, our study hypothesized that the structure and core symptoms of the comorbid symptom network between NSSI and depression are different from those of NSSI alone or depression alone and that there are bridge symptoms connecting the two. Based on this, the primary purpose of this study is to explore the comorbidity structure between NSSI and depressive symptoms in adolescents and to investigate specific symptoms (bridge symptoms) that connect the two diseases. Additionally, we explored the prevalence of depressive symptoms in adolescents’ non-suicidal self-injurious behaviors to examine the extent to which these two disorders are comorbid in adolescents.
Method
Participants and Procedure
This study adopted a multi-center cross-sectional study design and utilized the convenient sampling method in psychiatric outpatient clinics of three tertiary hospitals in Zhejiang Province between April 10 and July 10, 2023. Two of the hospitals are comprehensive hospitals and one is a psychiatric hospital. To prevent inconsistencies in the criteria used by physicians to judge patients with self-injury, uniform training was provided to participating staff before the start of the study.
For our study, the inclusion criteria were: (1) age between 12 and 18 years; (2) NSSI status as diagnosed by specialized psychiatrists according to the diagnostic criteria recommended by the DSM-5. When patients were asked “Have you ever, intentionally or deliberately injured yourself without suicidal intent?” They answered positively in outpatient clinics; (3) Relatively stable emotions and normal reading, comprehension and expression skills. The study exclusion criteria were (1) patients with cognitive disorders, schizophrenia, substance use disorder, and developmental delay; (2) any history of significant head trauma or neurological deficit.
Prior to implementation, trained researchers explained in detail the purpose, content and methodology of the study to the study participants in a face-to-face manner, as well as informing them of the matters requiring their attention and cooperation. After obtaining written informed consent from both adolescents and their guardians, they answered an online anonymous self-report questionnaire as part of a study investigating self-injury and suicide among adolescents.
Measures
Demographics Questionnaire
Participants were asked to complete the demographics questionnaire, including age, gender, and education level. They also answered questions about their family structure and the marital status of their biological parents.
Non-Suicidal Self-Injury Symptoms
Non-suicidal self-injury symptoms were gathered using a scale adapted from DSM-5 diagnostic criteria. Buelens et al32 provided a precise overview of the issues based on five NSSI criteria (A, B, C, D, E, F), where criterion C1 was split into negative feelings or thoughts and conflicts with others, and affirmed its value as a symptom of the NSSI.30 The scores for criteria A, B, C, and E were all on a 5-point Likert scale ranging from 1 to 5 (Table S1). In this study, the Non-Suicidal Self-Injury Symptoms Scale had a Cronbach’s alpha of 0.80, a KMO value of 0.80, passed the Bartlett test of homogeneity of variances, and had a cumulative variance explained of 60%, which gave it good reliability and validity.
Depressive Symptoms
The Chinese version of the Patient Health Questionnaire-9 (PHQ-9)33 was used to assess depressive symptoms and severity. The previous study34 have shown that the Chinese version of PHQ-9 has sufficient internal consistency and expected strong correlations with anxiety, self-esteem, and perceived control in a group of Chinese adolescents, making it a reliable and valid scale for assessing and comparing the severity of depression in adolescence. The questionnaire consists of 9 items scored on a 4-point Likert scale ranging from 0 to 3 and results in a summed score ranging from 0 to 27 or a mean score ranging from 0 to 3. Higher mean scores indicate more depressive symptoms.35 The severity of a depressive episode can be assessed by the summary score. Scores of 5–9 indicate mild depression, 10–14 indicate moderate depression, 15–19 indicate moderately severe depression, and ≥ 20 indicate severe depression. The Cronbach’s alpha of the PHQ-9 was 0.90 in the current study.
All data were collected by the Questionnaire Star platform36 and kept in the hospital as required. Only research personnel had access to the questionnaires, and they all pledged to keep the data collected strictly confidential. See Figure 1 for the statistical analysis flow chart.
 |
Figure 1 The network statistical analysis flow chart. |
Statistic Analysis
Descriptive Statistics
A descriptive analysis was conducted on demographic data, depression severity, and symptoms of adolescents with NSSI behaviors. Continuous variables are reported as the mean and standard deviation, while categorical variables are presented as frequencies and percentages.
Network Statistical Analysis
We first analyzed the sample size to ensure that the sample size was sufficient. We then mapped the structure of the co-morbidity network and performed a stability analysis on this structure map to ensure that the structure was stable and met the criteria. Finally, we performed the required indicators such as centrality analysis to get the core symptoms, bootstrap difference test to get the difference map of edges and nodes, and bridging analysis to get the bridging symptoms of the co-morbidity network. See Figure 1 for the network statistical analysis flow chart.
Sample Size Analysis
The sample size is an essential consideration in any statistical analysis. In our study, we used two methods to determine the sample size. First, we have an a priori expectation of the sample size. According to research,37 for a network with P nodes, P(P-1)/2 parameters must be estimated. Since the expected number of nodes in this study is 21 (the sum of the number of NSSI quantitative entries and the number of PHQ-9 entries), 210 parameters were required. Then, we used the “NetSimulator” function to simulate the data under a given network model and expected network structure to check whether the sample size is sufficient.37 Sensitivity, specificity, and correlation between the edge weights or centrality estimates of the real network and the estimated network are the most important attributes when estimating the sample size.38
Network Estimation
In PMAF, the number of parameters to estimate grows rapidly with the size of the network, which typically requires far more observations than the characterized psychological data. Therefore, “least absolute shrinkage and selection operator” (LASSO)39 was used to deal with this problem by limiting the total sum of absolute parameter values, leading many edge estimates to shrink to precisely zero and dropping out of the model, ultimately yielding a sparse and easy-to-interpret network model. This technique is a form of regularization. However, LASSO needs to control the extent to which regularization is applied using a tuning parameter that can be chosen by minimizing the extended Bayesian information criterion (EBIC).40 When the data are quantitative, the appropriate PAMF model is the Gaussian graphical model. Thus, Gaussian Markov random field estimation using graphical LASSO (glasso) and extended Bayesian information criteria (EBIC) was used in the network.37
R packages “bootnet”41 and “qgraph”42 were used for analysis.
Network Stability
Nonparametric bootstrapping for edge-weight accuracy and case-dropping subset bootstrapping for centrality stability were assessed in the robustness of network estimated parameters. Case-dropping subset bootstrapping yields correlation stability coefficients (CS-coefficient) should not be lower than 0.25 and preferably higher than 0.5 when the maximum drop proportions to retain a correlation of 0.7 in at least 95% of the samples.37
Network Centrality
Strength, betweenness, closeness and expected influence (EI) were used to assess centrality. Node strength quantifies the absolute sum of all the connections of a node, reflecting the degree to which the node is directly connected to other nodes. Betweenness quantifies how often a node is on the shortest path of any two other nodes, reflecting the importance of that node on the average path between the other two nodes. Closeness quantifies the inverse of the sum of the shortest path distances from all other nodes in the network to that node, reflecting the degree to which a node is indirectly connected to other nodes.41 EI quantifies the total weight of all edges extending from a given node and is considered an accurate measure of centrality since it considers both positive and negative edges.43 We also performed the bootstrapped difference test to determine if the edge weights or centralities differed from one another by checking if zero was in the bootstrapped CI.41
Network Bridges
Using the “networktools” package, we estimated bridge strength, which is calculated as the sum of absolute edge weights from one node to all nodes not in the same community. It is recommended to retain only the top 20% of bridges with the strongest centrality.29
P-values < 0.05 were considered statistically significant. Statistical analysis was performed with R software version 4.3.0.
Result
Sample Characteristics
A total of 248 people were recruited and 248 questionnaires were completed with a validity rate of 100%. We performed the test and found that the observations did not have duplicates and missing values. Subsequently, outlier detection was carried out using the Z-score method and interpolated using the mean. The characteristics of the participants are shown in Table 1, and the scores of NSSI and depressive symptoms are shown in Table 2.
 |
Table 1 Characteristics and Depressive Severity of Participants (N=248) |
 |
Table 2 Descriptive Statistics of the NSSI Symptoms and Depressive Symptoms (N = 248) |
Sample Size Selection and Stability
Figure 2 shows the corresponding plots, which may be used to gain rough insight into the required sample size. Approximately 250 samples can achieve a correlation between the true and estimated networks above 0.9 for edge weights, and above 0.7 for strength and specificity. Therefore, a sample size of 248 participants meets both the calculation and examination criteria, and the finalized sample size for this study is 248. Centrality stability was perfect for expected influence (EI CS-coefficient = 0.673) and acceptable for strength and closeness (strength CS-coefficient = 0.44, closeness CS-coefficient = 0.363). See Figure S1 for the centrality stability plot. The edge-weight stability of the network was acceptable with moderate bootstrapped 95% confidence intervals (see Figure S2).
Estimated Network
The comorbid network structure of NSSI and depressive symptoms among adolescents is displayed in Figure 3. A description of the node labels can be seen in Table 2. The estimated network has 21 nodes and 88 non-zero edges out of 210 possible edges. From the strength of the edge connection between each symptom (Table S2), the most significant edge weights of NSSI symptoms were observed between nodes NSSI-11 “influences my performance (school/work/…) negatively” and NSSI-12 “influences other important areas negatively” (part r = 0.4671) and nodes NSSI-3 “to resolve interpersonal difficulty” and NSSI-6 “interpersonal conflicts prior to self-injury” (part r = 0.3922). The most significant edge weights of depressive symptoms were between nodes D-1 “little interest or pleasure in doing things” and D-6 “feeling down, depressed or hopeless” (part r = 0.4647), and between D-1 “little interest or pleasure in doing things” and D-4 “feeling tired or lacking in energy” (part r = 0.4012). The bootstrap difference test for edge weights found that these edges were significantly different from most edges in the network (Figure S3). The strongest edge between NSSI and depression nodes can better understand the relationship between these two symptoms. The correlation between nodes NSSI-8 “frequent thinking about self-injury” and D-9 “the thought of dying or harming oneself” (part r =0.215) was the strongest edges. This is consistent with the empirical results, because the intrusive thought or repeated thinking of self-harm or risky situation of suicide are always concerned by the clinician. In addition to this, strong correlations were similarly found for the NSSI-8“frequent thinking about self-injury” and D-6 “feeling bad, failing or letting yourself or your family down” (part r = 0.133), and NSSI-1 “frequency of NSSI within one year” and D-7 “trouble concentrating” (part r = 0.0929).
Network Centrality
Figure 4 shows the corresponding centrality indices for the comorbidity network, Figure 5 shows the centrality indices for the depressive symptom network alone, and Figure 6 shows the centrality indices for the NSSI symptoms alone, where the node labels are described in Table 2. Given that the expected influence had the highest stability, we focused on the centrality index for interpretation. Node D-6 “feeling bad, failing or letting yourself or your family down” (EI = 1.09), D-1 “little interest or pleasure” (EI = 1.08) and D-4 “feeling tired” (EI = 1.07) were the strongest and most central symptoms in the comorbid network. D-1 (EI = 1.12), D-4 (EI = 1.05), D-2 “Feeling down, depressed or hopeless” (EI = 1.03) were the core symptoms of depression alone, while NSSI-12 (EI = 1.04), NSSI-11 (EI = 1.01), NSSI-7 “Preoccupation with the act that I can’t control prior to self-injury” (EI = 1.00) were the core symptoms of NSSI alone. See Figure S4 for the results of the node EI difference test in comorbidity network.
 |
Figure 4 Corresponding centrality indices of the comorbidity network. Centrality indices are shown as standardized z-scores. |
 |
Figure 5 Corresponding centrality indices of the depression network. Centrality indices are shown as standardized z-scores. |
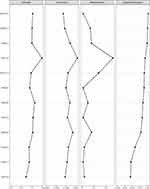 |
Figure 6 Corresponding centrality indices of the NSSI network. Centrality indices are shown as standardized z-scores. |
Bridge Symptoms
The bridge centrality plot of the comorbid network is presented in Figure 7. The strongest bridge nodes in the network were node NSSI-8 “frequent thinking about self-injury” (bridge strength = 0.33), D-9 “the thought of dying or harming oneself” (bridge strength = 0.28), D-6 “feeling bad, failing or letting yourself or your family down” (bridge strength = 0.16) and NSSI-1 “frequency of non-suicidal self-injury within one year” (bridge strength = 0.14). The strongest bridges are colored and presented in Figure 8. A description of the node labels can be seen in Table 2.
 |
Figure 7 Bridge centrality for the comorbidity estimated network shown as standardized z-scores. |
 |
Figure 8 The network graph with colored bridges. |
Discussion
In our study, we evaluated the comorbid network structure of NSSI and depression in a clinical sample of adolescents and identified bridge symptoms between this comorbid network through network analysis. Additionally, the severity of depression in non-suicidal self-injured adolescents was investigated. To our knowledge, this study is the first to evaluate the comorbidity network structure of adolescent NSSI and depression, which not only improves our understanding of the comorbid but also identifies potential effective treatment targets to prevent and treat the comorbidity between adolescent NSSI and depression.44
On the whole, based on the PHQ-9 scores and grades, the incidence of depression in adolescents with non-suicidal self-injury behavior was relatively high (N=235, 94.76%), with the majority having severe depression (N=112, 45.16%) and moderately severe depression (N=54, 21.77%). In our study, the prevalence of depression (N=235, 94.76%) was slightly higher than in previous studies (MDD = 81.3%), and the prevalence of severe and higher depression (N = 66.94%) was slightly lower than in previous studies, which may be related to the different research tools and scoring criteria used. However, both the present and previous studies have highlighted the prevalence of NSSI and depression comorbidity.
Analyzed from the perspective of the structure of the comorbid symptom network, the NSSI symptom of NSSI-8 “frequent thinking about self-injury” was strongly and positively correlated with the depressive symptom of D-9 “thoughts of dying or harming oneself”, and D-6 “feeling bad, failing or letting yourself or your family down”. On the one hand, consistent with reality, the present study similarly emphasized the importance of thinking repeatedly about self-injury and the correlation between D-9 and NSSI-8. On the other hand, we stressed the relevance of self-blame in comorbidity networks. Previous studies36 have shown that, the aim of reproach is punishment with an aggressive tone, often accompanied by explicit denunciation (I should not disappoint my family). This is not a simple statement, but an acceptance of moral responsibility and spiritual struggle in self–reproach.36 Adolescents are in a sensitive and fragile period of personality pathology development, and they usually cannot control this complex emotion and adopt a stress response such as frequent thinking about self-injury.6,45–47 Overall, those three items are the only ones describing cognitions (even if D-6 includes the word “feel”), exposing the thinking patterns of comorbid adolescents. For the same event, people with comorbidity will think about it from a negative perspective, repeatedly, and produce negative cognitive outcomes. That explanation would also lead directly to treatment recommendation that are consistent with empirical data, to focus on the cognitions. The relevant personnel, parents and schools can organize activities to analysis and review the stressful life events of young people on a regular basis, so as to guide young people to look at and solve their problems from a positive perspective. Although a person’s personality cannot be changed easily, adolescents can change their cognitive thinking when facing similar life events, thereby reducing the occurrence of NSSI and depression.
This study also proposed the role of poor concentration in comorbidity between NSSI and depression. According to the comorbidity network, the NSSI-1 “frequency within one year” was related to the D-7 “trouble concentrating”. This is consistent with the discovery that inattention was associated with NSSI in childhood and adolescence.48 Concentration difficulties are present in many mental disorders, such as anxiety disorder49 and eating disorder,50 which are commonly comorbid with NSSI.51,52 In our study, concentration was assessed by one of the items on the PHQ-9 (Trouble concentrating on things, such as reading the newspaper or watching television), which was more subjective. More objective methods could be used in the future. This finding suggests that the relationship between inattention and NSSI may play a role in maintaining NSSI-depression comorbidity and should be studied further. At the same time, it is reminded that medical staff should also pay attention to the possibility of NSSI and depression in the treatment of patients with inattention.
In terms of core symptoms, the core symptoms of the comorbidity network differed from those of depression alone or NSSI alone, which is consistent with our previous hypothesis. In our study, the core symptoms of the comorbidity were depressive symptoms of D-6 “feeling bad, failing, letting yourself or your family down”, D-1 “little interest or pleasure” and D-4 “feeling tired or lacking in energy”, which were determined by node expected influence. The pleasure response and associated neurotransmitters and brain circuits play a significant role in non-suicidal self-injury, which is consistent with the common non-suicidal self-injury purpose of ending a negative emotional state or numb feeling and regulating high-energy states.53–55 Significantly, these symptoms were related to other symptoms and had the most significant impact on the structure of the NSSI-depression network,56 but not on NSSI or depression separately. Therefore, we speculate that comorbidity has its specificity, and depressive symptoms are more severe in the comorbidity of NSSI and depression. It is recommended that healthcare professionals, when treating and caring for adolescents with NSSI and comorbidities of depression, provide timely guidance to adolescents with self-blame tendencies and self-guilt to prevent their condition from worsening.
Consistent with the study hypothesis, there are bridge symptoms connecting NSSI and the depression symptoms network. NSSI-8 “frequent thinking about self-injury”, D-9 “the thought of dying or harming oneself”, D-6 “feeling bad, failing or letting yourself or your family down” and NSSI-1 “frequency of non-suicidal self-injury within one year” were key bridge nodes. That is, if an adolescent with NSSI develops these symptoms - bridge symptoms that also belong to network associates with depressive disorder - and as a result comorbid patterns of symptom interaction will arise in depression network. It’s partly confirmed previous findings. Previous research has found that rumination has a deleterious impact on the course of depressive symptoms.57 Frequent thinking about NSSI may aggravate the condition of adolescents. Additionally, the self-punishment function is a significant risk factor for non-suicidal self-injury in adolescents, which is positively correlated with the frequency of self-injury and negative thoughts.47 Bridge symptoms could be considered as treatment targets for adolescents with NSSI and depression.
There are also limitations in our study. First, cross-sectional data were examined in this study, which does not allow directional conclusions to be drawn on symptom relationships. However, according to the analysis of in our study, the structure and core symptoms of the comorbid symptom network between NSSI and depression are different from those of NSSI alone or depression alone, and the core symptoms in the co-morbidity network were all depressive symptoms, which may provide some reference to the propensity for comorbid causation. In the future, longitudinal studies could be conducted to obtain time series data to draw conclusions about time directionality between adolescent NSSI and depressive symptoms (ie, what’s first, depression or NSSI). In addition, the study focused on clinical samples, which hinders the generalization of the research results to non-clinical samples. Future research can expand the sampling range to improve the generalizability of the results.
Conclusion
This study used network analysis to explore the comorbidity network structure of NSSI and depression in a clinical sample of adolescents. According to core symptoms, the network core symptoms of comorbidity are different from depression alone or NSSI alone, and have their own specificity with depressive emotions being more pronounced. The identification of NSSI-8 “frequent thinking” (bridge symptom), D-9“the thought of dying or harming oneself” (bridge symptom), D-6“self-blame” (both bridge symptom and core symptom), NSSI-1“frequency of non-suicidal self-injury within one year” (bridge symptom) and D-7 “trouble concentrating” (symptoms with high correlation) can provide potential targets for the treatment and screening of adolescents with NSSI and depression in outpatient clinical setting.
Ethics Approval
This study was approved by the Ethics Committee of Second Affiliated Hospital of Zhejiang University School of Medicine [Grant No. (2023-0822)] and other participating hospitals. This study was conducted in accordance with the ethical standards of the Helsinki declaration.
Acknowledgments
The authors are grateful to the adolescents who participated in this research and to the hospitals and research assistants who facilitated data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Nock MK. Self-Injury. In: NolenHoeksema S, Cannon TD, Widiger T, editors. Annual Review of Clinical Psychology. Vol. 6. Annual Review; 2010:339–363.
2. Li M, Wang H, Li J, Deng Y, Yu C. Peer victimization, depression, and non-suicidal self-injury among Chinese adolescents: the moderating role of the 5-HTR2A gene rs6313 polymorphism. Child Adolesc Psychiatr Ment Health. 2022;16(1):108. doi:10.1186/s13034-022-00532-4
3. Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threaten Behav. 2014;44(3):273–303. doi:10.1111/sltb.12070
4. De Luca L, Pastore M, Palladino BE, Reime B, Warth P, Menesini E. The development of Non-Suicidal Self-Injury (NSSI) during adolescence: a systematic review and Bayesian meta-analysis. J Affective Disorders. 2023;339:648–659. doi:10.1016/j.jad.2023.07.091
5. Blasco-Fontecilla H, Fernandez-Fernandez R, Colino L, Fajardo L, Perteguer-Barrio R, de Leon J. The addictive model of self-harming (non-suicidal and suicidal) behavior. Front Psychiatry. 2016;7:78. doi:10.3389/fpsyt.2016.00008
6. Sharp C, Wall K. Personality pathology grows up: adolescence as a sensitive period. Curr Opinion Psychol. 2018;21:111–116. doi:10.1016/j.copsyc.2017.11.010
7. Bjureberg J, Kuja-Halkola R, Ohlis A, et al. Adverse clinical outcomes among youths with nonsuicidal self-injury and suicide attempts: a longitudinal cohort study. J Child Psychol Psychiatry. 2022;63(8):921–928. doi:10.1111/jcpp.13544
8. Buelens T, Luyckx K, Gandhi A, Kiekens G, Claes L. Non-suicidal self-injury in adolescence: longitudinal associations with psychological distress and rumination. J Abnormal Child Psychol. 2019;47(9):1569–1581. doi:10.1007/s10802-019-00531-8
9. Zhu J, Chen Y, Su B. Non-suicidal self-injury in adolescence: longitudinal evidence of recursive associations with adolescent depression and parental rejection. J Adolesc. 2020;84(1):36–44. doi:10.1016/j.adolescence.2020.08.002
10. Liu ZZ, Tein JY, Jia CX, Liu X. Depression as a mediator between frequent nightmares and non-suicidal self-injury among adolescents: a 3-wave longitudinal model. Sleep Med. 2021;77:29–34. doi:10.1016/j.sleep.2020.11.015
11. Wei C, Li J, Yu C, Chen Y, Zhen S, Zhang W. Deviant peer affiliation and non-suicidal self-injury among Chinese adolescents: depression as a mediator and sensation seeking as a moderator. Int J Environ Res Public Health. 2021;18(16):8355. doi:10.3390/ijerph18168355
12. Liao C, Gu X, Wang J, et al. The relation between neuroticism and non-suicidal self-injury behavior among college students: multiple mediating effects of emotion regulation and depression. Int J Environ Res Public Health. 2022;19(5). doi:10.3390/ijerph19052885
13. Liu S, Wu W, Zou H, et al. Cybervictimization and non-suicidal self-injury among Chinese adolescents: the effect of depression and school connectedness. Front Public Health. 2023;11:1091959. doi:10.3389/fpubh.2023.1091959
14. Faura-Garcia J, Calvete E, Orue I. Longitudinal associations between nonsuicidal self-injury, depressive symptoms, hopelessness, and emotional dysregulation in adolescents. Arch Suicide Res. 2023;1–15. doi:10.1080/13811118.2023.2237075
15. Poudel A, Lamichhane A, Magar KR, Khanal GP. Non suicidal self injury and suicidal behavior among adolescents: co-occurrence and associated risk factors. BMC Psychiatry. 2022;22(1):96. doi:10.1186/s12888-022-03763-z
16. Daukantaite D, Lundh LG, Wångby-Lundh M, et al. What happens to young adults who have engaged in self-injurious behavior as adolescents? A 10-year follow-up. Eur Child Adolesc Psychiatry. 2021;30(3):475–492. doi:10.1007/s00787-020-01533-4
17. Zhang B, Zhang W, Sun L, Jiang C, Zhou Y, He K. Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatry. 2023;23(1):445. doi:10.1186/s12888-023-04938-y
18. Xiao Q, Song X, Huang L, Hou D, Huang X. Association between life events, anxiety, depression and non-suicidal self-injury behavior in Chinese psychiatric adolescent inpatients: a cross-sectional study. Article. Frontiers in Psychiatry. 2023;141140597. doi:10.3389/fpsyt.2023.1140597
19. Serra M, Presicci A, Quaranta L, et al. Assessing clinical features of adolescents suffering from depression who engage in non-suicidal self-injury. Children. 2022;9(2):201. doi:10.3390/children9020201
20. Peng B, Liao JW, Li Y, et al. Personality characteristics, defense styles, borderline symptoms, and non-suicidal self-injury in first-episode major depressive disorder. Front Psychol. 2023:14989711. doi:10.3389/fpsyg.2023.989711
21. Wang L, Liu J, Yang Y, Zou HO. Prevalence and risk factors for non-suicidal self-injury among patients with depression or bipolar disorder in China. BMC Psychiatry. 2021;21(1):389. doi:10.1186/s12888-021-03392-y
22. Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol. 2008;64(9):1089–1108. doi:10.1002/jclp.20503
23. Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi:10.1002/wps.20375
24. Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. In: NolenHoeksema S, editor. Annual Review of Clinical Psychology. Vol. 9. Annual Review; 2013:91–121.
25. Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33(2–3):137–+. doi:10.1017/s0140525x09991567
26. Costantini G, Epskamp S, Borsboom D, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Personality. 2015;54:13–29. doi:10.1016/j.jrp.2014.07.003
27. Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. 2019;48(4):656–668. doi:10.1080/15374416.2018.1437735
28. Manfro PH, Pereira RB, Rosa M, et al. Adolescent depression beyond DSM definition: a network analysis. Eur Child Adolesc Psychiatry. 2023;32(5):881–892. doi:10.1007/s00787-021-01908-1
29. Jones PJ, Ma RF, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivar Behav Res. 2021;56(2):353–367. doi:10.1080/00273171.2019.1614898
30. Buelens T, Costantini G, Luyckx K, Claes L. Comorbidity between non-suicidal self-injury disorder and borderline personality disorder in adolescents: a graphical network approach. Article. Front Psychiatry. 2020;11580922. doi:10.3389/fpsyt.2020.580922
31. Cai H, Chow IHI, Lei SM, et al. Inter-relationships of depressive and anxiety symptoms with suicidality among adolescents: a network perspective. J Affective Disord. 2023;324:480–488. doi:10.1016/j.jad.2022.12.093
32. Buelens T, Luyckx K, Kiekens G, Gandhi A, Muehlenkamp JJ, Claes L. Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affective Disord. 2020;260:314–322. doi:10.1016/j.jad.2019.09.009
33. Wang WZ, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. General Hospital Psychiatry. 2014;36(5):539–544. doi:10.1016/j.genhosppsych.2014.05.021
34. Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Article. Asia Pac Psychiatry. 2020;12(3):e12381. doi:10.1111/appy.12381
35. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
36. Shapiro D. Self-reproach and personal responsibility. Psychiatry Interpersonal Biol Proces. 2006;69(1):21–25. doi:10.1521/psyc.2006.69.1.21
37. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. 2018;23(4):617–634. doi:10.1037/met0000167
38. van Borkulo CD, Borsboom D, Epskamp S, et al. A new method for constructing networks from binary data. Sci Rep. 2014:45918. doi:10.1038/srep05918
39. Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc Ser B Stat Methodol. 1996;58(1):267–288. doi:10.1111/j.2517-6161.1996.tb02080.x
40. Chen JH, Chen ZH. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi:10.1093/biomet/asn034
41. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50(1):195–212. doi:10.3758/s13428-017-0862-1
42. Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Statist Software. 2012;48(4):1–18. doi:10.18637/jss.v048.i04
43. Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnormal Psychol. 2016;125(6):747–757. doi:10.1037/abn0000181
44. Finch JE, Xu Z, Baker JH. Understanding comorbidity between eating disorder and premenstrual symptoms using a network analysis approach. Article. Appetite. 2023;181106410. doi:10.1016/j.appet.2022.106410
45. Yager J, Kay J. Autotraumatic stress disorders posttraumatic stress disorder variants when the victim bears responsibility for the trauma. J Nerv Ment Dis. 2020;208(12):947–952. doi:10.1097/nmd.0000000000001235
46. Mahtani S, Melvin GA, Hasking P. Shame proneness, shame coping, and functions of Nonsuicidal Self-Injury (NSSI) among emerging adults: a developmental analysis. Emerging Adulthood. 2018;6(3):159–171. doi:10.1177/2167696817711350
47. Sheehy K, Noureen A, Khaliq A, et al. An examination of the relationship between shame, guilt and self-harm: a systematic review and meta-analysis. Clinic Psychol Rev. 2019:73101779. doi:10.1016/j.cpr.2019.101779
48. Ojala O, Kuja-Halkola R, Bjureberg J, et al. Associations of impulsivity, hyperactivity, and inattention with nonsuicidal self-injury and suicidal behavior: longitudinal cohort study following children at risk for neurodevelopmental disorders into mid-adolescence. BMC Psychiatry. 2022;22(1):679. doi:10.1186/s12888-022-04311-5
49. Elkins RM, Carpenter AL, Pincus DB, Comer JS. Inattention symptoms and the diagnosis of comorbid attention-deficit/hyperactivity disorder among youth with generalized anxiety disorder. J Anxiety Disord. 2014;28(8):754–760. doi:10.1016/j.janxdis.2014.09.003
50. Yates WR, Lund BC, Johnson C, Mitchell J, McKee P. Attention-deficit hyperactivity symptoms and disorder in eating disorder inpatients. Int J Eating Disord. 2009;42(4):375–378. doi:10.1002/eat.20627
51. Claes L, Turner B, Dierckx E, Luyckx K, Verschueren M, Schoevaerts K. Different clinical presentations in eating disorder patients with non-suicidal self-injury based on the co-occurrence of borderline personality disorder. Psychologica Belgica. 2018;58(1):243–255. doi:10.5334/pb.420
52. Bushnell GA, Gaynes BN, Compton SN, Dusetzina SB, Brookhart MA, Sturmer T. Incidence of mental health hospitalizations, treated self-harm, and emergency room visits following new anxiety disorder diagnoses in privately insured US children. Depression Anxiety. 2019;36(2):179–189. doi:10.1002/da.22849
53. Worley J. The role of pleasure neurobiology and dopamine in mental health disorders. J Psychosocial Nurs Ment Health Serv. 2017;55(9):17–21. doi:10.3928/02793695-20170818-09
54. Bresin K, Gordon KH. Endogenous opioids and nonsuicidal self-injury: a mechanism of affect regulation. Review. Neurosci Biobehav Rev. 2013;37(3):374–383. doi:10.1016/j.neubiorev.2013.01.020
55. Moseley RL, Gregory NJ, Smith P, Allison C, Baron-Cohen S. A ‘choice’, an ‘addiction’, a way ‘out of the lost’: exploring self-injury in autistic people without intellectual disability. Article. Mol Autism. 2019;1018. doi:10.1186/s13229-019-0267-3
56. McNally RJ. Can network analysis transform psychopathology? Article. Behav Res Ther. 2016;86:95–104. doi:10.1016/j.brat.2016.06.006
57. Carter JD, Frampton CMA, Mulder RT, Luty SE, McKenzie JM, Joyce PR. Rumination: relationship to depression and personality in a clinical sample. Personal Ment Health. 2009;3(4):275–283. doi:10.1002/pmh.91
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


