Back to Journals » Journal of Pain Research » Volume 16
Ultrasound-Guided Quadratus Lumborum Block at the Lateral Supra-Arcuate Ligament versus Subcostal Transversus Abdominis Plane Block for Postoperative Analgesia Following Open Hepatectomy: A Randomized Controlled Trial
Authors Mao Y , Zhao W, Hao M , Xing R, Yan M
Received 14 January 2023
Accepted for publication 31 March 2023
Published 27 April 2023 Volume 2023:16 Pages 1429—1440
DOI https://doi.org/10.2147/JPR.S404810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ellen M Soffin
Ye Mao,* Wei Zhao,* Mengxiao Hao, Rui Xing, Ming Yan
Department of Anesthesiology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou City, Jiangsu Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ming Yan, Department of Anesthesiology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou City, Jiangsu Province, 221000, People’s Republic of China, Tel +86 18052268329, Email [email protected]
Purpose: Many studies confirmed that several approaches of quadratus lumborum block (QLB) were superior to transversus abdominis plane block (TAPB) in reducing opioid consumption during postoperative period. As a new QLB approach at the lateral supra-arcuate ligament (QLB-LSAL), the analgesic efficacy and safety in patients undergoing open hepatectomy are still unknown. This study aims to compare postoperative analgesia between the blocks in open hepatectomy.
Patients and Methods: Sixty-two patients undergoing open hepatectomy were enrolled and randomly allocated into the QLB-LSAL group (group Q) and the subcostal TAPB group (group T). Preoperatively, patients received ultrasound-guided bilateral QLB-LSAL or subcostal TAPB with injection of 0.5% ropivacaine (a total volume of 40 mL). The primary outcome was cumulative total morphine equivalent consumption in the first postoperative 24 h. Other outcomes included numerical rating scale (NRS) scores at rest and coughing, cumulative total morphine equivalent consumption at 2, 6, 12, 48 h, Quality of Recovery-15 (QoR-15) scores, time to first patient-controlled intravenous analgesia (PCIA) request, time to first ambulation and adverse effects.
Results: The cumulative total morphine equivalent consumption in group Q was decreased significantly at all postoperative time points (P < 0.01). The postoperative NRS scores at rest and coughing in group Q were lower than those in group T at all postoperative time points except 48 h (P < 0.05). A significant increase was also observed in the QoR-15 scores among patients in group Q. Time to first PCIA request was significantly prolonged in group Q than in group T, and time to first ambulation was shortened. Adverse effects showed no statistical significance between the two groups.
Conclusion: Compared with subcostal TAPB, preoperative bilateral QLB-LSAL provided superior analgesic properties and promoted early postoperative recovery quality in patients undergoing open hepatectomy.
Trial Registration: China Clinical Trials Registration Center (http://www.chictr.org.cn) ChiCTR2200063291, 3/9/2022.
Keywords: quadratus lumborum block, transversus abdominis plane block, open hepatectomy, analgesia
A Letter to the Editor has been published for this article.
Introduction
At present, open hepatectomy is still a common clinical procedure for hepatolithiasis, benign or malignant hepatic tumour due to the complex state of an illness. This procedure mostly adopts a right subcostal margin incision or an inverted L-shaped incision accompanied by severe postoperative somatic and visceral pain.1 Effective analgesic measures are contributed to reducing complications, promoting early mobilization, shortening the length of hospital stay and improving postoperative recovery quality.2 The use of opioid is still a universal choice for pain control. However, single application of intravenous opioid is prone to opioid-related side effects, such as excessive sedation, respiratory depression, pruritus, postoperative nausea and vomiting (PONV) and delayed intestinal function recovery. Besides, inappropriate opioid use is likely to increase the risk of opioid addiction or tolerance in patients.3
In order to minimize opioid usage and improve patient outcomes on the basis of sufficient perioperative analgesia, enhanced recovery after surgery (ERAS) recommended regional nerve blocks including subcostal transversus abdominis plane block (TAPB) or thoracic epidural analgesia (TEA), which are a key element of the multimodal analgesic strategy.1,4
As a common performed truncal block, TAPB improved analgesic effect with a wide usage in open and laparoscopic abdominal surgery.5 In previous studies, subcostal TAPB was proved to reduce the accumulated opioid consumption without obvious side effects in patients undergoing open hepatectomy.6–8 Moreover, quadratus lumborum block at the lateral supra-arcuate ligament (QLB-LSAL) is a new form of interfascial plane block reported in 2020, and its advantage over TAPB is that the local anesthetic (LA) can diffuse into the low thoracic paravertebral space.9,10 To our knowledge, there is no definitive study to demonstrate the analgesic effect of QLB-LSAL in patients undergoing open hepatectomy.
Therefore, our study aimed to confirm the hypothesis that QLB-LSAL could improve postoperative analgesia, reduce opioid consumption and promote early postoperative recovery quality when compared with TAPB.
Methods
Study Design and Population
This prospective, single-blinded, randomized, controlled study was conducted at the Affiliated Hospital of Xuzhou Medical University, adhering to the Consolidated Standards of Reporting Trials (CONSORT) statement and the Declaration of Helsinki. The study scheme was approved by the medical ethics committee of the Affiliated Hospital of Xuzhou Medical University, Jiangsu, China (XYFY2022-KL256-01). Then, it was registered with the Chinese Clinical Trial Register on 3 September 2022 (identifier: ChiCTR2200063291). This study was conducted between September 2022 and December 2022, and all participants signed the informed consent the day before surgery.
Inclusion criteria were as follows: (1) aged 18–65 years; (2) BMI 18.5–30.0 kg/m2; (3) American Society of Anesthesiologists (ASA) status I–III.
Exclusion criteria: (1) severe organ dysfunction or coagulation disorders; (2) diabetes; (3) history of chronic pain; (4) analgesic drugs including opioid abuse or addiction; (5) infection on the injection site; (6) history of allergy or contraindication to LA; (7) the existent scar blocking the spread of LA; (8) inability to communicate; (9) failure to block before surgery.
Randomization and Blinding
The patients were randomly divided 1:1 into either the QLB-LSAL group (group Q) or the subcostal TAPB group (group T) in terms of a computer-generated block randomization list. The grouping was kept in sealed envelopes by an anesthesia assistant with no involvement in this study. The blocks were performed by the same experienced regional anesthesiologist, withdrawing from anesthesia management. The postoperative follow-up assessments were conducted by an evaluator blinded to the group allocation.
Preoperative Nerve Block
All patients were monitored after entering the anesthesia induction room for preoperative preparation, including pulse oximetry, 5-lead electrocardiogram and invasive arterial blood pressure. The fluid intake was limited after a peripheral intravenous access to infusion. The patients underwent ultrasound-guided nerve blocks before general anesthesia induction.
Ultrasound-Guided QLB-LSAL
The patients were placed in a prone or lateral decubitus position before disinfecting the skin strictly. The low-frequency curvilinear probe (diagnostic ultrasound system, model Navis, Shenzhen Wisonic Medical Technology Co., China) was placed between the T12 rib and the tip of the L1 transverse process (TP) by a sagittal scan. Then the probe was shifted cephalad or caudally so as to confirm that the T12 rib, the L1 TP, the L2 TP, the quadratus lumborum (QL) and diaphragm were all displayed on the ultrasound images. After local infiltration, using 3 mL of 2% lidocaine, a 22G, 120-mm needle (Braun, Ogaki, Japan) was applied to puncture by in-plane insertion caudally, until the needle penetrated the QL and reached the target between the QL and diaphragm (Figure 1).10,11 After injecting approximately 2–3 mL of normal saline to identify the correct position, 20 mL of 0.5% ropivacaine was injected with repeated aspiration. The identical procedure was duplicated on the opposite side. The separation between the QL and diaphragm indicated a successful diffusion plane.
 |
Figure 1 Ultrasound image of quadratus lumborum block at the lateral supra-arcuate ligament. Abbreviations: QL, quadratus lumborum; TP, transverse process. |
Ultrasound-Guided TAPB
The patients were placed in a supine position. Then the high-frequency linear array probe was placed parallel to the anterior subcostal margin and moved laterally until the transversus abdominis lying posterior to the rectus abdominis muscle was identified. Meanwhile, the external oblique muscle, the internal oblique muscle and the transversus abdominis were also presented under ultrasound. A 22G, 50-mm needle was inserted in the fascial plane at the lateral migration between the rectus abdominis muscle and the transversus abdominis (Figure 2). After the correct position was verified, 20 mL of 0.5% ropivacaine was injected per side for bilateral block.
 |
Figure 2 Ultrasound image of transversus abdominis plane block. Abbreviations: EOM, external oblique muscle; IOM, internal oblique muscle; RAM, rectus abdominis muscle; TA, transversus abdominis. |
The bilateral block levels were evaluated regularly with pinprick sensation within 30 min. A successful blockade was defined as the block plane of right abdominal wall above T7 level.
Intraoperative Management
General anesthesia was induced after the blocks by intravenous injection of midazolam 0.05 mg kg−1, etomidate 0.2–0.3 mg kg−1, sufentanil 0.5 ug kg−1 and cis-atracurium 0.15–0.2 mg kg−1. Palonosetron 75 ug was also used for antiemetic. The mechanical ventilation mode was set to volume control, and the adjustment of respiratory rate was properly to maintain PetCO2 at 35–45 mmHg. Anesthesia was maintained by inhaled 1% sevoflurane, intravenous infusion of propofol 2~4 mg·kg−1·h−1, remifentanil 0.05–0.3 µg·kg−1·min−1 and cis-atracurium 0.1 mg·kg−1·h−1, which were adjusted at any time in order to sustain blood pressure and heart rate within 30% of baseline value and bispectral index values of 40–60. Intraoperative sufentanil (0.1–0.2 ug kg−1) was supplemented according to the surgical needs and hemodynamic indicators. Ketorolac tromethamine 30mg was injected intravenously 30min before the end of the operation.
Postoperative Pain Management
After completing the surgery, patients were monitored in the post-anesthesia care unit (PACU) and received the patient-controlled intravenous analgesia (PCIA) subsequently. The PCIA was composed of sufentanil 100 ug, tropisetron 6 mg and 0.9% normal saline in 100 mL, delivering a bolus of 2 mL with a lockout interval of 15 min and no background infusion. All patients and their families received guidance on the PCIA pump usage at preoperative interview and once again at the ward room after surgery, the PCIA button could be pressed when they experienced unbearable pain. In addition, the patients would request rescue analgesia with a single intravenous injection of dezocine 5 mg, if the pain intensity was not relieved after 2 bolus doses continuously.
Outcomes and Assessment Scales
The primary outcome was cumulative total morphine equivalent consumption at postoperative 24 h (from the end of surgery to the time of event occurrence). The other outcomes included cumulative total morphine equivalent consumption at other points (2, 6, 12, 48 h postoperatively); NRS (numerical rating scale) pain scores at postoperative 2, 6, 12, 24, 48 h; rescue analgesia rates at 48 h postoperatively, time to first PCIA request, time to first rescue analgesia, time to first ambulation and flatus; blood glucose at T0 (preoperative rest), T1 (hepatectomy) and T2 (skin suture); intraoperative use of propofol, sufentanil and remifentanil; invalid bolus times (difference between actual and effective bolus times) in PCIA and Quality of Recovery-15 (QoR-15) scores in the first postoperative 24, 48 h; postoperative length of stay and analgesia satisfaction scores before discharge. Besides, we also monitored the occurrence of opioid-related side effects (respiratory depression, PONV, pruritus) and block-related adverse events (diaphragm injury, hematoma, local anesthetic systemic toxicity (LAST), lower limbs weakness).
The QoR-15 scale with 15 questions consisted of physical comfort and independence, emotional state, psychological support and pain. The score range was 0–150, positively correlated with the recovery quality. The NRS was scored from 0 to 10 for gauging pain severity (0 = “no pain”, 10 = “imaginable worst pain”). The scoring criteria of analgesia satisfaction scores was similar with NRS, while a score of 10 represented extreme satisfaction.
Statistical Analysis
According to our previous pilot study, the cumulative total morphine equivalent consumption (mean ± SD) at postoperative 24 h was 41.78 ± 13.28 mg in the TAPB group and 31.67 ± 12.03 mg in the QLB-LSAL group. Twenty-six patients per group were assigned based on a two-tailed alpha level of 0.05 and power level of 0.8. Considering the 15% of dropouts, we recruited 62 patients totally in the study.
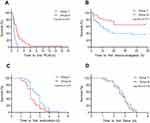
All data were analyzed by SPSS Software (version 26.0, IBM, New York, USA) and GraphPad prism 8.0 (GraphPad Software, San Diego, USA). The normality of continuous data distribution was determined by the Shapiro–Wilk test and presented as mean ± standard deviation (SD) or median ± interquartile range (IQR). The unpaired t-test or Mann–Whitney U-test was performed for the comparisons in the two groups according to data normality. The comparisons within group were analyzed by repeated measures analysis of variance (ANOVA) or Friedman test. Categorical data were reported as frequency (n) and percentage (%), using the Chi-square test or Fisher’s exact test for comparison between the groups. The cumulative morphine equivalent consumption was expressed by the 95% CI of median difference. Simple linear regression was used to analyze the correlation between total morphine equivalent consumption and recovery quality. The time-to-event data were represented by Kaplan–Meier survival curve and Log rank test. The statistically significant level was set at p < 0.05.
Results
A total of 65 patients were approached and recruited for this study, of whom 3 cancelled the operation in advance. Then, the remaining 62 patients were allocated randomly (n=31/group). Two patients in group Q were excluded for more than six-hour operation and withdrawing from PCA analgesia. One patient in group T entered the ICU after surgery, thus were excluded from the analysis (Figure 3). There were no statistically significant differences observed between the two groups in baseline characteristics (age, sex, BMI and ASA status) (P > 0.05, Table 1).
 |
Table 1 Demographic and Clinical Characteristics |
 |
Figure 3 Patient enrollment flow diagram. |
The group Q showed lower intraoperative use of sufentanil (41.2 [SD 7.7] vs 36.2 [SD 9.0] ug, P = 0.025) and remifentanil (3.1 [IQR 2.4–3.6] versus 2.5 [IQR 2.1–3.0], P = 0.046, Table 1). Blood glucose was not significantly different between the two groups at all time points (P > 0.05, Table 1). Nevertheless, there were significant differences at preoperative and intraoperative time points within the group (P < 0.05, Table 1).
Considering the primary outcome, cumulative total morphine equivalent consumption in the first postoperative 24 h was significantly decreased in group Q than that in group T (36.0 [IQR 26.5–50.0] versus 52.0[IQR 45.5–61.5] mg, 95% CI, 8.0 to 24.0 mg, P = 0.002). At 2, 6, 12 and 48 h postoperatively, cumulative morphine equivalent consumption was also significantly lower in group Q compared with group T (P < 0.01, Table 2 and Figure 4).
 |
Table 2 Cumulative Morphine Equivalent Consumption in the Postoperative Period (Mg) |
 |
Figure 4 Cumulative morphine equivalent consumption in Group T and Group Q. *P value < 0.05 vs Group T. |
NRS pain scores at rest and coughing were reduced 2, 6, 12 and 24 h postoperatively in group Q when compared with controls (P < 0.05, Figure 5). In contrast, the two groups had similar NRS pain scores at 48 h postoperatively. Repeated-measures analysis of variance on NRS pain scores showed significant difference in main effect of time or group effect, but interactions between the group and time intervals were non-significant (Figure 5).
Compared with group T, time to first PCIA request was significantly prolonged in group Q (0.83 [IQR 0.67–1.21] versus 1.77 [IQR 0.83–2.92]). The Kaplan–Meier survival curve analysis with the Log rank test proved a p value of <0.001 (Figure 6). Time to first rescue analgesia and time to first ambulation also revealed significant differences between the groups, whereas time to first flatus did not differ (P > 0.05, Figure 6).
Invalid bolus times in PCIA revealed significant difference between the groups over the 24–48 h postoperative period (P < 0.01, Table 3). Besides, a significant increase in QoR-15 recovery quality scores was observed among patients in group Q compared with those in group T at 24 and 48 h postoperatively (P < 0.01, Table 3). The QoR-15 scores were correlated negatively with cumulative total morphine equivalent consumption. The analgesia satisfaction scores were increased by 1 point in group Q compared with group T (95% CI 0–1, P = 0.001, Table 3).
 |
Table 3 Postoperative Analgesia and Recovery Conditions |
Postoperative length of stay was also similar. When comparing opioid-related side effects and adverse effects, no statistical significance was detected, and no patients experienced weakness of lower limbs in the groups (P > 0.05, Table 3).
Discussion
Our results showed that compared with TAPB, the preoperative QLB-LSAL combined with multimodal analgesia could significantly reduce postoperative 24 h morphine consumption by 31%, decrease pain intensity and rescue analgesia rates, prolong the duration of the first postoperative PCIA, and facilitate the early quality of recovery. Based on these findings, QLB-LSAL could be an effective and promising intervention to alleviate postoperative pain in patients undergoing open hepatectomy.
The incision of open hepatectomy usually ranges from 25 to 30 cm, which is 2 cm below the xiphoid process and approached the umbilical region downwards. The main causes of severe postoperative pain include dissection and resection of the lesion, transection of multiple anterior spinal nerve branches, and traction injury of intercostal nerves caused by prolonged traction of the ribs.2,12 Therefore, adequate postoperative pain control for this procedure requires to block somatic pain in at least the T7-T11 abdominal dermatomes and visceral pain. Given the knowledge presented in the above, we consider that the blocks should be performed bilaterally in relation to open hepatectomy.
TAPB is commonly applied to analgesia of the anterolateral abdominal wall, for blocking the thoracolumbar nerves which originate from the T6 to L1 spinal roots. There are clear distinctions in the width of the anesthetized field among all the approaches.5,13 Lee reported that the subcostal approach blocked a median of four segments, the most cephalad being T8 segments.14 Additionally, it also produced a marked effect where the lower end of the incision was at or above the T10 dermatome.15 The above findings suggest that the subcostal TAPB approach is suitable for upper abdominal surgery analgesia. Furthermore, a volunteer study showed that the subcostal approach gave rise to a dominantly anterior spread, little posterior spread and no spread to the paravertebral space.16 It seemed to explain anatomically that TAPB failed to provide visceral analgesia.
As an emerging technique for regional nerve blocks, quadratus lumborum block (QLB) is improved from lateral TAPB with the similar concept.17 Many studies have proposed different QLB approaches performed for postoperative analgesia in abdominal and hip surgery, including a posterior approach, a transmuscular approach, an intramuscular approach and a subcostal approach.18–22 In this study, we chose the approach at the lateral arcuate ligament (LAL), developed from subcostal QLB. The barrier action of the LAL can restrict the cephalad spread of LA.23 However, the injection site of QLB-LSAL is at the T12 rib and L1 transverse process, which means that LA is possible to circumvent the obstacle of LAL, spread into the lower thoracic paravertebral space directly, and cover the thoracic sympathetic trunk and somatic nerves.9–11 Based on this point, QLB-LSAL performs faster onset and wider dermatomal coverage than other approaches, with the block range of T9-T12 obtained 5 min after LA injection and the greatest cephalocaudal spread of T4-L3 finally.11 Our study used the same concentration and dose of ropivacaine, and found that the final sensory block of dermatomes was basically consistent with the above findings. Nevertheless, the slower onset could be related to different methods for determining the sensory blockade range, and we measured the dermatomal coverage with pinprick sensation, distinguished from abatement of temperature sensation.
The superiority of QLB over TAPB is also reflected in the duration of analgesia. A review showed that QLB extended pain-free condition to 24–48 h, yet the duration of TAPB was only 8–12 h.24 However, even though our study found that the opioid consumption and pain scores of group Q were significantly lower than those of TAPB at least 24 hours after surgery, we were not able to calculate the exact duration of analgesia for either block due to the lack of a non-blocking group.
In terms of the current anatomical evidence, the QLB-LSAL achieved an adequate somatic and visceral coverage, while most of TAPB approaches only provided somatic and not visceral analgesia.5,11 This study did not observe a demonstrable difference in the effect of the two blocks on visceral analgesia, as some patients had a blurred perception of the distinction between visceral and abdominal pain. Nevertheless, we observed that several patients who accepted QLB-LSAL felt only very mild surgical site pain in the early post-operative period, which could verify that the bilateral QLB-LSAL with PCIA provided a significant advantage in improving postoperative analgesia.
Our findings confirmed the hypothesis that QLB-LSAL was superior to TAPB in reducing postoperative opioid requirements and contributing to postoperative analgesia. This is consistent with studies on the other QLB approaches compared with TAPB in laparoscopic or open surgery.18,21,22 As we stated earlier, the use of long-lasting opioids in the postoperative period can increase the risk of opioid addiction, opioid-induced adverse events and immunological suppression.25 Regional nerve blocks have significant analgesic and opioid-sparing effects. A narrative review showed that compared with TAPB, QLB resulted in 2.5 to 7.5 mg decreases in morphine consumption at 24 h postoperatively in the open hysterectomy, cesarean section, or lower abdominal surgery.5 Therefore, we believed that the 24-h morphine requirement of this study was clinically significant in the 16 mg median difference, indicating the noticeable opioid-sparing effect of QLB-LSAL. Notably, although ERAS management was also carried out in the wards by routine intravenous low-dose flurbiprofen, the difference in analgesic effect was still significant between the groups, which showed that QLB-LSAL could add an analgesic advantage even in the presence of NSAIDs. Further, although there were no statistical differences in the incidence of postoperative PONV caused by more opioid consumption, the frequency of PONV in group Q was lower (13.3% vs 6.9%). This can be explained that the prophylactic antiemetic drug probably weakened this clinical variability.
The study also revealed the comparable postoperative pain scores both at rest and coughing within 24 h after surgery. The difference in NRS scores between the groups represented no clinical relevance, despite being statistically significant. In addition, the NRS pain scores reached the peak at 12h postoperatively. It may be explained as follows. The removal of substantial volume of liver resulted in the extended metabolic duration of anesthetic drugs and earlier blurred consciousness, and the early postoperative demands for PCIA boluses were not met in time.
Effective analgesia is not only reflected in lower opioid consumption, pain intensity and incidence of opioid-related adverse events, but also correlated closely with higher early postoperative recovery. The QoR-15 scale is a patient-centered measure of early health status after surgery and anesthesia, and the minimal clinically important difference (MCID) was reported as a change in value of 8.26 Our study reported that the QoR-15 scores at postoperative 24 h and 48 h were 12 and 10 points respectively higher in patients receiving QLB-LSAL than in TAPB, positively consistent with a notable decrease in cumulative opioid consumption. The above findings indicated an obvious clinical significance of QLB-LSAL to relieve postoperative pain and promote early recovery quality after surgery.
Patients who received QLB-LSAL did not have lower limb weakness in our study, which was attributed to partial lumbar plexus block and spread to the femoral nerve.27 The result was adverse to that of the Shi study, which reported that QLB-LSAL occurred in 16.7%.11 Moreover, no patient developed hematoma, LAST or organ injury in both groups. Murouchi reported that QLB led to lower peak arterial ropivacaine concentrations than TAPB, indicating higher safe values for the risk of systemic toxicity in patients.28
The TEA is also advocated for patients undergoing open hepatectomy, and some researchers are increasingly interested in analgesia effects of the two approaches. Aditianingsih had proven that the continuous QLB maintained the postoperative mean arterial pressure (MAP) and shortened urinary catheter usage, when compared to TEA.29 In several contrary studies, regardless of the QLB approaches, or whether a continuous catheter was implanted, the patients allocated to TEA consumed less opioids than those given QLB following open surgery. However, it was worth noting that TEA does not have an overall advantage in terms of other postoperative analgesia and recovery indicators.20,30 The difference in analgesic effect was probably affected by the surgical site, the incision range, the level of the catheter insertion and the doses of LA. Except perfect somatic and visceral analgesia, TEA may not only reduce intraoperative blood loss by the associated sympathetic blockade and vasodilatation, but also allow opioid-sparing and improve gastrointestinal function.1 However, considering simplicity and safety, TEA is more difficult to perform and is prone to complications such as LAST, orthostatic hypotension, catastrophic neurological injuries and epidural hematoma, especially for patients with coagulation disorders after hepatectomy.1,4,8 Therefore, even if there is no obvious advantage in analgesia, QLB-LSAL may still be a beneficial alternative, considering catheter-related damage caused by coagulopathy. Future studies could be conducted to evaluate the efficacy of QLB-LSAL versus TEA under other specific conditions.
We acknowledge that there are several limitations in our study. This study was single-center and small-sample, which might lead to some clinical indicators showing no statistical significance. Besides, we used a higher dose of ropivacaine in view of the analgesic requirements, which was not suitable for all populations. Since the lack of studies on QLB-LSAL, the optimal volume and concentration of LA still needs to be determined.
Conclusion
In conclusion, compared with bilateral single-injection TAPB, preoperative bilateral single-injection QLB-LSAL significantly lowered perioperative opioid consumption and pain intensity, shortened the time to first ambulation and promoted postoperative recovery quality after open hepatectomy. Therefore, the QLB-LSAL is a beneficial technique applied in multimodal analgesia. Further studies can be conducted to investigate the analgesia effect of QLB-LSAL in other types of abdominal surgery.
Data Sharing Statement
All participant data that support the findings of this study will be available for any reasonable request from the corresponding author, Ming Yan. The data will be accessible up to 6 months after publication date.
Disclosure
The authors declare no competing interests in this work.
References
1. Dieu A, Huynen P, Lavand’homme P, et al. Pain management after open liver resection: procedure-Specific Postoperative Pain Management (PROSPECT) recommendations. Reg Anesth Pain Med. 2021;46(5):433–445. doi:10.1136/rapm-2020-101933
2. Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–2298. doi:10.2147/JPR.S144066
3. Neuman MD, Bateman BT, Wunsch H. Inappropriate opioid prescription after surgery. Lancet. 2019;393(10180):1547–1557. doi:10.1016/S0140-6736(19)30428-3
4. Thornblade LW, Seo YD, Kwan T, et al. Enhanced recovery via peripheral nerve block for open hepatectomy. J Gastrointest Surg. 2018;22(6):981–988. doi:10.1007/s11605-017-3656-y
5. Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus Abdominis Plane Block. Anesthesiology. 2019;131(5):1166–1190. doi:10.1097/aln.0000000000002842
6. Kitlik A, Erdogan MA, Ozgul U, et al. Ultrasound-guided transversus abdominis plane block for postoperative analgesia in living liver donors: a prospective, randomized, double-blinded clinical trial. J Clin Anesth. 2017;37:103–107. doi:10.1016/j.jclinane.2016.12.018
7. Huang HM, Chen RX, Zhu LM, et al. Combined use of transversus abdominis plane block and laryngeal mask airway during implementing ERAS programs for patients with primary liver cancer: a randomized controlled trial. Sci Rep. 2020;10(1):14892. doi:10.1038/s41598-020-71477-x
8. Guo JG, Li HL, Pei QQ, Feng ZY. The analgesic efficacy of subcostal transversus abdominis plane block with Mercedes incision. BMC Anesthesiol. 2018;18(1):36. doi:10.1186/s12871-018-0499-3
9. Wang Y. A transverse approach for ultrasound-guided anterior quadratus lumborum block at the lateral supra-arcuate ligament. Anaesthesia. 2020;1–2. doi:10.1111/anae.15058
10. Li H, Shi R, Shi D, Wang R, Liu Y, Wang Y. Anterior quadratus lumborum block at the lateral supra-arcuate ligament versus transmuscular quadratus lumborum block for postoperative analgesia in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. J Clin Anesth. 2021;75:110561. doi:10.1016/j.jclinane.2021.110561
11. Shi R, Li H, Wang Y. Dermatomal coverage of single-injection ultrasound-guided parasagittal approach to anterior quadratus lumborum block at the lateral supra-arcuate ligament. J Anesth. 2021;35(2):307–310. doi:10.1007/s00540-021-02903-1
12. Zhu Q, Li L, Yang Z, et al. Ultrasound guided continuous Quadratus Lumborum block hastened recovery in patients undergoing open liver resection: a randomized controlled, open-label trial. BMC Anesthesiol. 2019;19(1):23. doi:10.1186/s12871-019-0692-z
13. Tsai HC, Yoshida T, Chuang TY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363. doi:10.1155/2017/8284363
14. Lee TH, Barrington MJ, Tran TM, Wong D, Hebbard PD. Comparison of extent of sensory block following posterior and subcostal approaches to ultrasound-guided transversus abdominis plane block. Anaesth Intensive Care. 2010;38(3):452–460. doi:10.1177/0310057X1003800307
15. Niraj G, Kelkar A, Jeyapalan I, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66(6):465–471. doi:10.1111/j.1365-2044.2011.06700.x
16. Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66(11):1023–1030. doi:10.1111/j.1365-2044.2011.06855.x
17. Blanco R, Garnier T, Komly B. 271: tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. 2007;32(5):130. doi:10.1016/j.rapm.2007.06.268
18. Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762. doi:10.1097/AAP.0000000000000495
19. Yoshida K, Tanaka S, Watanabe K, Obara S, Murakawa M. The effectiveness of the intramuscular quadratus lumborum block in postoperative analgesia after cesarean section with vertical incision: a randomized, double-blinded placebo-controlled study. J Anesth. 2020;34(6):849–856. doi:10.1007/s00540-020-02829-0
20. Elsharkawy H, Ahuja S, Sessler DI, et al. Subcostal anterior quadratus lumborum block versus epidural block for analgesia in open nephrectomy: a randomized clinical trial. Anesth Analg. 2021;132(4):1138–1145. doi:10.1213/ANE.0000000000005382
21. Huang D, Song L, Li Y, Xu Z, Li X, Li C. Posteromedial quadratus lumborum block versus transversus abdominal plane block for postoperative analgesia following laparoscopic colorectal surgery: a randomized controlled trial. J Clin Anesth. 2020;62:109716. doi:10.1016/j.jclinane.2020.109716
22. Xue Q, Chu Z, Zhu J, et al. Analgesic efficacy of transverse abdominis plane block and quadratus lumborum block in laparoscopic sleeve gastrectomy: a randomized double-blinded clinical trial. Pain Ther. 2022;11(2):613–626. doi:10.1007/s40122-022-00373-1
23. Elsharkawy H, Bajracharya GR, El-Boghdadly K, Drake RL, Mariano ER. Comparing two posterior quadratus lumborum block approaches with low thoracic erector spinae plane block: an anatomic study. Reg Anesth Pain Med. 2019;44:549–555. doi:10.1136/rapm-2018-100147
24. Akerman M, Pejcic N, Velickovic I. A review of the quadratus lumborum block and ERAS. Front Med. 2018;5:44. doi:10.3389/fmed.2018.00044
25. Dam M, Hansen C, Poulsen TD, et al. Transmuscular quadratus lumborum block reduces opioid consumption and prolongs time to first opioid demand after laparoscopic nephrectomy. Reg Anesth Pain Med. 2021;46(1):18–24. doi:10.1136/rapm-2020-101745
26. Myles PS, Myles DB, Galagher W, Chew C, MacDonald N, Dennis A. Minimal clinically important difference for three quality of recovery scales. Anesthesiology. 2016;125(1):39–45. doi:10.1097/ALN.0000000000001158
27. Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72(2):230–232. doi:10.1111/anae.13754
28. Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. 2016;41(2):146–150. doi:10.1097/AAP.0000000000000349
29. Aditianingsih D, Pryambodho AN, Tantri AR, Mochtar CA, Mochtar CA. A randomized controlled trial on analgesic effect of repeated Quadratus Lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019;19(1):221. doi:10.1186/s12871-019-0891-7
30. Gu B, Zhou H, Lian Y, et al. Ultrasound-guided anterior quadratus lumborum block at lateral supra-arcuate ligament vs thoracic epidural analgesia after open liver surgery: a randomized, controlled, noninferiority trial. J Am Coll Surg. 2022;235(6):871–878. doi:10.1097/XCS.0000000000000354
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.