Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
TRITRIAL: The Impact of Fixed Triple Therapy with Beclometasone/Formoterol/Glycopyrronium on Health Status and Adherence in Chronic Obstructive Pulmonary Disease in an Italian Context of Real Life
Authors Richeldi L, Schino P, Bargagli E, Ricci A , Rocca A, Marchesani F, Pennisi A, Camiciottoli G , D'Amato M, Macagno F, Scaffidi Argentina U, Ingrassia E , Piraino A
Received 9 November 2023
Accepted for publication 6 February 2024
Published 23 February 2024 Volume 2024:19 Pages 475—487
DOI https://doi.org/10.2147/COPD.S445858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jill Ohar
Luca Richeldi,1 Pietro Schino,2 Elena Bargagli,3 Alberto Ricci,4 Alberto Rocca,5 Francesca Marchesani,6 Alfio Pennisi,7 Gianna Camiciottoli,8,9 Maria D’Amato,10 Francesco Macagno,1 Ulrica Scaffidi Argentina,11 Eleonora Ingrassia,11 Alessio Piraino11
1Division of Pulmonary Medicine, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Università Cattolica del Sacro Cuore, Rome, Italy; 2Miulli Hospital, Acquaviva Delle Fonti, Bari, Italy; 3Respiratory Diseases Unit, Department of Medical and Surgical Sciences, Neuro Sciences, Siena University Hospital, Siena, Italy; 4Department of Medical-Surgical Sciences and Translational Medicine, Via di Grottarossa 1035, Sapienza University of Rome, Rome, Italy; 5Department of Respiratory Medicine, Bellaria Hospital, Bologna, Italy; 6Division of Pneumology, Ospedale di Macerata, Macerata, Italy; 7Department of Respiratory Medicine, Hospital Clinic “Casa di Cura Riabilitativa Calaciura”, Catania, Italy; 8Department of Biomedical, Experimental and Clinical Sciences, University of Florence, Florence, Italy; 9Department of Cardiothoracovascular, Careggi University Hospital, Firenze, Italy; 10UOSD Malattie Respiratorie ”Federico II”, Ospedale Monaldi, Napoli, 80131, Italy; 11Medical Affairs, Chiesi Italia S.p.A, Parma, Italy
Correspondence: Ulrica Scaffidi Argentina, Chiesi Italia S.P.A, Via Giacomo Chiesi 1, Parma, 43122, Italy, Tel +39 0521 1689690 ; +39 346 82 61 074, Email [email protected]
Purpose: The TRITRIAL study assessed the effects of beclometasone dipropionate/formoterol fumarate/glycopyrronium (BDP/FF/G) fixed combination in patients with chronic obstructive pulmonary disease (COPD) in a real-world setting, focusing on patient’s experience and perspective through the use of patients reported outcomes.
Patients and Methods: TRITRIAL was a multicenter, prospective, observational study conducted on patients with moderate-severe COPD treated with BDP/FF/G fixed therapy for 12 months. The main objective was to evaluate the impact of BDP/FF/G on health status through the COPD Assessment Test (CAT) score. Additional assessments included adherence and satisfaction, measured by the TAI-10/12 questionnaire and a specifically designed eight-item questionnaire, quality of life through the EQ-5D-5L test, sleep quality through the COPD and Asthma Sleep Impact Scale (CASIS), as well as safety and disease-related outcomes.
Results: Data from 655 patients were analyzed in the study. The mean total CAT score significantly improved (from 22.8 at baseline to 18.1 at 6 months and 16.5 at 12 months; p < 0.0001), as well as all the eight CAT sub-items, which decreased on average by 0.5– 0.9 points during the study. Adherence and usability of the inhaler also improved during the study, with a decrease in poor compliance (from 30.1% to 18.3%) and an increase in good compliance (from 51.8% to 58.3%) according to the TAI score. Patients also benefited from significantly improved quality of life (EQ Index from 0.70 to 0.80; EQ-5D VAS score from 55.1 to 63.1) and sleep quality (CASIS score from 41.1 to 31.8). Finally, patients reported a significant reduction in exacerbation during the study.
Conclusion: TRITRIAL showed that the BDP/FF/G fixed combination is effective and safe in patients with moderate-severe COPD and poorly controlled disease, improving patients’ HRQoL, sleep quality, adherence and inhaler usability and reducing COPD symptoms and the risk of exacerbation in a real-life setting.
Keywords: beclometasone/formoterol/glycopyrronium, chronic obstructive pulmonary disease, real-world, fixed triple therapy, adherence, patient-reported outcomes
Introduction
Triple therapy with inhaled corticosteroid (ICS), long-acting β2-agonist (LABA), and long-acting muscarinic antagonist (LAMA) is recommended for the treatment of patients with chronic obstructive pulmonary disease (COPD) who remain symptomatic and/or continue to experience exacerbations despite maintenance therapy with free or fixed combination double therapy.1
Triple therapy is available both as multiple-inhaler triple therapy (MITT), which requires the use of separate inhalers or as single inhaler triple therapy (SITT), in which three agents are combined in a single fixed-dose inhaler.
One of the fixed triple combinations available on the market is beclometasone dipropionate/formoterol fumarate/glycopyrronium (BDP/FF/G, Trimbow®, Chiesi Farmaceutici S.p.A.), which is approved in Europe for the maintenance treatment of adult patients with moderate-to-severe COPD who are not adequately controlled by the combination LABA/ICS or LABA/LAMA. The product is available in two fixed-dose inhalers, a pressurized metered-dose inhaler (pMDI) and the innovative multi-dose dry-powder inhaler NEXThaler, delivering an extra fine formulation.2 Data from regulatory trials, including three large Phase III studies (ie, TRILOGY,3 TRINITY4 and TRIBUTE)5 and a comparison study of the two inhalers (TRI-D trial)6 showed that BDP/FF/G fixed triple combination is superior to ICS/LABA, to LAMA monotherapy, and LABA/LAMA in terms of lung function and exacerbation prevention in COPD patients with a history of previous exacerbations. Moreover, the BDP/FF/G fixed triple combination is associated with a relevant and consistent improvement in patients’ health-related quality of life (HRQoL), assessed by the Saint George Respiratory Questionnaire (SGRQ).3–5
Despite the results reported in regulatory trials, the effects of fixed BDP/FF/G combination on patients’ HRQoL, treatment adherence and clinical outcomes need to be assessed in a real-world population to expand the evidence of conventional trials to a larger and more representative patients’ population. Real-world studies allow taking into consideration several factors that may influence a patient’s treatment in routine clinical practice, such as the complexity of treatment, the presence of comorbidities, issues with treatment adherence, polypharmacy, dosing frequency and improper inhaler technique.7–12 In particular, two aspects that should be further explored in the real-world setting are treatment adherence and inhaler usability, as they represent common challenges in the COPD population, especially in the case of multiple inhaler use.8,9 Adopting a single inhaler device may greatly facilitate patient treatment, increasing treatment persistence and adherence and reducing the number of errors, ultimately improving clinical effectiveness.10–12
In this paper, we report the results of TRITRIAL, an observational prospective multicenter study conducted in Italy to assess the effects of BDP/FF/G fixed combination on patients’ HRQoL, adherence and clinical outcomes in a real-world setting. The main focus of the study was understanding patients’ experiences and perspectives through patient-reported outcomes (PROs) focusing on quality of life, adherence, sleep quality and inhaler usability. Notably, the study was built for digital conduction, and patients were provided with electronically validated questionnaires available on their preferred hardware to facilitate compliance and data collection.
Methods
Study Design and Population
TRITRIAL was a multicenter, cohort, longitudinal, and prospective observational study conducted in 47 Italian respiratory medicine centers from August 2019 to March 2022. The study aimed to assess the impact of treatment with BDP/FF/G 87/5/9 µg pressurized metered dose inhaler (pMDI) fixed therapy on the health status and adherence of Italian COPD patients treated for 12 months as per clinical practice.13
Included patients were male and female subjects aged ≥40 years, with a diagnosis of moderate to very severe COPD, who had been prescribed and had started treatment with BDP/FF/G pMDI fixed combination as per local clinical practice and according to Trimbow® Summary of Product Characteristics (SmPC) within the previous 14 days, who had a COPD Assessment Test (CAT) ≥10 at the start of BDP/FF/G and at least one moderate–severe exacerbation during the previous year. Based on the clinician’s independent therapeutic judgment, the decision to prescribe and start treatment with BDP/FF/G was taken according to standard clinical practice and irrespective of the patient’s participation in the study. Patients were excluded if they participated in an interventional clinical trial within 30 days prior to enrolment and if they presented with any condition/illness contraindicating the conduct of the study according to the clinician’s evaluation.
The study plan included a brief retrospective phase to allow data collection from the time of the switch from previous therapy to BDP/FF/G to the patient’s enrolment. After an initial visit (baseline, Visit 1), patients were followed for up to 12 months and performed follow-up visits after 6±1 months (Visit 2) and 12±1 months (Visit 3).
The study was approved by the Ethics Committee of each clinical site and by the Ethics Committee of Policlinico Agostino Gemelli IRCCS (Rome) as the coordinating center (Supplementary Table 1). The study was conducted in compliance with the Declaration of Helsinki (1964 and amendments), current ICH E6 Good Clinical Practices and all other laws and regulations as applicable to non-interventional studies. All the patients provided written informed consent before enrollment to allow for participation in the study and use of data.
Study Objectives and Endpoints
The main objective of the study was to evaluate the impact of BDP/FF/G fixed combination on patients’ health status, as assessed by the change in CAT score from the time of initiation of BDP/FF/G fixed combination to month 12 (or early withdrawal). The CAT is an eight-item self-administered questionnaire easily used in daily clinical practice to assess the burden of COPD respiratory symptoms and the subject’s general health status (ie, lack of energy or sleep disturbances, limitations in doing activities at home or confidence leaving home) in patients with COPD.14
Secondary endpoints included adherence and satisfaction with the BDP/FF/G fixed combination, effect on HRQoL and sleep quality measured through different ePROs.
Treatment adherence was measured by the TAI-12 questionnaire, a validated questionnaire designed to evaluate adherence to inhaled therapy, which comprises both a patient domain (items from 1 to 10) and a physician domain (items 11 and 12), with higher scores indicating higher levels of treatment adherence.15 Questions from 1 to 10, giving a possible maximum score of 50, indicate level of adherence, classified as: good (score = 50), intermediate (score = 46–49), or poor (score ≤45). The questions for healthcare professionals are scored with 1 or 2 points (poor or good knowledge of the regimen and/or inhalation technique).
To better explore patients’ perspective towards the inhaler, the study measured patients’ satisfaction, perceived usability and ease of use, probably capturing also a comparison with previous therapies through the administration by the investigators of a set of eight questions in the form of an electronic 8-item non-validated questionnaire designed specifically for this study, in order to better understand practical aspects referred to the pMDI used in this study. Each item was assessed on a scale from 0 (fully disagree) to 5 (fully agree), with higher scores associated with greater patient satisfaction and device usability, evaluating the proportion of patients totally satisfied (Supplementary Table 2).
HRQoL was evaluated both through changes in total CAT score and individual CAT items and through the EQ-5D-5L test, a simple validated questionnaire that assesses quality of life on five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) and five levels of severity.16
Finally, sleep quality was measured through the COPD and Asthma Sleep Impact Scale (CASIS), a validated questionnaire used to measure sleep impairment associated with obstructive pulmonary diseases (eg trouble falling asleep in the night or staying awake during the day, sleep quality),17 and which may help identify patients with a higher risk of exacerbations.18
All the questionnaires were provided electronically via the Bring Your Own Device (BYOD) technology, which enables patients to provide study data using their own internet-enabled hardware, thus facilitating patients’ compliance and data collection.19
Secondary endpoints also included measurement of patients’ disease-related outcomes (eg, lung function parameters and occurrence of COPD exacerbations), economic resource consumption (data not shown) and the safety profile of BDP/FF/G fixed combination.
Exacerbations were classified according to the GOLD definition. Specifically, moderate exacerbations are those requiring treatment with short-acting bronchodilators plus antibiotics and/or oral corticosteroids, while severe exacerbations are those requiring hospitalization or access to the emergency room and may be associated with acute respiratory failure.20
Statistical Analysis
An initial sample size of 720 subjects was calculated with a paired distribution, considering an effect size of 0.144, predicted using a minimal clinically important difference of 1 in CAT score and a predicted pooled standard deviation of 6.9 – from previous studies3 with an alpha level of 0.01 (two-sided) and a power of 0.90. However, calculating a 10% dropout, a final sample of 800 subjects was established. R statistical analysis (version 3.5.2) with the pwr package was used to compute the sample size. The sample size was reconsidered after the second wave of the COVID-19 pandemic. Assuming the same effect size, minimal importance clinical difference and pooled standard deviation used to calculate the initial sample size, we recalculated a sample size of 560 patients with a power of 0.80.
Data from all the patients who signed the informed consent and received at least one administration of BDP/FF/G were considered for the safety endpoints; data from patients who also had a valid baseline assessment and at least one post-baseline evaluation of effectiveness were considered for the effectiveness endpoints. The primary and secondary effectiveness and safety results of the study are presented in the form of default descriptive statistics. Continuous variables are summarized by number of cases, mean, standard deviation (SD), median, minimum, and maximum. Categorical variables are summarized using counts of patients and percentages. Where appropriate, the 95% CI for means and percentages is presented.
The change of CAT over the study was analyzed using the analysis of variance for repeated measures; the change of CAT score from the start of treatment with BDP/FF/G (retrospective data) to endpoint (Month 12 or early withdrawal) was calculated with the two-sided 95% CI. For other secondary effectiveness variables, the two-sided 95% CI was calculated for changes from the start of treatment with BDP/FF/G (retrospective data) for CAT and pulmonary function tests and changes from baseline (Visit 1) for the other secondary effectiveness variables, to Month 6 and Month 12 (or early withdrawal).
Results
Patients’ Characteristics
In total, 656 patients were enrolled across 43 centers in Italy; one patient was excluded from the analysis because he/she did not receive at least one administration of BDP/FF/G (Supplementary Figure 1). The baseline demographics and clinical characteristics are summarized in Table 1. The majority were male (68.2%), the mean age was 71.2 years (range 41–91), most of the patients were ex-smokers (62.7%), and 25.6% were current smokers. Patients had approximately 10 years of COPD history; the mean total CAT score at baseline was 22.5 (SD 7.5); 89% of the patients had at least one moderate exacerbation during the last year, while 27% had at least one severe exacerbation; mean number of prior exacerbations per patient was 1.9 overall and 1.1 for severe exacerbations. Most patients (77.3%) had at least one comorbidity: the most frequent ones were vascular (42.6%), cardiac (25.3%), metabolic (22.7%) and gastrointestinal (11.8%) disorders. Concomitant diseases were present in the majority of the population (Table 1 and Supplementary Table 3), but the percentages of patients with concomitant asthma, rhinitis or allergic disorders were not relevant (data nor reported). Patients started BDP/FF/G approximately 6 days before informed consent signature; previous therapies included SITT (9.5%) and MITT (24.7%); reasons for switching from previous therapies to BDP/FF/G were mainly related to persistence of symptoms (74.5%) and exacerbations (55.6%) (Supplementary Table 4). Of note, 28.6% of the patients were not treated with ICS before starting treatment with BDP/FF/G.
 |
Table 1 Patients’ Baseline Characteristics |
CAT Score
Mean total CAT score significantly improved during the study, decreasing from 22.8 (95% CI: 22.3–23.3) at baseline to 18.1 (95% CI: 17.5–18.7) after 6 months (mean difference −4.7; p < 0.0001) and further decreasing to 16.50 (95% CI: 16.0–17.0) after 12 months of treatment (or early termination; mean difference −6.3; p < 0.0001) (Figure 1). Approximately 75.4% of the patients benefited from an improvement of at least 2 points in the mean total CAT score starting from 6 months after treatment; the improvement was also maintained after 12 months (75.0%; data not shown). The larger improvement in CAT score was measured in patients previously treated with bronchodilators (mean change −6.1 after 6 months and −7.2 after 12 months), followed by ICS + bronchodilator and free triple therapy (Supplementary Table 5).
 |
Figure 1 Change in mean total Chronic obstructive pulmonary disease Assessment Test score from baseline to 12 months. |
All eight CAT sub-items (cough, mucus, chest tightness, breathlessness, activities, confidence, sleep and energy) decreased on average by 0.5–0.9 points over the course of the study; the decrease was statistically significant for all the items both at 6 and 12 months compared with baseline (p < 0.0001) (Figure 2).
 |
Figure 2 Changes in CAT subcategories from baseline to 12 months. |
Adherence and Patient Satisfaction
At baseline, treatment compliance, according to TAI-10, was poor in 30.1% of the patients, moderate in 18.0%, and good in 51.8%. After 6 months, the percentage of patients with poor adherence decreased to 23.0%, moderate adherence increased to 26.5%, and good adherence was stable at 50.5%. Adherence further improved at 12 months (18.3% poor, 23.4% moderate and 58.3% good compliance). Overall, the TAI-10 total score increased from a mean of 46.4 (95% CI: 46.0–46.7) at baseline to 47.2 (95% CI: 46.8–47.6) at 6 months (mean difference +0.84; p < 0.001) and 47.8 (95% CI: 47.5–48.2) after 12 months (mean difference +1.47; p < 0.001) (Figure 3). Similar results were observed in terms of TAI-12, which captures also the reasons for lack of adherence and which score increased from 50.2 (95% CI: 49.8–50.5) at baseline to 50.9 (95% CI: 50.6–51.4) at 6 months (mean difference +0.79; p < 0.001) and 51.6 (95% CI: 51.2–51.9) after 12 months (mean difference +1.41; p < 0.001). Specifically, sporadic non-compliance increased from 45.1% at baseline to 47.2% at 6 months and 47.5% at 12 months; deliberate non-compliance decreased from 39.9% to 37.4% at 6 months and 38.9% at 12 months, while unconscious non-compliance increased from 5.1% to 8.8% and 12.1%, respectively, after 6 and 12 months (data not shown).
 |
Figure 3 Change in mean TAI-10 score from baseline to 12 months. |
Patient satisfaction and usability of the inhaler improved during the study; most importantly, the percentage of patients fully satisfied (ie, reaching the maximum score at every question composing the 8-item questionnaire) increased from 34.8% at baseline to 46.6% after 12 months (p < 0.001) and results were similar regardless of previously used therapy (Supplementary Table 6).
Quality of Life
The mean EQ Index significantly improved from 0.70 (95% CI: 0.68–0.71) at baseline to 0.79 (95% CI: 0.77–0.81) at 6 months (mean difference +0.09; p < 0.001) and to 0.80 (95% CI: 0.79–0.82) at 12 months (mean difference +0.10; p < 0.0001) (Figure 4A). Similarly, a statistically significant increase in EQ-5D VAS score was observed: mean score improved from 55.1 (95% CI: 53.8–56.3) at baseline to 60.6 (95% CI: 59.2–62.0) at 6 months (mean difference +5.50; p < 0.0001) and to 63.1 (95% CI: 61.9–64.4) at 12 months (mean difference +8.04; p < 0.0001) (Figure 4B).
 |
Figure 4 Change in mean EQ-5D Index (A) and VAS (B) from baseline to 12 months. |
Sleep
Mean CASIS total score improved from 41.1 (95% CI: 39.8–42.4) at baseline to 36.1 (95% CI: 34.7–37.6) at 6-month (mean difference −4.99; p < 0.0001) and to 31.8 (95% CI: 30.5–33.1) at 12-month (mean difference −9.33; p < 0.0001) (Figure 5). Statistically significant differences were observed from baseline to month 6 and month 12. Of note, the CAT subdomain related to sleep quality at baseline was 2.54 (95% CI: 2.4–2.6) vs 1.99 (95% CI: 1.8–2.1) at 6 months (mean difference −0.55; p < 0.0001) and 1.69 (95% CI: 1.6–1.8) at 12 months (mean difference −0.85; p < 0.0001) (Figure 2).
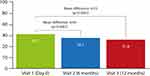 |
Figure 5 Change in mean CASIS score from baseline to 12 months. |
Lung Function and Exacerbations
In terms of clinical outcomes, after the initiation of the BDP/FF/G fixed combination, there was an improvement in lung function parameters, such as FEV1%, FVC%, and FEF25-75%; the improvement was maintained during the course of treatment, up to 12 months follow-up (Supplementary Table 7). Since many patients could not perform the complete set of lung function tests due to restrictions related to the COVID-19 pandemic, a separate analysis was conducted considering only patients who did perform all the assessments foreseen by the protocol (n = 34). The results showed that FEV1 in this population was stable throughout the study, with a mean absolute value equal to 1.3 L from treatment initiation up to 12 months follow-up.
A significant reduction was reported in the percentage of patients who experienced exacerbations in the past year, which decreased from 99.5% to 19.5%. The occurrence of moderate exacerbations was reduced from 89.0% to 14.6% of the patients, while severe exacerbations were registered in only 5.4% of the patients during the study, compared with 27.0% of the patients at baseline (Figure 6). Patients experiencing exacerbations were treated with systemic corticosteroids (64.4%), antibiotics (75.7%) or other medications (12.9%); 14.9% of the subjects were hospitalized due to the exacerbation (data not shown).
 |
Figure 6 Change in proportion of exacerbating patients before and after treatment with BDP/FF/G. |
Safety
In total, 36% of the patients experienced a treatment-emergent adverse event (TEAE), of which 11.6% experienced a serious TEAE. About 5.2% of the patients discontinued the study due to an adverse event. Only 2.9% of the patients experienced an adverse event that was judged as correlated with BDP/FF/G treatment; only one case was classified as a serious event. Additional details on the adverse events registered during the study are reported in Supplementary Table 8.
Discussion
This observational study provides evidence of the effectiveness and safety of the BDP/FF/G fixed combination in treating patients with COPD, highlighting the positive effects on patients’ HRQoL, sleep quality, inhaler usability and treatment adherence. The study has an observational nature, and its objectives did not contemplate a comparator arm; therefore, no comparison between drugs has been inferred.
The results corroborate previous findings from randomized clinical trials,3–6 and allow us to better understand the effects of BDP/FF/G in a larger population of real-life patients, taking into account the variability and common issues encountered in routine clinical care. Notably, the population under study was characterized by moderate-severe, poorly controlled (ie, at least one exacerbation in the previous year) COPD, and patients were prescribed triple therapy by their physicians due to the persistence of symptoms (74.5%) or persistent exacerbations (55.6%) despite habitual therapy. The criteria followed by clinicians for the prescription of triple therapy in the study thus reflected the indication of the use of BDP/FF/G as recommended by GOLD guidelines.1 Moreover, the study duration (ie, 1 year) was comparable to what is expected in standard clinical care, where patients suffering from a chronic disease, such as COPD usually require long-term treatments.
The advantage of real-life studies like TRITRIAL is to better understand the clinical course of the disease and therapy effectiveness in a population closer to real life compared to randomized trials. In this regard, we observed a high proportion of patients with comorbidities, mainly cardio-vascular ones, that represent a not negligible characteristic of COPD patients, able to affect prognosis and being progressively clarified and addressed by the scientific community. TRITRIAL shows that triple therapy is commonly used in these patients. Moreover, the study population included a portion of patients previously not treated with ICS. We acknowledge that this might have led to a potential increase in the therapeutic effect of BDP/FF/G measured on the whole population, especially in terms of exacerbation reduction and QoL improvement, as suggested by some randomized clinical trials.21 However, our data show that the effect of BDP/FF/G is statistically significant in patients naïve to ICS, as well as in patients previously treated with ICS-LABA or other treatments, and that no statistically significant difference is present between the sub-groups of patients with different previous therapies.
Overall, the study showed that patients with moderate-severe and poorly controlled COPD, with a history of exacerbations, starting BDP/FF/G fixed combination therapy benefited from a significant reduction in CAT total score, an improvement in HRQoL, and COPD-specific symptoms, improvement of sleep quality and better adherence to treatment and satisfaction with the device. These results are in line with those reported in similar observational studies on the use of triple therapy in patients with COPD. The TriOptimize study showed that switching from dual/triple therapies with multiple inhalers to extra-fine single-inhaler triple therapy was associated with an improvement of HRQoL, COPD-specific symptoms, lung function parameters and adherence, measured with TAI-12 among German patients with moderate-severe COPD and poor symptom control.22 Similarly, the Austrian real-world study TRICOP reported an improvement in lung function, symptom control and a significant reduction in exacerbations in patients with COPD treated with BDP/FF/G over 52 weeks.23
One peculiar feature that sets TRITRIAL apart from previous observational studies is the patient-centric nature and the specific focus on capturing patients’ perceptions and points of view on the everyday use of the BDP/FF/G fixed combination. The majority of the endpoints of the study were PROs, and all the questionnaires were presented to patients through an online platform delivered through the BYOD technology. This user-friendly platform allows participants to express their opinions in an easier, more comfortable and less biased way.19 The digital approach was also fundamental to facing some of the challenges caused in 2020 by the SARS-CoV-2 pandemic, challenges that were also overcome thanks to the use of electronic informed consent forms and the implementation of remote visits.
In terms of results, TRITRIAL showed a significant reduction in the primary outcome, the CAT total score, a validated questionnaire commonly used in clinical practice and is a key determinant in assessing disease severity and guiding treatment according to GOLD guidelines.1,24 Notably, the average decrease in total CAT score over 6 and 12 months was −4.7 and −6.3 points, respectively, largely meeting the minimal clinically important difference (MCID) of −2.0 points.25 Moreover, all CAT sub-items decreased over the course of the study, showing an improvement in patients’ COPD symptoms, such as cough, mucus, chest tightness and breathlessness, but also activities, confidence, sleep and energy levels.
The improvement in patients’ HRQoL measured through the CAT score was also reflected by the improvement in the EQ-5D-5L test, a validated questionnaire commonly used to assess patients’ quality of life.16
Another important result is the improvement in sleep quality as measured both by the decrease in the CAT sub-item “sleep” (from 2.54 to 1.69 after 12 months) and by the improvement in the CASIS total score, with a mean difference of −4.99 and −9.33 points, respectively, after 6 and 12 months. To our knowledge, this is the first time the CASIS score has been used in a large-scale study to measure the effects of an approved drug; moreover, although no MCID has been established for this questionnaire, the results registered in the study were markedly positive and, therefore, possibly clinically impactful.
Treatment with BDP/FF/G fixed combination was also associated with a remarkable improvement in treatment adherence. According to TAI-10, the percentage of patients with poor adherence decreased from 30.1% to 18.3% over 12 months; at the same time, good adherence was well maintained and even slightly increased during the study (from 50% to 58%). A limitation of this questionnaire is the lack, so far, of an MCID in the literature; however, it is now a well-established tool in the real-life contest, and it is being more and more used to assess the level of adherence at different visits.22,23,26 Moreover, the improvement in treatment adherence with extrafine triple therapy has been reported in other observational studies using the TAI score.22,26,27 On average, the level of adherence reported in this study was already acceptable at the first visit (average score of 46.3). This is probably explained by the fact that patients included in the study represent a cohort that has already started therapy with BDP/FF/G. The statistically significant numerical difference at 6 and 12 months vs baseline was important to evaluate the adherence trend over the study period.
The improvement in treatment adherence is particularly relevant as poor compliance is one of the main issues reported with inhalation therapy,28 especially when multiple inhalers are needed, and it is recognized as a negative factor in long-term treatment success.29,30 The fixed combination and the use of a single inhaler seem beneficial in increasing long-term adherence and could improve symptom control, reduce the exacerbation risk, and even potentially decrease healthcare costs.11,31,32
In parallel, the study allowed us to assess the potential impact of patients’ satisfaction in supporting treatment adherence, thanks to a set of questions chosen to evaluate the usability of the device. These questions were developed as a specific tool for this study, as no validated questionnaire is commonly used in clinical practice to highlight aspects related to the inhaler’s features and patients’ perspectives from a practical point of view. It was very interesting to observe patients showing complete satisfaction, thus reaching the maximum score for every item in the questionnaire. The prevalence of complete satisfaction improved during the course of the study, as well as good adherence.
Finally, the occurrence of exacerbations was massively decreased over the study, with the percentage of patients experiencing an exacerbation in the past 12 months dropping from 99.5% to 19.5%, therefore confirming the beneficial effects of BDP/FF/G fixed combination in controlling the risk of exacerbation in this population. Lung function parameters also improved after initiating the BDP/FF/G fixed combination and were maintained for up to 12 months of follow-up. Notably, the collection of these parameters was heavily limited by the COVID-19 pandemic. Therefore, it was not possible to have a complete picture of the lung function in all the patients, and only 34 patients performed all the tests foreseen in the protocol.
One interesting aspect highlighted by the study is that the BDP/FF/G fixed combination is also used in patients previously treated with open triple therapy, thus suggesting that this treatment choice is frequent and appropriate in real life.
Conclusion
The TRITRIAL study shows a good safety profile and an improvement in health status over 12 months in moderate-severe COPD patients with poorly controlled disease, treated with BDP/FF/G extra-fine fixed combination in a real-life setting. Patients treated with the fixed triple therapy had experienced one or more exacerbations and were previously treated with bronchodilators, ICS-LABA or a different triple therapy but still required a step-up to triple therapy. In general, they had a long-lasting disease history and presented multiple comorbidities, thus accurately representing the population of COPD patients treated in real-life clinical practice. These figures are in line with the registered indication of these drugs and with the suggested therapeutic treatment algorithm, suggesting that this treatment can be considered appropriate for these patients. These results reinforce the evidence of pivotal trials on the value of BDP/FF/G fixed combination as a treatment option in COPD; moreover, the results are in line with those of similar observational studies, contributing to describing the real-life experience of COPD patients in Europe. Overall, an improvement in the cohort of patients treated with BDP/FF/G extra-fine fixed combination was shown in terms of HRQoL, COPD symptoms reduction reported in the CAT questionnaire, decreased proportion of patients experiencing exacerbations referred to the previous year, and sleep quality improved during 12 months. The improvement in patient clinical outcomes is also associated with an appreciation of the inhaler usability and a prevalently good treatment adherence, a key step for achieving a successful treatment in routine clinical practice.
Ethics Approval
All procedures performed were in accordance with the 1964 Helsinki Declaration and its later amendments, Good Clinical Practice and local applicable regulations. The present study was approved by the Ethics Committee of Policlinico Agostino Gemelli IRCCS (Rome) and all the centers involved in the study.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, USA, upon reasonable request.
Consent to Participate
All subjects provided informed written consent prior to enrollment in the study.
Consent for Publication
All subjects provided informed written consent for the publication of their data.
Acknowledgments
Editorial assistance was provided by Ambra Corti, Aashni Shah, Valentina Attanasio and Massimiliano Pianta (Polistudium, Milan, Italy).
Author Contributions
Study conception and design: AP, EI, USA, LR; collection and interpretation of data: AP, EI, USA, LR, FM; statistical analysis: AP, EI, USA; manuscript drafting: AP, USA, EI. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in revising or critically reviewing the article; agree on the journal to which the article will be submitted; agree all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage; agree to take responsibility and be accountable for the contents of the article.
Funding
The clinical study TRITRIAL is sponsored by Chiesi Italia S.p.A. The editorial assistance for the preparation of this manuscript is funded by Chiesi Italia S.p.A.
Disclosure
LR has received grants/research support from Roche and Boehringer Ingelheim; he has received honoraria or consultation fees from Boehringer Ingelheim, Promedior, Biogen, FibroGen, Sanofi-Aventis, Promedior, RespiVant, Roche, Celgene, Nitto, and Veracyte. GC reports personal fees from Astra Zeneca, Sanofi, and GSK, outside the submitted work. AP, USA and EI are employees of Chiesi Italia, Parma, Italy. The other authors report no conflicts of interest in this work.
References
1. Agustí A, Celli BR, Criner GJ, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir J. 2023;61(4):2300239. doi:10.1183/13993003.00239-2023
2. EMA. Trimbow summary of product characteristics. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/trimbow.
3. Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–973. doi:10.1016/S0140-6736(16)31354-X
4. Vestbo J, Papi A, Corradi M, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–1929. doi:10.1016/S0140-6736(17)30188-5
5. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084. doi:10.1016/S0140-6736(18)30206-X
6. Beeh KM, Kuna P, Corradi M, Viaud I, Guasconi A, Georges G. Comparison of dry-powder inhaler and pressurized metered-dose inhaler formulations of extrafine beclomethasone dipropionate/formoterol fumarate/glycopyrronium in patients with COPD: the TRI-D randomized controlled trial. Int J Chron Obstruct Pulmon Dis. 2021;16:79–89. doi:10.2147/COPD.S291030
7. Heddini A, Sundh J, Ekström M, et al. Effectiveness trials: critical data to help understand how respiratory medicines really work? Eur Clin Respir J. 2019;6:1565804. doi:10.1080/20018525.2019.1565804
8. Melani AS, Paleari D. Maintaining control of chronic obstructive airway disease: adherence to inhaled therapy and risks and benefits of switching devices. COPD. 2016;13(2):241–250. doi:10.3109/15412555.2015.1045972
9. Zucchelli A, Vetrano DL, Bianchini E, et al. Adherence to COPD free triple inhaled therapy in the real world: a primary care based study. Clin Respir J. 2020;14(8):732–739. doi:10.1111/crj.13190
10. Kocks JWH, Chrystyn H, van der Palen J, et al. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. NPJ Prim Care Respir Med. 2018;28(1):43. doi:10.1038/s41533-018-0110-x
11. Mäkelä MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–1490. doi:10.1016/j.rmed.2013.04.005
12. van der Palen J, Moeskops-van Beurden W, Dawson CM, et al. A randomized, open-label, single-visit, crossover study simulating triple-drug delivery with Ellipta compared with dual inhaler combinations in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:2515–2523. doi:10.2147/COPD.S169060
13. Richeldi L, Piraino A, Macagno F, Micarelli G, Ingrassia E. The impact of fixed triple therapy with beclometasone/formoterol/glycopyrronium on health status and adherence in chronic obstructive pulmonary disease (COPD) in an Italian Context of real life: the TRITRIAL Study Protocol. Int J Chron Obstruct Pulmon Dis. 2021;16:159–166. doi:10.2147/COPD.S286559
14. Gupta N, Pinto LM, Morogan A, Bourbeau J. The COPD assessment test: a systematic review. Eur Respir J. 2014;44(4):873–884. doi:10.1183/09031936.00025214
15. Plaza V, López-Viña A, Entrenas LM, et al. Differences in adherence and non-adherence behaviour patterns to inhaler devices between COPD and asthma patients. COPD. 2016;13(5):547–554. doi:10.3109/15412555.2015.1118449
16. Nolan CM, Longworth L, Lord J, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71(6):493–500. doi:10.1136/thoraxjnl-2015-207782
17. Pokrzywinski RF, Meads DM, McKenna SP, Glendenning GA, Revicki DA. Development and psychometric assessment of the COPD and Asthma Sleep Impact Scale (CASIS). Health Qual Life Outcomes. 2009;7:98. doi:10.1186/1477-7525-7-98
18. Lange P, Marott JL, Vestbo J, Nordestgaard BG. Prevalence of night-time dyspnoea in COPD and its implications for prognosis. Eur Respir J. 2014;43(6):1590–1598. doi:10.1183/09031936.00196713
19. Demanuele C, Lokker C, Jhaveri K, et al. Considerations for conducting bring your own “Device (BYOD) Clinical Studies”. Digit Biomark. 2022;6(2):47–60. doi:10.1159/000525080
20. Global initiative for chronic obstructive lung disease (GOLD). Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf.
21. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680. doi:10.1056/NEJMoa1713901
22. Gessner C, Trinkmann F, Bahari Javan S, et al. Effectiveness of extrafine single inhaler triple therapy in chronic obstructive pulmonary disease (COPD) in Germany - The TriOptimize study. Int J Chron Obstruct Pulmon Dis. 2022;17:3019–3031. doi:10.2147/COPD.S382405
23. Marth K, Renner A, Pohl W. TRICOP - A Real-world effectiveness study with a single-inhaler extrafine triple therapy over 52 weeks in Austrian patients with COPD. Respir Med. 2021;182:106398. doi:10.1016/j.rmed.2021.106398
24. Jones PW, Brusselle G, Dal negro RW, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. doi:10.1183/09031936.00177210
25. Kon SSC, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med. 2014;2(3):195–203. doi:10.1016/S2213-2600(14)70001-3
26. Porpodis K, Bartziokas K, Chatziapostolou P, et al. Extrafine single inhaler triple therapy effect on health status, lung function and adherence in COPD patients: a Panhellenic prospective non-interventional study - The TRIBUNE study. Respir Med. 2023;212:107219. doi:10.1016/j.rmed.2023.107219
27. Brusselle G, Himpe U, Fievez P, et al. Evolving to a single inhaler extrafine LABA/LAMA/ICS - Inhalation technique and adherence at the heart of COPD patient care (TRIVOLVE). Respir Med. 2023;218:107368. doi:10.1016/j.rmed.2023.107368
28. National report on medicines use in Italy Year 2021. Available from: https://www.aifa.gov.it/documents/20142/1740782/Rapporto-OsMed-2021_EN.pdf.
29. Restrepo RD, Alvarez MT, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3(3):371–384. doi:10.2147/COPD.S3036
30. Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. doi:10.1136/thx.2007.086041
31. Bosnic-Anticevich S, Chrystyn H, Costello RW, et al. The use of multiple respiratory inhalers requiring different inhalation techniques has an adverse effect on COPD outcomes. Int J Chron Obstruct Pulmon Dis. 2017;12:59–71. doi:10.2147/COPD.S117196
32. Lareau SC, Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:401–406. doi:10.2147/COPD.S14715
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
