Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Transarterial Chemoembolization Combined with Tyrosine Kinase Inhibitors Plus Immune Checkpoint Inhibitors for Advanced Hepatocellular Carcinoma: A Propensity Score Matching Analysis
Authors Gao B, Yang F , Zheng D , Hu S, Liu J, Liu H, Liu Y, Liu L, Wang R , Zhao Y, Cui C, Fang C, Yang J, Su S, Han Y , Yang X, Li B
Received 4 October 2023
Accepted for publication 5 December 2023
Published 13 December 2023 Volume 2023:10 Pages 2265—2276
DOI https://doi.org/10.2147/JHC.S443041
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mohamed Shaker
Benjian Gao,1,2,* Fengyi Yang,1,2,* Dongning Zheng,1,2 Shuai Hu,1,2 Jie Liu,1,2 Hong Liu,1,2 Yongfa Liu,1,2 LinXin Liu,1,2 Rui Wang,1,2 Yi Zhao,1,2 Cheng Cui,1,2 Cheng Fang,1,2 Jin Yang,1,2 Song Su,1,2 Yunwei Han,3 Xiaoli Yang,1,2 Bo Li1,2
1Department of General Surgery (Hepatopancreatobiliary Surgery), The Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China; 2Academician (Expert) Workstation of Sichuan Province, Metabolic Hepatobiliary and Pancreatic Diseases Key Laboratory of Luzhou City, The Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China; 3Department of Oncology, The Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoli Yang; Bo Li, Email [email protected]; [email protected]
Purpose: This study aimed to explore the clinical efficacy of transarterial chemoembolization (TACE) in combination with tyrosine kinase inhibitors (TKIs) plus immune checkpoint inhibitors (ICIs) (triple therapy) compared to TACE alone (monotherapy) for advanced hepatocellular carcinoma (HCC).
Material and Methods: Data of consecutive advanced HCC patients receiving triple therapy or monotherapy at our center between January 2019 and December 2022 were collected and retrospectively analyzed. Propensity score matching (PSM) and subgroup analyses were performed to reduce the bias between the two groups. The primary outcomes of the study were the overall survival (OS) and progression-free survival (PFS). The secondary outcomes were the objective response rate (ORR) and disease control rate (DCR).
Results: A total of 104 patients were enrolled in this study: 41 in the triple therapy group and 63 in the monotherapy group. After PSM analysis, each group included 37 patients. The median OS and PFS were significantly longer in the triple therapy group than in the monotherapy group in the whole cohort (median OS, 18.8 vs 11.7 months, P = 0.022; median PFS, 10.5 vs 6.4 months, P = 0.012) and after PSM (median OS, 19.6 vs 12.5 months, P = 0.030; median PFS, 10.5 vs 6.7 months, P = 0.008). Furthermore, the treatment modality was an independent prognostic factor for OS (hazard ratio [HR]: 0.449, 95% confidence interval [CI]: 0.240– 0.840, P = 0.012) and PFS (HR: 0.406, 95% CI: 0.231– 0.713, P = 0.002) according to the multivariate cox regression analysis. A greater ORR was also observed in the triple therapy group (ORR: 56.7% vs 32.4%, P = 0.035). No significant difference was observed in DCR between the two groups (83.7% vs 72.9%, P = 0.259).
Conclusion: The triple therapy was superior to the monotherapy regarding OS, PFS, and ORR of advanced HCC patients.
Keywords: hepatocellular carcinoma, transarterial chemoembolization, tyrosine kinase inhibitors, immune checkpoint inhibitors, efficacy
Introduction
Hepatocellular carcinoma (HCC) is the most prevalent type of primary liver cancer ranking as the third leading cause of cancer-related death worldwide.1 Most HCC patients are often diagnosed at an advanced stage due to the insidious onset of this disease and patients frequently have comorbidities of chronic liver disease. This limitation limits the feasibility of curative treatments such as surgical resection, liver transplantation, and ablation. The corresponding practice guidelines recommend transarterial chemoembolization (TACE) and systemic therapies for these patients to improve the overall prognosis.2,3
TACE has been established worldwide as the standard local treatment for intermediate and advanced HCC, with an overall objective response rate (ORR) ranging from 30% to 40%.4 However, the prognosis of patients receiving only TACE remains poor because most patients develop resistance after repeated treatment, probably due to the hypoxia-induced angiogenesis in the residual viable tumors after TACE.5 Therefore, the combination of TACE with systemic therapy is the preferred strategy for these patients. Several studies reported the efficacy of the combination TACE with tyrosine kinase inhibitors (TKIs, targeting angiogenesis), and most of these studies showed an improved progression-free survival (PFS) but without any significant overall survival (OS) benefit.6,7 In addition, the LAUNCH trial demonstrated that TACE combined with lenvatinib significantly prolonged the median OS in patients with advanced HCC compared to lenvatinib monotherapy (17.8 months versus 11.5 months).8 Thus, the combined treatments are promising in the management of advanced HCC and are still under investigation.
Immune checkpoint inhibitors (ICIs) have recently shown promising results in trials of advanced HCC, thus considering immunotherapy as a valid treatment to cure HCC. The IMbrave150 trial revealed that atezolizumab plus bevacizumab are significantly better in prolonging OS and PFS than sorafenib in patients with advanced HCC, making this combination the first-line treatment option.9 Additionally, dual-combination modalities of other systemic therapies, such as lenvatinib plus pembrolizumab10 and apatinib plus camrelizumab11 show promising results with tolerable toxicity. A meta-analysis showed that the triple combination of TACE, TKIs, and ICIs results in better short- and long-term outcomes of patients with unresectable HCC.12 Besides, numerous clinical trials on the triple therapy are in progress to confirm this synergetic effect, but the results have not yet been published.13,14 Therefore, in this work a retrospective was performed to evaluate the efficacy of TACE in combination with TKIs plus ICIs versus TACE alone for advanced HCC.
Materials and Methods
Study Design and Patients
This study was performed according to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Hospital of Southwest Medical University (Ethical number: 23,023). Written informed consent was not necessary due to the retrospective nature of the study. Consecutive patients with advanced HCC who received TACE in combination with TKIs plus ICIs (triple therapy group) or TACE alone (monotherapy group) in our hospital from January 2019 to December 2022 were screened.
The inclusion criteria were the following: (1) histologically or clinically confirmed diagnosis of HCC according to the current practice guidelines3,15; (2) Barcelona Clinic Liver Cancer (BCLC) stage B or C; (3) Child-Pugh grade A and B; (4) Eastern Cooperative Oncology Group performance status 0 or 1; (5) at least one radiologically measurable lesion; (6) patients received either TACE combined with TKIs plus ICIs or TACE monotherapy, with an interval ≤ 1 month between TACE and the initial administration of TKIs and ICIs. The exclusion criteria were the following: (1) patients with metastatic hepatic carcinoma or other primary malignancies; (2) combined with other treatments, including resection, ablation, or transplantation; (3) concomitant with contraindications for therapy; (4) absence of baseline clinical or imaging data; (5) incomplete follow-up data.
Collected baseline data included age, sex, etiology, cirrhosis, portal hypertension, ascites, Child-Pugh classification, tumor size, tumor number, portal vein tumor thrombosis (PVTT), presence of extrahepatic metastasis, and BCLC stage. The treatment strategy was decided by multidisciplinary teams, and the treatment to be performed was decided based on physicians’ discretion, financial burden and patient consent.
TACE Treatment
The TACE procedure was performed by experienced interventional radiologists following standardized procedures. In brief, a microcatheter was inserted through the right femoral artery, and angiography was performed to identify the tumor-feeding artery. Subsequently, chemoembolization was performed using superselective intra-arterial oxaliplatin (100–200 mg), 5-fluorouracil (500 mg), epirubicin (30–50 mg), and lipiodol (5–20 mL), followed by the administration of gelatin sponge particles.16 The specific regimen and dosage were determined based on factors such as tumor burden, body surface area, and physical condition. The need for repeat TACE was assessed based on the results of contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging (MRI) using “on-demand” mode.
Systemic Treatment
Sorafenib or lenvatinib were chosen as TKIs, the former as an oral administration of 400 mg twice daily, the latter as an oral administration of 8 mg (for patients weighing less than 60 kg) or 12 mg (for those weighing more than 60 kg) once daily, following practice guidelines and expert consensus. TKIs agents were discontinued 3 days before and after the TACE procedure. The ICIs camrelizumab and sintilimab were intravenously administered at a dose of 200 mg every 3 weeks. Patients received systemic treatments until unacceptable toxic effects or disease progression.
Follow-Up and Outcome Assessments
Enhanced CT/MRI scans and laboratory tests were performed during the follow-up period prior to each treatment session, with a frequency of every 2–3 months. OS was calculated as the time from the initial treatment to either death or the last follow-up. PFS was determined as the time from the initial treatment to the first indication of tumor progression, death, or the last follow-up. Tumor response was assessed by two independent radiologists with over five years of experience, following the modified Response Evaluation Criteria in Solid Tumors (mRECIST).17 The response was divided into complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD) depending on the results. The overall response rate (ORR) included both CR and PR, while disease control rate (DCR) was calculated as the combination of CR, PR, and SD. All patients were subjected to a routine follow-up until April 2023 or death.
Statistical Analysis
Statistical analysis was performed using IBM SPSS version 22.0 and R version 4.2.1. Propensity score matching (PSM) analysis was performed to minimize the impact of confounding factors between the two groups. A logistic regression model was used, incorporating the following variables: age, sex, etiology, Child-Pugh class, tumor size, tumor number, extrahepatic metastasis, PVTT, BCLC stage, and alpha-fetoprotein (AFP) level (≤ 400/> 400 μg/L). The nearest-neighbor matching method with a caliper of 0.2 was used to achieve a 1:1 matching between the groups.
Continuous variables were presented as median with interquartile range (IQR), and the comparison between groups was performed using either the Student’s t-test or the Mann–Whitney U-test. Categorical variables were presented as frequencies with proportions, and differences between groups were evaluated using the Chi-squared test or Fisher’s exact test. OS and PFS curves were plotted using the Kaplan-Meier method, and the difference was assessed using the Log rank test. The prognostic factors associated with OS and PFS were evaluated using Cox univariate and multivariate analyses. Variables with a P value < 0.10 in the univariate analysis were subjected to a further multivariable analysis. Moreover, a subgroup analysis was performed to compare the OS and PFS between the triple therapy group and the monotherapy group, taking into account the baseline characteristics. A value of P < 0.05 was considered statistically significant.
Results
Patient Characteristics
A total of 104 eligible patients were included in this study: 41 receiving TACE combined with ICIs plus TKIs and 63 receiving TACE alone (Figure 1). The baseline characteristics of all patients are listed in Table 1. Most of the patients were male with an age < 60 years. In total, 22 patients had extrahepatic metastasis, and 53 had portal vein tumor thrombus. Thirty (73.2%) patients in the triple therapy group were diagnosed with BCLC stage C compared to 45 (71.4%) in the monotherapy group. The mean follow-up period was 14.3 months. However, 74 patients remained (37 patients in each group) in the study cohort after performing PSM analysis in a 1:1 ratio. The median number of TACE sessions was 2 (IQR: 2–3) in the triple therapy group, compared to 3 (IQR: 2–3) in the monotherapy group (P = 0.536). No significant difference was observed between the two groups in any of the clinical variables.
 |
Table 1 Patient Baseline Characteristics of Triple Therapy and Monotherapy Groups Before and After PSM |
 |
Figure 1 Flowchart of the study. Abbreviations: HCC, hepatocellular carcinoma; BCLC, Barcelona Clinic Liver Cancer; TACE, transarterial chemoembolization. |
OS
The median follow-up time was 15.3 months (IQR: 11.00–21.63) in the triple therapy group and 10.7 months (IQR: 7.17–17.17) in the monotherapy group. Twenty-three (56.10%) patients in the triple therapy group and 44 (69.84%) in the monotherapy group died during the follow-up. The median OS in the triple therapy group (18.8 months, 95% CI: 12.07–25.53) was longer than that in the monotherapy group (11.7 months, 95% CI: 7.86–15.54, P = 0.022) before PSM (Figure 2A). The corresponding median OS was 19.6 months (95% CI: 11.52–27.74) and 12.5 months (95% CI: 17.50–17.42, P = 0.030, Figure 2B) after PSM. Moreover, subgroup analysis showed a significantly longer OS in the triple therapy group within the following subgroups: male, HBV-positive, tumor size ≥ 5cm, and BCLC stage C (Figure 3). Furthermore, the univariate and multivariate analyses revealed that extrahepatic metastasis (HR= 2.062, 95% CI: 1.069–3.975, P = 0.031) and treatment modality (HR = 0.449, 95% CI: 0.240–0.840, P = 0.012) were independent prognostic factors for OS (Table 2).
 |
Table 2 Univariate and Multivariate Analyses of Risk Factors for OS |
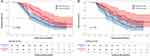 |
Figure 2 Kaplan–Meier survival curves for OS before PSM (A) and after PSM (B). Abbreviations: OS, overall survival; PSM, propensity score matching. |
PFS
Thirty (73.17%) patients in the triple therapy group and 54 (85.71%) in the monotherapy group showed a progression of the disease during the follow-up. The median PFS was 10.5 months (95% CI: 7.3–13.7) in the triple therapy group while it was 6.4 months (95% CI: 5.2–7.6) in the monotherapy group before PSM (P= 0.012), as shown in Figure 4A. The corresponding median PFS after PSM was 10.5 months (95% CI: 6.1–14.9) and 6.7 months (95% CI: 4.9–8.5, P = 0.008, Figure 4B). Besides, the subgroup analysis of PFS is shown in Figure 5. The triple therapy induced evident PFS benefits in the following subgroups: male, HBV-positive, tumor size ≥ 5 cm, AFP > 400 µg/L, and extrahepatic metastasis. In addition, extrahepatic metastasis (HR= 6.858, 95% CI: 3.471–13.55, P < 0.001) and treatment modality (HR = 0.406, 95% CI: 0.231–0.713, P = 0.002) were independent prognostic factors for PFS as revealed by the univariate and multivariate analyses (Table 3).
 |
Table 3 Univariate and Multivariate Analyses of Risk Factors for PFS |
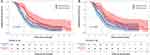 |
Figure 4 Kaplan–Meier survival curves for PFS before PSM (A) and after PSM (B). Abbreviations: PFS, progression-free survival; PSM, propensity score matching. |
Tumor Response
The best response evaluation results of the two groups are shown in Table 4. According to the mRECIST criteria, 3/18/10 patients in the triple therapy group had the best tumor response of CR/PR/SD compared with 1/11/15 of the monotherapy group. The ORR in the triple therapy group was significantly higher than that in the monotherapy group (56.7% vs 32.4%, P = 0.035). In addition, a trend towards a higher DCR was observed in the triple therapy group, although the difference was not statistically significant (83.7% vs 72.9%, P = 0.259).
 |
Table 4 Best Overall Response According to mRECIST |
Discussion
The administration of local therapy plus systemic agents has been widely applied in real-world implementation and resulted in significant survival improvements in patients with advanced HCC. The multicenter CHANCE001 trial in China demonstrated that TACE plus PD-(L)1 blockades and molecular targeted treatments significantly improve PFS, OS, and ORR versus TACE monotherapy for advanced HCC in real-world practice.18 Several other studies reported similar findings.19–21 These results suggest that the triple therapy can result in a satisfactory clinical efficacy. Therefore, a retrospective comparison of the efficacy of triple therapy compared to the monotherapy was performed, aiming to provide a more reliable basis for clinical decision-making.
The present study revealed that patients in the triple therapy group had significantly longer median OS and median PFS, as well as higher ORR than those in the monotherapy group, whereas a not significant trend in DCR was observed. In addition, similar results were obtained after PSM analysis, confirming the effectiveness of triple therapy for advanced HCC. Moreover, the triple therapy was an independent predictor of longer OS and PFS. This suggests that TACE combined with systemic therapy had a synergistic effect that improved the therapeutic efficacy against HCC. Theoretically, TACE induces tumor tissue necrosis, releases tumor antigens, and potentially transforms the immunosuppressive microenvironment into an immunosupportive form, thus promoting tumor-specific immune responses and enhancing the response of ICIs.22,23 Besides, TKIs promote the infiltration of effector lymphocyte cells into the tumor microenvironment through tumor vascular normalization, and alleviate hypoxia and immunosuppression, thereby exerting a synergistic effect with immunotherapy.24 Yang et al25 also found that cellular and humoral immunity are activated by triple therapy, and circulating IgG, Igλ, and Igκ serve as potential biomarkers. Overall, the aforementioned evidence lays a theoretical foundation for the amelioration of TACE effect when combined with TKIs plus ICIs.
Subgroup analyses were further conducted to identify the potential effectiveness of the triple therapy regimen. The results showed that this regimen was beneficial for OS in the subgroups of male, HBV-positive, tumor size ≥ 5 cm, and BCLC stage C, as well as for PFS in the subgroups of male, HBV-positive, tumor size ≥ 5 cm, AFP > 400 µg/L, and presence of extrahepatic metastasis. Similarly, Huang et al26 found that the triple therapy prolongs OS in male patients with PVTT and AFP > 400 µg/L. Besides, Chen et al27 demonstrated an increased survival after triple therapy correlated with the expression of PD-L1 in the tumor. The CHANCE001 trial showed that triple therapy is associated with a significant longer PFS and OS in patients with extrahepatic metastases and macroscopic portal vein invasion.18 Thus, combination therapy might yield superior survival benefits in these patients. The reason might be that TACE only controls intrahepatic lesions, while the systemic treatment alleviates extrahepatic metastases and vascular tumor thrombus. However, our subgroup analyses revealed that these patients had longer PFS, but not OS, which might be due to an insufficient sample size. Therefore, further efforts should focus on identifying the specific subset of HCC patients who might benefit the most from triple therapy to offer more precise treatment options.
To date, several studies reported the clinical outcomes of the triple therapy in the treatment of advanced HCC. A single-arm retrospective study revealed that TACE+TKIs+camrelizumab triple therapy achieved an ORR of 64.5%, a DCR of 77.4%, and a median PFS of 6.5 months in 31 patients with unresectable HCC.28 Cai et al19 revealed that the median OS and PFS in patients with advanced HCC after triple therapy were 16.9 months and 7.3 months, while our results obtained a slightly higher values. Wu et al29 demonstrated that drug-eluting bead TACE combined with lenvatinib and ICIs results in a higher ORR of 82.9%, a DCR of 91.4%, and a median PFS of 9.0 months in 35 patients with unresectable HCC. The differences in the results might be attributed to different baseline characteristics among the studies. For example, the proportions of patients with BCLC stage C (54.3%) and extrahepatic metastasis (8.6%) in Wu et al’s study29 was significantly lower compared to those observed in our study, and these features were associated with poor prognosis.
The heterogeneity in the selection of systemic therapeutic agents could also contribute to the observed differences in the results. Sorafenib and lenvatinib are now approved agents for first-line systemic treatment of advanced HCC thanks to the encouraging results in clinical trials.30,31 Currently, these two TKIs are still preferred in clinical practice and were also used in our study. ICIs such as camrelizumab and sintilimab have been covered by health insurance or by complimentary drug policies in China, which are much cheaper than atezolizumab, nivolumab, and pembrolizumab. Besides, the efficacy and safety of these two ICIs have been confirmed in randomized controlled trials for advanced HCC.11,32 In addition to camrelizumab and sintilimab, other ICIs such as tislelizumab, pembrolizumab, and toripalimab have also been used in similar studies.19,29 However, the optimal drug regimen for advanced HCC remains uncertain in real-world practice due to the heterogeneity of this tumor, and our study provided new insights into multi-drug combination therapy.
The present study has several limitations. First, the retrospective nature of our study inevitably leads to some potential biases. Although PSM and subgroup analyses were performed, this limitation cannot be completely avoided. Second, this study was conducted in a single center with a limited sample size, which may be a risk of selection bias. Third, the TKIs and ICIs agents used in our study were diverse; thus, it is difficult to avoid the confounding effects caused by the different drugs.
Conclusion
In conclusion, the triple combination of TACE, TKIs, and ICIs might be a promising and beneficial treatment for patients with advanced HCC, offering significant improvements in OS, PFS and ORR compared to TACE monotherapy. However, multicenter prospective randomized controlled studies are still needed in the future due to the limitations of this study, to further explore the optimal regimen of a combination therapy, the beneficiary populations, and the potential mechanisms to provide a reasonable guidance in the treatment of HCC.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the corresponding authors, without undue reservation.
Ethics Approval and Informed Consent
This study was performed according to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Hospital of Southwest Medical University (Ethical number: 23023). Given that this was a retrospective study of the patient’s anonymous clinical data and that no identifying information was used, the waiver of written informed consent was approved.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (No. 92059207), the Key Research and Development Project of the Science & Technology Department of Sichuan Province (Nos. 2022YFS0256, Nos. 2023YFQ0101).
Disclosure
The authors have no relevant financial or non-financial interests to disclose for this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–693. doi:10.1016/j.jhep.2021.11.018
3. Singal AG, Llovet JM, Yarchoan M, et al. AASLD practice guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023. doi:10.1097/hep.0000000000000466
4. Li QJ, He MK, Chen HW, et al. Hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin versus transarterial chemoembolization for large hepatocellular carcinoma: a randomized phase III trial. J Clin Oncol. 2022;40(2):150–160. doi:10.1200/jco.21.00608
5. Shim JH, Park JW, Kim JH, et al. Association between increment of serum VEGF level and prognosis after transcatheter arterial chemoembolization in hepatocellular carcinoma patients. Cancer Sci. 2008;99(10):2037–2044. doi:10.1111/j.1349-7006.2008.00909
6. Lencioni R, Llovet JM, Han G, et al. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: the SPACE trial. J Hepatol. 2016;64(5):1090–1098. doi:10.1016/j.jhep.2016.01.012
7. Kudo M, Ueshima K, Ikeda M, et al. Final results of TACTICS: a randomized, prospective trial comparing transarterial chemoembolization plus sorafenib to transarterial chemoembolization alone in patients with unresectable hepatocellular carcinoma. Liver Cancer. 2022;11(4):354–367. doi:10.1159/000522547
8. Peng Z, Fan W, Zhu B, et al. Lenvatinib combined with transarterial chemoembolization as first-line treatment for advanced hepatocellular carcinoma: a Phase III, randomized clinical trial (LAUNCH). J Clin Oncol. 2023;41(1):117–127. doi:10.1200/jco.22.00392
9. Cheng AL, Qin S, Ikeda M, et al. Updated efficacy and safety data from IMbrave150: atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J Hepatol. 2022;76(4):862–873. doi:10.1016/j.jhep.2021.11.030
10. Finn RS, Ikeda M, Zhu AX, et al. Phase Ib Study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol. 2020;38(26):2960–2970. doi:10.1200/jco.20.00808
11. Xu J, Shen J, Gu S, et al. Camrelizumab in combination with apatinib in patients with advanced hepatocellular carcinoma (RESCUE): a nonrandomized, open-label, Phase II trial. Clin Cancer Res. 2021;27(4):1003–1011. doi:10.1158/1078-0432.Ccr-20-2571
12. Ke Q, Xin F, Fang H, Zeng Y, Wang L, Liu J. The significance of transarterial chemo(embolization) combined with tyrosine kinase inhibitors and immune checkpoint inhibitors for unresectable hepatocellular carcinoma in the era of systemic therapy: a systematic review. Front Immunol. 2022;13:913464. doi:10.3389/fimmu.2022.913464
13. Ben Khaled N, Seidensticker M, Ricke J, et al. Atezolizumab and bevacizumab with transarterial chemoembolization in hepatocellular carcinoma: the DEMAND trial protocol. Future Oncol. 2022;18(12):1423–1435. doi:10.2217/fon-2021-1261
14. Llovet JM, Vogel A, Madoff DC, et al. Randomized Phase 3 LEAP-012 Study: transarterial chemoembolization with or without lenvatinib plus pembrolizumab for intermediate-stage hepatocellular carcinoma not amenable to curative treatment. Cardiovasc Intervent Radiol. 2022;45(4):405–412. doi:10.1007/s00270-021-03031-9
15. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the study of liver diseases. Hepatology. 2018;68(2):723–750. doi:10.1002/hep.29913
16. Lu J, Zhao M, Arai Y, et al. Clinical practice of transarterial chemoembolization for hepatocellular carcinoma: consensus statement from an international expert panel of International Society of Multidisciplinary Interventional Oncology (ISMIO). Hepatobiliary Surg Nutr. 2021;10(5):661–671. doi:10.21037/hbsn-21-260
17. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60. doi:10.1055/s-0030-1247132
18. Zhu HD, Li HL, Huang MS, et al. Transarterial chemoembolization with PD-(L)1 inhibitors plus molecular targeted therapies for hepatocellular carcinoma (CHANCE001). Signal Transduct Target Ther. 2023;8(1):58. doi:10.1038/s41392-022-01235-0
19. Cai M, Huang W, Huang J, et al. Transarterial chemoembolization combined with lenvatinib plus PD-1 inhibitor for advanced hepatocellular carcinoma: a Retrospective Cohort Study. Front Immunol. 2022;13:848387. doi:10.3389/fimmu.2022.848387
20. Wu JY, Yin ZY, Bai YN, et al. Lenvatinib combined with anti-PD-1 antibodies plus transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: a Multicenter Retrospective Study. J Hepatocell Carcinoma. 2021;8:1233–1240. doi:10.2147/jhc.S332420
21. Pan X, Wu SJ, Tang Y, Zhou YF, Luo JW, Fang ZT. Safety and efficacy of transarterial chemoembolization combined with tyrosine kinase inhibitor and immune checkpoint inhibitors for unresectable hepatocellular carcinoma: a single center experience. J Hepatocell Carcinoma. 2023;10:883–892. doi:10.2147/jhc.S404500
22. Pinato DJ, Murray SM, Forner A, et al. Trans-arterial chemoembolization as a loco-regional inducer of immunogenic cell death in hepatocellular carcinoma: implications for immunotherapy. J Immunother Cancer. 2021;9(9):e003311. doi:10.1136/jitc-2021-003311
23. Palmer DH, Malagari K, Kulik LM. Role of locoregional therapies in the wake of systemic therapy. J Hepatol. 2020;72(2):277–287. doi:10.1016/j.jhep.2019.09.023
24. Li SJ, Chen JX, Sun ZJ. Improving antitumor immunity using antiangiogenic agents: mechanistic insights, current progress, and clinical challenges. Cancer Commun. 2021;41(9):830–850. doi:10.1002/cac2.12183
25. Yang F, Xu GL, Huang JT, et al. Transarterial chemoembolization combined with immune checkpoint inhibitors and tyrosine kinase inhibitors for unresectable hepatocellular carcinoma: efficacy and systemic immune response. Front Immunol. 2022;13:847601. doi:10.3389/fimmu.2022.847601
26. Huang JT, Zhong BY, Jiang N, et al. Transarterial chemoembolization combined with immune checkpoint inhibitors plus tyrosine kinase inhibitors versus immune checkpoint inhibitors plus tyrosine kinase inhibitors for advanced hepatocellular carcinoma. J Hepatocell Carcinoma. 2022;9:1217–1228. doi:10.2147/jhc.S386672
27. Chen S, Wu Z, Shi F, et al. Lenvatinib plus TACE with or without pembrolizumab for the treatment of initially unresectable hepatocellular carcinoma harbouring PD-L1 expression: a retrospective study. J Cancer Res Clin Oncol. 2022;148(8):2115–2125. doi:10.1007/s00432-021-03767-4
28. Yang F, Yang J, Xiang W, et al. Safety and efficacy of transarterial chemoembolization combined with immune checkpoint inhibitors and tyrosine kinase inhibitors for hepatocellular carcinoma. Front Oncol. 2021;11:657512. doi:10.3389/fonc.2021.657512
29. Wu SJ, Ruan DD, Wu QY, et al. Safety and efficacy of drug-eluting bead transarterial chemoembolization combined with lenvatinib and anti-PD-1 antibodies for unresectable hepatocellular carcinoma: a retrospective analysis. J Hepatocell Carcinoma. 2023;10:807–820. doi:10.2147/jhc.S408819
30. Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi:10.1056/NEJMoa0708857
31. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–1173. doi:10.1016/s0140-6736(18)30207-1
32. Ren Z, Xu J, Bai Y, et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, Phase 2–3 study. Lancet Oncol. 2021;22(7):977–990. doi:10.1016/s1470-2045(21)00252-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


