Back to Journals » Clinical Epidemiology » Volume 13
The Validity of Danish Prescription Data to Measure Use of Aspirin and Other Non-Steroidal Anti-Inflammatory Drugs and Quantification of Bias Due to Non-Prescription Drug Use
Authors Gaster N , Hallas J , Pottegård A , Friis S, Schmidt M
Received 17 March 2021
Accepted for publication 8 June 2021
Published 13 July 2021 Volume 2021:13 Pages 569—579
DOI https://doi.org/10.2147/CLEP.S311450
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Natascha Gaster,1 Jesper Hallas,2 Anton Pottegård,2 Søren Friis,3 Morten Schmidt1,4
1Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark; 2Clinical Pharmacology, Pharmacy, and Environmental Medicine, Department of Public Health, University of Southern Denmark, Odense, Denmark; 3Danish Cancer Society Research Center, Danish Cancer Society, Copenhagen, Denmark; 4Department of Cardiology, Aarhus University Hospital, Aarhus, Denmark
Correspondence: Natascha Gaster
Department of Clinical Epidemiology, Aarhus University Hospital, Olof Palmes Allé 43-45, Aarhus N, DK-8200, Denmark
Tel +45 87168063
Fax +45 87167215
Email [email protected]
Purpose: To evaluate the potential of Danish prescription registries to capture aspirin and non-aspirin non-steroidal anti-inflammatory drug (NSAID) use and to quantitatively evaluate the magnitude of bias from misclassification of true NSAID and aspirin use as apparent non-use in drug outcome studies.
Patients and Methods: In a population-based cohort study, we retrieved sales statistics for NSAIDs and aspirins based on nationwide data from the Danish Health Data Authority and the Danish National Prescription Registry. We estimated prevalence of recorded and non-recorded NSAID use in the prescription registry and resulting proportions of true NSAID and aspirin use misclassified as apparent non-use from 1999 to 2019 at population and patient levels.
Results: The prevalence of true use misclassified as non-use (mainly due to over-the-counter use) peaked at 4.7% in 2012 for NSAIDs overall, 5.5% in 2012 for ibuprofen, and at 5.9% in 2002 for high-dose aspirin. Misclassification of other individual NSAIDs was near null. Misclassification of true low-dose aspirin use as non-use declined during the study period but remained around 1% since 2005. In subgroups of cardiac patients, the highest prevalence of true NSAID use misclassified as non-use was 5.0% in 2002 and 4.3% in 2017. Quantitative bias analyses showed how such misclassification of true NSAID and aspirin use as non-use remained minimal both at population and patient levels. In hypothetical examples simulating real study populations with differing exposure prevalence and prevalence of true NSAID and aspirin use misclassified as apparent non-use, the approximate percentage change due to misclassification of use as non-use did not exceed 5% and in most scenarios stayed around 1%.
Conclusion: The Danish prescription registries are valid data sources for assessing the effects of aspirin and NSAID use. The influence of non-recorded NSAID and aspirin use on estimates of association is virtually negligible.
Keywords: registries, over-the-counter, bias epidemiology
Introduction
Over the last decades, use of non-aspirin, non-steroidal anti-inflammatory drugs (NSAIDs) has increased.1 In addition to the well-established gastrointestinal side effects,2 evidence of cardiovascular risks associated with NSAID use has also accumulated.2,3 Outcomes related to NSAID and aspirin exposure are mainly studied by observational studies using healthcare registry data and therefore rely on accurate exposure data.3 In Danish pharmacoepidemiologic studies,4 NSAID and aspirin use are primarily identified from the Danish prescription registries.5–8 Using health registries to assess use of drugs that are not exclusively available on prescription requires consideration of potential exposure misclassification due to non-recorded drug use. Previous reports on the potential of Danish prescription registries to capture NSAID and aspirin use with consideration of over-the-counter (OTC) use did not take bulk hospital sales into account or evaluated the influence on drug outcome studies.1 We therefore investigated the potential of Danish prescription data to capture aspirin and NSAID use and evaluated the potential magnitude of bias from true NSAID and aspirin use misclassified as apparent non-use.
Patients and Methods
Setting
In Denmark, the tax-supported health-care system provides free and equal access to general practitioners and hospitals as well as partial reimbursement for prescription medications.4 A unique personal identifier, received upon birth or immigration, ensures linkage across all Danish health databases.9
NSAID and Aspirin Data
Total NSAID and aspirin sales are comprised of hospital and primary care sales. We obtained statistics for total, primary-sector, and hospital-sector sales for the total Danish population (5.8 million in 2019) from January 1, 1999, to December 31, 2019, from the Danish online drug use statistics MEDSTAT, managed by The Danish Health Data Authority.10 We assessed hospital drug sales and the proportion of OTC sales in primary care for each year of the study period to assess non-prescription use of NSAIDs and aspirins. The annual proportion of the Danish population with OTC dispensation or prescription filling of NSAID or aspirin was presented as the annual prevalence of use.
MEDSTAT has provided publicly available aggregate statistics on sales of pharmaceuticals since 1995 and complete statistics from 1999 onward.11 This online data source complements the Danish prescription registries with information on aggregate drug sales, including primary- and hospital-sector sales.11 Such data permit calculation of a wider range of descriptive statistics including proportion of sales by prescription while allowing for stratification by age, sex and region.11 Primary health care drug sales include sales from pharmacies, non-pharmacy outlets, the Danish Health Data Authority, and general practices. Hospital drug sales include all drug sales to hospitals, including private hospitals and private clinics.10
The Danish National Prescription Registry is based on prescription data from all Danish retail pharmacies.7 Each prescription record includes information on personal identifier, Anatomical Therapeutic Chemical (ATC) classification,12 quantity dispensed (including number and strength of the pharmaceutical entities, eg, tablets, and defined daily doses per package), and date of filled prescription, transferred electronically from all Danish pharmacies.5
Regulations of OTC NSAID Use
In Denmark, OTC NSAID and aspirin sales are limited to preparations of aspirin and low-dose ibuprofen.13 In addition, diclofenac was available OTC from July 16, 2007, to December 14, 2008.14 To reduce suicide attempts by analgesic overdose, the Danish Health Authorities have implemented several restrictions over the last 20 years.15–17 On October 1, 2004, packages of ≥30 tablets of aspirin and paracetamol were furnished with red label warnings alerting parents to read warnings and to store the drugs safely.15 On March 7, 2011, OTC sales of aspirin, paracetamol and ibuprofen were limited to persons ≥18 years and a maximum of one package per purchase.16 Since September 30, 2013, pack sizes have been further restricted to 10 g of aspirin, 10 g of paracetamol and 4 g of ibuprofen.17
Low-dose aspirin is primarily used as chronic thromboprophylaxis,18 which, like chronic use of high-dose ibuprofen and other NSAIDs, is more convenient on prescription, owing to reimbursement with reduced costs of the drugs and the OTC restrictions.5 In contrast, the vast majority of high-dose aspirin, and low-dose ibuprofen, is mostly used for acute transient pain conditions and remain available OTC.
Misclassification of True NSAID and Aspirin Use
Misclassification of true NSAID and aspirin use as non-use in register-based studies would result from OTC sales in primary care and bulk hospital drug sales. Misclassification of true non-use as NSAID or aspirin use will primarily result from patient non-adherence or stockpiling of prescribed NSAIDs or aspirins. In contrast, misclassification of true NSAID and aspirin use as non-use will be present in the apparently non-exposed group (ie, those without filled prescriptions) and depend on the proportion of NSAID and aspirin bulk sales in the hospital and community and the proportion of OTC use.
The proportion of OTC use of any NSAID and aspirin equals the prevalence of true use misclassified as apparent non-use by primary care sales. However, the impact of this prevalence of true NSAID and aspirin use misclassified as non-use depends on the prevalence of use, which leads to the misclassification of true use as non-use based on the hospital-sector sales proportion of NSAID and aspirin sales; this is equally true for the bulk sales proportion in the hospital sector. These estimates will be presented as misclassification of true NSAID and aspirin use as apparent non-use in the primary and hospital sectors, respectively.
Statistical Analyses
To explore the prevalence of true NSAID and aspirin use misclassified as apparent non-use based on NSAID and aspirin data from Danish prescription registries, we examined the following aspects: (1) The theoretical relationship between the proportion of non-prescription drug use and drug prevalence and the resulting misclassification of true use misclassified as apparent non-use; (2) the prevalence of true NSAID and aspirin use misclassified as non-use at the population level; (3) the prevalence of true NSAID and aspirin use misclassified as non-use at the patient level (using cardiac patients as example); and (4) the magnitude of bias resulting from such misclassification of true NSAID and aspirin use as non-use.
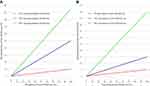
First, we illustrated how the prevalence of true NSAID and aspirin use misclassified as apparent non-use depends on both the prevalence of NSAID and aspirin use, ie, the number of individuals using NSAIDs and aspirins, and the prevalence of non-prescription NSAID and aspirin use. We assigned fixed values of either non-prescription NSAID and aspirin use or prevalence of NSAID and aspirin use, and the other parameter was assigned all possible values (0–100%) to simulate a multitude of possible study exposure compositions and resulting prevalence of true drug use misclassified as non-use.
Second, we calculated the annual proportion of in-hospital and community NSAID and aspirin sales in the total Danish population and the associated prevalence of true NSAID and aspirin use misclassified as apparent non-use in the entire population. Consequently, we identified the proportion of non-prescription NSAID and aspirin use based on hospital-sector sales and primary-sector OTC use for the total population. Estimates for the prevalence of true aspirin and NSAID use misclassified as non-use were calculated and graphically illustrated, overall and based on primary care and hospital sales, separately (1999–2019). Data on all individual NSAIDs and aspirins on the Danish market were included in the analyses (listed in Supplementary Material Tables S1–S6). Separate results were illustrated for the individual drugs comprising the majority of non-prescription NSAID and aspirin sales (ie, low-dose aspirin, high-dose aspirin, and ibuprofen).
Third, to ascertain clinical relevance of the population-level estimates, we calculated the prevalence of true NSAID use misclassified as apparent non-use in patients with cardiac disease, using actual prescribed proportions of NSAID use between 2002 and 2017.19 As specific OTC use for cardiac patients was not available, we used population-level OTC and hospital-sector sales proportions of total sales in the calculations. All graph trend lines were generated using smooth function; exact numbers are provided in Supplementary Tables S1–S6.
Lastly, to quantify bias on estimates of association due to misclassification of true NSAID and aspirin use as apparent non-use in drug-outcome studies, we calculated the magnitude of bias based on simulations of different prevalence of NSAID and aspirin use and true NSAID and aspirin use misclassified as non-use in a case–control design.
Results
The interplay between the prevalence of NSAID and aspirin use, non-prescription NSAID and aspirin use, and the resulting misclassification of true NSAID and aspirin use as non-use is illustrated in Figure 1. If the overall NSAID or aspirin prevalence is high (>20%), the non-recorded NSAID or aspirin use proportion has to be small to keep the prevalence of true NSAID or aspirin use misclassified as non-use low (Figure 1A, red line). However, if the proportion of non-recorded NSAID or aspirin use is high, the prevalence of true NSAID or aspirin use misclassified as non-use will remain minimal if the prevalence of NSAID or aspirin use is low (Figure 1B, red line).
Prevalence of True NSAID and Aspirin Use Misclassified as Non-Use at the Population Level
NSAIDs
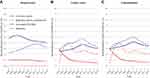
Over the 20-year study period, 97% of NSAIDs were sold in the primary care sector and 3% was used in the hospital sector. The overall NSAID prevalence, ie, the percentage of individuals using NSAIDs in the total population, including both hospital- and primary-sector use, increased from 16% in 1999 to 18% in 2002 and then decreased to 16% in 2019 (Figure 2 and Table S1). The prevalence of ibuprofen use in the total population was 9.3% in 1999, peaked at 16% in 2016, and then decreased to 14% in 2019.
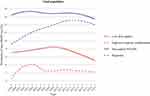 |
Figure 2 The proportion of the total Danish population using non-steroidal anti-inflammatory drugs (NSAIDs) in Denmark, 1999–2019. |
In the primary sector, the proportion of overall NSAIDs sold on prescription decreased from 85% in 1999 to 75% in 2013 and then increased to 78% in 2019 (Table S4). Ibuprofen constituted the main part of OTC use throughout the study period. The proportion of ibuprofen sold on prescription decreased from 70% in 1999 to 66% in 2012 and then increased to 74% in 2019 (Figure 3B). For overall NSAIDs, the prevalence of true NSAID use misclassified as apparent non-use due to OTC use varied between 2.5% and 4.3%, with a peak around 2012 (4.3%). True use of ibuprofen misclassified as non-use increased until 2012 (5.1%) and then decreased until 2019 (3.7%) (Figure 4B and Table S4). For all other individual NSAIDs, misclassification was near null (Table S5).
In the hospital sector, the proportion of total use of NSAIDs decreased from around 3.0% until 2009 to around 2.5% thereafter. The proportion of ibuprofen hospital use remained around 2.5% over the 20-year study period. The prevalence of true NSAID use misclassified as apparent non-use due to non-prescribed NSAID use in the hospital sector was low (<0.6%) for NSAID use overall and for all individual NSAIDs (Figure 4A and Table S3). This misclassification was stable throughout the study period (0.4–0.5%) (Figure 4A). Between 0.3% and 0.4% of true ibuprofen use was misclassified as non-use due to hospital-sector use in the study period.
Considering both the hospital and primary care sectors, the prevalence of true NSAID use misclassified as apparent non-use based on non-prescription drug use remained under 5%, peaking at 4.7% in 2012 (Figure 4C). A similar pattern of misclassification of true use as non-use was seen for ibuprofen, with a peak at 5.5% in 2012, decreasing to 4.0% in 2019. Likewise, misclassification of true use as non-use for all other individual NSAIDs remained almost non-existent throughout the study period (Table S6).
Aspirin
Like NSAIDs, total low-dose aspirin sales were mainly comprised of primary-sector sales (99% in 2019). The prevalence of low-dose aspirin use in the total Danish population increased from 7.0% in 1999 to 8.5% in 2009 and then decreased to 5.3% in 2019 (Figure 2 and Table S1). The prevalence of high-dose aspirin use peaked at 6.0% in 2002 and then decreased steadily until 2019 (2.5%).
In the primary care sector, the proportion of aspirin sales on prescription varied according to dose. Since 2006, the prescribed proportion of low-dose aspirin remained around 90%, whereas the majority of high-dose aspirin was OTC (7% on prescription in 2019) (Figure 3B and Table S4). The prevalence of true low-dose aspirin use misclassified as apparent non-use due to OTC use decreased from around 2.8% in 1999 to 0.6% in 2019 (Figure 4B and Table S5). True high-dose aspirin use misclassified as non-use due to OTC use increased until 2002 (5.9%) and then remained stable around 2.5% since 2006.
In the hospital sector, the proportion of low-dose aspirin use of total use was low (1.5% in 2019). Similarly, the proportion was low (0.05%) for high-dose aspirin throughout the study period (Figure 3A and Table S2). Misclassification of true low-dose aspirin use as non-use was stable around 0.1% from 1999 to 2019 and non-existent for high-dose aspirin (Figure 4A and Table S3).
Considering both the hospital and primary care sectors, misclassification of true aspirin use as non-use based on non-prescription use was similar to the results based solely on OTC use (Figure 4C and Table S6).
Prevalence of True NSAID Use Misclassified as Non-Use at the Patient Level
The prevalence of true NSAID use misclassified as apparent non-use did not differ substantially between the population and patient levels (Table 1). Among the different cardiac subgroups, the highest prevalence of NSAID use misclassified as non-use was overall 5.0% in 2002 and 4.3% in 2017.19 The corresponding estimates at the population level were 3.3% in 2002 and 3.4% in 2017. The calculation can be illustrated by the 1-year prescribed prevalence of NSAID use in 2002 among patients with angina pectoris (24.7%), who had the highest prevalence of NSAID use of the cardiac subgroups.19 Assuming a prescribed proportion equivalent to that of the total Danish population (85%) and a hospital-sector misclassification of true NSAID use as non-use of 0.6%, the prevalence of true NSAID use in patients with angina pectoris would be 29%, and the prevalence of true NSAID use misclassified as non-use would be 5.0% (calculations detailed in Table 1 footnote). The prevalence of true NSAID use misclassified as non-use was lower in all other cardiac subgroups who had lower prevalence of NSAID use (Table 1). Theoretically, in a subpopulation with 100% prevalence of true ibuprofen use and 30% OTC use, 30% of true ibuprofen use would be misclassified as non-use. However, it is unlikely that NSAID use would be comprised solely of ibuprofen. Moreover, since the prevalence of NSAID use in most cardiac subgroups was below 20%, it is unlikely that the prevalence of true NSAID use misclassified as apparent non-use would exceed 5% and even less likely 10% (upper limit included in Table 2).
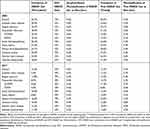 |
Table 1 Prevalence of True Non-Aspirin NSAID Use Misclassified as Apparent Non-Use in Subgroups of Patients with Cardiac Disease |
Impact of Misclassification on Estimates of Association
The size of bias resulting from misclassification of true NSAID and aspirin use as apparent non-use remains minimal as long as the prevalence of true NSAID and aspirin use misclassified as non-use is not overly large (Table 2). This fact can be illustrated in different hypothetical examples based on case–control studies with varying prevalence of NSAID exposure among cases and controls (Table 2). Assuming true NSAID use in the control group is similar to that of the total population (15% exposed and 85% non-exposed) and 20% of cases are true NSAID users, the resulting true odds ratio would be 1.42 (95% CI 0.68–2.96) (calculations detailed in Table 2 footnote). When assuming a 5% non-differential misclassification of true NSAID use as apparent non-use (see above), ie, 5% of the true NSAID users is allocated to the non-exposed group in both cases (19.0%) and controls (14.3%), it is possible to calculate the resulting biased odds ratio (1.41, 95% CI 0.67–2.99) and the approximate percentage change (0.36%) due to misclassification of true NSAID use as non-use. The impact on estimates of association from misclassification of true NSAID use as apparent non-use remained minimal despite changes in the prevalence of NSAID use among cases and controls, and thereby the derived magnitude of the point estimate, independent of study design (eg, cohort study) and sample size (Table 2).
Discussion
Population-level misclassification of true NSAID and aspirin use as apparent non-use has remained low during the last 20 years. The prevalence of hospital-sector- and primary sector-based misclassification of true NSAID and aspirin use as non-use has remained below 5.5% for NSAIDs and below 6.0% for aspirin and decreased since 2012. These population-level estimates did not substantially differ from the estimated prevalence of true NSAID use misclassified as non-use in subgroups of cardiac patients. Furthermore, the magnitude of bias on estimates of association due to misclassification of true NSAID and aspirin use as non-use was negligible.
The low prevalence of true NSAID and aspirin use misclassified as apparent non-use in the study period derived from both user prevalence and non-recorded drug use. Even for drugs with high unrecorded use, eg, high-dose aspirin use (93% OTC use), valid registry-based studies are feasible if the true prevalence is low, eg, 1%, as false-negative exposure in the apparently unexposed group in this example would be less than 1%, and no material misclassification of true use would be present in the exposed group. This relationship also explains why the prevalence of true NSAID and aspirin use misclassified as non-use varied over time as the two parameters are influenced by changes in guidelines and prescription practice. Until 2001, high-dose aspirin exhibited a low prevalence, resulting in low misclassification of true use despite nearly 100% OTC use. When the prevalence of high-dose aspirin increased in the population, so did the prevalence of true use misclassified as non-use. However, as OTC use began to decrease slightly, misclassification of true high-dose aspirin use was reduced likewise. The pattern for low-dose aspirin was mainly explained by an increasing OTC proportion (11% in 2019) and accentuated by a lower user prevalence in recent years, possibly due to the national Danish and European guidelines, no longer recommending low-dose aspirin as routine thromboprophylaxis in patients over 65 years in the absence of cardiovascular disease.20 For NSAIDs overall, the misclassification of true use as non-use was primarily due to OTC availability of ibuprofen. The increase in prescribed proportion of ibuprofen from 2012 to 2019 was paralleled by a lower user prevalence, resulting in a reduction in misclassified prevalence of true ibuprofen use as non-use. The recent increase in prescription use was probably due to the restrictions in OTC use of NSAIDs allowing only one daily package of 10–20 tablets,21 while the decrease in prevalence over the last two decades may partly be explained by increasing evidence of cardiovascular risks associated with NSAID use and the subsequent changes in guidelines.3,22 These examples demonstrate the impact of guideline changes on prevalence of true NSAID and aspirin use misclassified as non-use and emphasize the importance of considering such changes when evaluating potential bias.
Our estimates of the prevalence of true NSAID and aspirin use misclassified as apparent non-use were based on data from the total Danish population. Therefore, the results cannot readily be applied to other study populations if the prevalence of either true NSAID and aspirin use or non-prescribed use differs substantially from those of the general population. The OTC restrictions in Denmark limit potential misclassification of true use as non-use to ibuprofen and all preparations of aspirin. Thus, the only difference in non-prescription NSAID and aspirin use between specific study populations and the total Danish population depends on OTC proportions of these drugs. In most cases, as NSAID and aspirin prevalence increases, one would expect a simultaneously higher proportion of NSAID and aspirin use on prescription (low non-recorded drug use), which would further reduce bias from misclassification. Although the prevalence of true NSAID and aspirin use in specific study groups may differ from the population prevalence, the misclassification estimates will most likely not be substantially different, as also seen in our study.
We described the maximum population-level misclassification of true NSAID and aspirin use as apparent non-use in patients based on prescription registry data, as we did not account for non-adherence to non-prescription drugs in the registered non-user group. Patients registered as non-users, non-adhering to OTC drugs, would effectively be non-users and therefore not lead to misclassification and bias. Furthermore, any patient recorded as exposed had to have purchased and filled a prescription, and the exposed status was therefore not influenced by any unrecorded NSAID and aspirin use. However, in the apparently exposed group, there may be misclassification due to non-adherence. No data exist on patient adherence in the Danish prescription registries. However, the prescription registries include information on number of pharmaceutical entities, typically tablets, and defined daily dosages per prescription,5 which enable estimation of exposure more accurately, eg, in chronic users of low-dose aspirin who generally take one pill daily.23 In any case, as the Danish prescription registries prospectively record prescriptions, misclassification of true NSAID and aspirin use as apparent non-use due to non-adherence or non-recorded use would be non-differential and bias estimates towards the null. Thus, based on the presented data, the Danish prescription registries are reliable data sources for capture of aspirin and NSAID use with a large potential to reflect actual drug use. Risk estimates and etiologic fraction in the exposed group will not be affected by misclassification of the size observed. However, etiologic fraction in the population will be underestimated.
Strengths and Limitations
Complete data on prescribed and total sales in both the primary and hospital sectors from 1999 to 2019 were available through MEDSTAT.10 Although the number of OTC users was not available, data on proportion of sales on prescription enabled a sufficient evaluation. No data were available on non-recorded drug use by sex and age groups, as the publicly available data is not personally identifiable. This limited the possibility of estimating the prevalence of true NSAID and aspirin use misclassified as non-use between the two genders and within different age groups. It is conceivable that some OTC NSAID and aspirin use occurs concomitantly with prescribed NSAID and aspirin use. In these cases, there is no misclassification of exposure status, and our bias estimates would tend to be exaggerated. Unfortunately, there are no data to address the extent of co-used OTC and prescription NSAIDs and aspirins.
Conclusions
The Danish prescription registries can be considered valid data sources for assessing NSAID and aspirin use in Denmark, as the influence of non-differential misclassification of true drug use is negligible. Furthermore, we observed an accordance between population-level and patient-level estimates. This finding supports the value of studies of NSAID and aspirin exposure in different patient subgroups based on prescription registry data. For future use, it will be important to stay vigilant for any major change in either non-recorded proportion or user prevalence, especially in connection with guideline changes or changes in OTC availability.
Ethics Committee Approval
The study was based on publicly freely available data from the website www.medstat.dk and hence required no approval from either an institutional review board or ethics committee.
Disclosure
MS is supported by the Novo Nordisk Foundation (NNF19OC0054908). JH has participated in research projects funded by Novartis, Pfizer, Menarini, MSD, Nycomed, and Astellas, with grants paid to the institution where he was employed. JH has personally received fees for teaching or consulting from the Danish Association of Pharmaceutical Manufacturers, Nycomed, Pfizer, Novartis, AstraZeneca, Lundbeck, Menarini, Leo Pharmaceuticals, and Ferring. SF has personally received fees for teaching or consulting from the Danish Association of Pharmaceutical Manufacturers. The authors declare no other conflicts of interest.
References
1. Schmidt M, Hallas J, Friis S. Potential of prescription registries to capture individual-level use of aspirin and other nonsteroidal anti-inflammatory drugs in Denmark: trends in utilization 1999–2012. Clin Epidemiol. 2014;6:155–168.
2. Bhala N, Emberson J, Merhi A, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382(9894):769–779.
3. McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8(9):e1001098. doi:10.1371/journal.pmed.1001098
4. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi:10.2147/CLEP.S179083
5. Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, Sorensen HT, Hallas J, Schmidt M. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798f. doi:10.1093/ije/dyw213
6. Hallas J, Hellfritzsch M, Rix M, Olesen M, Reilev M, Pottegård A. Odense pharmacoepidemiological database: a review of use and content. Basic Clin Pharmacol Toxicol. 2017;120(5):419–425. doi:10.1111/bcpt.12764
7. Johannesdottir SA, Horváth-Puhó E, Ehrenstein V, Schmidt M, Pedersen L, Sørensen HT. Existing data sources for clinical epidemiology: the Danish National Database of reimbursed prescriptions. Clin Epidemiol. 2012;4:303–313. doi:10.2147/CLEP.S37587
8. Ehrenstein V, Antonsen S, Pedersen L. Existing data sources for clinical epidemiology: Aarhus University prescription database. Clin Epidemiol. 2010;2:273–279. doi:10.2147/CLEP.S13458
9. Schmidt M, Pedersen L, Sorensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
10. Danish Serum Institute. Statistics on the annual sale of medicines in Denmark based on the data from the register of medicinal product statistics. Available from: https://medstat.dk/.
11. Schmidt M, Hallas J, Laursen M, Friis S. Data resource profile: Danish online drug use statistics (MEDSTAT). Int J Epidemiol. 2016;45(5):1401–1402g. doi:10.1093/ije/dyw116
12. World Health Organization Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs. 2019. Available from: https://www.whocc.no/atc_ddd_index/.
13. Danish Health and Medicines Authority. Over-the-counter painkillers. Available from: https://laegemiddelstyrelsen.dk/en/pharmacies/over-the-counter-medicines/over-the-counter-painkillers/.
14. Danish Health and Medicines Authority. Report on the cardiovascular risk of non-selective NSAIDs (non-steroidal anti-inflammatory drugs). 2008. Available from: https://www.ft.dk/samling/20081/almdel/suu/bilag/265/645749.pdf.
15. Danish Health and Medicines Authority. Special warning on the labelling of pain relievers. April 8, 2011. Available from: https://laegemiddelstyrelsen.dk/en/licensing/licensing-of-medicines/spcs,-package-leaflets-and-labelling/special-warning-on-the-labelling-of-pain-relievers/.
16. Centre for Suicide Research. New age limit of 18 years for the purchase of painkillers. February 18, 2011. Available from: https://selvmordsforskning.dk/ny-18-aars-graense-for-smertestillende-medicin/.
17. Danish Serum Institute. Limit prescriptions of big packsizes of over-the-counter painkillers. 2013. Available from: https://www.sst.dk/da/udgivelser/2013/rationel-farmakoterapi-7-2013/begraens-recepter-paa-store-pakninger-af-smertestillende-haandkoebsmedicin.
18. Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86. doi:10.1136/bmj.324.7329.71
19. Schmidt M, Pottegård A. Prescriber responsibility, predictors for initiation, and 20-year trends in use of non-aspirin non-steroidal anti-inflammatory drugs in patients with cardiovascular contraindications: a nationwide cohort study. Eur Heart J Cardiovasc Pharmacother. 2020. doi:10.1093/ehjcvp/pvaa073
20. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. doi:10.1093/eurheartj/ehw106
21. Danish Serum Institute. Sale of weak painkillers has decreased following large pack sizes becoming prescription only. 2014. Available from: https://www.ssi.dk/aktuelt/nyheder/2014/2014-07_salg-smertestillende-laegemidler-receptpligt-store-pakninger_03072014.
22. Schmidt M, Olsen A-MS, Fosbøl EL, et al. Recommendation on NSAID use in patients with cardiovascular disease. Danish Society of Cardiology. 2016. Available from: https://www.cardio.dk/nsaid-behandling-hos-patienter-med-hjertekarsygdom.
23. Danish Pharmaceutical Information. Drugs and package sizes on the Danish drug market. Available from: https://pro.medicin.dk/.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.