Back to Journals » Cancer Management and Research » Volume 14
The Systemic Immune-Inflammation Index (SII) Increases the Prognostic Significance of Lymphovascular Invasion in Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy
Authors Jan HC , Wu KY, Tai TY, Weng HY, Yang WH, Ou CH , Hu CY
Received 16 June 2022
Accepted for publication 27 October 2022
Published 7 November 2022 Volume 2022:14 Pages 3139—3149
DOI https://doi.org/10.2147/CMAR.S378768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Hau-Chern Jan,1,2 Kuan-Yu Wu,1 Ta-Yao Tai,1 Han-Yu Weng,1 Wen-Horng Yang,1,3 Chien-Hui Ou,1,3 Che-Yuan Hu1,4
1Department of Urology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 2Division of Urology, Department of Surgery, National Cheng Kung University Hospital Dou-Liou Branch, Yunlin, 640, Taiwan; 3Department of Urology, College of Medicine, National Cheng Kung University, Tainan, 701, Taiwan; 4Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, Tainan, 701, Taiwan
Correspondence: Che-Yuan Hu; Chien-Hui Ou, Department of Urology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, No. 138, Sheng-Li Road, Tainan, 70403, Taiwan, Tel +886-6-235-3535, Fax +886-6-238-3678, Email [email protected]; [email protected]
Purpose: Lymphovascular invasion (LVI) and systemic immune-inflammation index (SII) both have been proved to correlate with oncologic outcomes in upper tract urothelial carcinoma (UTUC). We hypothesize that integrating SII with LVI may be an aid for risk-stratification of prognosis. This study aimed to evaluate the prognostic significance of combined SII and LVI in patients with localized UTUC.
Patients and Methods: A retrospective analysis of clinicopathological data of 554 UTUC patients who underwent radical nephroureterectomy (RNU) was conducted. The SII was calculated using the equation (preoperative serum neutrophil*platelet/lymphocyte). Use of Kaplan–Meier analyses and Cox proportional hazards models were to evaluate associations of combining SII and LVI with overall survival (OS), cancer-specific survival (CSS), and progression-free survival (PFS). Furthermore, receiver operating characteristic (ROC) analysis was applied to estimate predictive ability of combining SII and LVI for oncological outcomes.
Results: Positive LVI was significantly associated with advanced stage, high grade, necrosis, lymph node metastasis, and high-level SII. Positive LVI and high-level SII co-existence was significantly associated with unfavorable OS, CSS, and PFS in Kaplan-Meier analyses (all p < 0.001) and was an independent indicator of OS, CSS, and PFS (HR [95% CI]: 3.918 [2.168– 7.078], 5.623 [2.679– 11.801], 3.377 [2.138– 5.334]), respectively) in multivariate analyses. Furthermore, adding LVI and SII to a model that included standard pathologic predictors exhibited a better ability to predict survival in ROC analysis.
Conclusion: The integration of SII and LVI was demonstrated to be a potential factor of poor outcomes in patients with localized UTUC. Notably, the combined use of LVI and SII can be a feasible and complementary factor to TNM staging in the prognostic assessment of UTUC patients in clinical practice. The validity of combination of the two markers would be considered in future prospective studies to evaluate its usefulness in staging and application of post-operative chemo or immunotherapy.
Keywords: upper tract urothelial carcinoma, lymphovascular invasion, systemic immune-inflammation index, survival
Introduction
Upper tract urothelial carcinoma (UTUC) is a rare cancer worldwide, accounting for approximately 5–10% of all urothelial carcinomas in the urinary system.1 However, a high incidence of UTUC has been observed in Taiwan, especially in the south-west area.2 Nowadays, radical nephroureterectomy (RNU) with bladder cuff excision has been the standard treatment for high-risk localized UTUC, particularly multifocal tumors, large tumor size (> 2cm), high tumor grade, or advanced clinical stage at the time of diagnosis, whereas kidney-sparing surgery has been adopted as an alternative treatment for low-risk UTUC.3,4 After RNU for high-risk UTUC, further management includes either adjuvant chemotherapy or salvage radiotherapy, depending on the stage, grade, and other pathological findings. Nevertheless, this stratification remains insufficient to identify patients with a high risk for disease progression due to the diverse biological nature of tumors, despite being considered the same pathological stage. Therefore, it is of clinical importance to recognize potential prognostic factors to provide better risk stratification for future treatment plans.
The literature from Morgan Roupret et al listed significant predictors for adverse prognoses in UTUC, including tumor grade, tumor stage, lymph node metastasis, lymphovascular invasion (LVI), concurrent carcinoma in situ (CIS), and so on.3 Among these, LVI has been believed to have an increased risk of lymph node involvement and distant metastasis, thus leading to worse prognoses.5–9 Undoubtedly, LVI can be considered a relatively reliable prognostic factor in UTUC; however, part of UTUCs with LVI was clinically found not to have inferior outcomes. So, there remained limitations in the use of LVI alone to distinguish between patients at a high and low risk of disease progression. Furthermore, increasing data showed that tumor-related inflammation has been recognized as playing a crucial role in tumor growth/development, progression, and metastasis.10–12
The systemic immune-inflammation index (SII) was associated with oncologic outcomes.13–16 However, no study has examined the relationship between LVI and SII, and their prognostic value in determining disease progression and survival among UTUC patients after RNU. Therefore, the purpose of the present study was to evaluate the prognostic significance of integrating the LVI and SII in patients with UTUC after RNU.
Patients and Methods
Study Population
After approval from the ethical committee of the National Cheng-Kung University Hospital (NCKUH) (IRB number: A-ER-109-131), our study reviewed the records of patients with localized UTUC undergoing laparoscopic RNU from 2008 to 2019, which waived the requirement for informed consent from participants and allowed access to the follow-up clinical records. The data of medical records was anonymized and maintained with confidentiality. It was conducted based on the Declaration of Helsinki. RNU was performed according to standard procedures, and regional lymphadenectomy was generally performed if the preoperative imaging studies indicated that enlarged/palpable nodes were identified in the intraoperative examination. The exclusion criteria were as follows: use of neoadjuvant chemotherapies or immunosuppressant agents, radical cystectomy for bladder cancer, distant metastasis before surgery, incomplete blood data, active infection with fever episode (>38.3C), other malignancy, and the presence of chronic inflammatory, hematological, or autoimmune diseases. In addition, adverse histological variants, including micropapillary and sarcomatoid types were omitted as well. Ultimately, 554 patients were enrolled in our study. For each patient, the following clinical and pathologic features were analyzed: gender, age at surgery, comorbidities (diabetes mellitus, hypertension, hemodialysis), symptoms (hematuria or hydronephrosis), previous/concomitant bladder cancer, tumor location (renal pelvis, ureter, both), tumor stage, lymph node (LN) involvement, tumor necrosis, tumor grade, LVI, AC, and SII (neutrophil*platelet/lymphocyte). Tumor staging was determined according to the American Joint Committee on Cancer TNM Classification, 7th edition, and pathological grades were determined according to the 2007 WHO classification. AC was defined as the administration of more than two cycles of the platinum-based regimen (gemcitabine plus cisplatin/carboplatin) within 90 days post-surgery.
Use of Receiver Operating Characteristic (ROC) analysis determined the optimal cut-off value of SII as 580 in accordance with Jan et al study.13 Follow-up evaluations included regular interview, physical examination, urinalysis, urine cytology, abdominal ultrasonography, and abdominal computed tomography. Cystoscopy was performed every three months for the first two years, every six months for the next two years, and annually thereafter.
The survival outcomes in our study were overall (OS), cancer-specific (CSS), and progression-free survival (PFS). OS was defined as the interval from RNU until death; CSS was defined as the interval from RNU until death due to UTUC; PFS was defined as the duration from RNU until disease recurrence (included local recurrence/distant metastases, but did not include bladder or contralateral upper tract recurrence) or cancer-specific death. Moreover, bladder or contralateral upper urinary tract relapse was not defined as local recurrence in our study.
Statistical Analysis
The OS, CSS, and PFS were estimated by Kaplan–Meier analyses, and the Log rank test was applied to compare survival curves. Univariate/multivariate analyses were performed to evaluate the prognostic effects of clinical and pathological factors. Associations between the variables and the survival outcomes were presented as hazard ratios (HRs) with corresponding 95% confidence intervals (CIs). All p values were two-sided, and < 0.05 was considered significant. Furthermore, the area under the ROC curve (AUC) was used to calculate the predictive ability of the candidate marker. All analyses were performed using IBM SPSS 25.0 (SPSS Inc., Chicago, IL, USA) or MedCalc 19.7.2.
Results
Clinicopathogic Characteristics in Patients with UTUC Stratified by LVI
In Table 1, among the 554 patients treated with RNU for UTUC, 155 (28%) and 399 (72%) were positive and negative for LVI, respectively. At the time of surgery, the mean age (years) was 69.4 ± 10.8 and 69.2 ± 11.3 for positive and negative LVI patients, respectively. The mean follow-up duration (months) was 40.5 ± 32.1 and 49.2 ± 32.1, respectively, for positive and negative LVI patients. Significant correlations with positive LVI were found in tumor location involving renal pelvis and ureter, advanced pT stage, LN metastasis, high grade, necrosis, AC, and high-level SII. By contrast, no significant difference was noted for gender, age, renal function status, hemodialysis, diabetes mellitus/hypertension, hematuria/hydronephrosis, or previous/concomitant BC between two groups.
 |
Table 1 Correlations of Lymphovascular Invasion with Clinicopathologic Characteristics in Patients Treated with Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma |
Additionally, concerning the relationship between SII and LVI, UTUC with positive LVI had a significant association with higher SII values than those without positive LVI. The SII value increased with the advancing stages of UTUC progression (Supplementary S1).
Association of LVI and SII with Poor Outcomes
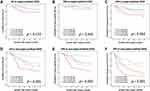
Kaplan-Meier analyses showed that positive LVI and high-level SII were both significantly associated with a worse OS, CSS, and PFS (all p < 0.05) (Supplementary S2 and S3). We further integrated LVI and SII to examine their influence on survival outcomes. After patients were stratified by LVI and SII, Kaplan-Meier plot revealed that positive LVI combined with high-level SII was significantly associated with a worse OS, CSS, and PFS (all p < 0.001) (Figure 1).
Considering the existence of different molecular or pathophysiologic features in patients with UTUC based on tumor stage, we attempted to analyze the effect of the combination of LVI and SII on survival between different pT stages. No obvious differences were observed in OS, CSS, and PFS in the presence of positive LVI and high-level SII in organ-confined diseases (Figure 2A–C). Nevertheless, in non-organ-confined diseases, the concurrence of positive LVI and high-level SII markedly exerted an adverse effect on OS, CSS, and PFS (all p < 0.05) (Figure 2D–F).
Integrating LVI and SII as a Useful Marker of Predicting Survival
In a Cox proportional hazards regression model (Table 2), multivariate analyses showed that other than tumor location involving both pelvis and ureter, advanced pT stage, and LN metastasis, the concurrence of positive LVI and high-level SII was significantly associated with poorer OS, CSS, and PFS than either or one risk factor alone, which indicated to be an independent prognosticator.
Further ROC analyses evaluated the predictive ability of integrated LVI and SII for OS, CSS, and PFS in UTUC in comparison with that of the basal model (constituted by relevant prognostic factors: pT stage, LN involvement, and tumor grade). Adding LVI and SII to the basal model resulted in the AUCs of 0.753, 0.826, and 0.779, respectively, in predicting OS, CSS, and PFS (all p < 0.001). Incorporating LVI and SII into the basal model was demonstrated to be superior to the basal model for predictive accuracy of survival (all p < 0.05) (Figure 3).
Discussion
Both LVI and SII have been shown as prognosticators in several types of cancer. However, the prognostic role of the combination of LVI and SII in UTUC has not been investigated before. In this study, the addition of SII enhanced the prognostic value of LVI in UTUC patients treated with RNU. Regarding the relationship between LVI and SII, the SII value positively correlated with the presence of LVI in a stage-dependent manner. Concurrence of positive LVI and high-level SII was a significant indicator of poorer OS, CSS, and PFS in UTUC after RNU, particularly in non-organ-confined disease. Furthermore, ROC analyses revealed that combining LVI and SII was a feasible and valuable auxiliary for risk stratification except for the TNM staging system.
To our knowledge, LVI appeared during the early metastatic process when tumor cells invaded vascular/lymphatic channels, which presented the active and dynamic status of cancer.17,18 Bolenz et al found that LVI may enhance the risk of tumor cell spreading due to increased peritumoral lymphatic vessel density and proliferating lymphatic endothelial cells.19 Several studies have demonstrated that LVI in UTUC can serve as a predictive marker of disease recurrence and progression.20–23 Moreover, increasing evidence indicated that systemic immune inflammation can mutually modulate cancer invasion and metastasis.12,24,25 Previous studies have reported that circulating immune-cell concentrations, such as neutrophils, platelets, monocytes, and lymphocytes, played key roles in promoting tumor growth/development and extension.11,26,27 SII, composed of serum neutrophils, platelets, and lymphocytes, was believed to mirror certain systemic inflammatory responses to tumor aggressiveness.16 A high SII represented relatively high neutrophil and platelet counts, as well as low lymphocyte counts, which may indicate a strong pro-tumor inflammatory response and a weak anti-tumor immune status. Moreover, in the case of a higher SII, the increased number of circulating tumor cells was found in hepatocellular carcinoma and small cell lung cancer.14,15 A high SII state implied enhanced viability and invasiveness of tumor cells, thus resulting in worsening survival.
Upon considering LVI and SII to be analyzed together, we observed that the presence of LVI significantly had higher SII values compared to the absence of LVI and positively correlated with high-level SII. The simultaneous presence of positive LVI and high-level SII indicated a worse prognosis than positive LVI or high-level SII alone, particularly in locally advanced diseases. Positive LVI or high-level SII alone significantly had a poorer outcome than none of positive LVI and high-level SII. More interesting, positive LVI devoid of high-level SII did not have inferior oncologic outcomes compared with negative LVI with high-level SII. Importantly, LVI positivity having high-level SII significantly exhibited a worse OS, CSS, and PFS than that lack of high-level SII. Furthermore, our study confirmed that high-level SII and positive LVI was an independent factor for predicting a poorer OS, CSS, and PFS in patients with UTUC after RNU in multivariate analysis. Herein, our results demonstrated that SII increased the clinical significance of LVI in predicting prognosis in patients with UTUC after RNU. These results may be explained by the fact that significant immune-inflammation which was implied by high-level SII may enhance or alter UTUC tumors’ malignant behaviors during LVI. So, we supposed that when LVI has occurred, inflammatory immune cells participating in the tumor microenvironment played a role in promoting tumor cells’ invasiveness/dissemination and viability. As such, combining these two factors led to an unfavorable outcome. However, the crosstalk between inflammatory immune cells and the aggressive behavior of cancer cells during LVI remains ill-defined in UTUC and requires further investigation.
Recently, large-scale studies have examined the prognostic significance of LVI and peripheral systemic inflammation-based index in non-metastatic UTUC.22,28 However, Colla Ruvolo et al recently showed that localized UTUC from Asian patients apparently had a worse outcome than that from non-Asian populations after statistical adjustment of tumor stage, grade, and LN invasion.29 The differing outcomes of UTUC between Asian and other races/ethnicities potentially results from discrepancies in the biological nature of the tumors. Moreover, LVI has been discovered as a poor prognostic factor for patients with UTUC after RNU, but the identified impact of LVI on prognosis was not significant in some studies. The development of a variety of new, feasible risk-stratifying methods/markers for predicting prognosis is urgently needed. Therefore, there is still room for discussion regarding the effect of LVI in combination with pre-treatment systemic immune-inflammation markers on survival in Asian patients with UTUC.
Notably, the advantage of our study was that it established a useful risk-stratification marker and provided new insights into the relationship between LVI and SII, which revealed an association between the pathological characteristics of the tumor and systemic immune-inflammation status. Furthermore, the information about SII and LVI was low-cost and easily available in clinical practice. Integrating SII and LVI was important to efficiently identify high-risk UTUC patients with unfavorable outcomes who may benefit from adjuvant chemotherapy or immunotherapy after RNU. Nevertheless, the detail of the biological mechanisms regarding LVI and SII remain uncertain in UTUC. In the future, it is essential to clarify an association between LVI and tumor immune cell infiltration in the tumor microenvironment, as well as to determine how inflammatory immune cells populating the tumor microenvironment promote cancer cell aggressiveness during LVI, such as proliferation, migration, and invasion. Meanwhile, it is also important to explore more specific molecular markers from tissue samples, serum, or urine, subsequently facilitating efficient and prompt clinical decision-making for precision medicine treatment in high-risk UTUCs.
Our study had several limitations. First, this retrospective study was performed in a single medical center in Taiwan, which may cause a selection bias. Prospective designed studies and more patients from other countries are necessary for the external validation of our findings. Second, patients who did not undergo RNU were excluded. This might have led to underestimation of the effectiveness of pure chemotherapy in locally advanced UTUC. Third, the underlying biological mechanisms to explain associated findings were not available, which might have reduced the strength of our conclusions. In addition, our study lacked some relevant molecular markers associated with more precise and targeted treatment, such as PD-1/PD-L1, PI3K, cyclin D, Ki-67, and FGFR 2/3 mutations.
Conclusion
The integration of LVI and SII as a new promising combination marker has an important clinical application value in predicting the prognosis of UTUC after RNU, except for the conventional TNM stage. Therefore, the clinical use of LVI and SII will help optimize the risk stratification of patients for individualized treatment planning. Due to this retrospective study, however, future prospective investigation and external validation are warranted.
Acknowledgments
We are grateful to Dr. Sheng-Hsiang Lin and Ms. Wan-Ni Chen for providing the statistical consulting services from the Biostatistics Consulting Center, Clinical Medicine Research Center, National Cheng Kung University Hospital.
Author Contributions
All authors made significant contributions to one or more aspects of the conception, study design, execution, acquisition, analysis, and interpretation of the data of this work. All authors participated in drafting, revising, or critically reviewing the manuscript; gave approval of the final version to be published; consented to the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This study was supported by National Science and Technology Council (111-2314-B-006-065-).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA. 2019;69(1):7–34. doi:10.3322/caac.21551
2. Shen CH, Chiou HY, Tung MC, et al. Clinical and demographic characteristics among patients with urothelial carcinomas of the upper urinary tract and bladder in Taiwan. J Chin Med Assoc. 2017;80(9):563–568. doi:10.1016/j.jcma.2017.03.008
3. Roupret M, Babjuk M, Burger M, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol. 2021;79(1):62–79. doi:10.1016/j.eururo.2020.05.042
4. National Comprehensive Cancer Network. Bladder cancer; 2022. Available from: https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf.
5. Novara G, Matsumoto K, Kassouf W, et al. Prognostic role of lymphovascular invasion in patients with urothelial carcinoma of the upper urinary tract: an international validation study. Eur Urol. 2010;57(6):1064–1071. doi:10.1016/j.eururo.2009.12.029
6. Kikuchi E, Margulis V, Karakiewicz PI, et al. Lymphovascular invasion predicts clinical outcomes in patients with node-negative upper tract urothelial carcinoma. J Clin Oncol. 2009;27(4):612–618. doi:10.1200/JCO.2008.17.2361
7. Sung SY, Kwak YK, Lee SW, et al. Lymphovascular invasion increases the risk of nodal and distant recurrence in node-negative stage I-IIA non-small-cell lung cancer. Oncology. 2018;95(3):156–162. doi:10.1159/000488859
8. Rakha EA, Martin S, Lee AH, et al. The prognostic significance of lymphovascular invasion in invasive breast carcinoma. Cancer. 2012;118(15):3670–3680. doi:10.1002/cncr.26711
9. Kang YJ, Kim HS, Jang WS, et al. Impact of lymphovascular invasion on lymph node metastasis for patients undergoing radical prostatectomy with negative resection margin. BMC Cancer. 2017;17(1):321. doi:10.1186/s12885-017-3307-4
10. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi:10.1016/j.cell.2011.02.013
11. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–e503. doi:10.1016/S1470-2045(14)70263-3
12. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi:10.1038/nature07205
13. Jan HC, Yang WH, Ou CH. Combination of the preoperative systemic immune-inflammation index and monocyte-lymphocyte ratio as a novel prognostic factor in patients with upper-tract urothelial carcinoma. Ann Surg Oncol. 2019;26(2):669–684. doi:10.1245/s10434-018-6942-3
14. Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. doi:10.1158/1078-0432.CCR-14-0442
15. Zheng L, Zou K, Yang C, Chen F, Guo T, Xiong B. Inflammation-based indexes and clinicopathologic features are strong predictive values of preoperative circulating tumor cell detection in gastric cancer patients. Clin Transl Oncol. 2017;19(9):1125–1132. doi:10.1007/s12094-017-1649-7
16. Yang R, Chang Q, Meng X, Gao N, Wang W. Prognostic value of Systemic immune-inflammation index in cancer: a meta-analysis. J Cancer. 2018;9(18):3295–3302. doi:10.7150/jca.25691
17. Barresi V, Reggiani Bonetti L, Vitarelli E, Di Gregorio C, Ponz de Leon M, Barresi G. Immunohistochemical assessment of lymphovascular invasion in stage I colorectal carcinoma: prognostic relevance and correlation with nodal micrometastases. Am J Surg Pathol. 2012;36(1):66–72. doi:10.1097/PAS.0b013e31822d3008
18. Aleskandarany MA, Sonbul SN, Mukherjee A, Rakha EA. Molecular mechanisms underlying lymphovascular invasion in invasive breast cancer. Pathobiology. 2015;82(3–4):113–123. doi:10.1159/000433583
19. Bolenz C, Fernandez MI, Trojan L, et al. Lymphangiogenesis occurs in upper tract urothelial carcinoma and correlates with lymphatic tumour dissemination and poor prognosis. BJU Int. 2009;103(8):1040–1046. doi:10.1111/j.1464-410X.2008.08135.x
20. Liu W, Sun L, Guan F, Wang F, Zhang G. Prognostic value of lymphovascular invasion in upper urinary tract urothelial carcinoma after radical nephroureterectomy: a systematic review and meta-analysis. Dis Markers. 2019;2019:7386140. doi:10.1155/2019/7386140
21. Ku JH, Byun SS, Jeong H, Kwak C, Kim HH, Lee SE. Lymphovascular invasion as a prognostic factor in the upper urinary tract urothelial carcinoma: a systematic review and meta-analysis. Eur J Cancer. 2013;49(12):2665–2680. doi:10.1016/j.ejca.2013.04.016
22. Zhang L, Wu B, Zha Z, Zhao H, Yuan J, Feng Y. The prognostic value of lymphovascular invasion in patients with upper tract urinary carcinoma after surgery: an updated systematic review and meta-analysis. Front Oncol. 2020;10:487. doi:10.3389/fonc.2020.00487
23. Godfrey MS, Badalato GM, Hruby GW, Razmjoo M, McKiernan JM. Prognostic indicators for upper tract urothelial carcinoma after radical nephroureterectomy: the impact of lymphovascular invasion. BJU Int. 2012;110(6):798–803. doi:10.1111/j.1464-410X.2011.10893.x
24. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
25. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi:10.1016/j.cell.2010.01.025
26. Lambert AW, Pattabiraman DR, Weinberg RA. Emerging biological principles of metastasis. Cell. 2017;168(4):670–691. doi:10.1016/j.cell.2016.11.037
27. Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6(4):283–287. doi:10.1023/B:AGEN.0000029415.62384.ba
28. Mori K, Resch I, Miura N, et al. Prognostic role of the systemic immune-inflammation index in upper tract urothelial carcinoma treated with radical nephroureterectomy: results from a large multicenter international collaboration. Cancer Immunol Immunother. 2021;70(9):2641–2650. doi:10.1007/s00262-021-02884-w
29. Colla Ruvolo C, Wenzel M, Nocera L, et al. The effect of race on stage at presentation and survival in upper tract urothelial carcinoma. Urol Oncol. 2021;39(11):788 e7–e13. doi:10.1016/j.urolonc.2021.07.001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.