Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Relationship Between On-Site Clinical Practice, Nursing Professional Value, and Nursing Clinical Self-Efficacy During COVID-19: A Cross-Sectional Study
Authors Lee J , Choi J , Kim J, Lee K
Received 5 October 2023
Accepted for publication 18 December 2023
Published 21 December 2023 Volume 2023:16 Pages 4163—4172
DOI https://doi.org/10.2147/JMDH.S443247
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jeongmin Lee, Junho Choi, Juyoung Kim, Kayoung Lee
College of Nursing, Gachon University, Incheon, South Korea
Correspondence: Kayoung Lee, College of Nursing, Gachon University, Health Science Building, Room# 412, 191 Hambakmoero, Yeonsu-gu, Incheon, 21936, South Korea, Tel: +82-32-820-4227, Email [email protected]
Background: During COVID-19, nursing students experienced variations in on-site clinical practice, such as a combination of on-site and non-face-to-face clinical practice. Although on-site clinical practice is critical for increasing nurses’ clinical self-efficacy and developing professional nursing values, there is a lack of knowledge that reflects the current clinical practice environment.
Aim: To examine the relationship between on-site clinical practice, nursing professional values, and nursing clinical self-efficacy during the COVID-19 pandemic.
Methods: This study is a cross-sectional correlational study design. Demographic characteristics, on-site clinical practice, nursing professional values, and nursing clinical self-efficacy were assessed using an online survey from October 3, 2022, to November 6, 2022. Data were analyzed using descriptive statistics, ANOVA, t-test, Pearson’s correlation coefficient, and multiple regression.
Results: Of the 86 participants, 18 (20.9%) were male and 68 (79.1%) were female. The duration of the participants’ average participation in on-site clinical practice was 39.67 days (61.04%). Nursing professional values significantly influenced clinical self-efficacy (β=0.379, p< 0.001). However, on-site clinical practice was not significantly related to clinical self-efficacy (β=0.051, p=0.611). In terms of nursing clinical self-efficacy, measuring blood glucose had the highest score. On the other hand, establishing and maintaining intravenous catheters had the lowest scores.
Conclusion: Nursing students’ professional values were significantly associated with nursing clinical self-efficacy; however, the extent of involvement in on-site clinical practice during the pandemic did not have a significant impact on nursing clinical self-efficacy. Given that this study focused on a single university, it is imperative to replicate this research using diverse samples in the future. In addition, there is a need to establish a range of teaching and learning approaches for clinical practice, including simulation, online learning, and the use of state-of-the-art technology for faculty-student feedback strategies, in anticipation of the need for alternative practices.
Keywords: clinical practice, COVID-19, self-efficacy, professionalism, nursing education, nursing students
A Letter to the Editor has been published for this article.
Introduction
In response to COVID-19 in 2020, the Korean Ministry of Education1 recommended limiting face-to-face education and implementing distance education. Moreover, the Korea Accreditation Board of Nursing Education2 established regulations for non-face-to-face clinical practice, in which the 1000 hours of on-site clinical practice in hospital settings was replaced with alternative clinical practices, such as watching nursing skills videos or using web-based simulation platforms, during the pandemic. Consequently, nursing schools in Korea quickly transitioned from face-to-face education to online courses, including clinical practice, to comply with the COVID-19 prevention regulations.2 Similarly, nursing students worldwide experienced changes in their clinical practice.3
During COVID-19, hospitals adjusted their clinical practice protocols. For instance, the length of on-site clinical placement was reduced,4 and clinical practice schedules were changed several times. This led to variations in student participation in on-site clinical practice.5,6 Alternative clinical practices have been implemented to compensate for the missed on-site clinical practice hours, especially when the on-site practice was not feasible (eg, national/natural disasters).7
Various alternative clinical practices have been implemented to maintain nursing education and ensure the continuous acquisition of clinical skills by students. One such method is the use of online simulation practice platforms that allow students to practice with virtual patients.8–10 Online learning replaced skills labs and allowed students to acquire nursing skills, indirectly experience hospital environments, and learn about diseases/nursing procedures through video materials. Faculty used video conferencing to conduct classes, provide feedback, and monitor students’ progress throughout alternative practice courses.7,10
Clinical practice can provide nursing students with opportunities to develop self-efficacy.11 On-site clinical practice is critical for increasing nurses’ clinical self-efficacy and developing professional nursing values. The source of self-efficacy is gaining confidence by observing the experiences and behaviors of others, which means that nursing students can observe the performance of instructors and nurses and develop nursing self-efficacy.12,13 Non-face-to-face educational materials have recently been developed, and nursing students have more opportunities for clinical experiences. However, students experiencing clinical practice through online learning have often expressed dissatisfaction with their clinical competence and anxiety about becoming a nurse.14,15
Along with self-efficacy, professional nursing values are considered fundamental components of nursing that influence professional competence.16 In nursing, professional values include human dignity, integrity, altruism, and justice, and serve as the basis for standards, practice, and evaluation.17 These are important values for nursing students to acquire. Previous studies have reported a significant relationship between self-efficacy and professional nursing values among nurses and nursing students.16,18–21 In addition, studies investigating the significant relationship between clinical practice and nursing professional values and/or self-efficacy were conducted prior to COVID-19.22–25
In response to the changing clinical environment due to the COVID-19 pandemic, blended on-off clinical education has been introduced. Recently, qualitative studies have revealed students’ experiences regarding this change. Yip et al26 found that male students had negative perspectives on limited clinical placements in women’s ward practice due to cultural context and gender bias, which differed from the clinical experiences of medical students without restrictions. Ha27 found that students have a mixed view of online-based clinical education, either negative or positive, when they are unable to go to the hospital due to the COVID-19 pandemic. Barison et al28 found that students felt the value of the profession through direct participation in COVID-19 ward practice, even during the COVID-19 pandemic. However, there is a lack of quantitative research on students’ self-efficacy according to the degree of clinical participation in hospitals and professional nursing values in the COVID-19 situation.
Therefore, the primary aim of this study was to examine the relationship between on-site clinical practice, nursing professional values, and nursing clinical self-efficacy during the COVID-19 pandemic. The secondary aim was to describe specific nursing skills in which nursing students lack confidence or have difficulty by measuring their clinical self-efficacy.
Materials and Methods
Design
This study used a descriptive cross-sectional correlational design using an online survey.
Participants and Data Collection
The study population was nursing students in Korea who participated in clinical practice between 2020 and 2022. The following inclusion criteria were considered to attain homogeneity of nursing students: (a) having been enrolled in the fourth year of the nursing program and (b) having completed three semesters (the junior first and second semesters and the senior first semester) consisting of clinical practice and theory courses between 2020 and 2022. Nursing students who did not experience clinical practice during the COVID-19 pandemic were excluded.
The sample size was calculated with the G*Power 3.1.9.7 program to ensure a statistical power of at least 80% to find out the multivariate association of nursing clinical efficacy with the degrees of on-site clinical practice and nursing professional values. At the significant level of 0.05 with a medium effect size of 0.15, the minimum sample size was 86 considering a 10% attrition rate based on two independent variables and one covariate. A convenience sampling method was used to select study participants from the XXX University in Incheon, South Korea. Data were collected from October 3, 2022 to November 6, 2022, using an online survey. The survey took approximately 20 minutes to complete. A total of 86 participants completed the survey questionnaires.
Instruments
Nursing Clinical Self-Efficacy
To measure self-efficacy, we used the Nursing Clinical Self-Efficacy Scale, which was modified by Ahn29 based on Harvey and McMurray’s Nursing Clinical Self-Efficacy Scale (NCSE) instrument13 and Parker’s Self-Efficacy Measurement Instrument.30 It consists of 25 questions; each question consists of a Likert scale ranging from “I do not think I could do it” (10 points) to “I am very sure I could do it” (100 points). The higher the score, the higher the participant’s clinical self-efficacy. In the study by Ahn,29 Cronbach’s alpha was 0.94. In this study, Cronbach’s alpha was 0.95.
Proportion of On-Site Clinical Practice
To measure the proportion of on-site clinical practice, we calculated the proportion of the number of days (only including those conducted at a hospital) to the total number of clinical practice days in the curriculum. This study included seven clinical practice subjects: medical-surgical nursing practice I, II, and III, maternity nursing practice I and II, and pediatric nursing practice I and II.
Nursing Professional Values
To measure nursing professional values, this study used the Korean version of the Nursing Professional Value Scale.31 The Nursing Professional Values Scale (NPVS) was originally developed by Weis and Schank32 based on the American Nurses Association (ANA) Code of Ethics for Nurses with interpretive statements.33 Since the NPVS was created for American nurses, it has limitations for use in other countries. Therefore, this study used the Korean version of the Nursing Professional Value Scale developed by Yeun et al31 to reflect the reality in Korea. It consists of 29 items: self-concept of the profession (nine items), social awareness (eight items), professionalism of nursing (five items), role of nursing service (four items), and originality of nursing (three items). Each item was rated on a 5-point Likert scale ranging from “strongly disagree” (1 point) to “strongly agree” (5 points). Higher scores indicate a higher level of nursing professional values. In the study by Yeun et al,31 Cronbach’s alpha was 0.92. In this study, Cronbach’s alpha was 0.95.
Demographic Characteristics
The demographic characteristics of the final-year nursing students were collected using four items (sex, age, religion, and GPA). Because a specific GPA may be considered sensitive information, it was collected in three categories (below 3.5, 3.5 or above, less than 4, and 4 or above).
Data Analysis
Descriptive statistics were used to analyze on-site clinical practice, nursing professional values, and nursing clinical self-efficacy. ANOVA and t-tests were used to analyze nursing clinical self-efficacy and professional values according to on-site clinical practice. Pearson’s correlation coefficient was used to analyze the relationship between on-site clinical practice, nursing professional values, and nursing clinical self-efficacy. Multiple regression was used to determine how the proportion of on-site clinical practice and nursing professional values independently influenced nursing clinical self-efficacy while controlling for GPA. Statistical Package for the Social Sciences, version. 29.0 (IBM SPSS Statistics) was used for statistical analysis.
Ethics Considerations
This study was approved by the Institutional Review Board of the university to which the researchers belong (approval no. 1044396–202209-HR-187-01). It was conducted only with those who voluntarily expressed their willingness to participate, and data collection was carried out anonymously. The explanation of this study included the purpose and method of the research. It was noted that there would be no disadvantage in participating in the research, refusing to participate, or dropping out and that personal information and confidentiality would be guaranteed.
Results
A total of 86 participants completed the survey. Eligibility for participation in the study was determined by the semester of completion and the year in which the questionnaire was completed.
Of the 86 participants, 18 (20.9%) were male, and 68 (79.1%) were female. The mean age was 22.98±1.20 years, and 22 years was the most common, with 32 people (37.2%). In terms of GPA, 37 students (43.0%) scored more than 3.5 to less than 4, and 62 people (72.1%) were non-religious.
The participation period of the participants’ on-site clinical practice was a total of 65 days, with an average of 39.67±11.34 days (61.04%). Medical-surgical nursing practice had an average of 23.47 days (78.22%), pediatric nursing practice had an average of 8.65 days (57.67%), and maternity nursing practice had an average of 7.56 days (37.79%) (Table 1).
 |
Table 1 Status of Proportion of On-Site Clinical Practice During Covid-19 Pandemic (2020–2022) |
The nursing professional values average was 3.69 points. The highest score was 3.98 for the “role of the nursing”. It was followed by 3.95 points for “professionalism of nursing”, 3.84 for “self-concept of the profession”, 3.37 for “originality of nursing”, and 3.35 for “social awareness” (Table 2).
 |
Table 2 Total Score and Sub-Item Scores of “Nursing Professional Values” (N=86) |
The average nursing clinical self-efficacy score was 71.43 points. Examining each item, the highest score was “measuring blood sugar” with 93.60 points, followed by “fall prevention” (86.51), “forming a positive working relationship with other nursing staff” (85.35), and “forming a positive working relationship with the senior nurse” (82.67). On the other hand, “establishing and maintaining intravenous catheters and performing intravenous infusion” had the lowest score of 45.93 points, followed by “establishing urinary catheter” (49.53), “giving a client enema or suppositories” (51.86), and “applying tracheal suction” (54.53) (Table 3). The demographic characteristics were not statistically significant regarding nursing clinical self-efficacy (Table 4).
 |
Table 3 Total Score and Sub-Item Scores of ‘Nursing Clinical Self-Efficacy (N=86) |
 |
Table 4 Differences in “Nursing Clinical Self-Efficacy” According to Demographic Characteristics |
Relationship Between On-Site Clinical Practice, Nursing Professional Values, and Nursing Clinical Self-Efficacy
There was a positive correlation between clinical self-efficacy and nursing professional values (r=0.383, p<0.001), while GPA was negatively correlated (r=−0.232, p=0.031). There was no significant correlation between nursing clinical self-efficacy and on-site clinical practice.
Factors Affecting Nursing Clinical Self-Efficacy
Before performing multiple regression, the variance inflation factor (VIF) ranged from 1.012 to 1.027, tolerance ranged from 0.974 to 0.988, and multicollinearity between the independent variables was not problematic. The results of the multiple regression showed that nursing professional values (β=0.379, p<0.001) had a significant influence on nursing clinical self-efficacy. (Table 5).
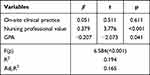 |
Table 5 The Association of on-Site Clinical Practice and Nursing Professional Value on Nursing Clinical Self-Efficacy |
Discussion
This study investigated the proportion of on-site clinical practice among nursing students during the COVID-19 pandemic and examined the relationship between on-site clinical practice, nursing professional values, and nursing clinical self-efficacy. Before the COVID-19 pandemic, the proportion of on-site clinical practice was 100% in acute care hospitals or community settings. During the COVID-19 pandemic, many hospitals reduced the number of wards available for students to practice on, resulting in the need for alternative practicums. The study hypothesized that the proportion of on-site clinical practice would affect clinical nursing self-efficacy. The study found that the average proportion of on-site clinical practice among nursing students was 61.04%; however, the proportion of on-site clinical practice did not have a significant effect on nursing clinical self-efficacy. This may be the reason for the relatively high proportion of on-site clinical practice in this study sample compared to other programs. Other studies showed that the proportion of on-site clinical practice was 57.52% in 2020,34 and most students had less than 40% of on-site clinical practice in 2021.35 The proportion of on-site clinical practice in this study was higher than in other studies because the university student participants had a tertiary general hospital as a partner hospital, which allowed easy access to on-site clinical practice. This study revealed that the proportion of medical-surgical nursing practice was the highest (78.22%). In contrast, the proportions of pediatric and maternity nursing were relatively low because patients in these units were vulnerable to COVID-19 complications,36 making it difficult to access them as subjects and secure practice sites.7,37,38
In terms of nursing professional values, “originality of nursing” and “social awareness” had low mean scores. The results were consistent with other studies using the same measure.39–44 Although the COVID-19 pandemic has shaped nurses’ professional contributions and positive images to the public image,45 the reason for the low score for “social awareness” in this study could be the nurses’ responses that their role is still underestimated by the public.46 This could be due to media reports about nurses that focus on dedication rather than professional skills,45,47 and stereotypes about nurses such as “female” and “assistant role” still exist.48–50 This is similar to the results in which the evaluation of the image of a nurse perceived by nursing students was low in their role and high in their identity, such as “devotion” and “angel”.39,43 For nursing students to clearly understand their identity, it is important to clarify their role as autonomous healthcare providers.
In this study, nursing professional values had a significant influence on nursing clinical self-efficacy. Nursing professional values were directly related to a nurse’s self-efficacy because they determined the nurses’ motivation and aspirations,18 and previous studies reported that nursing professional values and self-efficacy had a positive correlation.16,18–21 Previous Korean studies that investigated the relationship between self-efficacy and nursing professional values mainly used general or social self-efficacy measures, which did not fully reflect the characteristics of nursing students.19–21 However, this study was significant in that it measured the clinical self-efficacy of nursing students and explored the nursing skills they found difficult.
This study did not find a significant relationship between on-site clinical practice and nursing clinical self-efficacy or professional values. Similar to the results of this study, previous studies have found no significant differences when comparing simulation substitution for a portion of clinical practice across multiple domains, including nursing knowledge;51 student engagement, educational outcomes, and student competence;52 and the nursing process, nursing skills, interpersonal communication, and professionalism.53 These findings suggested that alternative clinical practice might be as effective as on-site practice in developing nursing professional values and clinical self-efficacy.
To improve nursing students’ clinical performance and achieve positive clinical practice outcomes, it is necessary to increase clinical self-efficacy and create an educational environment that enhances it.54 Therefore, we analyzed the factors that influenced nursing clinical self-efficacy. The factors that influenced nursing students’ clinical self-efficacy were nursing professional values (β=0.379, p<0.001). The nursing clinical self-efficacy with the highest score in this study was “measuring blood sugar”, while invasive nursing skills, such as intravenous injection (IV), urinary catheterization, enema, and tracheal suction had relatively lower scores. During their clinical practice in a clinical environment, 86.3% of Korean nursing students had experience in performing blood sugar tests on actual clients, while the experience in performing enemas, tracheal suction, and urinary catheterization was less than 10%, and IV was 54.5%.55 In addition, IV was a nursing skill that nursing students and hospital nurses find difficult.56 Alavi57 suggested that providing opportunities to practice clinical skills in the skill lab, receiving feedback, and a wide range of clinical experiences were necessary to improve nursing students’ self-efficacy. To improve clinical self-efficacy, it is important to help nursing students master nursing skills through repeated educational opportunities in hospital-like settings.
The following limitations must be considered when interpreting the results of this study. First, the sample was selected from one university; therefore, the generalizability of the results to all nursing students may be limited. Further studies are needed to diversify and increase the sample size. Second, during the COVID-19 pandemic, the criteria for academic evaluation were changed to ensure fairness in grades.58,59 However, the difference in grading standards between re-admitted and current students was not accounted for in the analysis of GPA. Third, in this study, the proportion of clinical practice and nursing professional values were selected as variables to explain the clinical self-efficacy during COVID-19, but other variables that affect clinical self-efficacy, such as communication skills,60 gender differences,61 and the degree of repetition of online-based learning,62 should be analyzed using a larger sample. Despite its limitations, this study examined the impact of clinical practice as modified by COVID-19 by considering the proportion of participation in on-site clinical practice. In addition, by measuring nursing clinical self-efficacy, the specific nursing skills in which nursing students lack confidence and where they need improvement in clinical practice were revealed. However, this study adopted a cross-sectional design, and future studies need to compare students before and after the pandemic or analyze the clinical adaptability of students who experienced the pandemic after graduation.
As a result of the lack of on-site clinical sites due to the COVID-19 pandemic, the need for alternative practices that could increase the effectiveness of on-site practice increased, and several attempts were made to replace the existing on-site practice in nursing education. In this study, the extent of involvement in on-site clinical practice did not have a significant effect on nursing clinical self-efficacy. This means that alternative clinical practice may also increase clinical effectiveness as much as on-site clinical practice if effective online or simulation-based educational methods that can enhance nursing skills are developed and used. Regarding the improvement of nursing skills for students, it is necessary to develop and test non-face-to-face but hands-on learning in education, such as digital technologies or virtual reality in clinical practice. Moreover, this study found that nursing professional value was important for increasing nursing clinical self-efficacy. Accordingly, future research is needed to qualitatively investigate the students’ experience of clinical self-efficacy and nursing professional values from the on-site clinical practice. At the same time, a variety of educational curricula should be developed to emphasize the nursing professional values of human dignity, altruism, and justice even when on-site clinical practice is not available.
Conclusion
This study assessed nursing students’ clinical self-efficacy during the pandemic and found a significant positive association between nursing professional values and clinical self-efficacy. In particular, nursing students’ low self-efficacy in invasive nursing skills, such as IV, urinary catheterization, enema, and tracheal suction, suggests the need for multimodal skill labs for nursing skills that nursing students have not frequently encountered in clinical practice. These findings provide the basis for developing strategies and interventions to optimize nursing education and promote effective clinical practice, particularly during pandemics. In addition, these findings underscore the importance of nursing educational institutions prioritizing the cultivation of nursing students’ sense of professional values, as this may contribute to the development of their self-efficacy.
Data Sharing Statement
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Interstitial Review Board of Gachon University (Approve No. 1044396-202209-HR-187-01). All participants gave their consent to participate in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2021R1C1C2011587). This work was supported by the Gachon University research fund of 2020 (GCU-202008420002).
Disclosure
The authors declare that they have no competing interests.
References
1. Ministry of Education [homepage on the internet]. South Korea: academic Operations and Support for Education in Response to COVID-19; 2022. Available from: https://www.moe.go.kr/boardCnts/view.do?boardID=294&boardSeq=79917&lev=0&m=02.
2. Korea Accreditation Board of Nursing Education [homepage on the internet]. South Korea: 2020 Second Half Nursing Education Accreditation Assessment Handbook for Universities; 2020. Available from: http://www.kabone.or.kr/m/notice/list/view.do?num=732.
3. Agu CF, Stewart J, McFarlane-Stewart N, Rae T. COVID-19 pandemic effects on nursing education: looking through the lens of a developing country. Int Nurs Rev. 2021;68(2):153–158. doi:10.1111/inr.12663
4. Susmarini D, Sumarwati M, Handayani F, Iskandar A. Nursing students’ clinical practice experience during the COVID-19 pandemic: a qualitative study. Open Access Maced J Med Sci. 2022;10(G):176–181. doi:10.3889/oamjms.2022.8116
5. Ulenaers D, Grosemans J, Schrooten W, Bergs J. Clinical placement experience of nursing students during the COVID-19 pandemic: a cross-sectional study. Nurse Educ Today. 2021;99:104746. doi:10.1016/j.nedt.2021.104746
6. Rohde G, Johannessen B, Maaseide M, et al. Baccalaureate nursing students’ experiences of how the COVID-19 pandemic influenced learning - a mixed method study. BMC Nurs. 2022;21(1):172. doi:10.1186/s12912-022-00955-6
7. Choi EJ. Strategies of pediatric nursing clinical practice in Ontact era. JKNR. 2020;4(4):29–40. doi:10.34089/jknr.2020.4.4.29
8. Sharoff L. Student’s perception of vSim for nursing® using the Simulation Effectiveness Tool-Modified. Clin Simul Nurs. 2022;68:1–8. doi:10.1016/j.ecns.2022.04.006
9. Kim MJ, Kang HS, De Gagne JC. Nursing students’ perceptions and experiences of using virtual simulation during the COVID-19 pandemic. Clin Simul Nurs. 2021;60:11–17. doi:10.1016/j.ecns.2021.06.010
10. Do ES. Factors affecting the clinical performance of nursing students participating in alternative clinical practicum. JKAIS. 2021;22(12):526–536. doi:10.5762/KAIS.2021.22.12.526
11. Abdal M, Masoudi Alavi N, Adib-Hajbaghery M. Clinical self-efficacy in senior nursing students: a mixed- methods study. Nurs Midwifery Stud. 2015;4(3):e29143. doi:10.17795/nmsjournal29143
12. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi:10.1037/0033-295X.84.2.191
13. Harvey V, McMurray N. Self-efficacy: a means of identifying problems in nursing education and career progress. Int J Nurs Stud. 1994;31(5):471–485. doi:10.1016/0020-7489(94)90017-5
14. Suliman WA, Abu-Moghli FA, Khalaf I, Zumot AF, Nabolsi M. Experiences of nursing students under the unprecedented abrupt online learning format forced by the national curfew due to COVID-19: a qualitative research study. Nurse Educ Today. 2021;100:104829. doi:10.1016/j.nedt.2021.104829
15. Lim SH. Content analysis on online non-face-to-face adult nursing practice experienced by graduating nursing students in the ontact era. JKAIS. 2021;22(4):195–205. doi:10.5762/KAIS.2021.22.4.195
16. Dellafiore F, Rosa D, Udugampolage NS, Villa G, Albanesi B. Professional values and nursing self-efficacy in the Italian context. Correlational descriptive study. Scand J Caring Sci. 2022;36(1):142–149. doi:10.1111/scs.12971
17. Schmidt BJ, McArthur EC. Professional nursing values: a concept analysis. Nurs Forum. 2018;53(1):69–75. doi:10.1111/nuf.12211
18. Cho EJ, Bang KS. Nursing Professionalism, Self-Efficacy and Nurse Parent Partnership in Pediatric Nurses. Child Health Nursing Re. 2013;19(2):94–101. doi:10.4094/chnr.2013.19.2.94
19. Ahn T, Song YA. Affecting factors of nursing professionalism perceived by nursing students. J East-West Nurs Res. 2015;21(1):10–17. doi:10.14370/jewnr.2015.21.1.10
20. Ham Y-S, Kim H-S, Cho I-S, Lim J-Y. Affecting factors of nursing professionalism perceived by senior nursing students. J Korean Acad Soc Nurs Educ. 2011;17(3):536–544. doi:10.5977/JKASNE.2011.17.3.536
21. Moon Y-S, Han S-J. Impact of self-efficacy and nursing professionalism on organizational commitment in nurses. J Korean Acad Soc Nurs Educ. 2011;17(1):72–79. doi:10.5977/JKASNE.2011.17.1.072
22. Kang D-H-S. Factors influencing nursing professionalism in male nursing students. Korean J Health Serv Manag. 2019;13(1):43–53. doi:10.12811/kshsm.2019.13.1.043
23. Kwon YE, Kim SY. Factors affecting satisfaction of clinical practice among prospective graduates in nursing colleges. J Korean Acad Soc Nurs Educ. 2018;24(1):80–88. doi:10.5977/jkasne.2018.24.1.80
24. Lim KM, Jo EJ. Influence of satisfaction with clinical practice and image of nurses on nursing professionalism of nursing students. JKAIS. 2016;17(4):556–566. doi:10.5762/KAIS.2016.17.4.556
25. Park HJ, Oh JW. The relationships of the clinical practice stress and the major satisfaction with the nursing professionalism of nursing college students. J Digital Convergence. 2014;12(12):417–426. doi:10.14400/JDC.2014.12.12.417
26. Yip YC, Yip KH, Tsui WK. Exploring the gender-related perceptions of male nursing students in clinical placement in the Asian context: a qualitative study. Nurs Rep. 2021;11(4):881–890. doi:10.3390/nursrep11040081
27. Ha EH. Alternative clinical practice experiences of Korean nursing students during the COVID-19 pandemic. Healthcare. 2023;11(17):2452. doi:10.3390/healthcare11172452
28. Barisone M, Ghirotto L, Busca E, et al. Nursing students’ clinical placement experiences during the COVID-19 pandemic: a phenomenological study. Nurse Educ Pract. 2022;59:103297. doi:10.1016/j.nepr.2022.10329729
29. Ahn EK. A Model for Clinical Nurses’ Self-Efficacy and Work Performance [Dissertation]. Daejeon: Chungnam National University; 2000.
30. Parker LE. When to fix it and when to leave: relationships among perceived control, self-efficacy, dissent, and exit. J Appl Psychol. 1993;78(6):949–959. doi:10.1037/0021-9010.78.6.949
31. Yeun EJ, Kwon YM, Ahn OH. Development of a Nursing Professional Value Scale. J Korean Acad Nurs. 2005;35(6):1091–1100. doi:10.4040/jkan.2005.35.6.1091
32. Weis D, Schank MJ. An instrument to measure professional nursing values. J Nurs Scholarsh. 2000;32(2):201–204. doi:10.1111/j.1547-5069.2000.00201.x
33. American Nursing Association. Code for Nurses with Interpretive Statements. ANA; 1985.
34. Song MK, Kim JS. Achieving nursing students’ clinical practice hours during the COVID-19 pandemic: effects of alternative and nonstandard practicum methods. Int J Nurs Pract. 2023;29(2):e13142. doi:10.1111/ijn.13142
35. Kang Y, Hwang H. The impact of changes in nursing practicum caused by COVID-19 pandemic on new graduate nurses. Nurse Educ Today. 2023;121:105675. doi:10.1016/j.nedt.2022.105675
36. Jafari M, Pormohammad A, Sheikh Neshin SA, et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: a systematic review and meta-analysis. Rev Med Virol. 2021;31(5):1–16. doi:10.1002/rmv.2208
37. Chin EY, Lee MI. Effects of e-learning contents in delivery room nursing for nursing students. KALCI. 2021;21(2):353–370. doi:10.22251/jlcci.2021.21.2.353
38. Kim JI, Kang HS, Mi PS, Ahn SH. Current status of women’s health nursing practicum and direction. Korean J Women Health Nurs. 2014;20(2):173–183. doi:10.4069/kjwhn.2014.20.2.173
39. Hwang HM. The effect of nurse image and major satisfaction on professional self-concept perceived by nursing students after clinical practice. JKAIS. 2018;19(6):476–483. doi:10.5762/KAIS.2018.19.6.476
40. Ji EJ. Influence of nursing professionalism, empathic ability on communication ability in senior nursing student. JKDAS. 2014;16(3):1685–1697.
41. Kim CH, Kim JY. Influence of nursing students’ clinical practice learning environment, self-leadership, and clinical practice belonging on nursing professionalism. J Korean Acad Soc Nurs Educ. 2019;25(1):5–16. doi:10.5977/jkasne.2019.25.1.5
42. Lee EK, Ji EJ. Factors influencing nursing professionalism in nursing students: clinical learning environment and attitude toward nurse-physician collaboration. J Korean Acad Fundam Nurs. 2016;23(2):126–135. doi:10.7739/jkafn.2016.23.2.126
43. Seong JA, Yeom EY, Do YS. Image of nurses and nursing professional values perceived by nursing students. J KoCon a. 2014;14(11):798–809. doi:10.5392/JKCA.2014.14.11.798
44. Yeun EJ, Kwon YM. A correlation study on nursing professional values, department satisfaction, sociality, self-esteem among nursing students. JKANA. 2007;13(3):285–292.
45. Chang SJ, Park S, Son Y. A topic modeling analysis for Korean online newspapers: focusing on the social perceptions of nurses during the COVID-19 epidemic period. J Korean Acad Soc Nurs Educ. 2022;28(4):444–455. doi:10.5977/jkasne.2022.28.4.444
46. Abuhammad S, AlAzzam M, Mukattash T. The perception of nurses towards their roles during the COVID-19 pandemic. Int J Clin Pract. 2021;75(4):e13919. doi:10.1111/ijcp.13919
47. Rossi S, Cosentino C, Bettinaglio GC, et al. Nurse’s identity role during Covid-19. Acta Biomed. 2021;92(S2):e2021036. doi:10.23750/abm.v92iS2.11959
48. ten Hoeve Y, Jansen G, Roodbol P. The nursing profession: public image, self-concept and professional identity. A discussion paper. J Adv Nurs. 2014;70(2):295–309. doi:10.1111/jan.12177
49. Kelly J, Fealy GM, Watson R. The image of you: constructing nursing identities in YouTube. J Adv Nurs. 2012;68(8):1804–1813. doi:10.1111/j.1365-2648.2011.05872.x
50. Pierrotti VW, Guirardello EB, Toledo VP. Nursing knowledge patterns: nurses’ image and role in society perceived by students. Rev Bras Enferm. 2020;73(4):e20180959. doi:10.1590/0034-7167-2018-0959
51. Zaragoza-García I, Ortuño-Soriano I, Posada-Moreno P, Sánchez-Gómez R, Raurell-Torredà M. Virtual simulation for last-year nursing graduate students in times of COVID-19: a quasi-experimental study. Clin Simul Nurs. 2021;60:32–41. doi:10.1016/j.ecns.2021.07.003
52. Roberts E, Kaak V, Rolley J. Simulation to replace clinical hours in nursing: a meta-narrative review. Clin Simul Nurs. 2019;37:5–13. doi:10.1016/j.ecns.2019.07.003
53. Bang KS, Kang JH, Nam ES, et al. Nursing students’ confidence in clinical competency and job readiness during the COVID-19 pandemic era. J Korean Acad Soc Nurs Educ. 2021;27(4):402–411. doi:10.5977/jkasne.2021.27.4.402
54. Oh YK, Kim EY. The effects of clinical learning environment on nursing students’ powerlessness and self-efficacy related to clinical practice. J East-West Nurs Res. 2018;24(1):36–43. doi:10.14370/jewnr.2018.24.1.36
55. Choi DW. Clinical competence according to experiences on the essential of fundamental nursing skills in nursing students. J Korean Acad Soc Nurs Educ. 2014;20(2):184–191. doi:10.5977/jkasne.2014.20.2.184
56. Liou SR, Liu HC, Tsai SL, Chu TP, Cheng CY. Performance competence of pregraduate nursing students and hospital nurses: a comparison study. J Clin Nurs. 2020;29(13–14):2652–2662. doi:10.1111/jocn.15287
57. Masoudi Alavi N. Self-efficacy in nursing students. Nurs Midwifery Stud. 2014;3(4):e25881. doi:10.17795/nmsjournal25881
58. Cavanaugh J, Jacquemin S, Junker C. A look at student performance during the COVID-19 pandemic. Qual Assur Educ. 2023;31(1):33–43. doi:10.1108/QAE-01-2022-0008
59. Rodríguez-Planas N. COVID-19, college academic performance, and the flexible grading policy: a longitudinal analysis. J Public Econ. 2022;207:104606. doi:10.1016/j.jpubeco.2022.104606
60. Song C. Changes in evidence-based practice self-efficacy among nursing students and the impact of clinical competencies: longitudinal descriptive study. Nurse Educ Today. 2024;132:106008. doi:10.1016/j.nedt.2023.106008
61. Demirelli EG, Karaçay P. Factors associated with nursing students’ online learning self-efficacy: a descriptive cross-sectional study. Nurse Educ Today. 2024;132:106029. doi:10.1016/j.nedt.2023.106029
62. Al Gharibi KA, Schmidt N, Arulappan J. Effect of repeated simulation experience on perceived self-efficacy among undergraduate nursing students. Nurse Educ Today. 2021;106:105057. doi:10.1016/j.nedt.2021.105057
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
