Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
The Relationship Between Comorbidities and Microbiologic Findings in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Authors Seo H , Sim YS , Min KH , Lee JH , Kim BK , Oh YM , Ra SW , Kim TH , Hwang YI , Park JW
Received 28 January 2022
Accepted for publication 3 April 2022
Published 20 April 2022 Volume 2022:17 Pages 855—867
DOI https://doi.org/10.2147/COPD.S360222
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Hyewon Seo,1 Yun Su Sim,2 Kyung Hoon Min,3 Jae Ha Lee,4 Byung-Keun Kim,5 Yeon Mok Oh,6 Seung Won Ra,7 Tae-Hyung Kim,8 Yong Il Hwang,9 Jeong-Woong Park10
1Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Republic of Korea; 2Division of Pulmonary, Allergy and Critical Care Medicine, Kangnam Sacred Heart Hospital, Seoul, Republic of Korea; 3Division of Pulmonology, Allergy and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Republic of Korea; 4Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Republic of Korea; 5Division of Pulmonology, Allergy and Critical Care Medicine, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Republic of Korea; 6Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea; 7Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea; 8Division of Pulmonary and Critical Care Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Republic of Korea; 9Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Republic of Korea; 10Department of Allergy, Pulmonary and Critical Care Medicine, Gachon University Gil Medical Center, Incheon, Republic of Korea
Correspondence: Jeong-Woong Park, Department of Allergy, Pulmonary and Critical Care Medicine, Gachon University Gil Medical Center, Namdong-daero 774 beon-gil, Namdong, Incheon, 21565, Republic of Korea, Tel +82-10-5574-0164, Fax +82-32-469-4320, Email [email protected]
Purpose: Data regarding the relationship between microbiologic features and comorbidities in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) are limited. The aim of this study was to correlate microbiologic findings with comorbidities in patients with moderate to severe AECOPD.
Patients and Methods: This multicenter observational study included patients with AECOPD seen at 28 hospitals in South Korea between January 2015 and December 2018, and the data were retrospectively collected. Pathogens were examined in patients with either pulmonary or extrapulmonary comorbidities, and compared to those of patients without comorbidities. The relationship between pathogen type and the number of comorbidities was also evaluated.
Results: Bacterial infections (178 [37.2%] vs 203 [28.7%], p = 0.002) and co-infections with bacteria and viruses (65 [13.6%] vs 57 [8.1%], p = 0.002) were more prevalent in patients with pulmonary comorbidities. Bacterial pathogens (280 [34.7%] vs 101 [26.7%], p=0.006) were detected at a higher rate in patients with extrapulmonary comorbidities. Previous pulmonary tuberculosis (PTB), bronchiectasis, and diabetes mellitus were risk factors for bacterial infection, and congestive heart failure was a risk factor for bacterial and viral co-infection. As the number of comorbidities increased, the risk of bacterial infection increased considerably. Pseudomonas aeruginosa was more frequently identified in patients with previous PTB (57 [15.3%] vs 59 [7.4%], p < 0.001) and bronchiectasis (33 [19.6%] vs 83 [8.3%], p < 0.001).
Conclusion: AECOPD patients with comorbidities were more likely to experience infection-related exacerbations compared to those without comorbidities. As the overall number of comorbidities increased, the risk of bacterial infection increased significantly.
Keywords: chronic obstructive pulmonary disease, acute exacerbation, comorbidity, bacteria, virus
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease with acute exacerbations throughout its course. Acute exacerbation of COPD (AECOPD) is defined as an acute worsening of respiratory symptoms that require additional treatment.1 An AECOPD is associated with increased risks of hospitalization and mortality, and higher healthcare costs.2–5 Many patients with COPD have comorbidities that significantly influence their prognosis.6 The presence of comorbidities in patients with COPD has been related to longer hospitalization, higher short-term mortality, and increased healthcare costs associated with hospitalization during an AECOPD.7,8 Spece et al reported that patients with comorbidities were less likely to receive corticosteroid and antibiotic treatment during an AECOPD.9 This may be due to the increased complexity of the overall treatment and concerns related to treatment-related adverse events.
COPD exacerbations can be triggered by several factors, including respiratory infections, air pollution, and other environmental conditions.10 Of these, bacterial and viral infections are the major causes of AECOPD.10–12 Therefore, appropriate antimicrobial treatment is important for managing AECOPD. Investigating the relationship between patient comorbidities and microbiologic features would help the selection of appropriate antimicrobial agents, thus aiding the management of AECOPD. However, data regarding this relationship are limited. The aim of this study was to explore the relationship between the microbiology and comorbidities of patients with moderate to severe AECOPD.
Materials and Methods
Study Design and Population
This multicenter observational study included patients that experienced an AECOPD between January 2015 and December 2018. Demographic, clinical, and microbiologic data were extracted from electronic medical records held by 28 hospitals in South Korea. Inclusion criteria included: aged > 40 years; COPD diagnosis confirmed by a pulmonary function test (post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity < 0.7) performed within 6 months before the onset of AECOPD; diagnosed with moderate to severe exacerbation, defined as acute worsening of respiratory symptoms that required antibiotics or systemic corticosteroid treatment or hospitalization; and patients who underwent both culture of lower respiratory tract samples, including sputum, tracheal aspirate, and bronchial washing fluid, and PCR test for viruses.
The positivity rate for bacterial or viral pathogens was investigated in patients with AECOPD who had pulmonary or extrapulmonary comorbidities. This was compared to the rate in patients without comorbidities. The association between the number of comorbidities and identity of the pathogen was also evaluated, in addition to the relationship between individual comorbidities and pathogen species. This study was approved by the Institutional Review Board of Kyungpook National University Hospital (KNHU IRB No. 2020-01-019). All the patients in the current study provided written informed consent for participation. This study was conducted in accordance with the guidelines of the 2013 Declaration of Helsinki.
Data Collection
Demographic data, including age, sex, smoking history, and body mass index, were collected. The presence and number of comorbidities in each patient were reviewed. Pulmonary comorbidities included previous pulmonary tuberculosis (PTB), bronchiectasis, and interstitial lung disease. Extrapulmonary comorbidities included diabetes mellitus, hypertension, liver cirrhosis, congestive heart failure (CHF), chronic kidney disease, cerebrovascular disease, and advanced cancer. Lung function according to FEV1 and symptom severity according to the Modified Medical Research Council (mMRC) dyspnea scale were also reviewed. In addition, moderate or severe exacerbations in the previous year and treatments of COPD were recorded.
Microbiological Data
Microbiological data were collected from bacterial and viral pathogen test results. Pathogens were deemed as the causative agent of AECOPD if any of the following criteria were met: a culture of bacteria from a lower respiratory tract sample collected within 2 days of hospitalization plus a compatible Gram-stain finding; positivity for a respiratory virus (adenovirus, influenza [types A and B], parainfluenza virus [types 1, 2 and 3], rhinovirus, respiratory syncytial virus, bocavirus, metapneumovirus, coronavirus [229E and OC43] or enterovirus) in a throat or nasopharyngeal swab as determined by multiplex reverse transcriptase (RT)-PCR test (Real-Q RV Detection kit, BioSewoom, Korea; Anyplex II RV16, Seegene, Korea; AdvanSure RV, LG Life Sciences, Korea); identification of influenza A or B antigen in a throat or nasopharyngeal swab (SD BIOLINE Influenza Antigen test, Standard Diagnostics, Yongin, Korea; BD Veritor System for Rapid Detection of FluA+B, BD Diagnostics, Sparks, MD, USA); presence of Mycoplasma pneumoniae, Chlamydophila pneumoniae, or Legionella pneumophila in sputum, as confirmed by polymerase chain reaction (PCR) tests (Seeplex® PneumoBacter ACE Detection, Seegene, Korea; AmpliSens Mycoplasma pneumoniae/Chlamydophila pneumoniae-FEP PCR, Central Research Institute for Epidemiology, Moscow, Russia); M. pneumoniae and C. pneumoniae were identified based on a positive immunoglobulin M result in blood.
Statistical Analysis
Data are expressed as means with standard deviations for continuous variables, and as numbers with percentages for categorical variables. Student’s t-test was used to compare continuous variables between groups and the chi-square test was used to compare categorical variables. Multiple logistic regression analysis was conducted to investigate the relationship between comorbidities and positive respiratory pathogen results. Age, gender, and ICS use were included as confounding variables when performing multiple logistic regression analyses. To assess the goodness-of-fit of the logistic regression models, the Hosmer‒Lemeshow test was used. SPSS Statistics software (version 25.0; IBM Corporation, Armonk, NY, USA) for Windows (Microsoft Corp., Redmond, WA, USA) was used for the statistical analysis. A p-value < 0.05 was considered statistically significant.
Results
Enrolled Patients
Overall, 1186 patients with AECOPD were included in the study. The mean age of the enrolled patients was 73.78 ± 9.22 years and 979 (82.5%) were male (Table 1). Of the patients, 844 (73%) had a history of smoking, with a mean average of 38.74 ± 26.03 packs/year; 966 (81.5%) patients had at least one comorbidity, with pulmonary and extrapulmonary comorbidities being present in 478 (40.3%) and 808 (68.1%) patients, respectively. Of the pulmonary comorbidities, previous PTB (31.8%) was the most common, followed by bronchiectasis (14.2%) and interstitial lung disease (2.3%). The most common extrapulmonary comorbidities were hypertension (49.2%), diabetes mellitus (26.8%), and CHF (14.0%). The mean FEV1 was 49.5% predicted, and the mean mMRC score was 2.25. Moderate and severe exacerbations in the previous year were 0.59 and 0.97, respectively. Nearly half of the patients received inhaled corticosteroid therapy.
 |
Table 1 Baseline Characteristics of Patients with Acute Exacerbation of COPD (n=1186) |
Identification of Respiratory Pathogens
Causative pathogens were identified in 55.1% of the patients with AECOPD (Figure 1). Bacteria and viruses were detected in 32.1% and 33.2% of the patients, respectively. Bacterial and viral co-infections were identified in 10.3% of patients. Bacterial infections (178 [37.2%] vs 203 [28.7%], p = 0.002) and bacterial/viral co-infection (65 [13.6%] vs 57 [8.1%], p = 0.002) were more prevalent in patients with pulmonary comorbidities compared to those without pulmonary comorbidities. In patients with extrapulmonary comorbidities, all causative pathogens (463 [57.3%] vs 190 [50.3%], p = 0.023) and bacteria (280 [34.7%] vs 101 [26.7%], p=0.006) were more commonly detected than in those without extrapulmonary comorbidities.
To evaluate the relationship between individual comorbidities and the presence of respiratory pathogens, multiple logistic regression analysis was performed (Table 2). Previous PTB [odds ratio (OR) 1.426, 95% confidence interval (CI) 1.096–1.857, p=0.008], bronchiectasis (OR 1.437, 95% CI 1.020–2.024, p=0.038), and diabetes mellitus (OR 1.318, 95% CI 1.003–1.733, p=0.048) were associated with an increased likelihood of detecting bacteria (Hosmer‒Lemeshow test, p= 0.625). Having CHF (OR 1.701, 95% CI 1.047–2.763, p=0.032) was a risk factor for bacterial and viral co-infection (Hosmer‒Lemeshow test, p=0.953). No comorbidities showed statistically significant associations with all causative pathogens and viruses (Table S1).
 |
Table 2 Multiple Logistic Regression Analysis of Comorbidities for Identification of Bacteria and Co-Infection with Bacteria and Viruses |
The association between the number of comorbidities and likelihood of detecting a causative pathogen was also examined (Table 3). A multiple logistic regression analysis that included the number of comorbidities, age, sex, and use of inhaled corticosteroids was performed. The risk of bacterial infection increased significantly as the number of comorbidities increased. Compared to patients without comorbidities, the OR for bacterial infection was 1.430 (95% CI 1.008–2.027. p=0.045) in patients with one or two comorbidities and 2.101 (95% CI 1.409–3.132, p<0.001) in patients with three or more comorbidities (Hosmer‒Lemeshow test, p=0.690).
 |
Table 3 The Multivariate Adjusted Odds Ratios for Identification of Respiratory Pathogens According to the Number of Comorbidities |
Microbiologic Analysis of Patients with Pulmonary Comorbidities
Among all patients with AECOPD, the most frequently detected bacteria were Pseudomonas aeruginosa (9.9%), M. pneumoniae (8.2%), Streptococcus pneumoniae (5.0%), and Klebsiella pneumoniae (4.4%) (Table 4). The most frequently detected viruses were influenza A virus (10.9%), rhinovirus (10.4%), and respiratory syncytial virus (RSV) (4.3%).
 |
Table 4 Microbiologic Analysis of AECOPD Patients with Pulmonary Comorbidities |
The causative microorganisms in patients with and without pulmonary comorbidities were compared. Of the bacterial pathogens, P. aeruginosa was more commonly detected in patients with previous PTB (57 [15.3%] vs 59 [7.4%], p < 0.001) and bronchiectasis (33 [19.6%] vs 83 [8.3%], p < 0.001) than in those with no history of those conditions. Escherichia coli was more frequently identified in patients with bronchiectasis (11 [6.5%] vs 17 [1.7%], p < 0.001) and interstitial lung disease (4 [15.4%] vs 50 [4.4%], p = 0.003) than in those without those conditions. Of the viral pathogens, rhinovirus was less frequently detected in patients with previous PTB (23 [7.5%] vs 80 [11.7%], p = 0.047), while adenovirus was more frequently detected in patients with bronchiectasis (5 [3.7%] vs 8 [0.9%], p = 0.023), compared to those without those conditions.
Microbiologic Analysis of Patients with Extrapulmonary Comorbidities
The causative microorganisms in patients with and without extrapulmonary comorbidities were compared (Table 5 and Table S2). Of the bacterial pathogens, E. coli was more frequently detected in patients with diabetes mellitus than in those without diabetes mellitus (14 [4.5%] vs 14 [1.6%], p = 0.005). M. pneumoniae was more frequently detected in patients with CHF (22 [16.5%] vs 51 [6.7%], p < 0.001) and advanced cancer (15 [15.0%] vs 58 [7.3%], p = 0.008) than in those without those conditions. Of the viruses, RSV was more commonly detected in patients with CHF than in those without it (12 [8.3%] vs 30 [3.6%], p = 0.009). Adenovirus was more common in patients with chronic kidney disease than in those without the disease (3 [4.6%] vs 10 [1.1%], p = 0.048), and metapneumovirus was more frequently detected in patients with cerebrovascular disease than in those without (6 [9.0%] vs 30 [3.3%], p = 0.030).
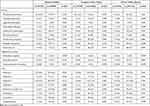 |
Table 5 Microbiologic Analysis of AECOPD Patients with Diabetes Mellitus, Congestive Heart Failure, and Chronic Kidney Disease |
Discussion
This study demonstrated that among patients with AECOPD, bacterial infections and viral/bacterial co-infections were more prevalent in those with than without pulmonary comorbidities. Bacterial pathogens were detected at higher rates in patients with extrapulmonary comorbidities. Previous PTB, bronchiectasis, and diabetes mellitus increased the risk of having a bacterial infection, while CHF increased the risk of experiencing a bacterial and viral co-infection. As the number of comorbidities increased, the risk of experiencing a bacterial infection increased considerably. Moreover, there was a correlation between pathogen species and the type of comorbidity. P. aeruginosa was more frequently detected in patients with previous PTB and bronchiectasis, while E. coli was more commonly detected in patients with bronchiectasis, interstitial lung disease, and diabetes mellitus.
In previous studies, the most commonly isolated bacteria in patients with AECOPD were Haemophilus influenzae, S. pneumoniae, Moraxella catarrhalis, and P. aeruginosa.11 However, H. influenzae and M. catarrhalis were not commonly identified in our study. According to a study conducted at a tertiary hospital in South Korea, P. aeruginosa was the most common cause of AECOPD, with H. influenzae accounting for 5.3% and M. catarrhalis accounting for 1.1%.13 The prevalence of H. influenzae and M. catarrhalis in patients with community-acquired pneumonia in the Korean population were also lower than in other countries.14 We assume that the low detection rate of these pathogens may be related to regional differences and laboratory environmental factors.
Many patients with COPD have comorbidities, and those with more advanced COPD are more likely to have comorbidities.7 This is associated with an increased risk of experiencing acute exacerbation and mortality.15,16 Moreover, many patients with COPD have more than one comorbidity.17 According to a previous study, the overall number of comorbidities has been related to the frequency of experiencing acute exacerbation.18 Previous studies have also demonstrated that comorbidities are highly prevalent among patients experiencing AECOPD,19 which was associated with longer hospitalization and a higher likelihood of mortality.6–9 Therefore, the presence of comorbidities must be recognized in the management of patients with AECOPD, which require more complex and individualized therapy.
The findings of this study suggested that respiratory infection was more likely to be a cause of exacerbation in patients with AECOPD who had comorbidities compared to those who did not. A previous study also demonstrated that infection-related exacerbations were more severe than exacerbations that were not related to infections.12 Considering the high incidence of infection-related AECOPD in patients with comorbidities and the severity of infection related exacerbation, efforts to identify causative pathogens to guide the appropriate use of antimicrobial agents are required in AECOPD patients with comorbidities. In addition, exacerbations caused by bacterial and viral co-infection are more severe than infection caused by bacteria or viruses alone.10,12 In this study, bacterial and viral co-infections occurred more often in patients with than without pulmonary comorbidities. In, addition, CHF was a risk factor for bacterial and viral co-infection. A recent study investigated the efficacy of a vaccine targeted at non-typeable H. influenzae and M. catarrhalis in preventing AECOPD.20 Our study will aid in determining which subgroups require vaccination against a particular pathogen.
P. aeruginosa may be associated with an increased risk of exacerbation and death in patients with COPD.21 Furthermore, P. aeruginosa in the sputum of patients hospitalized for AECOPD has been identified as an independent prognostic factor for 3-year mortality.22 Therefore, in patients with AECOPD who have risk factors for P. aeruginosa infection, it is more crucial to use a sputum culture to identify the causative bacteria, and the use of antipseudomonal agents should be considered. In this study, P. aeruginosa as a causative pathogen, was more common in patients experiencing AECOPD who had bronchiectasis or previous PTB. In patients with bronchiectasis, P. aeruginosa is well known to be a common cause of respiratory infection.23,24 Additionally, the presence of P. aeruginosa is associated with more severe disease and a higher risk of mortality.25 It was previously reported that COPD patients with prior PTB were more likely to have a positive P. aeruginosa culture during an exacerbation, and showed a higher prevalence of bronchiectasis.26 Previous PTB is a risk factor for bronchiectasis,27,28 and coexisting bronchiectasis might be associated with a higher rate of detection of P. aeruginosa in patients with AECOPD and previous PTB.
E. coli is an uncommon respiratory pathogen, but can cause respiratory tract infections in the elderly and those with compromised immunity.29 According to previous studies, E. coli pneumonia was associated with comorbidities such as diabetes mellitus, cerebrovascular disease, and chronic lung diseases.29,30 In this study of patients with AECOPD, E. coli was not a common causative agent, but it was significantly more prevalent in patients with bronchiectasis, interstitial lung disease, and diabetes mellitus. Previous investigations of the relationship between bacteriologic etiology and lung function in patients with AECOPD demonstrated that P. aeruginosa and Enterobacteriaceae were predominant in patients with severely impaired lung function.31,32 Since accompanying pulmonary diseases might contribute to decreased lung function in patients with COPD, the results of this study support those of the previous ones.
Viral infection is an important cause of exacerbation of COPD. Viruses have been identified in 20–40% of patients with AECOPD.33 Atypical bacteria, such as M. pneumoniae and C. pneumoniae, also contribute to AECOPD.10 However, data regarding the relationship between comorbidities and infection with a virus or atypical bacteria are scarce. Further study based on the present one may yield additional useful information.
This study had several limitations. First, data regarding comorbidities were retrospectively obtained from electronic medical records. Therefore, the prevalence of comorbidities might be underestimated. Compared to other studies investigating patients with AECOPD, the prevalence rates of most comorbidities in this study were similar. However, the prevalence of heart failure was relatively lower, and the prevalence of advanced cancer was relatively higher.9,19 In addition, chest computed tomography was not performed in all patients, so our ability to confirm the pulmonary comorbidities was limited. Second, the numbers of patients with AECOPD who had comorbidities such as liver cirrhosis and interstitial lung disease were too small to establish definitive conclusions. Third, serologic tests for atypical bacteria, and PCR tests for atypical bacteria and certain viruses, were not performed in all patients with AECOPD. Fourth, COPD severity, such as the GOLD group, was not included in the multiple logistic regression analyses for identification of pathogens.
Conclusion
In conclusion, patients with moderate to severe AECOPD who had comorbidities were more likely to have an infection-related exacerbation than those without comorbidities. Bacterial infection was associated with previous PTB, bronchiectasis, and diabetes mellitus. Bacterial and viral co-infection was associated with congestive heart failure. The risk of experiencing a bacterial infection increased significantly as the number of comorbidities increased. Of the causative pathogens, P. aeruginosa was more common in patients with previous PTB and bronchiectasis. Because infections are the major cause of AECOPD, pathogen identification and appropriate antimicrobial therapy are important in the management of AECOPD patients. Our findings suggest that in AECOPD patients with comorbidities, a more careful diagnostic evaluation for causative pathogens is required. In addition, our findings may help with the selection of empirical antimicrobial drugs in AECOPD patients with comorbidities.
Acknowledgments
We would like to thank Ji Ye Jung (Yonsei University College of Medicine, Seoul, Korea.), Myung Goo Lee (Hallym University College of Medicine, Chuncheon, Korea), Chin Kook Rhee (The Catholic University of Korea, Seoul, Korea), Hyonsoo Joo (The Catholic University of Korea, Uijeongbu, Korea), Eung Gu Lee (The Catholic University of Korea, Bucheon, Korea), Jin Hwa Lee (Ewha Womans University College of Medicine, Seoul, Korea), Hye Yun Park (Sungkyunkwan University School of Medicine, Seoul, Korea), Woo Jin Kim (Kangwon National University College of Medicine, Chuncheon, Korea), Soo-Jung Um (Dong-A University College of Medicine, Busan, Korea), Joon Young Choi (The Catholic University of Korea, Incheon, Korea), Chang-Hoon Lee (Seoul National University Hospital, Seoul, Korea), Tai Joon An (The Catholic University College of Medicine, Seoul, Korea), Yeonhee Park (The Catholic University of Korea, Seoul), Young-Soon Yoon (Dongguk University Ilsan Hospital, Goyang-si, Korea), Joo Hun Park (Ajou University School of Medicine, Suwon, Korea), Kwang Ha Yoo (Konkuk University School of Medicine, Seoul, Korea) and Deog Kyeom Kim (Seoul National University College of Medicine, Seoul, Korea) for their participation in this study.
Funding
This work was supported by Grant No. KATRD-S-2019-1 awarded by the Korean Academy of Tuberculosis and Respiratory Diseases.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
2. Niewoehner DE. The impact of severe exacerbations on quality of life and the clinical course of chronic obstructive pulmonary disease. Am J Med. 2006;119(10 Suppl 1):38–45. doi:10.1016/j.amjmed.2006.08.006
3. Spencer S, Calverley P, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J. 2004;23(5):698–702. doi:10.1183/09031936.04.00121404
4. Ramsey S, Sullivan S. The burden of illness and economic evaluation for COPD. Eur Respir J. 2003;21(41 suppl):29s–35s. doi:10.1183/09031936.03.00078203
5. Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥18 years in the United States for 2010 and projections through 2020. Chest. 2015;147(1):31–45. doi:10.1378/chest.14-0972
6. Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. doi:10.1183/09031936.00133805
7. Almagro P, Cabrera FJ, Diez J, et al. Comorbidities and short-term prognosis in patients hospitalized for acute exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI) study. Chest. 2012;142(5):1126–1133. doi:10.1378/chest.11-2413
8. Terzano C, Colamesta V, Unim B, et al. Chronic obstructive pulmonary disease (COPD) exacerbation: impact of comorbidities on length and costs during hospitalization. Eur Rev Med Pharmacol Sci. 2017;21(16):3680–3689.
9. Spece LJ, Epler EM, Donovan LM, et al. Role of comorbidities in treatment and outcomes after chronic obstructive pulmonary disease exacerbations. Ann Am Thorac Soc. 2018;15(9):1033–1038. doi:10.1513/AnnalsATS.201804-255OC
10. Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359(22):2355–2365. doi:10.1056/NEJMra0800353
11. Sapey E, Stockley RA. COPD exacerbations· 2: aetiology. Thorax. 2006;61(3):250–258. doi:10.1136/thx.2005.041822
12. Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med. 2006;173(10):1114–1121. doi:10.1164/rccm.200506-859OC
13. Choi J, Oh JY, Lee YS, et al. Bacterial and viral identification rate in acute exacerbation of chronic obstructive pulmonary disease in Korea. Yonsei Med J. 2019;60(2):216–222. doi:10.3349/ymj.2019.60.2.216
14. Lee MS, Oh JY, Kang CI, et al. Guideline for antibiotic use in adults with community-acquired pneumonia. Infect Chemother. 2018;50(2):160–198. doi:10.3947/ic.2018.50.2.160
15. Lenferink A, van der Palen J, van der Valk P, et al. Exacerbation action plans for patients with COPD and comorbidities: a randomised controlled trial. Eur Respir J. 2019;54(5):1802134. doi:10.1183/13993003.02134-2018
16. Vanfleteren LE, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):728–735. doi:10.1164/rccm.201209-1665OC
17. Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109. doi:10.2147/COPD.S54473
18. Fumagalli G, Fabiani F, Forte S, et al. INDACO project: COPD and link between comorbidities, lung function and inhalation therapy. Multidiscip Respir Med. 2015;10(1):4. doi:10.1186/2049-6958-10-4
19. Almagro P, Lopez Garcia F, Cabrera FJ, et al. Comorbidity and gender-related differences in patients hospitalized for COPD. The ECCO study. Respir Med. 2010;104(2):253–259. doi:10.1016/j.rmed.2009.09.019
20. Andreas S, Testa M, Boyer L, et al. Non-typeable Haemophilus influenzae–Moraxella catarrhalis vaccine for the prevention of exacerbations in chronic obstructive pulmonary disease: a multicentre, randomised, placebo-controlled, observer-blinded, proof-of-concept, phase 2b trial. Lancet Respir Med. 2022. doi:10.1016/S2213-2600(21)00502-6
21. Eklof J, Sorensen R, Ingebrigtsen TS, et al. Pseudomonas aeruginosa and risk of death and exacerbations in patients with chronic obstructive pulmonary disease: an observational cohort study of 22 053 patients. Clin Microbiol Infect. 2020;26(2):227–234. doi:10.1016/j.cmi.2019.06.011
22. Almagro P, Salvado M, Garcia-Vidal C, et al. Pseudomonas aeruginosa and mortality after hospital admission for chronic obstructive pulmonary disease. Respiration. 2012;84(1):36–43. doi:10.1159/000331224
23. Polverino E, Cilloniz C, Menendez R, et al. Microbiology and outcomes of community acquired pneumonia in non cystic-fibrosis bronchiectasis patients. J Infect. 2015;71(1):28–36. doi:10.1016/j.jinf.2015.03.009
24. Sanchez-Muñoz G, López-de-andrés A, Hernández-Barrera V, et al. Hospitalizations for community-acquired and non-ventilator-associated hospital-acquired pneumonia in Spain: influence of the presence of bronchiectasis. A retrospective database study. J Clin Med. 2020;9(8):2339. doi:10.3390/jcm9082339
25. Dicker AJ, Lonergan M, Keir HR, et al. The sputum microbiome and clinical outcomes in patients with bronchiectasis: a prospective observational study. Lancet Respir Med. 2021;9(8):885–896. doi:10.1016/S2213-2600(20)30557-9
26. Jin J, Li S, Yu W, Liu X, Sun Y. Emphysema and bronchiectasis in COPD patients with previous pulmonary tuberculosis: computed tomography features and clinical implications. Int J Chron Obstruct Pulmon Dis. 2018;13:375–384. doi:10.2147/COPD.S152447
27. Jin J, Yu W, Li S, Lu L, Liu X, Sun Y. Factors associated with bronchiectasis in patients with moderate-severe chronic obstructive pulmonary disease. Medicine. 2016;95(29):e4219. doi:10.1097/MD.0000000000004219
28. Byrne AL, Marais BJ, Mitnick CD, Lecca L, Marks GB. Tuberculosis and chronic respiratory disease: a systematic review. Int J Infect Dis. 2015;32:138–146. doi:10.1016/j.ijid.2014.12.016
29. Okimoto N, Hayashi T, Ishiga M, et al. Clinical features of Escherichia coli pneumonia. J Infect Chemother. 2010;16(3):216–218. doi:10.1007/s10156-010-0034-Z
30. Schneer S, Khoury J, Adir Y, et al. Clinical characteristics and outcomes of patients with Escherichia coli in airway samples. Clin Respir J. 2020;14(3):205–213. doi:10.1111/crj.13116
31. Miravitlles M, Espinosa C, Fernández-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116(1):40–46. doi:10.1378/chest.116.1.40
32. Eller J, Ede A, Schaberg T, Niederman MS, Mauch H, Lode H. Infective exacerbations of chronic bronchitis: relation between bacteriologic etiology and lung function. Chest. 1998;113(6):1542–1548. doi:10.1378/chest.113.6.1542
33. Mohan A, Chandra S, Agarwal D, et al. Prevalence of viral infection detected by PCR and RT-PCR in patients with acute exacerbation of COPD: a systematic review. Respirology. 2010;15(3):536–542. doi:10.1111/j.1440-1843.2010.01722.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

