Back to Journals » Journal of Pain Research » Volume 16
The Psychosocial Characteristics and Somatosensory Function of Children and Adolescents Who Meet the Criteria for Chronic Nociplastic Pain
Authors Ocay DD , Ross BD, Moscaritolo L, Ahmed N , Ouellet JA, Ferland CE, Ingelmo PM
Received 3 December 2022
Accepted for publication 10 February 2023
Published 15 February 2023 Volume 2023:16 Pages 487—500
DOI https://doi.org/10.2147/JPR.S397829
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Giorgio Veneziano
Don Daniel Ocay,1– 3 Brendan D Ross,4 Lorenzo Moscaritolo,3 Nabeel Ahmed,4 Jean A Ouellet,2,5– 7 Catherine E Ferland,1– 3,6– 8,* Pablo M Ingelmo3,6– 8,*
1Department of Experimental Surgery, McGill University, Montreal, QC, Canada; 2Department of Clinical Research, Shriners Hospitals for Children Canada, Montreal, QC, Canada; 3Edwards Family Interdisciplinary Centre for Complex Pain, Montreal Children’s Hospital, Montreal, QC, Canada; 4Faculty of Medicine, McGill University, Montreal, QC, Canada; 5Department of Pediatric Surgery, McGill University, Montreal, QC, Canada; 6Department of Anesthesia, McGill University, Montreal, QC, Canada; 7Research Institute-McGill University Health Centre, Montreal, QC, Canada; 8Alan Edwards Research Center for Pain, McGill University, Montreal, QC, Canada
*These authors contributed equally to this work
Correspondence: Pablo M Ingelmo, Edwards Family Interdisciplinary Centre for Complex Pain, Montreal Children’s Hospital, B02-3525-1001 Boulevard Décarie, Montreal, H4A 13J, Canada, Tel +1 514 412-4448, Fax +1 514 412-4341, Email [email protected]
Purpose: Nociplastic pain distinguishes individuals with pain and hypersensitivity in body regions with apparently normal tissues, without any signs of neuropathy, but with contribution of central and/or peripheral sensitization. There is a lack of literature describing nociplastic pain in the pediatric population. The objective of this study was to investigate the differences between pediatric patients with nociplastic pain compared with patients with non-nociplastic pain.
Patients and Methods: This study included 414 pediatric patients followed at an interdisciplinary centre for complex pain. All patients underwent an exhaustive pain assessment consisting of face-to-face interviews, validated self-report questionnaires and quantitative sensory testing. Recently established criteria for chronic nociplastic pain, and quantitative sensory testing was used to describe and stratify our cohort.
Results: One hundred and sixty-five patients (40%) were stratified as having possible nociplastic pain and two hundred and forty-nine (60%) patients, as non-nociplastic pain. Patients with nociplastic pain displayed pain hypersensitivity in the region of pain, more symptoms of panic and social phobia, and worse sleep quality than patients with non-nociplastic pain. The proportion of patients achieving a meaningful clinical outcome after completion of their treatment (medications, physiotherapy, psychology, nursing, social worker, and/or interventional procedures) was lower in patients with nociplastic pain (62%) than those without nociplastic pain (86%).
Conclusion: Our results suggest that patients who meet the criteria for nociplastic pain can be identified in a population of children and adolescents being treated in a center for complex pain. Combining screening with validated questionnaires and quantitative sensory testing facilitates the phenotyping and graded severity of patients with nociplastic pain in daily clinical practice.
Keywords: nociplastic pain, chronic pain, children, adolescents, quantitative sensory testing
Introduction
Nearly one in five children and adolescents reports persistent or recurrent chronic pain.1 In 2017, a third pain mechanism category alongside nociceptive and neuropathic pain, nociplastic pain, was introduced by the International Association for the Study of Pain (IASP).2 Nociplastic pain is defined as “pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain”.2
Research on nociplastic pain has used quantitative sensory testing (QST) to assess altered nociceptive processing.3,4 Recently, clinically useful criteria for nociplastic pain were established by the IASP Terminology Task Force (TTF).5 In summary, chronic nociplastic pain is defined as 1) pain duration >3 months, 2) a regional rather than discrete distribution, 3) not entirely explained by nociceptive or neuropathic pain mechanisms, and 4) displaying clinical signs of pain hypersensitivity in the region of pain. The presence of a history of pain hypersensitivity in the region of pain and defined co-morbidities (eg, sleep disturbance and cognitive problems) strengthens the probability of nociplastic pain.5 These criteria can be assessed through validated self-reported questionnaires and quantitative sensory testing.
Fibromyalgia, complex regional pain syndrome and irritable bowel syndrome are examples of chronic pain conditions which meet the criteria for nociplastic pain.2 These chronic pain conditions are also observed in pediatric populations, and studies have displayed altered nociceptive processing and the presence of comorbidities in youth.6–8 However, there is a lack of knowledge in describing nociplastic pain in pediatrics and whether the clinical criteria may also reflect what is observed in the pediatric population.
The objective of the study was to investigate differences between children and adolescents who do and do not meet the criteria for nociplastic pain. The aim was to characterize patients followed at an interdisciplinary center for complex pain based on variety of biopsychosocial factors, as well as their clinical outcomes, as recommended by the Pediatric Initiative on Methods, Measurement, and Pain Assessments in Clinical Trials (PedIMMPACT).9,10 We hypothesized that significant differences in the biopsychosocial factors and clinical outcomes will be observed between patients who do meet the criteria for nociplastic pain when compared with children who do not meet the criteria for nociplastic pain.
Materials and Methods
Ethics approval was obtained prior to the beginning of the recruitment from the Research Ethics Board of the McGill University Health Centre (2019–4887, 2019–4670). The study was conducted in accordance with the Declaration of Helsinki. Patients from the Edwards Family Interdisciplinary Center for Complex Pain of the Montreal Children’s Hospital were approached to approve the collection of their medical data from their electronic charts for research purposes. Written informed consent was provided by patients 14 years old and older, or their parent/legal guardian, along with the assent of the patient if under 14 years old, prior to them being included in the analysis.
Population
The retrospective analysis included patients assisted by the Edwards Family Interdisciplinary Center for Complex Pain that underwent QST assessment between May 2016 and September 2021, and reported chronic pain defined as persistent or recurrent pain for at least three months. The team of the Edwards Family Interdisciplinary Center for Complex Pain accepts patients with chronic pain independent of the type or diagnosis, referred primarily by specialists (more than 90%) rather than primary care doctors or general pediatricians.
Nociplastic Pain
We used a recently established clinical criteria and grading system for chronic nociplastic pain affecting the musculoskeletal system to stratify our cohort as meeting or not meeting the criteria for nociplastic pain as a dominant pain mechanism.2,5,11 We defined patients as meeting the criteria for nociplastic pain5 when they have (1) regional pain rather than discrete/distinct in distribution, (2) with no evidence that nociceptive or neuropathic pain is entirely responsible for the pain, and (3) with the presence of evoked pain hypersensitivity that can be elicited clinically in the region of pain (ie presence of peripheral or central sensitization; allocated to a mechanical or thermal hyperalgesia somatosensory profile12).
Clinical Outcome Measures at the Initial Clinic Visit
Patient demographic characteristics, and past hospitalizations/surgeries were collected through questionnaires completed before the first appointment. Patients and parents also completed validated pain-related questionnaires. Current pain medication intake, previous pain medication taken, and previous medical treatment for pain were also collected. The team discussed the patient and parents’ self-assessment before the initial evaluation and were confirmed through face-to-face interviews.
Before the initial evaluation, each patient underwent a specific protocol of mechanical and thermal QST to obtain a comprehensive profile of somatosensory functioning and pain modulatory responses. The results of the QST were available during the first evaluation and were used to personalize the treatment program of each patient.13,14
During an interdisciplinary face-to-face interview, we evaluated the intensity, duration and frequency of the pain over the previous month using a numerical rating scale (NRS) ranging from 0 to 10, representing no pain at all and the worst pain imaginable, respectively. A pain specialist and a physiotherapist then conducted a detailed physical exam. This was followed by interviews with the patients/caregivers conducted by a psychologist, a social worker and a nurse clinician. At the end of the evaluation, the diagnosis and personalized treatment plan (eg medications, physiotherapy, psychology, nursing, social worker, and interventional procedures) was discussed with the patients and their parents/caregivers.13–18 Medication prescribed included non-steroidal anti-inflammatory drugs (eg ibuprofen, celecoxib), muscle relaxants (eg baclofen), opiates (eg morphine), anti-depressants (eg amitriptyline), anti-epileptics (eg gabapentin), anti-migraine agents, oral corticosteroids, sedatives (eg benzodiazepines), or other analgesics and antipyretics agents (eg acetaminophen, clonidine, magnesium, etc.). Interventional procedures included primarily peripheral nerve and interfascial plane single blocks, pulsed radiofrequency or local infiltrations.15
The evaluations, treatment, and follow-up provided by the Center for Complex Pain are entirely covered by the Quebec public health system. All the data gathered from the auto-evaluation and from the initial evaluation was prospectively documented in the database of the Center for Complex Pain and transferred to the patient’s electronic chart.
Quantitative Sensory Testing
We adapted our QST protocol from previous studies (see Supplementary Material for more details).19–21 Mechanical QST were performed on a control area (left hand) followed by the affected area (the most painful location reported by the patient). Thermal QST were performed on the forearms of the patient.
Patient- and Parent-Reported Psychosocial Outcome Measures
The Functional Disability Inventory (FDI) questionnaire,22 Revised Child Anxiety and Depression Scale (RCADS) questionnaire,23 and Pittsburgh Sleep Quality Index (PSQI) questionnaire24 was completed by patients to detect different levels of disability, children’s self-report of depression and anxiety, and sleep quality. The RCADS constitutes subscales representing separation anxiety disorder, generalized anxiety disorder, panic disorder, social phobia, obsessive compulsive disorder, and low mood (major depressive disorder). The Douleur Neuropathique 4 (DN4) questionnaire was completed by patients and their physicians to identify if their pain had a neuropathic component.25 The Pain Catastrophizing Scale for Children (PCS-C) was completed by patients to assess their negative thoughts or feelings while experiencing pain.26
The Impact on Family Scale (IOFS) was completed by parents of patients to assess family burden in the pediatric care context.27,28 A higher score represents a higher negative impact on the social and familial systems caused by a chronic childhood illness.27 The Pain Catastrophizing Scale for Parents (PCS-P) was completed by parents of patients to assess their negative thoughts or feelings while their child is experiencing pain.29
Meaningful Clinical Outcome and End of Treatment
We used the patients’ global impression of change scale (PGIC) as the primary clinical outcome measures.30,31 The PGIC is a 7-point scale and reflects a patient’s belief about treatment efficacy and overall improvement in their health condition. The treatment provided by the Center from Complex Pain ends when the patient achieved a meaningful improvement defined as the patient having normal school attendance, normal physical function, no pain, not using pain medication and reporting a PGIC score of 6 or 7.10,16
Whether patients were still receiving services at the center for complex pain as of October 2021 was noted. Other causes to be discharged from the program included transfer to adult care or to another specialist, lost to follow-up, and not compliant with the treatment.
Statistical Analysis
Available data were analyzed using R Studio and plotted using Prism-GraphPad. An average z-score (eg, z-score = affected sitepatient – control sitepatient cohort mean / control sitepatient cohort SD)12 for all QST parameters of the control and affected area was calculated for each patient. A positive z-score indicates a gain of function (hyperalgesia) while a negative score indicates a loss of function (sensory loss). A deterministic approach was used to phenotype the somatosensory profile of our cohort (sensory loss, mechanical hyperalgesia, thermal hyperalgesia or normative QST comparable to pain-free controls; see Supplementary Table 1 for more details).32,33
Differences in all outcome measures extracted from the initial visit at the center between patients allocated to meet criteria for nociplastic and non-nociplastic pain were determined with the chi-square test or Student’s t-test. Cohen’s d values were calculated for significant p-values of Student’s t-tests to determine the effect size (0.2 – small; 0.5 – medium, 0.8 – large). For patients no longer being followed by the center of complex pain, differences in the PGIC score, number of days between the initial visit date and end/transfer date, or treatment offered were determined using the Student’s t-test, an analysis of variance (ANOVA) model and the chi-square test, respectively.
Results
Four hundred and fifty patients underwent QST assessment between May 2016 and September 2021. The medical data of 18 patients was incomplete and 18 additional patients did not report pain longer than three months. Therefore, 414 patients aged 8 to 18 years were included in the analysis (Figure 1 and Table 1). The clinical presentations included patients with chronic widespread pain (n = 76), complex regional pain syndrome type I (n = 18), chronic primary (n = 33) or secondary (n = 12) headache or orofacial pain, chronic primary (n = 13) or secondary (n = 5) visceral pain, chronic primary (n = 115) or secondary (n = 75) musculoskeletal pain, chronic postsurgical or posttraumatic pain (n = 48), and chronic secondary neuropathic pain (n = 19). On average, patients reported mild-moderate pain the day of the QST assessment, but moderate-severe pain over the last month. Most patients reported pain for more than 12 months (n = 296), daily (n = 339), and constant painful episodes (n = 312) (Table 1).
 |
Table 1 Characteristics of Cohort |
Stratification for Nociplastic Pain Using Quantitative Sensory Testing
One hundred and sixty-five patients were categorized as possible nociplastic pain (40%) and two hundred and forty-nine patients presented non-nociplastic mechanisms (60%). Since evoked pain hypersensitivity was part of the criteria for meeting nociplastic pain, patients with possible nociplastic pain presented with a thermal hyperalgesia and mechanical hyperalgesia somatosensory profile more often than those with non-nociplastic pain (Figure 2A). Patients with possible nociplastic pain displayed more significant loss of function in regard to mechanical and vibration detection. Moreover, patients with possible nociplastic displayed evoked pain hypersensitivity to mechanical and thermal stimuli (Figure 2B). In addition, patients with possible nociplastic pain reported higher pain intensity the day of the assessment and over the last month (Table 1).
Temporal summation of pain (TSP) and conditioned pain modulation (CPM) assessment showed a spectrum of facilitatory and inhibitory pain modulatory responses in patients who did and did not meet the criteria for nociplastic pain (Figure 3A–D). No significant difference was observed in the CPM efficiency or TSP between patients with possible nociplastic pain and non-nociplastic pain (Table 2).
 |
Table 2 Characteristics of Patient Sample with or without Possible Nociplastic Pain |
Psychosocial Characteristics
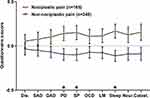
Controlling for the patients’ current and average pain over the last month, patients with nociplastic pain reported significantly higher scores for panic disorder, social phobia, and poor sleep quality than patients without nociplastic pain (Figure 4).
The impact on family scales scores was comparable between parents of children with and without nociplastic pain (Table 2). However, the pain catastrophizing scores of parents of children with nociplastic pain were higher than those without nociplastic pain (Table 2).
Meaningful Clinical Outcome and End of Treatment
Out of 267 patients no longer followed by the center of complex pain, 149 patients (56%) ended treatment and were discharged from the center and 85 patients (32%) were transferred to another clinic, institution or specialist, or transferred to an adult center. The remaining patients were either lost to follow-up (5%) or were non-compliant to the planned treatment (8%).
Sixty-one (41%) patients with nociplastic pain and eighty-eight (59%) patients without nociplastic pain completed treatment and were discharged from the center. The proportion of patients achieving a meaningful clinical outcome after completion of their treatment was significantly lower in patients with nociplastic pain (n = 38; 62%) than those without nociplastic pain (n = 76; 86%,) (χ2= 10.31, p = 0.001; Figure 5A). Thirty-nine (46%) patients with nociplastic pain and forty-six (54%) patients without nociplastic pain were transferred to another clinic, institution or specialist, or transferred to an adult center. The proportion of patients not achieving a meaningful clinical outcome upon transfer from the center was similar between patients with nociplastic pain (n = 33; 85%) and without nociplastic pain (n = 41; 89%) (χ2= 0.07, p = 0.788; Figure 5A).
The treatment time of patients discharged from the center, or the time patients are transferred to another center or adult care was similar between patients with and without nociplastic pain, when correcting for their age at admission to the clinic (Figure 5B and C).
No significant association was observed between the planned treatment of patients with or without nociplastic pain whether they completed their treatment or were transferred (Table 3).
 |
Table 3 Follow-Up Outcome Measures of Patient Sample with or Without Nociplastic Pain |
Discussion
In this study, we were able to identify children and adolescents with nociplastic pain in a sample of patients assisted in a center for complex pain. Using self-reported questionnaires and QST, patients who meet the criteria for nociplastic pain displayed differences regarding their biopsychosocial factors and clinical outcomes when compared to patients with non-nociplastic pain.
With the recent introduction of the terminology of nociplastic pain, there is still limited data characterizing this pain mechanism and its prevalence. A study on adults with multiple sclerosis and chronic pain identified that 50% had nociplastic pain with or without neuropathic pain,34 while a study on adults with symptomatic hip OA observed that 23% of their cohort displayed neuropathic, nociplastic, or mixed pain.35 Nevertheless, 40% of our sample were classified as possible nociplastic pain. Studies in pediatrics with chronic pain conditions in which nociplastic pain may be present, such as fibromyalgia, complex regional pain syndrome and irritable bowel syndrome, have provided evidence of altered nociceptive processing in these conditions through quantitative sensory testing.6–8 Similar to our findings, they have observed sensitization in the region of pain or poor functioning of the endogenous inhibitory pain pathways despite no clear lesion in the somatosensory system. Our results therefore provide evidence that nociplastic pain can be possibly identified in the clinical practice with the criteria described by Kosek et al5 and quantitative sensory testing. However, additional research is warranted to determine the prevalence of possible nociplastic in distinct pediatric chronic pain conditions.
Patients with nociplastic pain displayed more symptoms of panic disorder and social phobia, and worse sleep quality when compared to patients with non-nociplastic pain. Studies in adults with chronic pain conditions in which nociplastic pain may be present highlight that these comorbidities contribute to predicting the responsiveness of patients to pharmacological and non-pharmacological approaches.5 Furthermore, studies in pediatrics have shown that pain widespreadedness, which may involve nociplastic pain mechanisms such as altered brain function,36 has been associated with poor pain-related pain outcomes such as pain interference, pain catastrophizing, fatigue, anxiety, and depression.37 Although pain widespreadedness was not reported in our sample, we may hypothesize that pediatric patients with possible nociplastic pain may also display altered brain function leading to poorer pain-related outcomes. Notably, the parents/caregivers of patients with nociplastic pain reported higher pain catastrophizing. These findings can also be associated with social learning mechanisms and the social communication model of pain stressing the need for family interventions for patients with possible nociplastic pain.38 However, although a significant difference was observed between patients with possible nociplastic pain and those with non-nociplastic pain in regard to psychosocial factors, it’s effect size was small in magnitude probably because of the large sample size that was analyzed in the current study. We have previously identified distinct psychosocial profiles among a large sample of pediatric chronic musculoskeletal pain patients: one with high levels of distress and disability, another with relatively low scores of distress and disability, and a third group in between the other two on these measures.12 Therefore, the current criteria for nociplastic pain which includes comorbidities to make the “diagnostic probable” may not discriminate patients who may require early psychological or psychiatric interventions to reduce pain symptoms and its negative impact on the daily lives of the patients.
The lack of association between the planned treatment and the identification of nociplastic pain can be attributed to the patients included in our study receiving a multimodal interdisciplinary treatment program. However, even if our team personalized the therapeutic approaches addressing distinct pain mechanisms, more patients with non-nociplastic pain report a meaningful outcome than patients with nociplastic pain. Recently, Ferro Moura Franco et al39 conducted a systematic review on the prescription of physical exercises for patients with chronic pain along the nociplastic spectrum, and observed that global exercises should be emphasized for patients with nociplastic pain, while specific exercises should be emphasized for patients with non-nociplastic pain. Future research should evaluate the effects of targeting nociplastic pain mechanisms to optimize the personalized treatment programs in pediatric populations. Moreover, the addition of confirmatory tests and biomarkers may be important further investigate pediatric patients with nociplastic pain.40
The main strength of our study is that we provide a comprehensive description of the characteristics of pediatric patients with nociplastic pain using the clinical data collected during the daily activities of an interdisciplinary center for complex pain. We also phenotyped the patient’s somatosensory profile (sensory loss, mechanical hyperalgesia, thermal hyperalgesia or normative QST)32,33 and described their psychosocial characteristics from self-report validated questionnaires. We also used meaningful clinical outcomes to describe the changes in the health condition of pediatric patients with nociplastic pain. In other words, our study may help to make pediatric nociplastic pain matter, be better understood, be more visible and eventually be better treated.41
Our study has several limitations. Data were retrospectively obtained from a sample of patients from a single center with diverse pathological diagnoses that were determined in parallel with the QST assessment leading to some missing data to understand intergroup differences and creating some bias. However, the large heterogeneous sample size promotes the external validity of our findings to clinicians caring for children and adolescents with a diversity of chronic pain clinical presentations with the potential for reproducibility. The QST protocol measures have similarities to established protocols in the literature20 with modifications or exclusions. However, these modifications were made to fit within the time constraints of clinical routines. Somatosensory profiles determined to stratify patients with nociplastic pain are parallel to, but do not mirror adult mechanism-related profiles.33 The pharmacological and non-pharmacological treatments prior to the initial evaluation were not controlled for patients with and without nociplastic pain. However, the assessment conducted allows for it to be adapted and evaluated for application in similar clinical settings for replication.
Conclusion
In conclusion, our results provide evidence that patients who meet the criteria for nociplastic pain can be identified in a population of children and adolescents with chronic pain. The combination of screening patients with self-reported questionnaires and quantitative sensory testing facilitates identifying patients with chronic nociplastic pain with distinct characteristics and outcomes.
Acknowledgments
The Edwards Family Interdisciplinary Centre for Pediatric Complex Pain is partially funded by the Louise and Allan Edwards Foundation. DDO was supported by the Edwards PhD Studentship in Pain Research provided by the Louise and Allan Edwards Foundation. The authors would like to thank the patients and all the clinical staff of the Edwards Family Interdisciplinary Centre for Pediatric Complex Pain of the Montreal Children’s Hospital for their precious collaboration.
Disclosure
Dr Jean A. Ouellet reports grants from AO Foundation, outside the submitted work. The authors report no conflicts of interest in this work.
References
1. King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–2738. doi:10.1016/j.pain.2011.07.016
2. Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157(7):1382–1386. doi:10.1097/j.pain.0000000000000507
3. Maier C, Baron R, Tolle TR, et al. Quantitative sensory testing in the German research network on neuropathic pain (DFNS): somatosensory abnormalities in 1236 patients with different neuropathic pain syndromes. Pain. 2010;150(3):439–450. doi:10.1016/j.pain.2010.05.002
4. Zafereo J, Wang-Price S, Kandil E. Quantitative sensory testing discriminates central sensitization inventory scores in participants with chronic musculoskeletal pain: an exploratory study. Pain Pract. 2021;21(5):547–556. doi:10.1111/papr.12990
5. Kosek E, Clauw D, Nijs J, et al. Chronic nociplastic pain affecting the musculoskeletal system: clinical criteria and grading system. Pain. 2021;162(11):2629–2634. doi:10.1097/j.pain.0000000000002324
6. Coles ML, Weissmann R, Uziel Y. Juvenile primary Fibromyalgia syndrome: epidemiology, etiology, pathogenesis, clinical manifestations and diagnosis. Pediatr Rheumatol Online J. 2021;19(1):22. doi:10.1186/s12969-021-00493-6
7. Verriotis M, Peters J, Sorger C, Walker SM. Phenotyping peripheral neuropathic pain in male and female adolescents: pain descriptors, somatosensory profiles, conditioned pain modulation, and child-parent reported disability. Pain. 2021;162(6):1732–1748. doi:10.1097/j.pain.0000000000002172
8. Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain. 2012;153(9):1798–1806. doi:10.1016/j.pain.2012.03.026
9. Palermo TM, Walco GA, Paladhi UR, et al. Core outcome set for pediatric chronic pain clinical trials: results from a Delphi poll and consensus meeting. PAIN. 2021;162(10):2539–2547. doi:10.1097/j.pain.0000000000002241
10. McGrath PJ, Walco GA, Turk DC, et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: pedIMMPACT recommendations. J Pain. 2008;9(9):771–783. doi:10.1016/j.jpain.2008.04.007
11. Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Hauser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397(10289):2098–2110.
12. Ocay DD, Larche CL, Betinjane N, et al. Phenotyping chronic musculoskeletal pain in male and female adolescents: psychosocial profiles, somatosensory profiles and pain modulatory profiles. J Pain Res. 2022;15:591–612. doi:10.2147/jpr.S352607
13. Bruneau A, Ferland CE, Pérez-Medina-Carballo R, et al. Association between the use of quantitative sensory testing and conditioned pain modulation and the prescription of medication and interventional procedures in children with chronic pain conditions. Children. 2022;9(8):1157. doi:10.3390/children9081157
14. Bruneau A, Carrié S, Moscaritolo L, Ingelmo P. Mechanism-based pharmacological treatment for chronic non-cancer pain in adolescents: current approaches and future directions. Paediatr Drugs. 2022;24(6):573–583. doi:10.1007/s40272-022-00534-x
15. Vega E, Rivera G, Echevarria GC, Prylutskyy Z, Perez J, Ingelmo P. Interventional procedures in children and adolescents with chronic non-cancer pain as part of a multidisciplinary pain treatment program. Paediatr Anaesth. 2018;28(11):999–1006. doi:10.1111/pan.13494
16. Vega E, Beaulieu Y, Gauvin R, et al. Chronic non-cancer pain in children: we have a problem, but also solutions. Minerva Anestesiol. 2018;84(9):1081–1092. doi:10.23736/s0375-9393.18.12367-4
17. Eccleston C, Fisher E, Cooper TE, et al. Pharmacological interventions for chronic pain in children: an overview of systematic reviews. Pain. 2019;160(8):1698–1707. doi:10.1097/j.pain.0000000000001609
18. Fisher E, Villanueva G, Henschke N, et al. Efficacy and safety of pharmacological, physical, and psychological interventions for the management of chronic pain in children: a WHO systematic review and meta-analysis. Pain. 2022;163(1):e1–e19. doi:10.1097/j.pain.0000000000002297
19. Ferland CE, Villemure C, Michon PE, et al. Multi-center assessment of quantitative sensory testing (qst) for the detection of neuropathic-like pain responses using the topical capsaicin model. Can J Pain. 2018;2:266–279. doi:10.1080/24740527.2018.1525682
20. Blankenburg M, Boekens H, Hechler T, et al. Reference values for quantitative sensory testing in children and adolescents: developmental and gender differences of somatosensory perception. Pain. 2010;149(1):76–88. doi:10.1016/j.pain.2010.01.011
21. Tousignant-Laflamme Y, Page S, Goffaux P, Marchand S. An experimental model to measure excitatory and inhibitory pain mechanisms in humans. Brain Res. 2008;1230:73–79. doi:10.1016/j.brainres.2008.06.120
22. Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16(1):39–58. doi:10.1093/jpepsy/16.1.39
23. Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther. 2000;38(8):835–855. doi:10.1016/S0005-7967(99)00130-8
24. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
25. Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114(1–2):29–36. doi:10.1016/j.pain.2004.12.010
26. Crombez G, Bijttebier P, Eccleston C, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104(3):639–646. doi:10.1016/S0304-3959(03)00121-0
27. Williams AR, Piamjariyakul U, Williams PD, Bruggeman SK, Cabanela RL. Validity of the revised impact on family (IOF) scale. J Pediatr. 2006;149(2):257–261. doi:10.1016/j.jpeds.2006.04.003
28. Stein RE, Riessman CK. The development of an impact-on-family scale: preliminary findings. Med Care. 1980;18(4):465–472. doi:10.1097/00005650-198004000-00010
29. Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–263. doi:10.1016/j.pain.2006.02.035
30. Farrar JT, Young JP
31. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi:10.1016/j.jpain.2007.09.005
32. Vollert J, Maier C, Attal N, et al. Stratifying patients with peripheral neuropathic pain based on sensory profiles: algorithm and sample size recommendations. Pain. 2017;158(8):1446–1455. doi:10.1097/j.pain.0000000000000935
33. Baron R, Maier C, Attal N, et al. Peripheral neuropathic pain: a mechanism-related organizing principle based on sensory profiles. Pain. 2017;158(2):261–272. doi:10.1097/j.pain.0000000000000753
34. De Blasiis P, de Sena G, Signoriello E, Sirico F, Imamura M, Lus G. Nociplastic pain in multiple sclerosis spasticity: dermatomal evaluation, treatment with intradermal saline injection and outcomes assessed by 3D gait analysis: review and a case report. Int J Environ Res Public Health. 2022;19(13):7872. doi:10.3390/ijerph19137872
35. Miyamoto S, Iida S, Miyashita T, et al. Mechanism of chronic pain of symptomatic hip osteoarthritis by association of its distribution, nociceptive, neuropathic, nociplastic, or mixed-pain screening, and the prevalence of lumbar spinal stenosis: a cross-sectional study. Clin J Pain. 2021;38(2):77–87. doi:10.1097/ajp.0000000000001004
36. Kaplan CM, Schrepf A, Mawla I, et al. Neurobiological antecedents of multisite pain in children. Pain. 2022;163(4):e596–e603. doi:10.1097/j.pain.0000000000002431
37. Foxen-Craft E, Bourchtein E, Kaplan C, Clauw DJ, Scott E. Pain widespreadedness, and not primary pain location, is associated with comorbid symptoms in children with chronic pain. Clin J Pain. 2023;39(1):1–7. doi:10.1097/ajp.0000000000001083
38. Levy RL. Exploring the intergenerational transmission of illness behavior: from observations to experimental intervention. Ann Behav Med. 2011;41(2):174–182. doi:10.1007/s12160-010-9254-9
39. Ferro Moura Franco K, Lenoir D, Dos Santos Franco YR, Jandre Reis FJ, Nunes Cabral CM, Meeus M. Prescription of exercises for the treatment of chronic pain along the continuum of nociplastic pain: a systematic review with meta-analysis. Eur J Pain. 2021;25(1):51–70. doi:10.1002/ejp.1666
40. Larkin TE, Kaplan CM, Schrepf A, et al. Altered network architecture of functional brain communities in chronic nociplastic pain. NeuroImage. 2021;226:117504. doi:10.1016/j.neuroimage.2020.117504
41. Eccleston C, Fisher E, Howard RF, et al. Delivering transformative action in paediatric pain: a lancet child & adolescent health commission. Lancet Child Adolesc Health. 2021;5(1):47–87. doi:10.1016/S2352-4642(20)30277-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.