Back to Journals » International Journal of General Medicine » Volume 15
The Predictive Value of Combining Symptoms, Residual Syntax Score and Non-Invasive Tests in the Diagnosis of Significant Coronary Artery Disease in Elderly Post-PCI Patients
Authors Zhang J, Li Y , Zheng B, Qiu J, Chen X, Zhou W, Fan Y, Liu M
Received 12 January 2022
Accepted for publication 12 April 2022
Published 3 May 2022 Volume 2022:15 Pages 4603—4612
DOI https://doi.org/10.2147/IJGM.S357996
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jing Zhang,1,* Yuxi Li,2,* Bo Zheng,2 Jianxing Qiu,3 Xiahuan Chen,1 Weiwei Zhou,1 Yan Fan,1 Meilin Liu1
1Department of Geriatrics, Peking University First Hospital, Beijing, 100034, People’s Republic of China; 2Department of Cardiology, Institute of Cardiovascular Disease, Peking University First Hospital, Beijing, 100034, People’s Republic of China; 3Department of Radiology, Peking University First Hospital, Beijing, 100034, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Meilin Liu, Department of Geriatrics, Peking University First Hospital, No. 8 Xishiku Street, Xicheng District, Beijing, 100034, People’s Republic of China, Tel +86-010-83572022, Email [email protected]
Purpose: To assess the diagnostic efficiency of a combination of symptoms, residual Syntax score (rSS) and non-invasive tests in elderly post-PCI patients.
Patients and Methods: This was a retrospective study that consecutively enrolled patients ≥ 60 years old with chronic coronary syndrome and previous stent implantation without lesions requiring further revascularization between March 2013 and June 2020. The patients were scheduled for exercise ECG, CCTA and invasive coronary angiography within 4 weeks. The study then calculated rSS and the sensitivity, specificity, positive and negative predictive values (PPV and NPV) and accuracy of symptoms, rSS, exercise ECG and CCTA, taking computational pressure-flow dynamics derived fractional flow reserve (caFFR) as the standard reference.
Results: A total of 114 patients were enrolled in this study, including 75 patients with caFFR-positive and 39 patients with caFFR-negative. The caFFR-positive group had more patients with typical angina. Furthermore, the rSS in the caFFR-positive group was higher than that in the caFFR-negative category (7.33 ± 6.56 vs 3.34 ± 4.26, p < 0.001). There was no significant difference in exercise ECG results between the two groups. However, the rate of positive CCTA in the caFFR-positive group was higher than that in the caFFR-negative category (89.33% vs 46.15%, p < 0.001). In addition, after combining symptoms, rSS and CCTA, the sensitivity, specificity, PPV, NPV and accuracy for diagnose were 77.5%, 84.2%, 90.2%, 66.7% and 79.8%, respectively.
Conclusion: The findings showed that exercise ECG had limited power to diagnose significant CAD in elderly post-PCI patients, but CCTA was more efficient. Moreover, combining symptoms, rSS and CCTA provided more accurate diagnostic performance with feasibility and safety.
Keywords: coronary CT angiography, residual syntax score, exercise ECG, percutaneous coronary intervention, elderly
Introduction
There has been a dramatic increase in percutaneous coronary interventions (PCIs) from 2009 to 2018, reaching up to 915, 256 cases in China as at 2018.1 Thus, assessing in-stent restenosis or progression of non-culprit lesions after PCIs becomes a major challenge in contemporary cardiology.2 The Fractional Flow Reserve (FFR) is a Class IA guide for decisions on whether to revascularize coronary stenosis; however, it is an invasive test associated with a small but not negligible proportion of complications, especially among the elderly.3,4 Therefore, selecting appropriate non-invasive methods is recommended to establish the diagnosis, assess the event risk and develop optimal intervention strategies. It has been proposed that a combination of the residual Syntax score (rSS) and clinical factors could predict clinically indicated revascularization.5 Additionally, the functional and anatomic tests such as exercise electrocardiogram (ECG) and coronary computed tomography angiography (CCTA) are broadly available because of their relatively low technical as well as personnel requirements and are also safe to the elderly. Nonetheless, to the best of our knowledge, the diagnostic performance of a combination of symptoms, rSS and these two tests is yet to be examined in elderly post-PCI patients in China.
Consequently, the present study sought to assess the diagnostic efficiency of a combination of symptoms, rSS, exercise ECG and CCTA in elderly post-PCI patients. Given that FFR has hardly been used over the past few years, the present retrospective study employed computational pressure-flow dynamics derived FFR (caFFR) as the standard reference. Notably, caFFR was demonstrated to have an overall diagnostic accuracy of 95.7%, compared to the invasive FFR.6
Methods
Study Population
This was a retrospective study that consecutively enrolled patients ≥60 years old with chronic coronary syndrome and previous stent implantation without lesions requiring further revascularization, between March 2013 and June 2020. The patients had been scheduled to undergo exercise ECG, CCTA and Invasive Coronary Angiography (ICA) within 4 weeks at the Peking University First Hospital. In addition, all the patients underwent ICA because of the high event risk revealed by the symptoms, exercise ECG or CCTA. Moreover, all the patients provided written informed consent before undergoing CCTA and ICA. The reporting of this study conformed to the STARD statement.7
Clinical History
The clinical history of patients was obtained from the electronic medical record system and the following cardiac risk factors were recorded in all the patients: 1) hypertension (blood pressure ≥140/90 mmHg or use of antihypertensive agents); 2) diabetes mellitus (fasting glucose level >7.0mmol/L or the need for insulin or oral antidiabetic drugs); 3) smoking (never, currently or previously); 4) alcohol use (never, currently or previously); 5) history of coronary artery disease (CAD) in first-degree relatives; 6) the body mass index (BMI), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), serum creatinine (Scr), uric acid and HbA1c, LDL-C target achievement was defined as LDL-C ≤1.8mmol/L; 7) left ventricular ejection fraction (LVEF), which was calculated by using Simpson method8; 8) antithrombotic regimen on admission; 9) number of stents and vessels involved; 10) the residual SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score (rSS), which was calculated based on the remaining obstructive coronary disease after treatment with PCI by a dedicated interventional cardiologist who was blinded to the clinical data. Additionally, each coronary lesion resulting to ≥50% stenosis in vessels ≥1.5 mm by visual estimation was scored separately then added to give the rSS.9,10 11) The symptoms were obtained from the medical records of patients and divided into typical or atypical angina, non-anginal chest pain and asymptomatic.3
Exercise ECG Analysis
Each patient took a submaximal exercise test and was defined as “reach target” when a maximal heart rate of ≥85% of the value of 220 – age (in years) was achieved. In addition, the stress test response was considered positive in the event of 1) typical angina during exercise; 2) horizontal or downsloping ST-segment depression ≥0.1mV, measured at 80 or 60ms after the J-point during exercise or recovery persisting for 2 minutes or longer; or 3) upsloping ST-segment depression of 0.15 mV at 80ms after the J-point. On the other hand, the stress test response was suspected to be positive in the event of 1) horizontal or downsloping ST-segment depression ≥0.05mV but <0.1mV or persisting for less than 2 minutes; 2) Severe arrhythmia (including multifocal premature beats, ventricular tachycardia, atrioventricular block, atrial fibrillation and atrial flutter); or 3) a decrease in systolic blood pressure by 10 mmHg or more with exercise.11
The CCTA Scan Protocol, Image Reconstruction and Analysis
All the CT datasets were obtained using a second-generation dual-source CT scanner (SOMATOM Definition Flash, Siemens, Munich, Germany). Additionally, a prospectively ECG-triggered sequential mode was used for all the patients. The contrast agent (370 mg of iodine/mL, Iopromide Injection) was intravenously injected through the antecubital vein at a flow rate of 5.0 mL/s and the volume was determined by the patient’s weight (0.8–1.0×body weight/kg). After the contrast injection, the patients were injected with 30 mL of saline solution. The following parameters were used for CCTA: Slice acquisition = 128 mm × 0.6 mm, rotation time = 0.28 s, pitch = 3.2. Moreover, the data was reconstructed with a slice thickness of 0.75 at 0.6 mm increments, using a medium-smooth soft-tissue convolution kernel (B26f). The images were then transferred to a commercial workstation for evaluation and were analyzed by two radiologists who were blinded to the history of patients. In addition, CCTA was considered positive if there was an anatomic stenosis ≥50% in the left main or stents, or ≥70% in other major epicardial coronary arteries.
The ICA Plus caFFR Procedure and Analysis
ICA was performed through standard techniques and all the segments were evaluated by two certified interventional cardiologists (Xia-Huan Chen and Mei-Lin Liu). In addition, coronary angiography from multiple views, at the operators’ discretion, was recorded at 15 frames per second. Moreover, offline caFFR was performed by an independent core laboratory (Cardiovascular Imaging Core Laboratory of Peking University First Hospital, Beijing, China) and details of the methodology are highlighted in the FLASH FFR study.6 Furthermore, aortic pressure was replaced by mean arterial pressure calculated from the blood pressure during ICA and a caFFR value of 0.80 or less was defined as caFFR-positive.
Statistical Analysis
Data were presented as the mean ± Standard Deviation (SD) or the median (interquartile) for continuous variables and as frequencies or percentages for categorical variables. Additionally, the Mann–Whitney and Chi-square tests were used to examine the statistical differences between the means and proportions of the two groups. Moreover, the sensitivity, specificity, positive and negative predictive values (PPV and NPV), accuracy and the area under the curve (AUC) of the receiver operating characteristic (ROC) curve were calculated to determine the ability of symptoms, rSS and the two non-invasive tests to detect caFFR-positive CAD. All the statistical analyses were conducted using the R (http://www.R-project.org, The R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA) software. A two-sided p value of 0.05 was considered to be statistically significant.
Results
Characteristics of the Study Participants
A total of 114 patients were enrolled in the study. The patients were classified into two groups, namely the caFFR-positive and caFFR-negative groups. The results also showed that 32% of patients in the caFFR-positive group had In-stent Restenosis (ISR), 46.7% had progression in other vessels and 21.3% had both. The clinical characteristics of the patients are shown in Table 1 and the average age in each group was more than 70 years. The results revealed no significant differences in age, sex, BMI, hypertension, diabetes mellitus, HbA1c, Scr, uric acid, TG, LDL-C, LDL-C target achievements, LVEF, the percentage of patients using DAPT, smoking, drinking and family history of CAD between the two groups. In patients treated with DAPT, three patients in each group took aspirin and ticagrelor on admission, while others took aspirin and clopidogrel. In the 41 patients with diabetes mellitus, 7 patients adopted lifestyle interventions, 4 patients took metformin alone, other patients added acarbose, sulfonylureas, dipeptidyl-peptidase IV (DPP-4) inhibitors, repaglinide, pioglitazone or insulin to metformin, sodium-glucose co-transporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RA) had not been used yet. In addition, there were more stents and involved vessels in the caFFR-positive group although there was no significant difference between the two categories.
 |
Table 1 Baseline Characteristics of the Study Participants |
Diagnostic Value of the Symptoms, rSS, Exercise ECG and CCTA
The caFFR-positive group had more patients with typical angina although nearly half of the patients in both categories had non-anginal chest pain or were asymptomatic. Moreover, the rSS in the caFFR-positive group was significantly higher than that of the caFFR-negative category (Table 2).
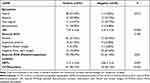 |
Table 2 The Symptoms, rSS, Exercise ECG and CCTA of the Study Participants |
In this study, no serious cardiac events were induced by exercise ECG and no contrast-induced nephropathy was observed after CCTA. Forty-one patients had reached the target heart rate, and 87 patients had reached 80% of the target heart rate while taking exercise ECG. The findings revealed that there was no significant difference in exercise ECG between the two groups. However, the rate of positive CCTA was higher in the caFFR-positive group than that in the caFFR-negative category (89.33% vs 46.15%, p<0.001) (Table 2).
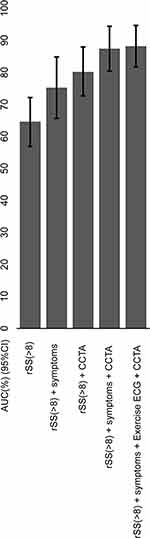
In addition, the sensitivity, specificity, PPV, NPV, accuracy and AUC of symptoms, exercise ECG, CCTA, symptoms and exercise ECG, symptoms and CCTA, exercise ECG and CCTA as well as symptoms, exercise ECG and CCTA are shown in Table 3. Moreover, the ROC for symptoms, exercise ECG and CCTA are shown in Figure 1. In addition, the sensitivity, specificity, PPV, NPV, accuracy and AUC of rSS (>8), and the combinations of rSS (>8) with symptoms, exercise ECG, CCTA are shown in Table 4 and Figure 2. Notably, the sensitivity, specificity, PPV, NPV, accuracy and AUC were 77.5%, 84.2%, 90.2%, 66.7%, 79.8% and 87.3% respectively after combining symptoms, rSS and CCTA.
 |
Table 3 Summary of the Diagnostic Parameters for Symptoms, Exercise ECG and CCTA |
 |
Table 4 Summary of Diagnostic Parameters for rSS, Symptoms, Exercise ECG and CCTA |
Discussion
The main findings from this study can be summarized as follows: 1) The caFFR-positive group had more patients with typical angina. 2) The rSS in the caFFR-positive group was significantly higher than that in the caFFR-negative category. 3) There was no significant difference in exercise ECG between the two groups, the value of exercise ECG was limited and the diagnostic efficiency was low. 4) CCTA was more efficient in giving the correct diagnosis. Although CCTA was an anatomical method of examination, it had high sensitivity and PPV (89.3% and 78.8%) in elderly patients after PCI. However, it had a specificity of only 53.9%, and 46.15% of the patients in the caFFR-negative group were CCTA-positive. 5) Combining symptoms, rSS and CCTA could significantly increase the specificity, PPV and accuracy with feasibility and safety.
Notably, symptoms are unreliable predictors of ischemia after PCI, and silent myocardial ischemia is fairly common. Moreover, elderly patients often present with atypical symptoms, which may delay proper diagnosis.3 In the present study, although the caFFR-positive group had more patients with typical angina, nearly half of the patients in both categories had non-anginal chest pain or were asymptomatic. There were no significant differences in comorbidities, blood glucose, lipid, uric acid and antithrombotic regimen between the two groups. New antilipemic and antiglycemic agents might impact on the results in follow-up studies.12,13
Exercise ECG has low technical and personnel requirements and is widely used in China although it has an inferior diagnostic performance compared to other non-invasive tests.14 It was previously reported that the sensitivity, specificity, PPV, NPV and accuracy of exercise ECG in detecting restenosis were 54% (24–93%), 70% (31–100%), 64% (42–100%), 61% (28–95%) and 62%, respectively. This wide fluctuation may have been caused by the heterogeneity of the study groups, distinct angiographic definitions, different types of medication and timing of evaluation.15 The present study similarly showed that exercise ECG had limited power to diagnose significant CAD in elderly patients, post PCI. On the other hand, CCTA can accurately rule out both anatomically and functionally significant CAD and is mostly preferred as it is associated with a high likelihood of good image quality.3 In patients with stents, the accuracy of CCTA is frequently impaired by blooming artifacts and incomplete evaluation of native vessels. Additionally, the overlap of stent struts can further interfere with image quality in patients with multiple stents.16 However, recent technological advancements have improved spatial resolution and allowed for improved diagnostic accuracy.17–19 For instance, Li et al reported that the third-generation dual-source CCTA enables accurate diagnosis of coronary ISR in both large and small calibre stents. Notably, the study reported that the diagnostic accuracy, sensitivity, specificity, PPV and NPV were all above 95% in the large calibre stent group and the numbers were slightly lower in the small calibre stent category.17 In the present study, the sensitivity, specificity, PPV, NPV and accuracy of CCTA were lower than those previously reported, probably due to lower spatial resolution, more stents, more vessels involved and more severe calcification.
It is noteworthy that patients previously treated with stents often have a high atherosclerotic burden of non-stented coronary segments.20,21 Therefore, rSS was developed to quantitatively assess the degree and complexity of residual stenosis and a rSS value >8 is associated with progressively increasing adverse long-term clinical outcomes.9,22 Additionally, Kashiwagi et al proposed that a combination of the anatomical residual disease, calculated by rSS and clinical factors, could predict clinically indicated revascularization.5 Furthermore, the present study showed that rSS was significantly higher in the caFFR-positive group and a combination of symptoms, rSS and CCTA could improve the diagnostic sensitivity and accuracy of myocardial ischemia. Clinical SYNTAX score has been confirmed to be an independent prognostic factor for patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock. Since clinical parameters such as creatinine clearance and ejection fraction play a role in clinical SYNTAX score.23–25 However, there were on significant differences in Scr and LVEF between the two groups in patients with chronic coronary syndrome in this study. So rSS is more effective to add to symptoms and CCTA in these patients.
In addition to the sensitivity, specificity and accuracy of the non-invasive tests, low technical requirements, site restrictions and safety of the elderly should also be considered in China. It has been proved that the sensitivity, specificity, PPV, NPV and accuracy of nuclear myocardial perfusion imaging and adenosine-stress myocardial perfusion assessed through CT are obviously superior to exercise ECG and CCTA.26–28 However, the risks of the pharmacological stress test, nuclear radiation and the fact that the third-generation dual-source CCTA is not available in most hospitals limit the application of these highly effective methods. Therefore, combining rSS with symptoms and CCTA which are simple and practicable may be highly beneficial in clinical practice.
Given that this was a retrospective study, there are several limitations that deserve to be mentioned. First, clinical data was obtained from the medical records of patients, which may have influenced the accuracy of symptoms. Second, exercise ECG and CCTA were conducted by attending physicians, except for patients with contraindications, the symptomatic patients with a high-risk clinical profile had taken ICA directly instead of CCTA, which may decrease the sensitivity and specificity of exercise ECG and CCTA (Details highlighted in Supplementary Figure 1 and Supplementary Table 1). Third, our study had a limited sample size, and only a few patients were included in each subgroup, yielding limited statistical power. These should be considered and included in future studies.
Conclusion
The findings showed that exercise ECG had limited power to diagnose significant CAD in elderly post-PCI patients, but CCTA was more efficient. Moreover, combining symptoms, rSS and CCTA provided more accurate diagnostic performance with feasibility and safety.
Data Sharing Statement
The data generated or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee of Peking University First Hospital and approval number is 2020 scientific research 379. Informed consent of this study has been granted an exemption by this committee because all information was collected from the medical record system and is maintained with confidentiality. This is a retrospective study and there is no need to collect additional blood samples, schedule extra inspections, conduct further medical interventions or to follow-up.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Scientific Research Seed Fund of Peking University First Hospital (grant number: 2020SF38).
Disclosure
The authors report no conflicts of interest to declare.
References
1. The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on cardiovascular health and diseases in China 2019: an updated summary. Chin Circulation J. 2020;35(9):833–854.
2. Crea F, Bairey Merz CN, Beltrame JF, et al. Mechanisms and diagnostic evaluation of persistent or recurrent angina following percutaneous coronary revascularization. Eur Heart J. 2019;40(29):2455–2462. doi:10.1093/eurheartj/ehy857
3. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi:10.1093/eurheartj/ehz425
4. Windecker S, Kolh P, Kolh P, et al.; Authors/Task Force Members. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–2619. doi:10.1093/eurheartj/ehu278
5. Kashiwagi D, Ebisawa S, Yui H, et al. Prognostic usefulness of residual SYNTAX score combined with clinical factors for patients with acute coronary syndrome who underwent percutaneous coronary intervention from the SHINANO registry. Heart Vessels. 2021;36(2):170–179. doi:10.1007/s00380-020-01680-3
6. Li J, Gong Y, Wang W, et al. Accuracy of computational pressure-fluid dynamics applied to coronary angiography to derive fractional flow reserve: FLASH FFR. Cardiovasc Res. 2020;116(7):1349–1356. doi:10.1093/cvr/cvz289
7. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527. doi:10.1136/bmj.h5527
8. Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2(5):358–367. doi:10.1016/S0894-7317(89)80014-8
9. Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128(2):141–151. doi:10.1161/CIRCULATIONAHA.113.001803
10. Serruys PW, Onuma Y, Garg S, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5(1):50–56. doi:10.4244/EIJV5I1A9
11. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA guidelines for exercise testing. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997;30(1):260–311. doi:10.1016/s0735-1097(97)00150-2
12. Scicchitano P, Milo M, Mallamaci R, et al. Inclisiran in lipid management: a literature overview and future perspectives. Biomed Pharmacother. 2021;143:112227. doi:10.1016/j.biopha.2021.112227
13. Marx N, Davies MJ, Grant PJ, et al. Guideline recommendations and the positioning of newer drugs in type 2 diabetes care. Lancet Diabetes Endocrinol. 2021;9(1):46–52. doi:10.1016/S2213-8587(20)30343-0
14. Section of Interventional Cardiology of Chinese Society of Cardiology, Section of Atherosclerosis and Coronary Artery Disease of Chinese Society of Cardiology, Specialty Committee on Prevention and Treatment of Thrombosis of Chinese College of Cardiovascular Physicians. Guideline on the diagnosis and treatment of stable coronary artery disease. Zhonghua Xin Xue Guan Bing Za Zhi. 2018;46:680–694. doi:10.3760/cma.j.issn.0253-3758.2018.09.004
15. Dori G, Denekamp Y, Fishman S, Bitterman H. Exercise stress testing, myocardial perfusion imaging and stress echocardiography for detecting restenosis after successful percutaneous transluminal coronary angioplasty: a review of performance. J Intern Med. 2003;253(3):253–262. doi:10.1046/j.1365-2796.2003.01101.x
16. Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8(5):342–358. doi:10.1016/j.jcct.2014.07.003
17. Li Y, Yu M, Li W, Lu Z, Wei M, Zhang J. Third generation dual-source CT enables accurate diagnosis of coronary restenosis in all size stents with low radiation dose and preserved image quality. Eur Radiol. 2018;28(6):2647–2654. doi:10.1007/s00330-017-5256-3
18. Eckert J, Renczes-Janetzko P, Schmidt M, Magedanz A, Voigtlander T, Schmermund A. Coronary CT angiography (CCTA) using third-generation dual-source CT for ruling out in-stent restenosis. Clin Res Cardiol. 2019;108(4):402–410. doi:10.1007/s00392-018-1369-1
19. Yang X, Yu Q, Dong W, et al. Performance of dual-source CT with high pitch spiral mode for coronary stent patency compared with invasive coronary angiography. J Geriatr Cardiol. 2016;13(10):817–823. doi:10.11909/j.issn.1671-5411.2016.10.002
20. Taniwaki M, Windecker S, Zaugg S, et al. The association between in-stent neoatherosclerosis and native coronary artery disease progression: a long-term angiographic and optical coherence tomography cohort study. Eur Heart J. 2015;36(32):2167–2176. doi:10.1093/eurheartj/ehv227
21. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. doi:10.1093/eurheartj/ehy394
22. Genereux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol. 2012;59(24):2165–2174. doi:10.1016/j.jacc.2012.03.010
23. Hayiroglu MI, Bozbeyoglu E, Yildirimturk O, Tekkesin AI, Pehlivanoglu S. Effect of acute kidney injury on long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock who underwent primary percutaneous coronary intervention in a high-volume tertiary center. Turk Kardiyol Dern Ars. 2020;48(1):1–9. doi:10.5543/tkda.2019.84401
24. Cinar T, Hayiroglu MI, Seker M, et al. The predictive value of age, creatinine, ejection fraction score for in-hospital mortality in patients with cardiogenic shock. Coron Artery Dis. 2019;30(8):569–574. doi:10.1097/MCA.0000000000000776
25. Hayiroglu MI, Keskin M, Uzun AO, et al. Predictive value of SYNTAX score II for clinical outcomes in cardiogenic shock underwent primary percutaneous coronary intervention; a pilot study. Int J Cardiovasc Imaging. 2018;34(3):329–336. doi:10.1007/s10554-017-1241-9
26. Andreini D, Mushtaq S, Pontone G, et al. CT perfusion versus coronary CT angiography in patients with suspected in-stent restenosis or CAD progression. JACC Cardiovasc Imaging. 2020;13(3):732–742. doi:10.1016/j.jcmg.2019.05.031
27. Pontone G, Guaricci AI, Palmer SC, et al. Diagnostic performance of non-invasive imaging for stable coronary artery disease: a meta-analysis. Int J Cardiol. 2020;300:276–281. doi:10.1016/j.ijcard.2019.10.046
28. Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J. 2018;39(35):3322–3330. doi:10.1093/eurheartj/ehy267
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.