Back to Journals » International Journal of General Medicine » Volume 16
The Learning Curve of Total Arch Replacement via Single Upper Hemisternotomy Approach in Aortic Dissection
Authors Xia L, Liu Y, Yang Z, Ge Y, Wang L, Du Y, Dong Y, Jiang H
Received 28 July 2023
Accepted for publication 8 November 2023
Published 16 November 2023 Volume 2023:16 Pages 5301—5308
DOI https://doi.org/10.2147/IJGM.S426882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Lin Xia,1,* Yu Liu,1,* Zhonglu Yang,1 Yuguang Ge,1 Lu Wang,1 Yejun Du,1 Yinan Dong,2 Hui Jiang1
1Department of Cardiovascular Surgery, General Hospital of Northern Theater Command, Shenyang, Liaoning Province, 110016, People’s Republic of China; 2Department of Thoracic Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang, Liaoning Province, 110016, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hui Jiang, Department of Cardiovascular Surgery, General Hospital of Northern Theater, Command, 83 Wenhua Road, Shenyang, Liaoning Province, 110016, People’s Republic of China, Tel +86-024-2889-7390, Fax +86-024-2889-7391, Email [email protected]
Purpose: Upper hemisternotomy (UHS) has benefits over conventional full sternotomy because it ameliorates trauma during cardiac surgery. Owing to its challenging and technically demanding nature, this incision in acute type A aortic dissection (ATAAD) has rarely been reported. This study aimed to analyze the learning curve of total arch replacement (TAR) with moderate hypothermic circulatory arrest via a single UHS approach, which is necessary to guide the training of surgeons in adopting minimally invasive procedures.
Patients and Methods: A total of 202 consecutive patients who were definitively diagnosed with ATAAD between July 2016 and June 2021 were enrolled in this retrospective analysis. Patients were divided into three groups based on cumulative sum plots for circulatory arrest time in chronological order. Perioperative characteristics were compared between the groups.
Results: There was significant difference in the circulatory arrest time and cross-clamp time respectively among three groups (39.0 min vs 28.0 min vs 15.0 min, P < 0.001; 104.5 min vs 106.2 min vs 84.1 min, P < 0.001). The ventilation time and first 24-h chest tube drainage were statistically different among groups (35.5 h vs 24.0 h vs 19.0 h, P = 0.031; 220.0 mL vs 192.5 mL vs 125.5 mL, P = 0.043). No other clinical outcome was observed as significant difference.
Conclusion: A cardiac surgeon can convert a conventional full sternotomy to a single UHS for TAR after experiencing a learning curve, to ensure patient safety. The mastery of this minimally invasive surgical technique may be beneficial for the prognosis of patients with ATAAD.
Keywords: aneurysm, dissecting, cardiac surgical procedures, sternotomy, circulatory arrest, deep hypothermia induced, learning curve
Introduction
Open surgical repair is considered the predominant management for most patients diagnosed with acute type A aortic dissection (ATAAD), a rare and devastating disease with a high mortality rate.1,2 Although the current surgical management strategy has reduced the 30-day mortality for ATAAD to about 10%,3 how to further minimize surgical trauma is arising the attention of cardiac surgeons all over the world.4 Since the first minimally invasive aortic valve was reported,5 several approaches have been used to achieve adequate exposure to conduct supra-cardiac structural procedures reliably and effectively, mainly including right anterolateral thoracotomy and upper hemisternotomy (UHS). These less-invasive approaches benefit from conventional full sternotomy by ameliorating trauma with fewer blood transfusions, incision infections, perioperative pain, and in-hospital stays.6–9 Furthermore, advancements in medical image processing, especially in predicting blood hemodynamics in aortic dissection, have significantly enhanced the planning and execution of minimally invasive surgical approaches.10 We have previously reported our experience and outcomes using a single UHS in patients with ATAAD under moderate hypothermic circulatory arrest.11 However, this surgical procedure is challenging and technically demanding; therefore, the evaluation of its learning curve is necessary to guide the training of surgeons.
The cumulative sum (CUSUM), which can help discern the trend of a dataset intuitively, has proven to be particularly valuable when analyzing the learning curve.12 A learning curve based on the CUSUM method may be helpful in guiding training and allowing implementation of the new surgical technique. The learning curve for emergent total arch replacement (TAR) in ATAAD was established based on the above analytical method.13 To the best of our knowledge, this is the first study on the required learning curve for TAR combined with frozen elephant trunk (FET) implantation via a single UHS approach in ATAAD. Additionally, this is by far the largest-scale and single-center study that retrospectively analyzed the perioperative indicators of the challenging procedure.
Materials and Methods
Study Population
A total of 261 patients diagnosed with ATAAD were assessed from July 2016 to June 2021, out of which 202 consecutive patients confirmed through computed tomographic arteriography (CTA) were enrolled in this retrospective study. All surgeries were performed by the same surgeon, anesthetist, perfusionist, and nurse. Fifty-nine patients were excluded based on our exclusion criteria, which encompassed neurological complications (N = 14), abdominal complications such as acute hepatic failure, gastrointestinal bleeding, and acute renal failure (N = 21), and concomitant operations that required full sternotomy, such as coronary heart disease, mitral valve disease, and congenital heart disease (N = 24). Bilateral selective antegrade cerebral perfusion (bSACP) was then performed. All procedures adhered to the Declaration of Helsinki and the standards of the Ethics Committee of the General Hospital of the Northern Theater Command, Shenyang City, China (k-2020-19), ensuring patient rights, integrity, and confidentiality. Informed consent was obtained from all the patients.
Surgical Procedure
The surgery was performed as previously described.11 Briefly, an incision was made from the sternal notch to the level of the fourth intercostal space and then extended to the right fourth intercostal space. Cardiopulmonary bypass (CPB) was established by cannulation of the direct innominate artery (right subclavian artery or right or left carotid artery) via arterial cannulation, with direct right atrial cannulation as venous cannulation. A left ventricular vent was placed through the right superior pulmonary vein. Antegrade cardioplegia was delivered through the aortic root or the coronary orifice after aortotomy. Moderate hypothermic circulatory arrest was instituted if the nasopharyngeal temperature was <28°C. Aortic root procedures were done (if indicated), during cooling. The proximal ends of the left subclavian, left common carotid, and innominate arteries were closed with Hem-o-lok ligation clips. The bSACP was started through arterial cannulation and a 15Fr femoral arterial cannula was placed into the distal end of the right or left common carotid artery after the innominate artery was cross-clamped, and the brain was perfused with the cardioplegia pump. Near-infrared spectroscopy (NIRS) has also been used for cerebral protection. Circulatory arrest was induced after occlusion of the innominate artery and FET implantation was performed. In the FET technique, a stent graft (MicroPort Medical Co., Ltd., Shanghai, China) was inserted into the true lumen of the distal aorta in a compressed state after the distal aorta was usually transected between the origin of the innominate artery and the left carotid artery (Zone 1). The distal aorta incorporating the stent graft was firmly attached to the distal end of the 4-branch prosthetic graft (Vascutek Ltd., Terumo Aortic, Inchinnan, Scotland, UK) using the open aortic procedure. After anastomosis was completed, blood perfusion of the lower body was started through the perfusion limb of the 4-branch prosthetic graft. The prosthetic graft was sequentially anastomosed to the left common carotid artery, proximal aortic stump, left subclavian artery, and innominate artery (to decrease SACP and cross-clamp times). After anastomosis to the left common carotid artery was accomplished, bSACP was discontinued, cardiopulmonary bypass gradually returned to normal flow, and rewarming was started.
Learning Curve-CUSUM
In our analysis of the learning curve using CUSUM plots, we focused on circulatory arrest time as the primary parameter for assessing proficiency in ATAAD surgery with TAR combined with FET implantation via a single UHS approach. The circulatory arrest time was selected due to its critical importance in determining the complexity and success of the surgical procedure. The mean circulatory arrest time from the 1st to the 202nd patient was determined as the reference value. Each data point was then compared against this reference, and the cumulative sum of these differences was plotted to assess the learning curve. We calculated each CUSUM in chronological order and analyzed circulatory arrest time by visually inspecting the plots. When two inflection points were observed in the CUSUM plot (71th and 137th patient), the first 70 patients were assigned to the Initial Stage Group (early experience group), the following 66 patients were assigned to the Platform Stage Group (middle experience group), and the last 66 patients were assigned to the Mastery Stage Group (late experience group). Demographic and clinical outcomes were compared between the three groups. For verification purposes, additional parameters such as cross-clamp and CPB times were also considered. These parameters were analyzed using the same CUSUM methodology to provide a comprehensive understanding of the learning process and to validate the results obtained from the circulatory arrest time analysis.
Statistical Analyses
Data were collected retrospectively and analyzed using SPSS Version 25.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are described as mean ± standard deviation or median (interquartile range, IQR) for continuous variables and frequency (%) for categorical variables. The chi-square test or Fisher’s exact probability test was used to compare the distribution of categorical variables between the groups. Continuous variables were analyzed using one-way analysis of variance with post-hoc Bonferroni test, Welch test with post-hoc Games–Howell test, or Kruskal–Wallis H-test with all pairwise multiple comparisons. A 2-sided P-value of less than 0.05 was considered to indicate a significant difference.
Results
Learning Curve
We drew CUSUM plots based on circulatory arrest time and calculated the fitting polynomial function: y = −3.17E-05x3-0.084x2+18.328x-80.29, R² = 0.985, P < 0.001. By visually inspecting the CUSUM plots, two inflection points for circulatory arrest time were observed at the 71th case and 137th case (Figure 1). The enrolled patients were divided into three groups according to chronological order: the Initial Stage Group consisted of the first 70 patients, the Platform Stage Group consisted of the middle 66 cases, and the Mastery Stage Group consisted of the last 66 cases. CUSUM plots of the cross-clamp and CPB times were also drawn according to the above method (Supplementary Figures 1 and 2).
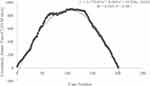 |
Figure 1 CUSUM plots of circulatory arrest time (Red point refers to 71th and 137th case). Abbreviation: CUSUM, Cumulative summation. |
Preoperative Characteristics
In this study, 202 patients in the surgical group underwent TAR combined with FET implantation for ATAAD. The case series comprised 148 men (73.3%) and 54 women (26.7%) with a mean of age was 50.3 years, 150 (74.3%) were diagnosed with hypertension, and 8 (4.0%) had diabetes. There were no significant differences in the preoperative variables among the three groups (Table 1).
 |
Table 1 Demographics and History |
Intraoperative Data
In this cohort, emergent operations were quite prevalent, with 173 out of 202 cases (85.6%) being performed under emergency conditions. Although the proportion of emergent operations did not show statistical differences between groups, there was an observed trend of an increasing percentage of emergent surgeries with the progression of surgical expertise. Regarding the conversion rate to full sternotomy, it was relatively low overall, with only 5 cases (2.5%) requiring conversion. There were no significant differences in the conversion rates between groups.
There was significant difference in the median and mean of circulatory arrest time and cross-clamp time respectively among three groups (39.0 min vs 28.0 min vs 15.0 min, P < 0.001; 104.5 min vs 106.2 min vs 84.1 min, P < 0.001). For circulatory arrest time, all pairwise comparisons among groups were statistically significant. However, the median CPB time did not differ significantly between the groups. The median of the minimum nasopharyngeal temperature was 26.9°C in these patients. When conditions were permitted, the innominate artery was selected as the pathway of arterial perfusion in 185 (91.6%) cases, while four (2.0%) had right subclavian arterial perfusion, two (1.0%) had right common carotid arterial perfusion, and 11 (5.4%) had left common carotid arterial perfusion. There were no significant differences in the other intraoperative variables (Table 2).
 |
Table 2 Intraoperative Data |
Postoperative Outcomes
The median intensive care unit (ICU) stay and postoperative hospital stay were not significantly different among the groups. However, there was significant different in ventilation time among groups (35.5 h vs 24.0 h vs 19.0 h, P = 0.031). The subsequent post hoc test demonstrated that the ventilation time in the Mastery Stage Group was significantly shorter than that in the Initial Stage Group. And the median of the first 24-h chest tube drainage among groups was significantly different (220.0 mL vs 192.5 mL vs 125.5 mL, P = 0.043). In-hospital mortality occurred in seven patients in the Initial Stage Group, three in the Platform Stage Group, and three in the Mastery Stage Group. Postoperative adverse events, including reintubation, reoperation for bleeding, stroke, and dialysis, did not differ significantly among the groups (Table 3).
 |
Table 3 Postoperative Outcomes |
Discussion
Aortic arch surgery, particularly ATAAD, is a major challenge in modern cardiac surgery. Undoubtedly, the UHS adds to the difficulty of TAR combined with FET implantation. Our surgical team has made long-term preparations to make this minimally invasive strategy beneficial to patients. First, deep hypothermic circulatory arrest was applied to limit systemic metabolism and provide a bloodless operative field when we started performing TAR for ATAAD. Second, moderate hypothermic circulatory arrest combined with SACP has been proven to be safe and promoted in many cardiac surgery centers,14,15 This technique was also used by our operative team with gradual proficiency of surgical procedures in TAR. As minimal access has been widely practiced and developed in aortic valve surgery,16–18 the aortic valve replacement and the Bentall procedure were performed via the UHS approach, which gave us the opportunity to perform complex aortic root procedures in a limited surgical space. After this arduous exploration, the development of a minimally invasive surgical strategy for ATAAD was attempted. However, large-scale clinical studies investigating minimally invasive techniques are lacking. Our surgical team has conducted several studies on this procedure and achieved encouraging outcomes.11,19 And To the best of our knowledge, the present study is the largest retrospective study to explore TAR with moderate hypothermic circulatory arrest using a single UHS approach. The summary and analysis of the baseline characteristics of patients can help establish the applicable population scope for this procedure, and the description of surgical details and perioperative results can help more accurately evaluate and promote this technique. Although the use of this challenging incision in ATAAD may be complicated and technically demanding, cardiac surgeons can overcome the difficulty of this minimally invasive operation and improve the clinical benefits for patients after experiencing the scientific learning curve.
The CUSUM method is useful for early detection of data trends.12 And It provides a risk-adjusted, quantitative measure of resident learning curves, which is necessary for cardiac surgery trainees.18 We carried out the first TAR combined with FET implantation using a single UHS approach after gaining sufficient experience with conventional full sternotomy. With an increase in the number of surgical cases, both cross-clamp and circular arrest times showed a significant downward trend. However, it is noteworthy that despite these improvements, the total bypass time remained relatively unchanged. This observation can be attributed to several factors: (1) Surgical Prudence: Cross-clamp and circulatory arrest times are highly dependent on surgical maneuvers. Our surgeons, prioritizing patient safety, make decisions regarding CPB arrest only after a comprehensive assessment of perioperative parameters. This cautious approach, while improving specific operative times, may contribute to the constancy of total bypass time. (2) Sample Size Limitations: Our study has a relatively small sample size, which might hinder the ability to exhibit variations in certain statistical outcomes, including total bypass time.
In the present series, CUSUM plots of circulatory arrest time presented inflection points at the 71th case and 137th cases, implying that 70 cases are needed to gain early proficiency in TAR combined with FET implantation via the single UHS approach, and the surgeon’s application of this procedure stabilized after 136 operations. This is the first report on the number of cases in which a surgeon is required to have worked on training and become proficient in this challenging surgical procedure. We summarized the following characteristics based on a comparison of the clinical data among the three groups. First, the incidence of postoperative adverse events (reintubation, reoperation for bleeding, stroke, dialysis, and in-hospital death) was not high even in the initial stage compared to the following period, which further confirms the safety of this procedure. Second, the advantages of minimally invasive aortic surgery will gradually emerge from the initial learning period to the mastery period, such as ventilation time and first 24-h chest tube drainage.
Limitations
Our study had some limitations. First, it was a retrospective study. Second, this study lacked data on long-term clinical outcomes.
Conclusion
A cardiac surgeon can convert a conventional full sternotomy to a single UHS for TAR with moderate hypothermic circulatory arrest after experiencing a learning curve to ensure patient safety. The mastery of this minimally invasive surgical technique is beneficial to the prognosis of patients with ATAAD, and the scope of indications may be the focus of further exploration.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of the General Hospital of the Northern Theater Command, Shenyang City, China (approval number: k-2020-19). Informed consent was obtained from all the patients. All methods were performed in accordance with the relevant guidelines and regulations.
Acknowledgments
The authors thank Qingrong Ni (Department of Dermatology, Air Force Medical Center, Fourth Military Medical University) for her tremendous help with the data analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Science and Technology Foundation of Liaoning Province, guided by the central government in 2023 (grant 2023JH6/100100034), the National Natural Science Foundation of China for Young Scholars (grant 82100513, 82203909), Science and Technology Projects in Shenyang (grant 21-173-9-49), and the Boost Program for Young Doctors of the Air Force Medical Center (grant 21ZT10).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Evangelista A, Isselbacher EM, Bossone E, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018;137(17):1846–1860. doi:10.1161/circulationaha.117.031264
2. Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the international registry of acute aortic dissection. J Am Coll Cardiol. 2015;66(4):350–358. doi:10.1016/j.jacc.2015.05.029
3. Tsai TT, Evangelista A, Nienaber CA, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the international registry of acute aortic dissection (IRAD). Circulation. 2006;114(1 Suppl):I350–6. doi:10.1161/circulationaha.105.000497
4. Appoo JJ. Invited Commentary. Ann Thorac Surg. 2020;109(5):1399–1400. doi:10.1016/j.athoracsur.2019.10.004
5. Rao PN, Kumar AS. Aortic valve replacement through right thoracotomy. Tex Heart Inst J. 1993;20(4):307–308.
6. Gilmanov D, Bevilacqua S, Murzi M, et al. Minimally invasive and conventional aortic valve replacement: a propensity score analysis. Ann Thorac Surg. 2013;96(3):837–843. doi:10.1016/j.athoracsur.2013.04.102
7. Phan K, Xie A, Di Eusanio M, Yan TD. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg. 2014;98(4):1499–1511. doi:10.1016/j.athoracsur.2014.05.060
8. Johnston DR, Atik FA, Rajeswaran J, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg. 2012;144(4):852–858.e3. doi:10.1016/j.jtcvs.2011.12.008
9. Attia RQ, Hickey GL, Grant SW, et al. Minimally invasive versus conventional aortic valve replacement: a propensity-matched study from the UK national data. Innovations. 2016;11(1):15–23. doi:10.1097/imi.0000000000000236
10. Polanczyk A, Piechota-Polanczyk A, Huk I, Neumayer C, Balcer J, Strzelecki M. Computational fluid dynamic technique for assessment of how changing character of blood flow and different value of hct influence blood hemodynamic in dissected aorta. Diagnostics. 2021;11(10). doi:10.3390/diagnostics11101866
11. Jiang H, Liu Y, Yang Z, Ge Y, Li L, Wang H. Total arch replacement via single upper-hemisternotomy approach in patients with type a dissection. Ann Thorac Surg. 2020;109(5):1394–1399. doi:10.1016/j.athoracsur.2019.08.095
12. Wohl H. The cusum plot: its utility in the analysis of clinical data. N Engl J Med. 1977;296(18):1044–1045. doi:10.1056/nejm197705052961806
13. Liu H, Liu S, Zaki A, et al. Quantifying the learning curve of emergent total arch replacement in acute type A aortic dissection. J Thorac Dis. 2020;12(8):4070–4081. doi:10.21037/jtd-20-912
14. Malaisrie SC, Szeto WY, Halas M, et al. The American association for thoracic surgery expert consensus document: surgical treatment of acute type A aortic dissection. J Thorac Cardiovasc Surg. 2021;162(3):735–758.e2. doi:10.1016/j.jtcvs.2021.04.053
15. El-Sayed Ahmad A, Papadopoulos N, Risteski P, Moritz A, Zierer A. The standardized concept of moderate-to-mild (≥28°C) systemic hypothermia during selective antegrade cerebral perfusion for all-comers in aortic arch surgery: single-center experience in 587 consecutive patients over a 15-year period. Ann Thorac Surg. 2017;104(1):49–55. doi:10.1016/j.athoracsur.2016.10.024
16. Gosev I, Yammine M, Leacche M, Ivkovic V, McGurk S, Cohn LH. Reoperative aortic valve replacement through upper hemisternotomy. Ann Cardiothorac Surg. 2015;4(1):88–90. doi:10.3978/j.issn.2225-319X.2014.11.10
17. Kirmani BH, Jones SG, Malaisrie SC, Chung DA, Williams RJ. Limited versus full sternotomy for aortic valve replacement. Cochrane Database Syst Rev. 2017;10(4):Cd011793. doi:10.1002/14651858.CD011793
18. Klein P, Klop IDG, Kloppenburg GLT, van Putte BP. Planning for minimally invasive aortic valve replacement: key steps for patient assessment. Eur J Cardiothorac Surg. 2018;53(suppl_2):ii3–ii8. doi:10.1093/ejcts/ezy086
19. Jiang H, Liu Y, Yang Z, Ge Y, Du Y. Mild hypothermic circulatory arrest with lower body perfusion for total arch replacement via upper hemisternotomy in acute type a dissection. Heart Surg Forum. 2021;24(2):E345–e350. doi:10.1532/hsf.3729
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
