Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
The Impact of Deep Inspiration Breath Hold (DIBH) Implementation on the Hybrid Technique in Left-Sided Whole Breast Irradiation: A Dosimetric Characteristic Study of 3D-CRT Hybrid VMAT in DIBH and Free Breathing Conditions, and VMAT in Free Breathing Conditions
Received 15 August 2023
Accepted for publication 28 September 2023
Published 12 October 2023 Volume 2023:15 Pages 683—693
DOI https://doi.org/10.2147/BCTT.S426903
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Hui-Ling Yeh,1 Jia-Fu Lin2
1Department of Radiation Oncology, Taichung Veterans General Hospital, Taichung, Taiwan; 2Division of Radiation Physics, Department of Radiation Oncology, Taichung Veterans General Hospital, Taichung, Taiwan
Correspondence: Jia-Fu Lin, Division of Radiation Physics, Department of Radiation Oncology, Taichung Veterans General Hospital, No. 1650, Sec. 4, Taiwan Blvd., Xitun District, Taichung, Taiwan, Tel +886-423592525 #5601, Fax +886-423741316, Email [email protected]
Aim: To investigate the impact of DIBH for heart sparing effect on left sided breast postoperative whole breast irradiation by comparing the dosimetric characteristics of 3D-CRT hybrid VMAT and pure VMAT treatment planning under DIBH condition.
Materials and Methods: The primary CT data sets from previously treated left sided early breast cancer were used for pure volumetric arc therapy (VMAT) technique re-planning for the dosimetric characteristics comparison. A treatment plan of 3D-CRT hybrid VMAT technique was re-planned on the free breath (FB) condition for the investigation of the dosimetric characteristics comparison on DIBH condition. The prescribed dose for all the treatment plans was 42.5Gy in 16 fractions. All plans were optimized to cover 100% of the PTV by 95% of prescribed dose. The dosimetric differences among the 3 treatment plans for the 20 patients were analyzed using Wilcoxon signed-rank test, with p value< 0.05 considered statistically significant.
Results: 3D-CRT hybrid VMAT using DIBH technique yielded the best results on the conformity index (CI) and homogeneity index (HI). By comparing this 3D-CRT hybrid VMAT technique using FB and DIBH technique, the mean heart dose (MHD) was reduced from 5.38Gy to 1.65Gy, respectively (p =0.001) and the left anterior descending coronary artery (LAD)0.03cc dose was reduced from 27.87Gy to 9.41Gy, respectively (p =0.001). 3D-CRT hybrid VMAT using DIBH technique significantly reduced the V5, V20 and D mean of the ipsilateral lung and D mean of the contralateral lung. The D5 of right breast was significantly reduced by 3D-CRT hybrid VMAT compared with VMAT using DIBH technique.
Conclusion: The incorporation of DIBH into 3D-CRT hybrid VMAT technique provides the best benefits for the heart and the OAR with respect to the radiation dose-sparing effect without compromising the target conformity and homogeneity in the treatment planning.
Keywords: left sided breast cancer, postoperative radiotherapy, whole breast irradiation, DIBH, hybrid technique, heart dose-sparing
Background
Postoperative whole breast irradiation (WBI) is now the standard therapy for early breast cancer after breast conserving surgery. Local control and overall survival are improved by postoperative WBI in early breast cancer.1 Postoperative radiotherapy could reduce the local recurrence rate by half and avoid one breast cancer death by year 15 for every four recurrences by year 10.2 Since most early breast cancer patients survive for a very long time after proper treatments including ever more effective targeted therapies for those subsequently developing metastatic disease, the long term side effects affecting quality of life should be considered before treatment.3 Secondary lung cancers, radiation lung fibrosis and radiation-induced cardiac disease could occur years later after postoperative radiotherapy.4 The risk of cardiac mortality is complicated by multiple factors, such as smoking habit, comorbidities, total irradiation dose, fraction size, and irradiation volume of the heart. The estimated risk for cardiac mortality was about 1% for smokers and 0.3% for non-smokers in patients receiving modern breast radiotherapy.4 A significant portion of ipsilateral lung volume and the heart were included in the high-dose field when whole breast irradiation was delivered by two tangential beam plus wedges in the two dimension radiotherapy era.5 Sparing radiation dose to the heart is an important issue during postoperative whole breast irradiation, especially for left-sided early breast cancers. The mean heart dose varies from 2Gy to 7Gy in modern treatment planning. The hazards for cardiac disease after postoperative radiotherapy may be greater if the mean heart dose is > 4 Gy.4 A previous report showed that the mean dose to the heart was a predictor for major coronary events. The estimated major coronary events increased with the mean dose to the heart by 7.4% per Gray.6 The conventional tangential beam irradiation for whole breast irradiation has been shown to increase risk of coronary damage.7 Three dimensional conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy (IMRT) was developed to improve the target coverage and sparing of organs at risk.8 More advanced techniques, such as volumetric modulated Arc therapy and Tomotherapy were developed to improve the dosimetric homogeneity of whole breast irradiation.9 Although 3D-CRT, IMRT, VMAT, and Tomotherapy improve the target coverage, the low-dose distribution to organs at risk may be increased.10 In a review study, it was shown that hybrid techniques allowed more conformal delivery of radiation doses to the whole breast with lower high radiation doses delivered to organs at risk (OAR).11 Most hybrid techniques use 2D- or 3D-tangential beam as the base plan. The second plan of hybrid techniques could consist of IMRT field in field or IMRT inverse plan, or VMAT.12 The weighting from the two base tangential beams usually comprises 70% to 80% of the prescribed doses and the remaining 30% to 20% were developed from the dynamic beam, either from IMRT or VMAT.11 Our department developed a different IMRT hybrid VMAT technique to further decrease the low radiation dose distribution area to the OAR in 2015. Our first plan delivers 75% of the prescribed dose from tangential IMRT beam and the remaining 25% of the prescribed dose is provided by two partial arcs of VMAT. The low-dose distribution to the ipsilateral lung V5, V20 was significantly less than the dose planned by fixed 7 fields of IMRT and pure VMAT. A detailed description of the hybrid IMRT and VMAT technique is provided in our previous report.13
To further overcome setup error, organ motion, and the proportion of heart irradiated with high-dose radiation during radiotherapy, respiratory control during radiation dose delivery should be considered in the treatment technique. New technology for respiratory control during radiation delivery may reduce the setup error. Respiratory control can be done by methods, such as respiratory gating, DIBH, aperture adaptive technique, and visual guidance.14,15 Previous studies investigated cardiac dose-sparing by utilizing DIBH and showed promising results in terms of dosimetric characteristics.16,17 Under DIBH technique, a considerable volume of the heart can be spared from the high radiation doses (Figure 1). To investigate whether incorporation of DIBH into the hybrid technique could further reduce cardiac doses, we retrospectively compared the dosimetric characteristics of 3D-conformal radiotherapy (3D-CRT) hybrid volumetric modulated arc therapy (VMAT) technique and pure VMAT treatment planning under DIBH and free breath condition using the CT simulation images and the treatment planning data from our previously treated patients. We also compared the dosimetric characteristics of 3D-CRT hybrid VMAT under DIBH and free breath condition. This study was approved by the Institutional Review Board (II) of Taichung Veterans General Hospital (IRB number: CE21447B). The requirement for informed consent was specifically waived by our ethics committee because this research is a study of dosimetry comparison only and involves no more than minimal risk to the subjects. The abstract of this paper was presented at the ESMO ASIA Congress 2022 as a poster presentation. The poster’s abstract was published in “Poster Abstracts” in the supplements of Annals of Oncology: DOI: https://doi.org/10.1016/j.annonc.2022.10.021.
Materials and Methods
Patient Selection and Structure Delineation
Twenty patients aged from 41 years old to 73 years old, with left-sided breast cancer stage 0-IIA, who underwent breast-conserving surgery and postoperative radiotherapy between Jan, 2021 and July, 2022 were selected in this retrospective study (Table 1). These patients were previously treated with 3D-CRT hybrid VMAT technique under DIBH to the left breast after breast-conserving surgery. Before radiotherapy, the CT images of the patients were collected for radiation dose calculation by CT simulation. Before CT simulation, all patients were immobilized in supine position on a customized vacuum bag with the left arm elevated above the head. A CT scan (CT scanner: GE Optima 580) with a slice thickness of 2.5 mm was acquired from each patient and the image coverage was from the mandible to the upper third liver area, so that the entire lung volume was covered. Our routine CT simulation images included two sets of CT images for patients receiving postoperative radiotherapy under deep-inspiration breath-hold (DIBH) condition, ie, one set of images under deep-inspiration breath-hold (DIBH) and one set of images under free-breathing (FB). Before the CT simulation process all of the patients received instruction on the training process of the breath-hold, and were educated about the procedures and oral commands that they would hear during the acquisition of CT images and the treatment process. We used Varian RPM Respiratory Gating System Version 1.7 for DIBH radiation delivery. The Radiation Therapy Oncology Group (RTOG) delineation guidelines were used as a reference for the target and the OAR contour delineation. The clinical target volume (CTV) for the breast was defined by the superior margin at the clinical reference plus the image below the clavicle head and the inferior margin at the clinical reference plus loss of CT apparent breast. The anterior margin was confined by the skin and the posterior margin was just above the pectoralis muscles, with the lateral margin at the clinical reference plus mid-axillary line and the medial margin at the sternal-rib junction. The CTV for the tumor bed was defined as the lumpectomy cavity (seroma), the fibrous scar tissue, and the area marked by the surgical clips. The normal tissue and OAR, including the lungs, the heart, the LAD, the spinal cord, and the contralateral breast, were contoured for dose calculation. In the set of CT images of structures acquired under DIBH, the planning target volume (PTV) was expanded by 5 mm from CTV, but was restricted to the tissue within 3 mm from the skin. In the set of CT images of structure acquired under FB, the PTV was expanded by 8 mm from CTV, but was restricted to the tissue within 3 mm from the skin. The distance (A) of the tangent cut line of the chest wall perpendicular to the heart was measured for every set of CT scan images when using DIBH technique. (Figure 2) Dosimetric characteristics of three treatment plans were analyzed. The first was the original treatment plan that was planned with 3D-CRT hybrid VMAT technique under DIBH condition. The second plan was designed with pure VMAT technique and re-planned under DIBH condition using the same contours, followed by re-planning on the original CT images data under FB condition. The prescribed dose for all the treatment plans was 42.5Gy in 16 fractions, which was the same as the previous treatment schedule. These treatment plans were created using Eclipse V15.6 (Varian Medical Systems, Alto, CA, USA). All treatment plans were optimized to cover 95% of the PTV by 100% of the prescribed dose, while minimizing the doses to the OAR as much as possible. The final dose calculation with a 0.25 cm grid resolution was performed with an Acuros XB algorithm. In this study, we examined the correlation between the mean heart dose and distance (A), which represents the shortest measurement from the heart border to the posterior chest wall in the CT scan images of each patient.
 |
Table 1 Patient Characteristics |
3D-CRT Hybrid VMAT Technique Under DIBH Condition
In 2015, we designed a hybrid technique treatment plan for left early breast cancer by integrating two tangential IMRT beams as the base plan plus 2 partial coplanar conformal arcs into one treatment plan to reduce the low-dose distribution area in the lungs and normal tissue. The details of our hybrid treatment planning have been described in our previously published study.13 The optimal condition for beam delivery is when the patient is in motionless position, ie, with no body movement or organ motion. Though it is impossible to prevent all motion of the patient’s organs, we can still control the patient’s body movement by respiratory control. Under DIBH condition, there is no need for skin flush to cover the breast displacement under free breath condition. We did not give patients simultaneous integrate boost (SIB) for early and low-risk breast cancer, and therefore IMRT was not necessary for treatment planning design. 3D-CRT treatment planning delivered fewer monitor output units, which could then reduce the treatment time when compared with IMRT. Based on these reasons, we changed our policy for those who could be treated under DIBH condition by using 3D-CRT technique to design the base plan instead of IMRT and the angle arrangement was done according to the patient’s body contour. One field angle at 296°-305° and the other at 155°-135° depending on the individual breast and body contour of the patient (Figure 3a). This 3D-CRT base plan contributed 50% to 60% of the prescribed dose and the remaining prescribed dose was delivered by the VMAT plan with 2 co-planar partial arcs. The gantry angle of the 2 partial co-planar arcs ran counterclockwise from 155°-135° to 296°-305° and then clockwise from 296°-305° to 155°-135° and also depended on the individual breast and body contour of the patient (Figure 3b). The collimator angle of the 2 arcs was set to 5° or 355°. The field size was limited to less than 15 cm so that the jaws of the linear accelerator could be checked. The VMAT plan was designed to compensate for the dose non-uniformity in the target of the base plan. The dose constraints after some adjustments were as follows: heart V25Gy < 0%, heart mean dose Dmean< 2Gy, LAD max dose <5Gy, LAD mean dose Dmean< 12Gy, ipsilateral lung received 20 Gy (V20 Gy) < 20%, ipsilateral lung received 5 Gy (V5 Gy) <50%, contralateral lung received 5 Gy (V5 Gy) <20%, right breast received 5Gy (V5 Gy) <15%, and spinal cord received 20 Gy (V20 Gy) 0%.
 |
Figure 3 (a) The arc arrangement of VMAT; (b) the beam arrangement of Hybrid. |
Pure VMAT Under DIBH Condition
The beam arrangements in the pure VMAT planning under DIBH were all the same as those of the VMAT plan used in the hybrid technique with DIBH. The dose constraints for the VMAT plans were also the same as those for the hybrid technique with DIBH.
3D-CRT Hybrid VMAT Technique Under Free Breathing Condition
The hybrid technique with free breathing used all of the same parameters as the hybrid technique with DIBH, including base plan and the VMAT boost plan, except that the PTV in FB was larger than that of the PTV in DIBH. The dose constraints were all the same as those for the hybrid technique with DIBH.
Plan Comparisons
The same organ constraints were applied for all 3 treatment plans. Dose volume histograms were generated for the PTVs and all OAR for dose analysis. The homogeneity index (HI) was calculated by
where D2, D50, and D98 refer to the doses to 2%, 50%, and 98% volumes of PTV, respectively. The lower the value, the better the dose homogeneity, so a perfect HI would be 0. The conformity index (CI) was calculated by
where VPTV, ref refers to a volume of PTV covered by 95% of the prescribed dose, VPTV refers to the volume of the contoured PTV, and Vref refers to the volume of the body covered by 95% of the prescribed dose. The other items collected for dosimetric comparisons of the different treatment plans were the mean dose (Dmean) and D0.03cc of the heart, LAD maximum dose (D0.03cc), the mean dose (Dmean) and D5 of both lungs, D20 of ipsilateral lung, the mean dose (Dmean) and D5 of the right breast.
Statistical Analysis
The dosimetric differences among the 3 treatment plans for the 20 patients were analyzed using Wilcoxon signed-rank test, with p values <0.05 considered statistically significant. All analyses were performed using a two-tailed Wilcoxon signed rank test with SPSS software, version 19.0 (SPSS Inc., Chicago, IL).
Results
Dosimetric Comparison of 3D-CRT Hybrid VMAT and VMAT Under DIBH
The 3D-CRT hybrid VMAT provided better results in terms of CI and HI (Table 2). The D mean to the heart and D 0.03cc of the LAD when using 3D-CRT hybrid VMAT was significantly reduced (Table 3). There was also a significant difference found between the V5 of the ipsilateral lung or the D5, and D mean of the contralateral lung and the ipsilateral lung (Table 4). The D mean and D5 of the right breast were also significantly reduced by 3D-CRT hybrid VMAT (Table 5).
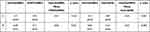 |
Table 2 Conformity Index (CI) and Homogeneity Index (HI) |
 |
Table 3 Dosimetric Characteristics of Heart and LAD |
 |
Table 4 Dosimetric Characteristics of the Ipsilateral Lung and Contralateral Lung |
 |
Table 5 Dosimetric Characteristics of the Right Breast |
Dosimetric Comparison of 3D-CRT Hybrid VMAT Under DIBH and FB
The 3D-CRT hybrid VMAT provided better CI and HI results using the DIBH technique (Table 2). There were significant reductions in the Dmean and D0.03cc to the heart and the LAD maximum dose (D0.03cc) under DIBH (Table 3). There were significant reductions of doses from the V5, V20, and D mean of the ipsilateral lung and D mean of the contralateral lung (Table 4). The D5 of the right breast was significantly reduced using the DIBH technique (Table 5).
The Overall Results
The incorporation of DIBH into 3D-CRT hybrid VMAT technique yielded the best CI and HI results as well as organ dose-sparing among the three types of treatment planning techniques (Figures 4–6). The mean heart dose was reduced from 5.38Gy to 1.65Gy (p value=0.002) and the LAD D0.03cc dose was reduced from 27.87Gy to 9.41Gy (p value=0.001) with 3D-CRT hybrid VMAT technique under FB and using DIBH technique. In this study we found that the mean heart dose could be estimated from the distance (A) of the tangent cut of the chest wall perpendicular to the heart. It varies case by case due to different deep inspiration amplitudes among patients. In the treatment planning using 3D-CRT hybrid VMAT, when the distance (A) is greater than 3.4±2.8mm in our study group, the mean heart dose will be reduced to 2Gy or below. If the distance (A) overlaps the heart, the mean heart dose will not be reduced to 2Gy or below (Figure 2).
 |
Figure 4 The isodose curves distribution of a patient created by (a) Hybrid (DIBH), (b) VMAT (DIBH), (c) Hybrid (FB). |
 |
Figure 5 Comparison of dose-volume-histograms (DVHs) for the PTV and the organ at risk between Hybrid (DIBH) and VMAT (DIBH). |
 |
Figure 6 Comparison of dose-volume-histograms (DVHs) for the PTV and the organ at risk between Hybrid (DIBH) and Hybrid (FB). |
Discussion
The most significant benefit of incorporating DIBH into 3D-CRT hybrid VMAT technique is the radiation dose-sparing to the organ at risk, especially the heart, while not compromising the radiation dose to the target.18 The volume of the heart under DIBH condition did not shrink significantly compared with the heart volume under FB. However, through this little spacing of the heart from the chest wall using DIBH technique, the mean heart dose planned by 3D-CRT hybrid VMAT using DIBH technique was reduced from 5.38Gy to 1.65Gy, (p value=0.002) and the LAD D0.03cc dose was reduced from 27.87Gy to 9.41Gy, (p value=0.001) compared with the same technique planned under FB condition. To reduce the risk of acute and late effects of radiation on normal organs, many studies have reported improvements using various treatment techniques.13,16,17 Radiotherapy under respiratory control in the supine position is an achievable method for the reduction of radiation doses to the heart.16,17,19 Respiratory control can be performed by DIBH technique on a linear accelerator. When the air is deeply inspired into the lungs, the position of the heart shifts slightly to the middle of the chest cavity as the volume of the lungs expands. The gap between the chest wall and the heart expands during DIBH (Figure 1). When the radiation dose is delivered by DIBH technique, the percentage of heart receiving a high radiation dose will be reduced. The mean dose of the heart and the percentage of the maximum dose of LAD are critical factors in cardiac events after radiotherapy.6 The reported rate of ischemic heart disease after postoperative radiotherapy to the left breast is about 2%.6 Previous studies suggested that the mean dose of the heart and LAD D0.03cc should be kept as low as possible.19
The maximum heart distance (MHD) has previously been investigated as a predictive surrogate for cardiac events. MHD was the perpendicular distance from the dorsal field border of the chest wall to the most distant part of the heart contour visible on the simulator film in the 2-dimensional era. Previous studies did not find any relationship between MHD value and cardiac events after radiotherapy.20 Not all patients benefit from utilizing DIBH technique for cardiac dose sparing.21 Patients who cannot hold their breath, or are not able to perform deep inspiration when lying down are not suitable candidates for the DIBH technique. Achieving sufficient dose coverage of the largest CTVs (whole breast) usually requires a worse arrangement of the tangential beams in 3D-CRT treatments, conditioning a greater radiation exposure of the heart, which can be significantly reduced by the use of the DIBH technique.22 The benefit of DIBH in radiation dose-sparing to the heart is dependent on the distance gap extension during deep inspiration breath hold. In this study, we found that the mean heart dose could be estimated from the distance (A) of the tangent cut of the chest wall perpendicular to the heart. If the mean distance (A) was greater than 3.4±2.8mm, the mean heart dose would be reduced to 2Gy or below. If the mean distance (A) overlaps part of the heart, the mean heart dose will not be reduced to 2Gy or below (Figure 2). According to Yamauchi’s report aimed at reducing cardiac doses, there is a relationship between specific patient parameters, including age, body mass index (BMI), and inspiratory volume, and the average heart dose in both DIBH and EB conditions.23 However, it did not analyze the average distance between the heart and the chest wall. We think this gap measurement could be investigated in future studies as a possible predictor of benefit using DIBH as a treatment technique.
Our 3D-CRT hybrid VMAT technique showed better radiation dose sparing to the lungs than VMAT on the ipsilateral and contralateral lungs under DIBH condition. The radiation doses to the contralateral OAR should be considered in treatment planning to further reduce the possibility of secondary cancer.4 To minimize the low radiation doses to the OAR we designed an IMRT hybrid VMAT technique, as described in our previous study in 2015. The low dose distribution area was significantly shifted away from the contralateral side and the back of the chest to the ipsilateral irradiated area.13 The same radiation dose sparing effect was not found in pure VMAT using DIBH technique in this study. By using the image guide radiotherapy and respiratory control technique, a more individualized radiation dose distribution could be achieved. We used 3D-CRT hybrid VMAT instead of IMRT as the base beam in this DIBH study, because when the patient was holding her breath, she was in a fixed position, ie, motionless, and therefore, skin flash was not necessary to cover the body displacement during respiration. Since no skin flash is needed and if no simultaneous integrated boost is added, IMRT is not necessary in the treatment planning when considering the dose gradient development. The benefit of using a 3D-CRT base plan instead of IMRT technique is a shorter total delivery time, because fewer monitor units are needed when it is planned by 3D-CRT.
We acknowledge that there is no perfect treatment plan in the management of postoperative radiotherapy for early breast cancer that is capable of providing all of the benefits for all types of patients. Although there is no universal threshold for mean heart dose, the radiation dose to the heart should always be kept as low as possible to reduce possible radiation-related cardiac morbidity. The limitations of this study are that our data were retrieved from previously treated patients retrospectively, limiting the randomization of the study group. The small number of patients involved may introduce bias that could affect the precision of the results. More patients should be included in the future study of the efficacy of implementing the Hybrid technique and DIBH for cardiac dose sparing.
Conclusion
The incorporation of DIBH into the 3D-CRT hybrid VMAT technique provides the best benefits for the heart and the OAR in terms of radiation dose sparing, without compromising the target conformity and homogeneity in the treatment planning.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–488. doi:10.1093/jnci/djr027
2. Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–1716.
3. Gagliano A, Prestifilippo A, Cantale O, et al. Role of the Combination of Cyclin-Dependent Kinase Inhibitors (CDKI) and Radiotherapy (RT) in the Treatment of Metastatic Breast Cancer (MBC): advantages and Risks in Clinical Practice. Front Oncol. 2021;11:643155. doi:10.3389/fonc.2021.643155
4. Taylor C, Correa C, Duane FK, et al. Estimating the risks of breast cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J Clin Oncol. 2017;35(15):1641–1649. doi:10.1200/JCO.2016.72.0722
5. Rutqvist LE, Lax I, Fornander T, Johansson H. Cardiovascular mortality in a randomized trial of adjuvant radiation therapy versus surgery alone in primary breast cancer. Int J Radiat Oncol Biol Phys. 1992;22(5):887–896. doi:10.1016/0360-3016(92)90784-F
6. Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–998. doi:10.1056/NEJMoa1209825
7. Correa CR, Litt HI, Hwang WT, Ferrari VA, Solin LJ, Harris EE. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol. 2007;25(21):3031–3037. doi:10.1200/JCO.2006.08.6595
8. Tsai PF, Lin SM, Lee SH, et al. The feasibility study of using multiple partial volumetric-modulated arcs therapy in early stage left-sided breast cancer patients. J Appl Clin Med Phys. 2012;13(5):3806. doi:10.1120/jacmp.v13i5.3806
9. Popescu CC, Olivotto IA, Beckham WA, et al. Volumetric modulated arc therapy improves dosimetry and reduces treatment time compared to conventional intensity-modulated radiotherapy for locoregional radiotherapy of left-sided breast cancer and internal mammary nodes. Int J Radiat Oncol Biol Phys. 2010;76(1):287–295. doi:10.1016/j.ijrobp.2009.05.038
10. Qiu J, Liu Z, Yang B, Hou X, Zhang F. Low-dose-area-constrained helical TomoTherapy-based whole breast radiotherapy and dosimetric comparison with tangential field-in-field IMRT. Biomed Res Int. 2013;2013:513708. doi:10.1155/2013/513708
11. Karaca S. The use of hybrid techniques in whole-breast radiotherapy: a systematic review. Technol Cancer Res Treat. 2022;21:15330338221143937. doi:10.1177/15330338221143937
12. Yu PC, Wu CJ, Tsai YL, et al. Dosimetric analysis of tangent-based volumetric modulated arc therapy with deep inspiration breath-hold technique for left breast cancer patients. Radiat Oncol. 2018;13(1):231. doi:10.1186/s13014-018-1170-3
13. Lin JF, Yeh DC, Yeh HL, Chang CF, Lin JC. Dosimetric comparison of hybrid volumetric-modulated arc therapy, volumetric-modulated arc therapy, and intensity-modulated radiation therapy for left-sided early breast cancer. Med Dosim. 2015;40(3):262–267. doi:10.1016/j.meddos.2015.05.003
14. Vedam SS, Keall PJ, Kini VR, Mohan R. Determining parameters for respiration-gated radiotherapy. Med Phys. 2001;28(10):2139–2146. doi:10.1118/1.1406524
15. Ho-Hsing Chen JW. Correction of respiratory motion for IMRT using aperture adaptive technique and visual guidance: a feasibility study. Nucl Instr Methods Phys Res A. 2007;577:6.
16. Gierga DP, Turcotte JC, Sharp GC, Sedlacek DE, Cotter CR, Taghian AG. A voluntary breath-hold treatment technique for the left breast with unfavorable cardiac anatomy using surface imaging. Int J Radiat Oncol Biol Phys. 2012;84(5):e663–e668. doi:10.1016/j.ijrobp.2012.07.2379
17. Gaál S, Kahán Z, Paczona V, et al. Deep-inspirational breath-hold (DIBH) technique in left-sided breast cancer: various aspects of clinical utility. Radiat Oncol. 2021;16(1):89. doi:10.1186/s13014-021-01816-3
18. Tang L, Ishikawa Y, Ito K, Yamamoto T, Umezawa R, Jingu K. Evaluation of DIBH and VMAT in hypofractionated radiotherapy for left-sided breast cancers after breast-conserving surgery: a Planning Study. Technol Cancer Res Treat. 2021;20:15330338211048706. doi:10.1177/15330338211048706
19. Sakka M, Kunzelmann L, Metzger M, Grabenbauer GG. Cardiac dose-sparing effects of deep-inspiration breath-hold in left breast irradiation: is IMRT more beneficial than VMAT? Strahlenther Onkol. 2017;193(10):800–811. doi:10.1007/s00066-017-1167-0
20. Borger JH, Hooning MJ, Boersma LJ, et al. Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: the role of irradiated heart volume. Int J Radiat Oncol Biol Phys. 2007;69(4):1131–1138. doi:10.1016/j.ijrobp.2007.04.042
21. Ferini G, Valenti V, Viola A, Umana GE, Martorana E. A critical overview of predictors of heart sparing by deep-inspiration-breath-hold irradiation in left-sided breast cancer patients. Cancers. 2022;14(14). doi:10.3390/cancers14143477
22. Ferini G, Molino L, Tripoli A, et al. Anatomical predictors of dosimetric advantages for Deep-inspiration-breath-hold 3D-conformal radiotherapy among women with left breast cancer. Anticancer Res. 2021;41(3):1529–1538. doi:10.21873/anticanres.14912
23. Yamauchi R, Mizuno N, Itazawa T, Saitoh H, Kawamori J. Dosimetric evaluation of deep inspiration breath hold for left-sided breast cancer: analysis of patient-specific parameters related to heart dose reduction. J Radiat Res. 2020;61(3):447–456. doi:10.1093/jrr/rraa006
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.