Back to Journals » Advances in Medical Education and Practice » Volume 14
The Effectiveness of OsiriX and the Anatomage Virtual Dissection Table in Enhancing Neuroanatomy and Neuroradiology Teaching
Authors Sadiq Z , Laswi I, Raoof A
Received 30 April 2023
Accepted for publication 17 September 2023
Published 22 September 2023 Volume 2023:14 Pages 1037—1043
DOI https://doi.org/10.2147/AMEP.S418576
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Zuhair Sadiq,1 Ibrahim Laswi,2 Ameed Raoof2
1Weiss Memorial Hospital, Chicago, IL, USA; 2Weill Cornell Medicine-Qatar, Education City, Qatar Foundation, Doha, Qatar
Correspondence: Zuhair Sadiq, Weill Cornell Medicine-Qatar, Education City, Qatar Foundation, Doha, Qatar, Tel +1-630-803-8220, Email [email protected]
Introduction: In recent years with the advent of technology in medical education, teaching methodology has shifted towards heavy use of online-learning modalities. This has been especially the case for anatomy and radiology courses since they require students to visualize structures of the human body. Several studies indicated that Anatomage and OsiriX can be effective at enhancing students’ learning experiences in anatomy and radiology.
Purpose: This aim of this study is to assess the effectiveness of online case-based learning modules in teaching medical students about the anatomy and radiology of different types of brain tumors.
Methods: Two online case-based learning modules were designed using Anatomage Table® and OsiriX DICOM viewer®, consisting of a clinical case and CT and MRI images. We recruited 36 fourth-year medical students that completed two 10-question quizzes (one on glioblastoma multiforme and one on pituitary adenomas). Participants were randomly assigned to either a study group that completed both modules prior to completing the quizzes, or a control group that completed the quizzes without access to the modules. The performance of both groups was compared to assess the effectiveness of the modules. Participants in the study group also completed a feedback survey to assess the quality and convenience of using the modules.
Results: Students who used the case-based learning modules performed significantly better than those who did not (Quiz 1: mean = 6.56 vs 3.28, p< 0.01. Quiz 2: mean = 6.67 vs 3.06, p< 0.01). Students who completed the modules would like to see similar modules used in teaching anatomy and radiology in the future (64%). They found them easy to navigate (72%), useful in teaching anatomy and radiology (72%), and helpful in improving understanding of anatomical and radiological clinical correlations (77%).
Conclusion: Online case-based learning modules created using Anatomage and OsiriX can be used effectively in teaching medical students about the anatomy and radiology of different types of brain tumors.
Keywords: anatomage, OsiriX, neuroanatomy, radiology, brain tumors, medical education
Introduction
The COVID-19 pandemic has established a sudden shift to all-online learning sessions. Teaching virtually requires access to effective educational tools, which can introduce new concepts and engage critical understanding among students. In particular, traditional medical anatomy curricula have a limited approach to educating and catering to different learning styles. However, many approaches exist for teaching anatomy: dissection, models, pro-section, computer software, and medical imaging are among the many modalities currently used in medical schools around the world.1 Each approach holds its strengths and weaknesses. Studies have reported a rise in the utilization of online learning resources following the COVID-19 pandemic. For instance, The Neurosurgical Atlas is an online interactive multimedia resource focused on neurosurgical techniques that has seen a dramatic increase (>20%) in traffic since the beginning of the pandemic.2,3
The Anatomage Virtual Dissection Table (Anatomage) is a computerized teaching tool in which CT scans of humans have been reconstructed in a 3D format so that the user can then look through them using a digital medium.4 Students can take slices through different planes as well as build up and take away cross-sections of the human body to identify organs and relate them to anatomical positions. Anatomage is interactive for students as they are offered the opportunity to essentially perform an electronic dissection of a virtual cadaver. Its main advantages are the level of detail and clarity built into the software, the ability to look through any section, and the capacity to zoom in and out.5 OsiriX is a Mac OS X-based open-source program that can process CT, MRI, PET, and PET-CT imaging. It was designed for the navigation and visualization of multidimensional images and offers a variety of rendering modes. The 3D volume rendering is the simplest and fastest way to obtain reconstructions to use for augmented reality.6 This model can be then manipulated depending on the structures the user wants to highlight. It is the most widely used medical images viewing software in the world and used by both medical professionals and learners.7
The utility of the Anatomage table in human anatomy teaching has been explored in multiple studies. In a study involving 200 Medicine and Dentistry students, Berkis et al reported that the Anatomage table allowed the students to learn the material better in a more enjoyable setting.8 A randomized, cross-sectional study focusing on the role the Anatomage table on teaching neuroanatomy showed that students using the table had comparable performance to those using traditional dissection methods. However, they reported better understanding of the topics and that it enhanced their classroom experience.9 As such, the utilization of Anatomage about other methods of student-centered learning can improve student’s perception of anatomical concepts and enhance learning.8,10 A study comparing different diagnostic imaging software and their use in veterinary medicine found that OsiriX is the highest ranked software based on functionality and user-friendliness.11
To incorporate recent literature focusing on online learning formats, and more specifically the Anatomage Table and OsiriX, new web-based teaching modules will be created for the anatomy curriculum. The objective of this study will be to create and assess the effectiveness of learning anatomy and medical imaging via online case-based learning modules created using Anatomage and OsiriX. The online modules aim to explore the synergistic learning effects of Anatomage and OsiriX with other learning tools such as clinical case-based learning. We hypothesize that modules created using Anatomage and OsiriX will improve the performances of medical students learning about different types of brain tumors.
Materials and Methods
Modules Creation
Anatomage provides an array of clinical cases and associated images. Using Microsoft PowerPoint, each case and corresponding MRI images were transformed into a module that integrated anatomic and radiographic images from OsiriX with clinical case-based learning (Figure 1). The difficulty level of each module was targeted toward students with a background in anatomy and was designed to be approximately 20 minutes in duration. The modules were published on Qualtrics Survey Software.
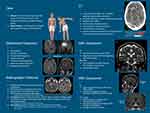 |
Figure 1 A few slides from a module (glioblastoma multiforme). |
After taking the module, students completed a 10-question quiz within the scope of the module’s learning objectives that assessed their initial knowledge of the anatomical concepts and relevant pathology. All questions were validated by anatomy faculty at Weill Cornell Medicine-Qatar. The correct answers were not shown after submission. The quizzes tested content regarding anatomy and radiology, but also covered relevant physiology and basic clinical knowledge.
Each module was prefaced with a set of learning objectives and began with an introduction to the clinical case presentation. The case introduction included the patient’s relevant demographics, chief complaint, and relevant initial neurological exam. The first module focused on Glioblastoma Multiforme, and the second module focused on Pituitary Adenomas. Both of these conditions are common in the general population and, as such, are commonly tested material in shelf and board exams. CT and MRI images from OsiriX and labeled Anatomage cadaver section images were used to assist students in understanding the placement of structures of the brain in relationship with one another. Following the necessary introduction to anatomy and radiology in the region of interest, general disease pathogenesis was discussed. In addition to pathogenesis, images of brain tumors were compared with normal anatomic findings. Other components of the modules included relevant patient’s history and physical exam findings, diagnostic imaging, and laboratory findings. Each module concluded with a list of differential diagnoses that explained the patient’s presentation.
Participants Recruitment
We recruited 36 fourth-year medical students who have completed a course in neuroanatomy during their second year. Students were randomized into two groups: Group 1 (control) completed the quizzes without completing the modules and Group 2 (test) completed the modules before completing the quizzes. To minimize observer bias, students were randomized using a computer system that did not consider their baseline knowledge of anatomy and radiology, as well as their general academic performance. Additionally, participants were unaware about the aims of the research (ie, participants assigned to the control group were not told about the modules). This study was approved by the Weill Cornell Medicine-Qatar Institutional Review Board with approval number 1943322–2 under the project title assessing the effectiveness of various online learning modules in medical students’ comprehension of anatomy.
Study Outcomes and Statistical Analysis
The scores of each of the quizzes (out of 10) were analyzed. Means were expressed as mean±SD and compared between the two groups using an independent samples t-test given the data was deemed to be normal using the Shapiro Wilks test. P-values less than 0.05 were considered significant. Statistical analysis was carried out using SPSS version 27 (IBM SPSS Statistics, IBM, Armonk, New York).
Participants who completed the modules (Group 2) were also asked to assess the quality and convenience of the modules using an anonymous feedback survey administered via Qualtrics Survey Software (Table 1). The feedback survey consisted of four five-point Likert Scale questions and an open-ended question. Categorical Likert Scale responses were expressed as a percentage of the total.
 |
Table 1 The Feedback Survey Questions and Answer Choices |
Results
Participants Performance
A total of 36 fourth-year medical students at Weill Cornell Medicine-Qatar participated in this study. All participants completed two 10-question quizzes; quiz 1 was on Glioblastoma Multiforme and quiz 2 was on Pituitary Adenomas. Participants assigned to Group 1 (control) completed the quizzes without completing the modules, while Group 2 (test) completed the quizzes after completing the modules created using Anatomage and OsiriX. For quiz 1, Group 1 (control) had a mean quiz score of 3.28±1.37 (out of 10), whereas Group 2 (test) had a mean quiz score of 6.56±1.89 (p<0.001). For quiz 2, Group 1 had a mean quiz score of 3.06±1.54 (out of 10), whereas Group 2 had a mean quiz score of 6.67±2.75 (p<0.001). The results of the quizzes are shown in Table 2.
 |
Table 2 Scores for Quiz 1 (Glioblastoma) and Quiz 2 (Pituitary Adenoma) for the Study Participants |
Quality and Convenience of the Modules
Participants who completed the modules (Group 2) were also asked to assess the quality and convenience of the modules through a feedback survey. The results of the feedback survey are summarized in Figure 2. Most students (72%, n=26) agreed or strongly agreed that they found the modules easy to navigate. This was also reflected in the comments section available in the survey, where one participant commented, “clear, concise and engaging” and another commented, “I enjoyed seeing the MRI images and being able to scroll through the cross-sections of the body while learning about the brain tumors.”
 |
Figure 2 Students opinions of the quality and convenience of the modules. |
Furthermore, 72% (n=26) of the participants reported the modules to be useful in helping them understand anatomy and radiology. Referring to the comments, an overwhelming majority of the students conveyed their satisfaction with being able to grasp the neuroanatomy presented in each of the modules. To be more specific, the participants found that they benefited most if the module began with a basic anatomical introduction before proceeding to discuss the radiology and other relevant clinical features of each case. This feedback was noted in the modules that followed this structure and were recommended as a suggestion or improvement in the modules which differed in the organization.
Moreover, 78% (n=28) of the participants agreed or strongly agreed that the modules helped improve their understanding of anatomical and radiological clinical correlations. They relayed their appreciation of the integration of clinical pearls and CT and MRI images in the modules. Many of them pointed out that this approach helped to understand how to distinguish between normal vs abnormal CT and MRI images.
To gauge the possibility of using and implementing such modules when teaching neuroanatomy, the participants were also asked if they would like to see similar modules in the future, to which 64% (n=23) agreed or strongly agreed. One participant explicitly mentioned, “This should be an added resource to the Neurology clerkship” and another participant mentioned, “Wish there were more modules on other brain tumors.”
Participants also mentioned certain areas for improvement using the open-ended question. For instance, several comments indicated a preference for more labels pointing out neuroanatomical structures. Additionally, some students mentioned that they lost interest or felt overwhelmed when faced with lengthy or wordy sections of the modules.
Discussion
Both Anatomage and OsiriX are valuable tools for creating clinical anatomy and radiology learning modules.7,10–13 In this study, we assessed and quantified the effectiveness of the clinical anatomy and radiology learning modules on brain tumors created using Anatomage and OsiriX. A total of 36 fourth-year medical students at Weill Cornell Medicine-Qatar were recruited as part of this study. The study group consisted of 18 students who completed two modules created using Anatomage and OsiriX prior to completing two 10-question quizzes to assess their performance. The control group, also consisting of 18 students, completed the same quizzes without access to the modules.
After analyzing the participants’ performance, we found that students who completed the modules performed significantly better than those who did not. Using the feedback survey, we determined that most participants who completed the modules would like to see similar modules used in teaching anatomy and radiology in the future. They found them easy to navigate, useful in teaching anatomy and radiology, and helpful in improving understanding of anatomical and radiological clinical correlations. Some students preferred more labels pointing out neuroanatomical structures and felt overwhelmed when faced with lengthy or wordy sections of the modules.
To our knowledge, this is the first study of its kind that assessed the effectiveness of both Anatomage and OsiriX in the teaching of brain tumors. Our findings are encouraging and support the implementation of technology and virtual software in this setting. Interestingly, Anand et al reported no significant difference in performance between students who learned neuroanatomy using traditional dissection methods compared to those using Anatomage. However, this study used Anatomage in the teaching of gross brain anatomy (ie, internal capsule, basal ganglion, and spinal cord).9 In comparison, our study focused on anatomical and radiological clinical associations. This discrepancy could shed light on the varying utility of Anatomage in teaching neuroanatomy.
Our cohort’s perception of the quality and convenience of the modules is also consistent with other studies. Bharati et al reported that among 150 medical students, 95% strongly agreed that Anatomage is better than traditional cadaveric dissections in visualizing body systems, and 90% strongly agreed that it can serve as to supplement anatomy learning.14 Another study reported that, like our participants, 75% of students perceived Anatomage as more engaging, and improved their understanding of anatomy.15
Limitations
Our study has some limitations that could impact the generalizability of the findings. Firstly, our study only included 36 fourth-year medical students. Even though we were able to recruit most students in the fourth-year class (around 40 students), our findings might not be generalizable to medical schools with larger cohorts. Secondly, even though all students completed a course in neuroanatomy during their second year, students with a stronger interest in neurology or neurosurgery completed additional clinical rotations in these fields. As such, these students might have higher baseline knowledge compared to those who did not complete any additional rotations. Finally, participants who completed the modules spent additional time with the material being tested compared to the control group. This limitation can be overcome in future studies by ensuring comparable study time between the study and control groups.
Conclusion
In summary, Anatomage and OsiriX can be used to create online case-based learning modules created using Anatomage and OsiriX can be used effectively in teaching medical students about the anatomy and radiology of different types of brain tumors. These modules can be perceived positively and improve students’ understanding of anatomical and radiological clinical correlations.
Data Sharing Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.
Ethical Approval
This study was approved by the Weill Cornell Medicine-Qatar Institutional Review Board with approval number 1943322-2 under the project title assessing the effectiveness of various online learning modules in medical students’ comprehension of anatomy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zargaran A, Turki MA, Bhaskar J, Spiers HVM, Zargaran D. The role of technology in anatomy teaching: striking the right balance. Adv Med Educ Pract. 2020;11:259–266. doi:10.2147/AMEP.S240150
2. Teton ZE, Freedman RS, Tomlinson SB, et al. The Neurosurgical Atlas: advancing neurosurgical education in the digital age. Neurosurg Focus. 2020;48(3):E17. doi:10.3171/2019.12.FOCUS19820
3. Tomlinson SB, Hendricks BK, Cohen-Gadol AA. Innovations in neurosurgical education during the COVID-19 pandemic: is it time to reexamine our neurosurgical training models? J Neurosurg. 2020;1–2. doi:10.3171/2020.4.JNS201012
4. Petriceks AH, Peterson AS, Angeles M, Brown WP, Srivastava S. Photogrammetry of human specimens: an innovation in anatomy education. J Med Educ Curric Dev. 2018;5. doi:10.1177/2382120518799356
5. Brucoli M, Boffano P, Pezzana A, Sedran L, Boccafoschi F, Benech A. The potentialities of the Anatomage Table for head and neck pathology: medical education and informed consent. Oral Maxillofac Surg. 2020;24(2):229–234. doi:10.1007/s10006-019-00821-x
6. Volonte F, Pugin F, Bucher P, Sugimoto M, Ratib O, Morel P. Augmented reality and image overlay navigation with OsiriX in laparoscopic and robotic surgery: not only a matter of fashion. J Hepatobiliary Pancreat Sci. 2011;18(4):506–509. doi:10.1007/s00534-011-0385-6
7. OsiriX DICOM Viewer; 2023. https://www.osirix-viewer.com/.
8. Berkis U, Kazoka D, Pilmane M, Vilka L. 3D dissection tools in Anatomage supported interactive human anatomy teaching and learning. SHS Web of Conferences. 2019;68. doi:10.1051/shsconf/20196802015
9. Anand MK, Singel T. A comparative study of learning with anatomage virtual dissection table versus traditional dissection method in neuroanatomy. Indian J Clin Anat Physiol. 2017;4(2):177–180. doi:10.18231/2394-2126.2017.0044
10. Said Ahmed MAA. Use of the Anatomage virtual table in medical education and as a diagnostic tool: an integrative review. Cureus. 2023;15(3):e35981. doi:10.7759/cureus.35981
11. Bruhschwein A, Klever J, Hoffmann AS, et al. Free DICOM-Viewers for Veterinary Medicine: survey and Comparison of Functionality and User-Friendliness of Medical Imaging PACS-DICOM-Viewer Freeware for Specific Use in Veterinary Medicine Practices. J Digit Imaging. 2020;33(1):54–63. doi:10.1007/s10278-019-00194-3
12. Patra A, Asghar A, Chaudhary P, Ravi KS. Integration of innovative educational technologies in anatomy teaching: new normal in anatomy education. Surg Radiol Anat. 2022;44(1):25–32. doi:10.1007/s00276-021-02868-6
13. Baratz G, Wilson-Delfosse AL, Singelyn BM, et al. Evaluating the anatomage table compared to cadaveric dissection as a learning modality for gross anatomy. Med Sci Educ Jun. 2019;29(2):499–506. doi:10.1007/s40670-019-00719-z
14. Bharati AS, Rani VS. A Study on Student Perception of Virtual Dissection Table (Anatomage) at GSL Medical College, Rajahmundry. Acad Anatomica Int. 2018;4(2):28–31. doi:10.21276/aanat.2018.4.2.8
15. Brown J, Stonelake S, Anderson W, et al. Medical student perception of anatomage – a 3D interactive anatomy dissection table. Int J Surgery. 2015;23:S17–S18. doi:10.1016/j.ijsu.2015.07.053
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
