Back to Journals » Nature and Science of Sleep » Volume 10
The DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure identifies high levels of coexistent psychiatric symptomatology in patients referred for insomnia treatment
Authors Meaklim H , Swieca J , Junge M , Laska I, Kelly D, Joyce R , Cunnington D
Received 7 May 2018
Accepted for publication 10 August 2018
Published 5 November 2018 Volume 2018:10 Pages 377—383
DOI https://doi.org/10.2147/NSS.S173381
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Steven A Shea
Video abstract presented by Hailey Meaklim.
Views: 921
Hailey Meaklim,1,2 John Swieca,1 Moira Junge,1 Irena Laska,1 Danielle Kelly,1,3 Rosemarie Joyce,1,3 David Cunnington1
1Melbourne Sleep Disorders Centre, East Melbourne, VIC, Australia; 2Discipline of Psychology, RMIT University, Bundoora, VIC, Australia; 3Sleep Disorders Unit, St Vincent’s Private Hospital, East Melbourne and Werribee, VIC Australia
Purpose: Referrals to sleep psychology services, even for a perceived single problem such as insomnia, can present with complex, coexistent psychiatric symptoms and comorbid disorders. This study aimed to assess the feasibility of implementing the DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure (CCSM) into a sleep psychology clinic to identify coexistent psychiatric symptomatology in insomnia referrals.
Patients and methods: Patients were 50 consecutive referrals to a private sleep psychology service within a sleep disorders center in Melbourne, Australia. Patients who attended sleep psychology services between June 2015 and January 2017 had their clinical records reviewed. Basic demographic information, comorbidities, and responses to the Insomnia Severity Index were gathered. The Diagnostic and Statistical Manual of Mental Disorders Ed. 5 Task Force and Work Groups created the CCSM in 2013 to deal with the issue of coexistent psychiatric symptomatology across mental health conditions, and this measure was included into the sleep psychology intake procedure and patient responses were reviewed.
Results: The CCSM was simple and quick to administer and score and revealed high levels of psychiatric symptomatology in sleep psychology referrals. Sleep problems were the most common domain of psychiatric symptomatology reported (86%). Anxiety (66%), depression (64%), anger (64%), and somatic symptoms (50%) were also very common. Suicidal ideation was acknowledged by 26% of patients. In addition, 82% of patients had at least one diagnosed comorbidity upon referral (eg, psychiatric, physical health, or other sleep disorder).
Conclusion: The findings support the CCSM as a feasible measure for identifying the high levels of coexistent psychiatric symptomatology in patients presenting for insomnia treatment at sleep psychology services.
Keywords: comorbidity, sleep, mental health, insomnia, assessment
Introduction
Insomnia is a common reason for referral to sleep psychology services. Insomnia is characterized by difficulties initiating or maintaining sleep and has a negative impact on individuals’ daytime functioning. Between 6% and 10% of the adult population meet diagnostic criteria for insomnia.1 Insomnia can be an independent problem, but it is also a frequently reported symptom in many psychiatric conditions (eg, depression), physical health issues (eg, cancer), and other sleep disorders (eg, obstructive sleep apnea).2–6 Therefore, referrals to sleep psychology services are often complex, and patients often report coexistent psychiatric symptomatology and comorbid disorders.
Prior to 2005, insomnia was diagnostically characterized according to the mode of origin: primary insomnia (no other condition precipitating insomnia) or secondary/comorbid insomnia (insomnia caused by/or alongside another mental disorder or general medical condition).7 With insomnia conceptualized in this way, the common practice for secondary or comorbid insomnia was to treat the underlying comorbid disorder (eg, depression) with the belief that insomnia would resolve on its own. It is now known that insomnia can have its’ own separate and independent trajectory from the comorbid condition and requires distinct and specific treatment.6,8,9 The most recent edition of The Diagnostic and Statistical Manual of Mental Disorders Ed. 5 (DSM-5) reflects this advance in the understanding of insomnia, with insomnia disorder now a separate diagnosis, as well as in the diagnostic criteria for a variety of psychiatric disorders.2 This change highlights the need for independent treatment of insomnia regardless of origin and comorbidities.10
Accurate diagnosis and treatment of comorbid conditions are also crucial for effective insomnia treatment. According to the Three-P Model of Insomnia, comorbid conditions can predispose an individual to insomnia (eg, a tendency toward anxiety), but they can also perpetuate the sleep difficulty (eg, chronic anxiety can delay sleep onset on a regular basis).11,12 If comorbid conditions are left untreated, insomnia is likely to return when there is an exacerbation of the comorbid condition. It is therefore essential for sleep psychology services to identify and treat (or refer for treatment) comorbidities that may be responsible for the development and maintenance of insomnia.
Prevalence data for coexistent medical and psychiatric conditions in sleep disorders clinics have, for some time, suggested high rates of comorbid disorders. In 1984, a study found that patients attending an insomnia clinic had high rates of psychiatric disorders (69%), personality disorders (26%), and medical comorbidities (28%).13 Another study in Singapore found that 39.5% of patients presenting to an insomnia clinic were diagnosed with psychiatric conditions of depression or anxiety.14 In addition, five sleep medicine centers in the USA found that under DSM-IV diagnostic criteria, insomnia related to a psychiatric disorder was the most common diagnosis (suggesting comorbidity) and that other sleep disorders were common in insomnia referrals.15 Conversely, in psychiatric practice, sleep disturbances are very common. Berlin et al16 found that out of 100 new psychiatric referrals, 72 patients had insomnia. A recent study identified that 31.8% of psychiatric outpatients had DSM-5 insomnia disorder and those with insomnia disorder had higher impairment outcomes.16 It is therefore paramount to understand and assess for psychiatric symptomatology and comorbidities in patients seeking help for sleep disturbances, given the bidirectional relationship between disturbed sleep and psychiatric symptoms.
The complex, bidirectional relationship between psychiatric conditions and sleep disturbance are highlighted in depression. Sixty-seven percent of people with major depressive disorder also receive a diagnosis of chronic insomnia, demonstrating high levels of comorbidity.17,18 Disturbed sleep can predict depression, and research suggests that young women, in particular, have a high chance of developing both depression and anxiety if they experience disturbed sleep in their early 20s.19 If sleep disturbances are not treated, the length and severity of an episode of improved depression is increased.20 Ongoing issues with sleep after an episode of depression can also increase the risk of a depression relapse.18,21 Taken together, these studies highlight the bidirectional relationship between sleep disturbances such as insomnia and depression and emphasize that both insomnia and depression require specific treatment.20
An increased understanding of the complex relationship between insomnia, comorbidities, and psychiatric symptomatology is reflected in the DSM-5. This latest edition of the DSM moves away from a categorical diagnostic classification system to a more dimensional one and reflects the high rates of symptom comorbidity that cross diagnostic boundaries.22 The DSM-5 Task Force and Work Groups developed the DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure-Adult (CCSM) to assess psychiatric symptomatology domains that are important, or cut across, diagnostic boundaries.23 The goal of this new measure was to help clinicians with clinical decision-making and treatment and ultimately lead to customizable treatment plans for coexistent psychiatric symptomatology and improve treatment outcomes. Given the complex relationship between insomnia, comorbidities, and psychiatric symptomatology, the CCSM may provide a quick and reliable way to identify coexistent psychiatric symptomology in sleep psychology referrals.
In order to understand coexistent psychiatric symptomatology and comorbidities present in sleep psychology referrals, the CCSM was implemented into the psychology intake process at a Melbourne-based private sleep disorders center. The study aimed to investigate the feasibility of implementing the CCSM into the sleep psychology intake process and also to undertake a clinical audit of sleep psychology referrals to study the frequency of coexistent psychiatric symptomatology and comorbid disorders. It was hypothesized that the CCSM would identify high rates of psychiatric symptomatology and comorbid disorders in this patient group. With a better understanding of these comorbidities, treatment strategies can evolve to a more transdiagnostic approach, given the bidirectional relationship between disturbed sleep and psychiatric symptoms.
Materials and methods
Participants
Fifty consecutive patients referred for an initial sleep psychology appointment with a psychologist, working one clinical day per week at a private sleep disorders center in Melbourne, Australia, between May 1, 2015 and January 31, 2017, had their electronic medical record and paper file reviewed. Most patients attending the center were from Melbourne, but some travelled from regional Victoria and interstate. Referrals to the clinic come from multiple sources, including general practitioners, specialist physicians such as psychiatrists, neurologists, and rheumatologists, as well as patients self-referring. Patients were generally seen by sleep physicians at the practice before referral to sleep psychology. Comorbidities were identified by screening the referral letter from the sleep physician at the practice, as well as patient referral letters to the sleep disorders center from general practitioners and specialist physicians. Referral letters from sleep physicians were the main source of identification of comorbidities.
Participant consent
This study received Low and Negligible Risk Human Research Ethics Committee approval from St Vincent’s Hospital (Melbourne). This retrospective clinical audit did not involve any additional intrusion upon the patients’ privacy outside of information gathered from existing medical records, and so patient consent to review their medical file was waived.
Study measures
Deidentified participant information was collected in a secure study SPSS database. Information collected included study ID, gender, date of birth, age, date of administration of intake questionnaires, referral reason, and diagnosed comorbidities upon referral.
The Insomnia Severity Index (ISI) was used to measure insomnia severity. The ISI is a seven-item questionnaire that identifies individuals’ perception of the severity of their insomnia symptoms.24 Patients record their responses on a 5-point scale (0–4) which align with DSM-IV-TR diagnostic criteria for insomnia, including severity of difficulties with sleep onset, maintenance, early morning awakenings, satisfaction with their current sleep pattern, difficulty with daily functioning, and the amount of worry or distress they experience. The ISI is a valid and reliable measure and is a useful tool for insomnia in both clinical and research settings.
CCSM was used to assess coexistent psychiatric symptomatology.23 The CCSM consists of 23 questions in a self-report format that evaluates mental health domains that are significant across psychiatric diagnoses. It is quick and easy to administer, taking patients around 5 minutes to complete in the waiting room. There are 13 psychiatric domains in this measure: depression, anger, mania, anxiety, somatic symptoms, suicidal ideation, psychosis, sleep problems, memory, repetitive thoughts and behaviors, dissociation, personality functioning, and substance use. A 5-point scale (0–4) is used to record responses and reflect how much or how often the person has been concerned by a specific symptom over the previous 2 weeks. Additional inquiry is recommended if an individual scores a mild or slight rating, depending on the psychiatric symptom being investigated. This measure has good test–retest reliability in research settings and is useful and feasible in clinical practice.22,25
Data analysis
Data were examined using statistical software package SPSS (Version 16.0 for Windows; SPSS Inc., Chicago, IL, USA). Descriptive statistics, including mean, SD, and percentages, are reported, as no significant results were obtained for correlation or regression analysis.
Results
Participant demographics
A total of 50 patients had their clinical record reviewed. Mean age of the sample was 38.60 years (age range 17–76 years). Fifty-four percent of the patients were females, and patients were primarily referred for insomnia (88%). Other referral reasons included hypersomnia (2%), continuous positive airway pressure adherence (4%), parasomnias (4%), and narcolepsy (2%).
For patients referred for insomnia (88% of the sample), ISI scores ranged from 8 to 28, with a mean of 16.63. As shown in Figure 1, clinical insomnia of moderate severity was the most frequently reported ISI score range (46.3%).
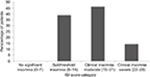  | Figure 1 ISI score categories. Abbreviation: ISI, Insomnia Severity Index. |
Psychiatric symptomatology
Administration of the CCSM was quick, with patients completing the measure in <5 minutes prior to their sleep psychology appointment. Analysis of CCSM responses indicated that psychiatric symptoms were common in sleep psychology referrals (Figure 2). As would be anticipated in a sample of sleep psychology referrals, sleeping problems were the most common domain of psychiatric symptomatology reported (86%). Anxiety (66%), depression (64%), anger (64%) and somatic symptoms (50%) were also very common.
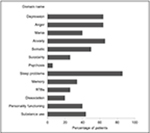  | Figure 2 Psychiatric symptomology reported by sleep psychology referrals. Abbreviation: RTBs, repetitive thoughts and behaviors. |
A high rate of substance use was reported in this sample (44%), and upon further clinical assessment, often related to self-medicating for sleep problems. Patients also frequently reported symptoms on the personality functioning domain (40%). This domain included questions such as not knowing who they were or wanted out of life, or not feeling close to others or enjoying relationships. Patients also endorsed items on the mania domain (40%), but upon further clinical assessment, this often related to symptoms of hyperarousal (eg, not sleeping well and feeling like they were running on “nervous energy” during the day). It was also concerning that 26% of the patients acknowledged items on the suicidal ideation domain.
Comorbidities
Eighty-two percent of all new sleep psychology referrals had at least one comorbid diagnosis (eg, psychiatric, physical health, or other sleep disorder). Psychiatric comorbidities were most common (26%) and included conditions such as depression, anxiety and bipolar disorder. Twenty-two percent of the patients had a sleep disorder comorbidity, such as periodic limb movement disorder, bruxism, obstructive sleep apnea, restless legs syndrome, circadian rhythm disorder or parasomnias. Physical health comorbidities were less common (14%) and included conditions such as chronic fatigue syndrome, fibromyalgia, thyroid disease, hypertension, polycystic ovarian syndrome, endometriosis, sarcoidosis, migraine, ulcerative colitis and chronic pain. Twenty percent of all patients had more than one comorbidity diagnosed upon referral (ie, a combination of psychiatric, physical health, and sleep disorder diagnoses).
Discussion
The aim of this study was to assess the feasibility of using the CCSM to identify coexistent psychiatric symptomatology in patients presenting to a sleep psychology service for insomnia treatment. It also aimed to conduct a clinical audit of patient comorbidities and co-occurring psychiatric symptomatology in insomnia referrals. The DSM-5 CCSM was implemented into the sleep psychology intake process and proved to be a quick and useful tool to identify coexistent psychiatric symptomatology in new referrals. As hypothesized, high rates of psychiatric symptomatology were observed in sleep psychology referrals, with patients frequently acknowledging symptoms of anxiety, depression, and anger, in addition to sleep problems on the CCSM. Of concern, one-quarter of the patients reported suicidal ideation. In addition, the majority of the patients had a diagnosis of least one other psychiatric, physical health, or sleep disorder comorbidity upon referral. These findings reflect the complexity of referrals seen within specialist sleep psychology service.
The results of this study are consistent with previous research demonstrating high prevalence rates for psychiatric symptomatology and comorbid disorders in patients seeking insomnia treatment at sleep disorders centers.13–16,26 This is the first study to use the CCSM in a sleep center to assist with the dimensional assessment of insomnia and psychiatric symptomatology. It is important to note that the CCSM measures psychiatric symptomatology, rather than providing a psychiatric diagnosis per se. For this reason, the rate of symptomatology for depression was much higher (60%) in this study compared to the prevalence rate of depressive disorder in the Australian population (5.9%).27 Further studies utilizing the CCSM, as well as other psychiatric diagnostic tools, are needed to ascertain whether or not this study provides a representative sample of psychiatric symptomatology and diagnoses in patients with seeking assistance for insomnia. It will also facilitate a thorough understanding of psychiatric symptomatology and sleep disturbances that cut across diagnostic boundaries as emphasized in the DSM-5.
Understanding and identifying the complexity of sleep psychology referrals has implications for assessment, treatment planning, service design, and staffing requirements for sleep disorders centers. First, identifying comorbidities and psychiatric symptomatology is important due to the bidirectional relationship between sleep disturbance and comorbidities. Regardless of which condition comes first, poorly treated comorbidities are perpetuating factors for insomnia and both conditions require treatment to improve outcomes.6,20 Although cognitive behavioral therapy for insomnia is an effective treatment for insomnia and can lead to symptom improvements in comorbid conditions, there are times in clinical practice when additional evidence-based treatment (eg, cognitive behavioral therapy for anxiety) is required to improve adherence to cognitive behavioral therapy for insomnia treatment and prevent exacerbations of insomnia. Acknowledging the high rate of psychiatric symptomatology and comorbidities present in this sample may also guide training for psychologists working in sleep psychology services, encouraging psychologists to use interdisciplinary or transdiagnostic approaches, and create customizable treatment plans, depending on comorbidities and psychiatric symptomatology. The goal of the CCSM was to aid clinicians in clinical decision-making and treatment and ultimately lead to customizable treatment plans and improve treatment outcomes, which is very relevant to sleep psychology services.28
Although this study was the first to explore the CCSM in a sleep psychology service, the study does have some limitations. This study presents data from only one sleep psychology service, which operates as part of a specialist sleep disorders center in Melbourne, Australia. It may not be representative of all sleep psychology services and may reflect the complexity of referrals seen within a specialist sleep disorder clinic in a busy urban center. Future clinical research using the CCSM will hopefully clarify this question by sampling a range of sleep psychology centers.
Second, there is no published research on the accuracy of the CCSM in a sleep psychology clinic in correctly identifying psychiatric symptomatology. The CCSM is a new tool and designed to measure on more dimensional aspects of psychiatric symptoms.23 Hence, it was assumed that it would be useful in a sleep psychology clinic, given sleep disturbances are a symptom of many different psychiatric diagnoses. However, further research is required to determine the CCSM’s accuracy in identifying psychiatric symptomatology in a sleep psychology setting.
Lastly, this study was conducted as a clinical audit of a small sleep psychology practice. The small sample size does limit the generalizability of the results. In addition, correlational and regression analysis did not yield any useful results due to the small sample size. Larger sample sizes would assist researchers to generalize the results to wider insomnia populations and to identify relationships between psychiatric symptomatology, comorbidities, patient demographics and insomnia severity, and hopefully, lead to a greater understanding of the complexity of sleep psychology referrals.
Conclusion
The CCSM was easy to administer and proved to be a feasible tool for understanding coexistent psychiatric symptomatology in new referrals to a sleep psychology service. The results of this clinical audit indicate high rates of coexistent psychiatric symptomatology and comorbid disorders in sleep psychology referrals, even for a perceived simple problem of insomnia. The results of this study have implications for psychological assessment and treatment at sleep psychology services, highlighting the need for psychologists to be skilled in working with high rates of coexistent psychiatric symptomatology and comorbidities in referrals. Future research could extend this study by implementing the CCSM in other sleep psychology services around the world to ensure the results are representative, compare the CCSM with other psychiatric diagnostic tools in a sleep psychology population, and also provide larger samples sizes to conduct further statistical analysis. It is hoped that information gained from this study will lead to the increased use of the CCSM in sleep psychology services, improve assessment of patients seeking assistance for sleep disturbance, and enable the creation of collaborative and customizable treatment plans that acknowledge the bidirectional relationship between disturbed sleep and comorbidities, to ultimately improve the sleep health and general well-being of this clinical population.
Acknowledgments
We would like to thank the reception staff at Melbourne Sleep Disorders Centre for assistance with administration and data collection of the assessment measures. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Dr David Cunnington is on the editorial board for Nature and Science of Sleep. The data reported in this manuscript was presented as a poster at the 29th Annual Scientific Meeting of the Australasian Sleep Association and the Australasian Sleep Technologists Association, held on October 25–28, 2017, in Auckland, New Zealand. This manuscript has also been accepted for a poster presentation at the 39th National Conference of the Australian Association for Cognitive and Behavioural Therapy, held on 25–27 October 2018 in Brisbane Australia.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Clinical Guidelines Committee of the American College of Physicians. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington DC, USA: American Psychiatric Association; 2013. | ||
Ohayon MM, Lemoine P. A connection between insomnia and psychiatric disorders in the French general population. Encephale. 2002;28(5 Pt 1):420–428. | ||
Szelenberger W, Soldatos C. Sleep disorders in psychiatric practice. World Psychiatry. 2005;4(3):186–190. | ||
Taylor DJ, Pruiksma KE. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: a systematic review. Int Rev Psychiatry. 2014;26(2):205–213. | ||
Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med. 2015;175(9):1461–1472. | ||
Cunnington D, Junge MF, Fernando AT. Insomnia: prevalence, consequences and effective treatment. Med J Aust. 2013;199(8):36–40. | ||
Lichstein KL, Wilson NM, Johnson CT. Psychological treatment of secondary insomnia. Psychol Aging. 2000;15(2):232–240. | ||
Sánchez-Ortuño MM, Edinger JD. Cognitive-behavioral therapy for the management of insomnia comorbid with mental disorders. Curr Psychiatry Rep. 2012;14(5):519–528. | ||
Dolsen MR, Asarnow LD, Harvey AG. Insomnia as a transdiagnostic process in psychiatric disorders. Curr Psychiatry Rep. 2014;16(9):471. | ||
Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10(4):541–553. | ||
Bélanger L, Morin CM, Langlois F, Ladouceur R. Insomnia and generalized anxiety disorder: effects of cognitive behavior therapy for gad on insomnia symptoms. J Anxiety Disord. 2004;18(4):561–571. | ||
Tan TL, Kales JD, Kales A, Soldatos CR, Bixler EO. Biopsychobehavioral correlates of insomnia. IV: Diagnosis based on DSM-III. Am J Psychiatry. 1984;141(3):357–362. | ||
Mahendran R. Characteristics of patients referred to an insomnia clinic. Singapore Med J. 2001;42(2):64–67. | ||
Buysse DJ, Reynolds CF, Hauri PJ, et al. Diagnostic concordance for DSM-IV sleep disorders: a report from the APA/NIMH DSM-IV field trial. Am J Psychiatry. 1994;151(9):1351. | ||
Berlin RM, Litovitz GL, Diaz MA, Ahmed SW. Sleep disorders on a psychiatric consultation service. Am J Psychiatry. 1984;141(4):582–584. | ||
Ashworth DK, Sletten TL, Junge M, et al. A randomized controlled trial of cognitive behavioral therapy for insomnia: an effective treatment for comorbid insomnia and depression. J Couns Psychol. 2015;62(2):115–123. | ||
Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473. | ||
Jackson ML, Sztendur EM, Diamond NT, Byles JE, Bruck D. Sleep difficulties and the development of depression and anxiety: a longitudinal study of young Australian women. Arch Womens Ment Health. 2014;17(3):189–198. | ||
Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. 2010;14(1):35–46. | ||
Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42(2–3):209–212. | ||
Narrow WE, Clarke DE, Kuramoto SJ, et al. DSM-5 field trials in the United States and Canada, Part III: development and reliability testing of a cross-cutting symptom assessment for DSM-5. Am J Psychiatry. 2013;170(1):71–82. | ||
American Psychiatric Association. Online assessment measures. Washington DC, USA: American Psychiatric Association; 2014. Available from: www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures. Accessed May 1, 2015. | ||
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. | ||
Mościcki EK, Clarke DE, Kuramoto SJ, et al. Testing DSM-5 in routine clinical practice settings: feasibility and clinical utility. Psychiatr Serv. 2013;64(10):952–960. | ||
Bianchi MT, Goparaju B, Moro M. Sleep apnea in patients reporting insomnia or restless legs symptoms. Acta Neurol Scand. 2016;133(1):61–67. | ||
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. | ||
Clarke DE, Kuhl EA. DSM-5 Cross-Cutting Symptom Measures: a step towards the future of psychiatric care? World Psychiatry. 2014;13(3):314–316. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
