Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
The Clinical Characteristics and Outcomes in Non-Frequent Exacerbation Patients with Chronic Obstructive Pulmonary Disease in the Chinese Population
Authors Liu D, Song Q, Zeng Y, Yi R, Liu Y, Li X , Chen Y, Cai S, Chen P
Received 17 April 2023
Accepted for publication 24 July 2023
Published 15 August 2023 Volume 2023:18 Pages 1741—1751
DOI https://doi.org/10.2147/COPD.S417566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Dan Liu,1,* Qing Song,2– 4,* Yuqin Zeng,2– 4 Rong Yi,5 Yi Liu,5 Xin Li,6 Yan Chen,2– 4 Shan Cai,2– 4 Ping Chen2– 4
1Department of Respiratory and Critical Care Medicine, Changsha Hospital of Traditional Chinese Medicine (Changsha Eighth Hospital), Changsha, Hunan, 410000, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, The Second Xiangya Hospital, Central South University, Changsha, Hunan, 410011, People’s Republic of China; 3Research Unit of Respiratory Disease, Central South University, Changsha, Hunan, 410011, People’s Republic of China; 4Diagnosis and Treatment Center of Respiratory Disease, Central South University, Changsha, Hunan, 410011, People’s Republic of China; 5Department of Pulmonary and Critical Care Medicine, Zhuzhou Central Hospital, Zhuzhou, Hunan, 412000, People’s Republic of China; 6Division 4 of Occupational Diseases, Hunan Prevention and Treatment Institute for Occupational Diseases, Changsha, Hunan, 412000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ping Chen, Department of Respiratory and Critical Care Medicine, The Second Xiangya Hospital, Central South University, 139 Renmin Middle Road, Changsha, Hunan, 410011, People’s Republic of China, Tel +86 731 8529 5248, Email [email protected]
Background: We analyzed the clinical characteristics and outcomes in non-frequent exacerbation patients with chronic obstructive pulmonary disease (COPD).
Methods: In this retrospective cohort study, we enrolled patients with stable COPD from 12 hospitals. Non-frequent exacerbation was defined as less than two times of exacerbations in the past year. The non-frequent exacerbation patients were classified into less and more symptomatic groups based on the COPD Assessment Test (CAT) and modified Medical Research Council (mMRC). Finally, the non-frequent exacerbation patients with less and more symptomatic were classified into the long-acting muscarinic antagonist (LAMA), long-acting β 2-agonist (LABA)+inhaled corticosteroids (ICS), LABA+LAMA, and LABA+LAMA+ICS groups. Minimum clinically important difference (MCID) was defined as a CAT score decrease of ≥ 2 during six months of follow-up. We recorded the number of exacerbations and mortality during one year of follow-up.
Results: A total of 834 (67.5%) non-frequent exacerbation patients with COPD were included in this study. The non-frequent exacerbation patients had a higher education level and body mass index (BMI), and lower CAT and mMRC scores (P< 0.05). In addition, the non-frequent exacerbation patients had lower mortality and risk of future exacerbation, and were more likely to attain MCID (P< 0.05). Furthermore, the non-frequent exacerbation patients with more symptomatic COPD treated with LABA+LAMA or LABA+LAMA+ICS were more likely to attain MCID and had a lower risk of future exacerbation (P< 0.05). However, there were no significant differences among the different inhalation therapies in non-frequent exacerbation patients with less symptomatic COPD.
Conclusion: The non-frequent exacerbation patients with COPD had a higher education level and BMI, a lower symptom burden, and better outcomes. In addition, LABA+LAMA should be recommended to non-frequent exacerbation patients with more symptomatic COPD, while mono-LAMA should be recommended to non-frequent exacerbation patients with less symptomatic COPD as the initial inhalation therapy.
Keywords: chronic obstructive pulmonary disease, non-frequent exacerbation, minimum clinically important difference, mortality, inhalation therapy
Introduction
Chronic obstructive pulmonary disease (COPD) is the most common chronic respiratory disease. It has high morbidity and mortality and exerts a huge burden on society.1 Therefore, identifying effective treatment is urgent.
Exacerbation is the important deterioration events in patients with COPD; it could lead to pulmonary function decline, worse health-related quality of life, a higher risk of future exacerbation, and mortality.2–4 In fact, previous study confirmed that even patients with COPD at a low risk of exacerbation also experience a severe risk of future exacerbation and mortality, while this has been relatively ignored.5 In addition, the clinical characteristics of non-frequent exacerbation patients with COPD have not described completely in the Chinese population.
Furthermore, it is necessary to recommend appropriate inhalation therapy for non-frequent exacerbation patients to reduce symptoms and risk of future exacerbation. In fact, long-term inhalation therapy including long-acting muscarinic antagonists (LAMA), long-acting beta-2-agonists (LABA)+inhaled corticosteroids (ICS), LABA+LAMA, and LABA+LAMA+ICS are the first choice for patients with stable COPD in the real world.6 Currently, frequent exacerbation patients with COPD have received considerable attention. The frequent exacerbation patients treated with ICS in addition to LAMA and LABA have a lower risk of exacerbation and mortality.7 However, ICS treatment increases the risk of pneumonia, so selection of patients with a low exacerbation risk may also be of clinical importance.8 Although, previous randomized controlled trials (RCTs) have confirmed the effectiveness of different inhaled bronchodilators with strict inclusion and exclusion criteria to reduce the risk of exacerbation.7,9,10 However, there is a lack of real-world data on the effects among different inhalation therapies in non-frequent exacerbation patients with COPD in the Chinese population which is crucial and the complexities of clinical practice needed to be fully considered.
Therefore, the purpose of this study was to analyze the clinical characteristics and outcomes in non-frequent exacerbation patients with COPD in the Chinese population, and to explore the outcomes among different inhalation therapies in non-frequent exacerbation patients.
Patients and Methods
Study Participants
This was a retrospective cohort study. All subjects were from the outpatient COPD database (Register number: ChiCTR-POC-17010431) that includes 12 hospitals (Supplement Table 1). The patients had been diagnosed with COPD between December 2016 and February 2022 according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017 report: a ratio of forced expiratory volume in one second to forced vital capacity (FEV1/FVC) of < 0.70 after inhaling a bronchodilator.11 Patients with asthma, lung cancer, pneumonia, bronchiectasis, and severe heart, liver or kidney disease were excluded from this study.
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Second Xiangya Hospital of Central South University (Hunan, China). All patients provided their informed consent.
Determination of the Sample Size
We used the PASS software (version 15.0.5) to calculate the sample size, with a proportion of non-frequent exacerbation patients with COPD of 0.65 based on a previous study,12 a confidence level of 0.95, and a confidence interval width (two-sided) of 0.08. Considering a dropout rate 20%, the minimum sample size was 712.
Data Collection
Data including age, sex, education level, body mass index (BMI), smoke history, FEV1%pred, FEV1/FVC, GOLD grades, COPD Assessment Test (CAT) scores, modified Medical Research Council (mMRC) scores, the number of exacerbations in the past year, and inhalation therapy regimens were collected at the patient’s first visit. At the six months follow-up, the CAT score was recorded. The number of exacerbations and mortality were collected during one year of follow-up.
Study Procedures
First, we classified the patients with COPD into the non-frequent exacerbation group, < 2 exacerbations in the past year, and frequent exacerbation group, ≥ 2 exacerbations in the past year, to determine the clinical characteristics and outcomes.
Then, we classified the non-frequent exacerbation patients into the less symptomatic group, with a CAT score of ≤ 10 and mMRC score of ≤ 1, and the more symptomatic group, a with CAT score of ≥ 10 or mMRC score of ≥ 2. Finally, we classified the non-frequent exacerbation patients with less and more symptomatic into the LAMA, LABA+ICS, LABA+LAMA, and LABA+LAMA+ICS groups based on the inhalation therapy regimens that they received at their first hospital visit.11 Thus, we analyzed the outcomes among the LAMA, LABA+LAMA, LABA+ICS, and LABA+LAMA+ICS in non-frequent exacerbation patients with less symptomatic COPD. Also, we analyzed the outcomes among the LAMA, LABA+LAMA, LABA+ICS, and LABA+LAMA+ICS in non-frequent exacerbation patients with more symptomatic COPD.
Variable Definitions
The minimum clinically important difference (MCID) was defined as a CAT score decrease of ≥ 2, and clinically symptom deterioration (CSD) was defined as a CAT score increase of ≥ 2 during six months of follow-up.13 An exacerbation is a COPD progression that requires antibiotics, oral corticosteroids, or hospitalization.14 A current-smoker has had smoking exposure of ≥ 10 pack/years, while an ex-smoker has had ≥ 10 pack/years but had not smoked for more than 6 months. We defined prescription outcomes including adjusted treatment as a change in the inhalation therapy drugs or stopping inhalation therapy drugs more than three months during one year of follow-up.15
Statistical Analysis
SPSS 26.0 (IBM, Armonk, NY, USA) and Free Statistics software version 1.7.1 (Beijing, China) were used for statistical analysis of the data. Continuous variables with a normal distribution and homogeneity of variance were analyzed with Student’s t test; otherwise, non-parametric tests were used. The chi-square test was used to analyze categorical variables. Logistic regression was used to analyze associations of non-frequent exacerbation patient characteristics with the variables (P values < 0.05) listed in Table 1, and adjusted odds ratio (aOR) and adjusted 95% confidence interval (a95% CI) were calculated. Multivariate analysis for outcomes among different inhalation therapies in non-frequent exacerbation patients and variables in the model including therapy, prescription outcomes, age, sex, education level, BMI, smoke history, biofuel exposure, FEV1%, FEV1/FVC, CAT scores and mMRC scores. To analyze the outcomes, the 1:1 propensity score matching (PSM) between non-frequent exacerbation and frequent exacerbation patients was conducted by using package R 2.15.3 (http://www.R-project.org) to control the confounding variable including age, sex, education level, BMI, smoke history, smoking (pack/year), biofuel exposure, FEV1%, FEV1/FVC, CAT scores, mMRC scores and therapy. A value of P values < 0.05 was considered to be statistically significant.
 |
Table 1 The Clinical Characteristics of Non-Frequent Exacerbation Patients with COPD |
Results
The Clinical Characteristics of the COPD Patients
A total of 1235 patients with COPD were enrolled in this study (Figure 1). The mean age was 64.3 ± 8.3 years. 834 (67.5%) were non-frequent exacerbation patients with COPD.
 |
Figure 1 Flow chart. Abbreviations: COPD, Chronic Obstructive Pulmonary Disease; ICS, Inhaled Corticosteroids; LAMA, Long-Acting Muscarinic Antagonist; LABA, Long-Acting β2-Agonist. |
The non-frequent exacerbation patients with COPD had lower ages, CAT and mMRC scores, and higher BMI, education level, FEV1%pred and FEV1/FVC (P < 0.05). In addition, the proportion of non-frequent exacerbation patients treated with LABA+LAMA+ICS was smaller (P<0.05) (Table 1).
Factors Correlated with the Non-Frequent Exacerbation Patients with COPD
After adjusting for age, FEV1/FVC, and GOLD grades, logistic regression revealed that the over high school education level (aOR = 1.388, a95% CI = 1.037–1.858), BMI 18.5–23.9 kg/m2 (aOR = 1.455, a95% CI = 1.012–2.091) and BMI more than 24 kg/m2 (aOR = 1.666, a95% CI = 1.121–2.475) were positively correlated with non-frequent exacerbation patients with COPD (P<0.05). However, CAT scores of 10–19 (aOR = 0.509, a95% CI = 0.355–0.731), 20–29 (aOR = 0.271, a95% CI = 0.178–0.415), and ≥ 30 (aOR = 0.257, a95% CI = 0.112–0.591), and mMRC scores of ≥ 2 (aOR = 0.705 a95% CI = 0.525–0.948) were negatively correlated with non-frequent exacerbation patients with COPD (P<0.05) (Table 2).
 |
Table 2 Multivariate Analysis of Relative Factors for Non-Frequent Exacerbation Patients with COPD |
The Outcomes of Non-Frequent Exacerbation Patients with COPD
There were 713 (67.3%) non-frequent exacerbation patients after one year of follow-up. After 1:1 PSM, there were 312 non-frequent exacerbation patients were to analyze the outcomes. The baseline clinical characteristics showed no significant differences (Supplement Table 2).
As described in Table 3, the non-frequent exacerbation patients with COPD had a lower risk of future exacerbation and mortality. In addition, the non-frequent exacerbation patients were more likely to attain MCID and had greater changes in CAT scores (P<0.05).
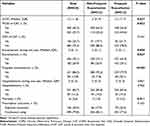 |
Table 3 The Outcomes of Non-Frequent Exacerbation Patients with COPD After Propensity Score Matching |
The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with COPD
A total of 713 non-frequent exacerbation patients were classified into the LAMA (24.3%), LABA+ICS (14.9%), LABA+LAMA (19.2%), and LABA+LAMA+ICS (41.6%) groups. After adjusting for sex, age, education level, smoke history, FEV1%pred, FEV1/FVC, CAT scores, mMRC scores, and prescription outcomes. The non-frequent exacerbation patients with COPD treated with LABA+LAMA or LABA+LAMA+ICS were more likely to attain MCID and had a lower future exacerbation risk than those treated with LAMA or LABA+ICS (P < 0.05) (Tables 4 and Supplement Table 3).
 |
Table 4 The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with COPD |
The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with Less Symptomatic COPD
A total of 117 non-frequent exacerbation patients with less symptomatic COPD were classified into the LAMA (35.0%), LABA+ICS (23.9%), LABA+LAMA (10.3%), and LABA+LAMA+ICS (30.8%) groups. After adjusting for sex, age, education level, smoke history, FEV1%pred, FEV1/FVC, CAT scores, mMRC scores, and prescription outcomes. There were no significant differences among different inhalation therapies in non-frequent exacerbation patients with less symptomatic COPD (Table 5 and Supplement Table 4).
 |
Table 5 The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with Less Symptomatic COPD |
The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with More Symptomatic COPD
A total of 596 non-frequent exacerbation patients with more symptomatic COPD were classified into the LAMA (22.1%), LABA+ICS (13.1%), LABA+LAMA (21.0%), and LABA+LAMA+ICS (43.8%) groups. After adjusting for sex, age, education level, smoke history, FEV1%pred, FEV1/FVC, CAT scores, mMRC scores, and prescription outcomes. The non-frequent exacerbation patients with more symptomatic COPD treated with LABA+LAMA or LABA+LAMA+ICS were more likely to attain MCID, had a lower future exacerbation risk, and had greater changes in CAT scores than patients treated with LAMA or LABA+ICS. However, there were no significant differences between LABA+LAMA and LABA+LAMA+ICS in MCID, CSD, future exacerbation, and mortality (Table 6, Supplement Tables 5 and 6).
 |
Table 6 The Outcomes Among Different Inhalation Therapies in Non-Frequent Exacerbation Patients with More Symptomatic COPD |
Discussion
Exacerbation is an important deterioration event in patients with COPD that could aggravate the progression of the disease. However, non-frequent exacerbation patients have been relatively ignored in COPD studies. Therefore, it is important to elucidate the clinical characteristics of these patients to identify better COPD prevention strategies. In this study, the non-frequent exacerbation patients accounted for 67.5%. This finding is consistent with previous studies that reported nearly 65% of the included non-frequent exacerbation patients.12,16 In addition, the majority of the patients had a low education level. In fact, China is a developing country and the overall level of education is not high in early time. Furthermore, in this study, we found that non-frequent exacerbation patients had a lower age and symptoms scores, and higher BMI, FEV1%pred, FEV1/FVC, and education level. Wu et al17 also found that non-frequent exacerbation patients had higher FEV1%pred and FEV1/FVC. Tashiro et al18 found that non-frequent exacerbation patients had higher BMI and FEV1%pred. These results are similar to our study. In addition, we are the first to identify several independent relative factors for non-frequent exacerbation patients with COPD, including over high school education level, BMI, CAT scores, and mMRC scores.
We also found that non-frequent exacerbation patients had a lower risk of future exacerbation, frequent exacerbation, and mortality. Larsson et al19 also found that compared with those having no or only one exacerbation, mortality was higher in patients with ≥ 2 annual exacerbations. In addition, the higher the exacerbation rate, the faster pulmonary function declined. Another study confirmed that an increasing number and severity of exacerbations were associated with increasing risk of future exacerbation and mortality.20 Furthermore, we are the first to find that non-frequent exacerbation patients with COPD are more likely to attain symptom improvement.
Inhalation drugs are the main treatment that could reduce symptoms and the risk of exacerbation and mortality, and improve the health status of patients with stable COPD.21,22 In our previous study, we found that non-frequent exacerbation patients had better outcomes. Therefore, we investigated which inhalation drugs would be better for non-frequent exacerbation patients with less symptomatic and more symptomatic COPD, respectively. We found that non-frequent exacerbation patients with more symptomatic COPD treated with LABA+LAMA or LABA+LAMA+ICS were more likely to attain MCID and had a lower risk of future exacerbation than those treated with LAMA or LABA+ICS. In fact, based on the EMAX study, LABA+LAMA consistently provides early and sustained improvements in lung function and symptoms and reduces the risk of deterioration/treatment failure versus LAMA or LABA in patients with more symptomatic COPD and a low exacerbation risk.23 Ferguson et al24 confirmed that COPD patients without exacerbation in the past year treated with LABA+LAMA+ICS had a lower risk of future exacerbation than treated with LABA+ICS. Based on the ILLUMINATE study, LABA+LAMA provides significant, sustained, and clinically meaningful improvements in lung function versus LABA+ICS. These results indicate the potential of dual bronchodilation as a treatment option for non-frequent exacerbation patients with more symptomatic COPD.25 However, it is notes that there were no significant differences between LABA+LAMA and LABA+LAMA+ICS in MCID, CSD, future exacerbation, and mortality. It implied that LABA+LAMA should be recommended to the non-frequent exacerbation patients with more symptomatic COPD as the initial inhalation therapy.
Interestingly, we found that the MCID, CSD, future exacerbation, and mortality showed no significant differences among the different inhalation therapies in non-frequent exacerbation patients with less symptomatic COPD. In fact, there were no RCTs conducted to explore the outcomes among different inhalation therapies in patients with less symptomatic COPD. A previous study confirmed that the future exacerbation and mortality showed no significant differences among different inhalation therapies in patients with less symptomatic COPD.26 It implied that mono-LAMA should be recommended to the non-frequent exacerbation patients with less symptomatic COPD as the initial inhalation therapy.
This study has some limitations. There were 121 (14.5%) non-frequent exacerbation patients lost to contact during follow-up. However, we found that the characteristics of the patients lost to follow-up and those that remained in the study were not significantly different (Supplement Table 7). The number of non-frequent exacerbation patients with less symptomatic COPD were relatively small, so larger samples sizes studies are needed in the future.
Conclusions
The non-frequent exacerbation patients with COPD had a higher education level and BMI, a lower symptom burden, and better outcomes. In addition, LABA+LAMA should be recommended to non-frequent exacerbation patients with more symptomatic COPD, while mono-LAMA should be recommended to non-frequent exacerbation patients with less symptomatic COPD as the initial inhalation therapy.
Abbreviations
BMI, Body Mass Index; COPD, Chronic Obstructive Pulmonary Disease; CAT, COPD Assessment Test; CSD, Clinically Symptom Deterioration; a95% CI, Adjusted 95% Confidence Intervals; FEV1, Forced Expiratory Volume in one second; FVC, Forced Vital Capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICS, Inhaled Corticosteroids; IQR, Interquartile Range; LAMA, Long-Acting Muscarinic Antagonist; LABA, Long-Acting β2-Agonist; mMRC, Modified Medical Research Council; MCID, Minimum Clinically Important Difference; aOR, Adjusted Odds Ratio; PSM, Propensity Score Matching; RCTs, Randomized Controlled Trials.
Data Sharing Statement
All data of this study are available from the corresponding author Ping Chen for reasonable request (http://120.77.177.175:9007/a/login).
Ethics Approval and Informed Consent
This study was approved by an institutional review board from the Second Xiangya Hospital of Central South University and conducted in accordance with the Declaration of Helsinki (ChiCTR-POC-17010431). All patients were offered informed consent.
Acknowledgments
We would like to thank the staff of the hospitals for their cooperation in collecting the study data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC, Grants 82270045) and Xiangya Mingyi grant (2013).
Disclosure
All authors have no conflicts of interest for this work.
References
1. Soriano JB, Kendrick PJ, Paulson KR.; GBD Chronic Respiratory Disease Collaborators. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 2020;8(6):585–596. doi:10.1016/S2213-2600(20)30105-3
2. Stöber A, Lutter JI, Schwarzkopf L, et al. Impact of lung function and exacerbations on health-related quality of life in COPD Patients within one year: real-world analysis based on claims data. Int J Chron Obstruct Pulmon Dis. 2021;16:2637–2651. doi:10.2147/COPD.S313711
3. Doll H, Miravitlles M. Health-related QOL in acute exacerbations of chronic bronchitis and chronic obstructive pulmonary disease: a review of the literature. Pharmacoeconomics. 2005;23(4):345–363. doi:10.2165/00019053-200523040-00005
4. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi:10.1136/thx.2005.040527
5. Kobayashi S, Hanagama M, Ishida M, et al. Clinical characteristics and outcomes in Japanese patients with COPD according to the 2017 GOLD classification: the Ishinomaki COPD network registry. Int J Chron Obstruct Pulmon Dis. 2018;13:3947–3955. doi:10.2147/COPD.S182905
6. Zeng Y, Cai S, Chen Y, et al. Current status of the treatment of COPD in China: a multicenter prospective observational study. Int J Chron Obstruct Pulmon Dis. 2020;15:3227–3237. doi:10.2147/COPD.S274024
7. Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48. doi:10.1056/NEJMoa1916046
8. Janson C, Johansson G, Ställberg B, et al. Identifying the associated risks of pneumonia in COPD patients: arctic an observational study. Respir Res. 2018;19(1):172. doi:10.1186/s12931-018-0868-y
9. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084. doi:10.1016/S0140-6736(18)30206-X
10. Rabe KF, Martinez FJ, Ferguson GT, et al. A Phase III study of triple therapy with budesonide/glycopyrrolate/formoterol fumarate metered dose inhaler 320/18/9.6 μg and 160/18/9.6 μg using co-suspension delivery technology in moderate-to-very severe COPD: the ETHOS study protocol. Respir Med. 2019;158:59–66. doi:10.1016/j.rmed.2019.08.010
11. GOLD Executive Committee. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2017 REPORT); 2017. Available from: https://goldcopd.org/.
12. Song Q, Zhao YY, Zeng YQ, et al. The characteristics of airflow limitation and future exacerbations in different GOLD groups of COPD patients. Int J Chron Obstruct Pulmon Dis. 2021;16:1401–1412. doi:10.2147/COPD.S309267
13. Kon SS, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD assessment test: a prospective analysis. Lancet Respir Med. 2014;2(3):195–203. doi:10.1016/S2213-2600(14)70001-3
14. Ritchie AI, Wedzicha JA. Definition, Causes, Pathogenesis, and Consequences of Chronic Obstructive Pulmonary Disease Exacerbations. Clin Chest Med. 2020;41(3):421–438. doi:10.1016/j.ccm.2020.06.007
15. Covvey JR, Mullen AB, Ryan M, et al. A comparison of medication adherence/persistence for asthma and chronic obstructive pulmonary disease in the United Kingdom. Int J Clin Pract. 2014;68(10):1200–1208. doi:10.1111/ijcp.12451
16. Song Q, Lin L, Cheng W, et al. Clinical-functional characteristics and risk of exacerbation and mortality among more symptomatic patients with chronic obstructive pulmonary disease: a retrospective cohort study. BMJ Open. 2023;13(3):e065625. doi:10.1136/bmjopen-2022-065625
17. Wu YK, Su WL, Yang MC, Chen SY, Wu CW, Lan CC. Characterization associated with the frequent severe exacerbator phenotype in COPD patients. Int J Chron Obstruct Pulmon Dis. 2021;16:2475–2485. doi:10.2147/COPD.S317177
18. Tashiro H, Kurihara Y, Takahashi K, et al. Clinical features of Japanese patients with exacerbations of chronic obstructive pulmonary disease. BMC Pulm Med. 2020;20(1):318. doi:10.1186/s12890-020-01362-w
19. Larsson K, Janson C, Lisspers K, et al. The impact of exacerbation frequency on clinical and economic outcomes in Swedish COPD patients: the arctic study. Int J Chron Obstruct Pulmon Dis. 2021;16:701–713. doi:10.2147/COPD.S297943
20. Whittaker H, Rubino A, Müllerová H, et al. Frequency and severity of exacerbations of COPD associated with future risk of exacerbations and mortality: a UK routine health care data study. Int J Chron Obstruct Pulmon Dis. 2022;17:427–437. doi:10.2147/COPD.S346591
21. Nici L, Mammen MJ, Charbek E, et al. Pharmacologic management of chronic obstructive pulmonary disease. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2020;201(9):e56–e69. doi:10.1164/rccm.202003-0625ST
22. Cheng W, Duan J, Zhou A, et al. Real-world effectiveness of inhalation therapy among patients with symptomatic COPD in China: a multicenter prospective study. Front Pharmacol. 2021;12:53653. doi:10.3389/fphar.2021.753653
23. Maltais F, Bjermer L, Kerwin EM, et al. Efficacy of umeclidinium/vilanterol versus umeclidinium and salmeterol monotherapies in symptomatic patients with COPD not receiving inhaled corticosteroids: the EMAX randomised trial. Respir Res. 2019;20(1):238. doi:10.1186/s12931-019-1193-9
24. Ferguson GT, Rabe KF, Martinez FJ, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, Phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–758. doi:10.1016/S2213-2600(18)30327-8
25. Vogelmeier CF, Bateman ED, Pallante J, et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med. 2013;1(1):51–60. doi:10.1016/S2213-2600(12)70052-8
26. Song Q, Lin L, Zhou A, et al. The effects of different inhalation therapies on less symptomatic chronic obstructive pulmonary disease patients in a Chinese population: a real-world study. Ann Med. 2023;55(1):1317–1324. doi:10.1080/07853890.2023.2192519
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
