Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
The Barriers to Insulin Therapy Initiation in Type 2 Diabetes Patients: A Study of General Practitioner Perceptions in Huinan Community in South Shanghai
Authors Wen S , Ruan Y, Shi Z, Dan S, Zhou L
Received 24 October 2023
Accepted for publication 19 January 2024
Published 24 January 2024 Volume 2024:17 Pages 393—405
DOI https://doi.org/10.2147/DMSO.S446349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Song Wen,1,* Yufeng Ruan,2,* Zhongyu Shi,3 Shujie Dan,2 Ligang Zhou1– 4
1Department of Endocrinology, Shanghai Pudong Hospital, Fudan University, Shanghai, People’s Republic of China; 2Department of General Practice, Huinan Health Service Center, Shanghai, People’s Republic of China; 3Department of International Medicine, Shanghai Pudong Hospital, Fudan University, Shanghai, People’s Republic of China; 4Shanghai Key Laboratory of Vascular Lesions Regulation and Remodeling, Shanghai Pudong Hospital, Fudan University Pudong Medical Center, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ligang Zhou, Department of Endocrinology, Shanghai Pudong Hospital, Fudan University, Shanghai, 201399, People’s Republic of China, Tel +8613611927616, Email [email protected]
Background: Despite the demonstrated benefits of insulin therapy, many general practitioners (GPs) are hesitant to administer it due to challenges such as a lack of knowledge, time constraints, and patient reluctance. The barriers that prevent a GP from initiating insulin therapy may vary in comparison to those encountered by a diabetic patient; this aspect of clinical research in the South Shanghai metropolitan area has received limited attention so far.
Objective: This is a 6-months of interventional analytic cohort study. The prime aim is to investigate the barriers general practitioners (GPs) face when initiating insulin therapy for patients with type 2 diabetes (T2D).
Materials and Methods: As part of a training program, all 189 registered GPs in Nanhui Health Service Center in Shanghai were given a structured online-multi-choice questionnaire before and after a six-month interval, during which the GPs received sessions of training on insulin therapy either on theoretic classes or clinical practices.
Results: Before and after training, via the methods of multiple-response analyses, the results showed that social, GP’s, and patient barriers to initiating insulin therapy were comparable. However, through the crosstabs chi-square test, we found significant changes in the basal insulin initiation following the prescription of the senior endocrinologists, the titration of insulin, and the need for training (p< 0.05). The Spearman analyses discovered significant changes associated with the cause of initial insulin refusal and the factors influencing insulin administration. Finally, the binary logistic regression analysis revealed that distinct causes such as social factors, insurance, GP experience, insulin dosage calculation, follow-up, and patients’ feelings are related to insulin treatment application before and after training.
Conclusion: According to this study, training increased general practitioners’ confidence in initiating insulin administration, especially basal insulin. General practitioners require additional education on insulin therapy, with a potential need for increased face-to-face training for insulin initiation.
Keywords: diabetes mellitus, insulin initiation barrier, general practitioner, community
Introduction
The chronic disease Type 2 Diabetes (T2D) affects millions of individuals worldwide. It is characterized by increased blood glucose levels caused by inadequate insulin production1 or utilization.2 Insulin is a hormone that regulates glucose levels in the blood, and its absence or resistance can result in severe diseases such as cardiovascular disease, renal failure, and blindness.3 Insulin therapy is necessary for the effective control of diabetes, but its acceptability by general practitioners (GPs) is limited by a variety of barriers.4,5 Insulin therapy initiation is challenging for various parties, including the patient, the physician, the family, the social worker, and the nurse.6,7 The patient’s fear of injections is a significant obstacle to using insulin in primary care.8 Nevertheless, GPs were presented with additional challenges to insulin therapy. Some GPs may lack the confidence to initiate insulin therapy and the knowledge and skills necessary to manage insulin therapy effectively.9 In addition, general practitioners may be concerned about patient compliance,10 the occurrence of severe hypoglycemia,11 and a lack of time to educate patients on insulin administration.12
To overcome these challenges, GPs must have adequate knowledge and training in insulin management.13,14 This may include lectures, workshops, and other training programs emphasizing the safe and effective administration of insulin to diabetic patients.15 In China, GPs are permanently affiliated with the endocrinologists in the central hospital. However, the status of GP’s initial insulin therapy, according to a previous community survey, was not promising; the mean hemoglobin A1c (HbA1c) while initial insulin therapy in Shanghai 2012 is about 8.35%; otherwise, the GPs themselves were DM patients were 8.1%. According to the analyses, one reason may be attributed to the lack of knowledge and skills on insulin therapy, which resulted in inadequate confidence and insulin “psychological resistance” towards insulin therapy, such as “pushing” the DM patients to the diabetes clinics or central hospital.16 The medical curriculum of a Bachelor’s in diabetes primarily covers the theoretical aspects of the pharmacological properties of all types of insulin. Still, it is sparse on its utilization, such as insulin treatment strategy and dosage calculation, for it is too specialized and could only included in fewer guidelines. It requires durations of clinical practices and experiences before they grasp it independently. Nonetheless, there is only a too short period of multiple weeks for internships to acquaint students with such specialized knowledge. Regardless of the quality of traditional teaching rounds and mini-classes on special clinical topics, they are far less likely to meet the demands of expanding the students’ clinical knowledge and actual skills. In addition, due to the overwhelming clinical workload for clinical residents and physicians, the distinct degrees of being focused by senior physicians, and disparity in their self-learning or reflect capacity, the final quality of acquirement of this skill in most rotation students may be even obviously varied. However, this experience may be the only chance for most rotation students with general practice orientation before entering their workplace community, where they may encounter many DM patients. Unfortunately, this gap, as one of multiple reasons, induced the phenomenon that many DM patients were “recommended” to the counseling room of an Endocrinologist in the central hospital to control better their blood sugar, which impacted the medical resources distribution of society, simultaneously and indirectly increased the burdens of doctors in most senior hospitals. Therefore, in recent years, there has been an increased robust contribution from the reform of medical undertakings and also emerges many clinical training and ability evaluation projects or classes, which our department is currently administering, such as the method of Mini-CEX, to train the students to grasp the insulin skills while their rotation under the monitoring of their senior doctors, and which could concurrently enhance the ability and responsibilities of their tutors.17 Moreover, we could also observe the moderate change in recent years from the medical reform, with social and government focuses and support on improving the quality of the role of GP’s “goal-keeper”; this crisis is already enduring melting. Now, the part of Endocrinologists at the central hospital can assist GPs in efficiently administering insulin therapy by providing the necessary resources and assistance. In this study, endocrinologists from Shanghai Pudong Hospital conducted a program on the barriers to initiating insulin therapy in the GPs at Huinan Health Service Center in South Shanghai, China. This study aims to identify and assess these barriers and provide methods for overcoming them so that GPs may enhance the quality of care delivered to T2D patients and assist them in achieving better health outcomes.
Materials and Methods
The Training is Designed to Improve the GP’s Ability to Initiate Insulin Therapy
From 2022 to 2023, this analytic interventional cohort study was conducted on 189 registered GPs (Cramer’s φ coefficient of refusal to initial all insulin, dfmin=1,1-β=0.40) at the Huinan Health Service Center in Shanghai. Initially, they were requested to complete a 14-question survey regarding their insulin therapy. The GPs agreed to participate in the six-month training sessions after the study. The training sessions include theoretical training, entailing classes held by the hospital and continuing educational lectures, examinations after exercise, and clinical practices, which entail advanced training at the superior or central hospitals and end with evaluations. The teacher of each training class specialized in different therapeutic fields such as insulin primary or clinical research or clinical application in different populations such as geriatrics or pregnant, etc. The objective of the training was to improve both the skill and confidence in the initial handling of insulin therapy. After six months, participants received the same questionnaire to assess the change in GPs’ confidence and other factors that potentially influence insulin therapy initiation. The type of insulin to be initialed in this study comprised insulin analogs and recombined human insulin, including long- or medium-acting insulin, rapid or short-acting insulin, and pre-mixed recombined human insulin frequently utilized in the Huinan community.
The Questionnaire’s Design Refers to the Barriers to Initial Insulin Therapy
The questionnaire (Validity: numbers of extracted factors: 3; KMO: 0.696; Bartlett’s sphere test: 236.961, p<0.0001) was tested via a designed mini-program of the survey in WeChat software, which can be generally divided into four sections: 1) The three multiple-choice questions are intended to analyze the causes for initial insulin refusal from the social (5 brief options), GP(6 brief options), and patient viewpoints (6 brief options). 2) Six questions on a survey of GPs’ insulin therapy skills, which is designed as binary choice questions (options contain Yes or No); 3) Two questions survey on kind or content of training on insulin therapy that GPs preferred, which are designed as multiple-choice questions (4–5 brief options for each question);. 4) Surveys on the frequency (5 brief options) and source (7 brief options) of GPs who have recently received insulin treatment training, structured as monomial choice questions. The structure of the questionnaire is displayed in Table 1. The GPs were required to complete the questionnaire within 10 minutes, ensuring the survey’s efficacy and consistency.
 |
Table 1 The Questionnaire Surveys the Initial Insulin Therapy in GP in Huinan Health Service Center and the Proportion of Choices Selected by GP Before and After Training |
Statistical Analyses
The results of multiple-choice questions were evaluated using multiple-response analyses, which summarized the frequencies of each option, followed by a crosstabs chi-square test to determine the difference between the pre-training and post-training questionnaires. Chi-square tests were also used to summarize and compare the frequency of binary or monomial choice questions. The correlational relationships between barriers of insulin therapy and insulin training for the GPs were investigated by Spearman analysis. The final examinations of binary logistic regression were conducted to identify the determinants of barriers to insulin therapy before and after training. For all analyses, significance was defined as p<0.05.
Results
Opinions of General Practitioners on the Social, GP, and Patient Barriers to Initiating Insulin Therapy
After conducting analyses, we determined that the most influential elements of the GP’s option on initial insulin were the absence of nurse follow-up, lack of family care, and the patient’s attitude to insulin therapy. Significantly few changes were identified after six months of training (Figure 1).
The Type and Contents of Insulin Therapy Training Preferred by GPs, as Well as the Frequency and Source of GPs Who Recently Completed Insulin Treatment Training
Surprisingly, the GPs did not appreciate the bedside teaching round as a training approach. GPs’ preferences for training seem to have minimally changed before and after the training. This research also showed that most GPs recently obtained training in insulin therapy, either through hospital training, lectures, self-learning, or other methods (Figure 2). The bedside teaching round did not seem to be considered a successful training strategy by the GPs. This demonstrates that our current way of conducting bedside teaching games by the endocrinologist at Pudong Hospital may be unsatisfactory. Training in person may be the superior option for our future training.
The Investigation Discovered Substantial Differences in the Questionnaire on Insulin Therapy Initiation Before and After Training
We observed no statistically significant differences in the percentage of insulin applications initiated before and after a 6-month training period for either insulin or basal insulin (p>0.05) (Figure 3). However, after six months of training, we noticed a significant decrease in following the endocrinologist’s prescription for insulin dosage at the central hospital (p>0.05). The GPs in Huinan Health Service Center preferred to start insulin therapy independently rather than following an endocrinologist’s recommendations. Furthermore, insulin titration results indicated that following training, GPs had greater confidence in slow and rapid insulin titration (p<0.05). The GPs also recognized that they needed more insulin training (p>0.05) (Figure 3).
The Relationship Between Insulin Initiation Barriers and GP Insulin Therapy Skills Before and After Training
The correlational analyses showed that the absence of nurse follow-up (r=−0.187, p=0.01), other social factors (supplemented by GPs, including patient and family refusal insulin, traditional medicine approach, cannot afford glucose meters) (r=0.299, p<0.0001), unfamiliar with insulin calculation (r=−0.153, p=0.035), lack of experience (r=−0.205, p=0.005) were associated with the initiation of all type of insulin before the training. The other social factors (patient and family refusal insulin, traditional medicine approach, cannot afford glucose meters) (r=0.174, p=0.017), lack of family care (r=0.171, p=0.019), unfamiliar with insulin calculation (r=−0.264, p<0.0001), lack of experience (r=−0.211, p=0.004) were associated with the barriers in initial basal insulin before the training. The lack of insulin guidelines (r=0.308, p<0.0001), other social factors (patient and family refusal insulin, traditional medicine approach, inability to afford glucose meters) (r=−0.282, p<0.0001), unfamiliar with insulin calculation (r=0.247, p=0.001), lack of experience (r=0.209, p=0.004) were associated with the following prescription by endocrinologists before the training. Lack of insulin guideline (r=−0.175, p=0.016), patient age (r=0.150, p=0.039), family care (r=0.248, p=0.001), unfamiliar with insulin calculation (r=−0.160, p=0.027), patients expenditure (r=−0.2, p=0.006) were factors related with the slow titration of insulin dosage in GPs before the training. In contrast, absence of nurse follow-up (r=−0.162, p=0.026), unfamiliar with insulin calculation for GPs (r=−0.163, p=0.025), patient inconvenience (r=−0.182, p=0.012), difficulty in injection for the patient (r=−0.154, p=0.034) were the barriers associated with rapid titration in GPs before the training. The patient inconvenience (r=0.249, p=0.001) and difficulty in injection for the patient (r=0.150, p=0.04) were associated with the GP requirement of training for insulin therapy (Figure 4A).
Notably, after training, this relationship has changed substantially. The issue of follow-up (r=0.266, p<0.0001), patient age (r=0.335, p<0.0001), family care (r=0.331, p<0.0001), patients’ compliance (r=0.189, p=0.01), patients’ expenditure (r=−0.260, p<0.0001), patients’ sense of difficulty in injection (r=0.328, p<0.0001) were the sources associated with the initiation of all type of insulin. The follow-up (r=−0.196, p=0.008), other social factors (dispensing insulin issues, patients prefer oral antidiabetics, cannot afford glucose meter) (r=0.326, p<0.0001), patient age (r=−0.175, p=0.017), family care (r=−0.216, p=0.003), patients’ expenditure (r=0.586, p<0.0001), patients’ misunderstanding (r=−0.161, p=0.029), patient’s inconvenience (r=−0.190, p=0.009), patients’ sense of complex in injection (r=−0.239, p=0.001) were factors associated with the initial basal insulin. The lack of insulin guidelines (r=0.213, p=0.004), lack of insulin dosage calculation (r=0.180, p=0.014), lack of experience (r=0.343, p<0.0001) were associated with the following the insulin prescription of Endocrinologists. Lack of insulin guidelines (r=0.333, p<0.0001), unfamiliarity with insulin calculation for GPs (r=0.298, p<0.0001), lack of experience (r=0.430, p<0.0001) were factors related to the slow titration of insulin dosage in GPs. In contrast, other social factors (dispensing insulin issues, cannot afford glucose meter) (r=0.234, p=0.001), unfamiliar with insulin calculation for GPs (r=−0.152, p=0.039), lack of experience (r=−0.281, p<0.0001), patient’s inconvenience (r=−0.185, p=0.012) were the barriers associated with rapid titration in GPs after the training. The lack of insulin guidelines (r=0.207, p=0.005), unfamiliarity with insulin calculation for GPs (r=0.155, p=0.035), lack of experience (r=0.280, p<0.0001) were associated with the GP’s requirement of insulin education (Figure 4B).
The Binary Logistic Regression Analyses on the Insulin Initiation
After that, we performed binary regression analyses on the insulin application to identify the possible determinators before and after the training. We found less GP’s experiences increased possibilities of refusal to initial all kinds of insulin before the training, while social aspects of too many patients to initial insulin therapy became the risk of deny to initial insulin therapy (Table 2). The analysis of initial basal insulin showed unfamiliarity with insulin calculation, which became the only increased risk factor before the training (Table 3). In addition, we found that other social factors (including patient and family refusal of insulin, traditional medicine approach, and not afford glucose meters) rather than the primary sources listed in the questionnaire became the only risk factor before the training (Table 4). Moreover, we analyzed the risk of GP’s slow insulin titration, which showed a significant change from the lack of insulin guidelines and patient expenditure issues to the patient’s misunderstanding of insulin therapy (Table 5). However, when we analyzed the possible obstacles related to rapid titration of insulin, we found unfamiliarity with insulin calculation and inconvenience for patients became risks before the training, whereas fewer GP experiences account for the risk after training (Table 6). Further, analyses showed that after training, the patient’s follow-up issue of social aspects became a risk for refusal of insulin therapy (Table 7).
 |
Table 2 The Binary Logistic Regression Analyses on the GPs’ Initiation of All Kinds of Insulin |
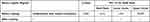 |
Table 3 The Binary Logistic Regression Analyses on the GPs’ Initiation of Basal Insulin |
 |
Table 4 The Binary Logistic Regression Analyses on the GPs Follow the Senior Hospital’s Formula |
 |
Table 5 The Binary Logistic Regression Analyses on the GPs’ Slow Insulin Dosage Titration |
 |
Table 6 The Binary Logistic Regression Analyses on the GPs’ Barriers in Rapid Insulin Dosage Titration |
 |
Table 7 The Binary Logistic Regression Analyses on the GPs’ Insulin Training are Required |
Discussion
This study investigated the barriers to insulin use in the primary care management of type 2 diabetes. We launched training sessions after the first survey, which included theoretical training classes held by the central hospital and continuing educational lectures and examinations post-training, as well as clinical training, which entailed advanced training at the superior or central hospital and ended with evaluations. Each training class was taught by an expert who specialized in insulin therapy regarding insulin primary or clinical research or clinical application in different populations such as geriatrics or pregnant women, respectively. The objective of the training was to improve both the skill and confidence in the initial handling of insulin therapy. After training, we assessed the ability and perception of GPs’ insulin therapy initiation. According to this study, the training increased GP’s abilities and confidence in initiating insulin therapy. This can potentially improve the health outcomes of people with T2D by enhancing the quality of services. This study emphasized the need to remove barriers to initial insulin therapy and provide GPs with ongoing training and support (Figure 5).
First, we observed that, regarding social reasons, the absence of nurse follow-up may be the most critical issue for GPs, as insufficient nurse follow-up could shield patients from professional supervision and assistance, frequently resulting in poor glycemic control.18,19 Lack of family care from a GP viewpoint is also crucial, as it may be beneficial in preventing the unfavorable effect of the incidence of hypoglycemia by insulin treatment and, therefore, achieving a better glycemic control target.20 From the perspective of the doctors, a patient’s reactions, such as their fear of receiving an injection, their misconceptions about insulin therapy (some patients thought insulin was addictive), and their difficulty with the complex insulin injection procedure, could render it difficult for them to receive proper treatment, enhancing the doctor’s unwillingness to begin administering insulin to them.6,21 Insurance and expense were not concerned for the GP because the national health insurance program insured most patients. However, even after training, we found that a higher percentage of these barriers remained, indicating that they could not be quickly addressed by clinical training for skill (ie, the shortage of nurse follow-up) and that further work from society and the health insurance system was necessary in addition to GP training.22–24
Subsequently, we investigated the training approach and content that the GP preferred. The most common training methods were lectures, case studies, and push notifications. Surprisingly, we discovered that the bedside teaching round was not appreciated as a training approach by GPs. This could be due to a shortage of Huinan Health Service Center laboratory tests essential for proper T2D in-patient diagnosis during bedside teaching. More laboratory tests should be performed at the Huinan Health Service Center, and the Huinan government should pay attention to this. Additionally, the endocrinologists’ experience at the central hospital, the most recent insulin research findings, and the contents of the diabetic guidelines will all benefit GPs in their daily duties.11,25 On the other hand, we found that training in insulin therapy would benefit GPs if it occurred once a month or for a shorter period. The activity could take place inside or outside of a hospital, as well as self-learning was essential for GPs to improve their insulin therapy skill. These training elements and topics did not significantly change following training, indicating that GPs emphasize these issues above all others.
Unlike the previous underlined survey,26–28 we observed significant changes in insulin initiation after training. Following training, GPs were more willing to initiate insulin therapy independently, evidenced by a decrease in the proportion of GPs who followed the endocrinologist’s insulin prescription in the central hospital. These findings suggested that GPs are more confident in titrating insulin dosage on their own if they receive personal guidance adapted to the distinctive condition of patients.29,30 Furthermore, following training, more GPs seek insulin training to increase their insulin management skills.31
We performed correlational analyses to examine the association between insulin therapy barriers and the percentage of GPs who began administering insulin before and after training. Interestingly, we discovered that the absence of nurse follow-up, lack of family care, lack of insulin guidelines, GPs’ unfamiliarity with insulin calculation, and fewer GPs’ experience with insulin injection were critical factors associated with the initiation of insulin therapy and influenced the GPs’ decision whether to follow the endocrinologist’s insulin prescription at the central hospital.24 Patient age, expenditure, and patient feelings over insulin therapy were also factors influencing the GP’s choice for initiation of insulin therapy.32
Finally, to identify factors that influence insulin therapy initiation, we performed binary logistic regression analysis, which examines the independent, crucial elements of insulin therapy initiation from the social, GP, and patient perspectives. These characteristics changed considerably after training, implying that GPs could administer insulin more appropriately based on training and familiarity with patients’ situations. In particular, GPs may overcome their lack of initial expertise with all forms of insulin through training and focus more on virtual cases such as PT compliance, expense, and patient feelings over injection. After training, GPs can handle basal insulin professionally, and the elements that impact their decision are generally derived from the absence of nurse follow-up, PT compliance, expenditure, and patient feelings over injection. After training, GPs could effectively initialize insulin and make decisions based primarily on the patient’s conditions. However, crucial social variables such as less professional follow-up by nurses, a lack of family care, and high expenses remain unresolved, needing substantial reform from society and the healthcare system.
Limitation
One of our study limitations lies in a survey of GPs only in a community setting, the results of which might be partially independent of other previous typical research held in hospitals or central health centers. In addition, we did not propose a complete strategy for improving this situation. It needs deepening transformations that contribute to changes in the GP’s perception and enhancement of their insulin skills; otherwise, this action may need further support from the social and healthcare system.
Conclusion
T2D treatment demands insulin therapy, which is not commonly accepted in Huinan Health Service Center GPs due to several barriers. Patients’ fear of injections, a lack of patient education, the cost of insulin, the complexity of insulin regimens, and some patients’ misunderstandings of insulin therapy are among the issues. To overcome such barriers, GPs must communicate effectively with patients while continuing to obtain insulin therapy training from endocrinologists and self-learning. Some barriers, such as the absence of nurse follow-up, were unsolvable even with GP training. In addition to GP efforts, additional efforts from society and the healthcare system are required.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The study, including surveys, has obtained ethics approvals and permissions from the Ethics Committee of Shanghai Pudong Hospital (NO. WZ-010). Informed consent was received from study participants before the study. The guidelines and procedures were outlined under the Declaration of Helsinki. All the data used in this study were anonymized before its use.
Statement on Guideline
The study was based on related institutional guidelines on clinical research and regulations of human participants in the investigation of Shanghai Pudong Hospital, Fudan University.
Acknowledgments
We would like to thank all Huinan Health Service Center participants who provided numerous invaluable contributions to this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Fudan Zhangjiang Clinical Medicine Innovation Fund Project (KP0202118), Fudan 2nd Reform of Education Grant (FD2023A227), Project of Key Medical Discipline of Pudong Hospital of Fudan University (Zdxk2020-11), Project of Key Medical Specialty and Treatment Center of Pudong Hospital of Fudan University (Zdzk2020-24), Integrative Medicine special fund of Shanghai Municipal Health Planning Committee (ZHYY- ZXYJHZX-2-201712), Special Department Fund of the Pudong New Area Health Planning Commission (PWZzk2017-03), Outstanding Leaders Training Program of Pudong Health Bureau of Shanghai (PWR12014-06), Pudong New Area Clinical Plateau Discipline Project (PWYgy-2021-03), the Natural Science Foundation of China (21675034), National Natural Science Foundation of China (81370932), Shanghai Natural Science Foundation (19ZR1447500), Pudong New Area Clinical Characteristic Discipline Project (PWYts2021-11)., Pudong New Area Clinical Characteristic Discipline Project (PWYts2021-01), Wenzhou Medical University Education Grant (JG2021197).
Disclosure
The authors declare that there are no competing interests related to this study.
References
1. Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol. 2020;16(7):349–362. doi:10.1038/s41574-020-0355-7
2. Lewis ST, Greenway F, Tucker TR, et al. A receptor story: insulin resistance pathophysiology and physiologic insulin resensitization’s role as a treatment modality. Int J Mol Sci. 2023;24(13). doi:10.3390/ijms241310927
3. Marassi M, Fadini GP. The cardio-renal-metabolic connection: a review of the evidence. Cardiovasc Diabetol. 2023;22(1):195. doi:10.1186/s12933-023-01937-x
4. de Lusignan S, McGovern A, Hinton W, et al. Barriers and facilitators to the initiation of injectable therapies for type 2 diabetes mellitus: a mixed methods study. Diabetes Ther. 2022;13(10):1789–1809. doi:10.1007/s13300-022-01306-z
5. Lee PY, Lee YK, Khoo EM, Ng CJ. How do health care professionals assess patients when initiating insulin therapy? A qualitative study. Prim Care Diabetes. 2014;8(1):49–55. doi:10.1016/j.pcd.2013.11.003
6. Fu CH, Lee LY, Huang LC, Tsay SL, Chen SC. Psychological insulin resistance and its impact on self-management in type II diabetes mellitus patients treated with insulin therapy. Int J Nurs Pract. 2023;e13190. doi:10.1111/ijn.13190
7. Peyrot M, Rubin RR, Khunti K. Addressing barriers to initiation of insulin in patients with type 2 diabetes. Prim Care Diabetes. 2010;4 Suppl 1:S11–S18. doi:10.1016/S1751-9918(10)60004-6
8. Grant RW, Wexler DJ, Watson AJ, et al. How doctors choose medications to treat type 2 diabetes: a national survey of specialists and academic generalists. Diabetes Care. 2007;30(6):1448–1453. doi:10.2337/dc06-2499
9. Abu hassan H, Tohid H, Mohd Amin R, Long Bidin MB, Muthupalaniappen L, Omar K. Factors influencing insulin acceptance among type 2 diabetes mellitus patients in a primary care clinic: a qualitative exploration. BMC Fam Pract. 2013;14:164. doi:10.1186/1471-2296-14-164
10. Davies MJ, Gagliardino JJ, Gray LJ, Khunti K, Mohan V, Hughes R. Real-world factors affecting adherence to insulin therapy in patients with type 1 or type 2 diabetes mellitus: a systematic review. Diabet Med. 2013;30(5):512–524. doi:10.1111/dme.12128
11. Ellis K, Mulnier H, Forbes A. Perceptions of insulin use in type 2 diabetes in primary care: a thematic synthesis. BMC Fam Pract. 2018;19(1):70. doi:10.1186/s12875-018-0753-2
12. Tan AM, Muthusamy L, Ng CC, Phoon KY, Ow JH, Tan NC. Initiation of insulin for type 2 diabetes mellitus patients: what are the issues? A qualitative study. Singapore Med J. 2011;52(11):801–809.
13. Deed G, Kilov G, Phillips P, et al. Peer-to-peer, interactive GP education can reduce barriers to best practice in diabetes management. Diabetes Ther. 2016;7(1):153–161. doi:10.1007/s13300-016-0156-0
14. Riddle M, Peters A, Funnell M. Increasing patient acceptance and adherence toward insulin. Postgraduate Med. 2016;128 Suppl 1:11–20. doi:10.1080/00325481.2016.1177969
15. Boeder S, Matamoros D, Mansy C. Practical guidance for healthcare providers on collaborating with people with type 2 diabetes: advancing treatment and initiating injectable therapy. Diabetes Ther. 2023;14(2):425–446. doi:10.1007/s13300-022-01330-z
16. Tang C. Psychological Insulin Resistance Survey to General Practitioners in Shanghai. Fudan University; 2013.
17. He Y, Wen S, Zhou M, Li X, Gong M, Zhou L. A pilot study of modified Mini-Clinical Evaluation Exercises (Mini-CEX) in rotation students in the department of endocrinology. Diabetes Metab Syndr Obes. 2022;15:2031–2038. doi:10.2147/DMSO.S372253
18. Levich BR. Diabetes management: optimizing roles for nurses in insulin initiation. J Multidiscip Healthc. 2011;4:15–24. doi:10.2147/JMDH.S16451
19. Kuo CR, Quan J, Kim S, Tang AH, Heuerman DP, Murphy EJ. Group visits to encourage insulin initiation: targeting patient barriers. J Clin Nurs. 2017;26(11–12):1705–1713. doi:10.1111/jocn.13577
20. Xie Y, Agiro A, Bowman K, DeVries A. Lowering cost share may improve rates of home glucose monitoring among patients with diabetes using insulin. J Manag Care Spec Pharm. 2017;23(8):884–891. doi:10.18553/jmcp.2017.23.8.884
21. Hussein A, Mostafa A, Areej A, et al. The perceived barriers to insulin therapy among type 2 diabetic patients. Afr Health Sci. 2019;19(1):1638–1646. doi:10.4314/ahs.v19i1.39
22. Reach G, Le Pautremat V, Gupta S. Determinants and consequences of insulin initiation for type 2 diabetes in France: analysis of the national health and wellness survey. Patient Preference Adherence. 2013;7:1007–1023. doi:10.2147/PPA.S51299
23. Harvey G, Llewellyn S, Maniatopoulos G, Boyd A, Procter R. Facilitating the implementation of clinical technology in healthcare: what role does a national agency play? BMC Health Serv Res. 2018;18(1):347. doi:10.1186/s12913-018-3176-9
24. Ratanawongsa N, Crosson JC, Schillinger D, Karter AJ, Saha CK, Marrero DG. Getting under the skin of clinical inertia in insulin initiation: the Translating Research Into Action for Diabetes (TRIAD) insulin starts project. Diabetes Educ. 2012;38(1):94–100. doi:10.1177/0145721711432649
25. Giugliano D, Maiorino MI, Bellastella G, Esposito K. Clinical inertia, reverse clinical inertia, and medication non-adherence in type 2 diabetes. J Endocrinol Invest. 2019;42(5):495–503. doi:10.1007/s40618-018-0951-8
26. Forst T, Choudhary P, Schneider D, Linetzky B, Pozzilli P. A practical approach to the clinical challenges in initiation of basal insulin therapy in people with type 2 diabetes. Diabetes/Metab Res Rev. 2021;37(6):e3418. doi:10.1002/dmrr.3418
27. Chan WB, Chen JF, Goh SY, et al. Challenges and unmet needs in basal insulin therapy: lessons from the Asian experience. Diabetes Metab Syndr Obes. 2017;10:521–532. doi:10.2147/DMSO.S143046
28. Escalada J, Orozco-Beltran D, Morillas C, et al. Attitudes towards insulin initiation in type 2 diabetes patients among healthcare providers: a survey research. Diabetes Res Clin Pract. 2016;122:46–53. doi:10.1016/j.diabres.2016.10.003
29. Campbell MD, Babic D, Bolcina U, et al. High level of clinical inertia in insulin initiation in type 2 diabetes across Central and South-Eastern Europe: insights from SITIP study. Acta diabetologica. 2019;56(9):1045–1049. doi:10.1007/s00592-019-01346-1
30. Berard L, Bonnemaire M, Mical M, Edelman S. Insights into optimal basal insulin titration in type 2 diabetes: results of a quantitative survey. Diabetes Obesity Metab. 2018;20(2):301–308. doi:10.1111/dom.13064
31. Perreault L, Vincent L, Neumiller JJ, Santos-Cavaiola T. Initiation and titration of basal insulin in primary care: barriers and practical solutions. J Am Board Fam Med. 2019;32(3):431–447. doi:10.3122/jabfm.2019.03.180162
32. Bin Rsheed A, Chenoweth I. Barriers that practitioners face when initiating insulin therapy in general practice settings and how they can be overcome. World J Diabetes. 2017;8(1):28–39. doi:10.4239/wjd.v8.i1.28
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





