Back to Journals » Journal of Pain Research » Volume 15
The American Society of Pain and Neuroscience (ASPN) Evidence-Based Clinical Guideline of Interventional Treatments for Low Back Pain
Authors Sayed D , Grider J, Strand N , Hagedorn JM , Falowski S , Lam CM , Tieppo Francio V , Beall DP, Tomycz ND, Davanzo JR, Aiyer R, Lee DW, Kalia H , Sheen S, Malinowski MN , Verdolin M, Vodapally S , Carayannopoulos A, Jain S, Azeem N , Tolba R, Chang Chien GC, Ghosh P, Mazzola AJ, Amirdelfan K, Chakravarthy K, Petersen E , Schatman ME , Deer T
Received 19 August 2022
Accepted for publication 17 November 2022
Published 6 December 2022 Volume 2022:15 Pages 3729—3832
DOI https://doi.org/10.2147/JPR.S386879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Alaa Abd-Elsayed
Dawood Sayed,1 Jay Grider,2 Natalie Strand,3 Jonathan M Hagedorn,4 Steven Falowski,5 Christopher M Lam,1 Vinicius Tieppo Francio,6 Douglas P Beall,7 Nestor D Tomycz,8 Justin R Davanzo,9 Rohit Aiyer,10 David W Lee,11 Hemant Kalia,12,13 Soun Sheen,13 Mark N Malinowski,14,15 Michael Verdolin,16 Shashank Vodapally,17 Alexios Carayannopoulos,18– 20 Sameer Jain,21 Nomen Azeem,22,23 Reda Tolba,24,25 George C Chang Chien,26,27 Priyanka Ghosh,28 Anthony J Mazzola,29 Kasra Amirdelfan,30 Krishnan Chakravarthy,31,32 Erika Petersen,33 Michael E Schatman,34,35 Timothy Deer36
1Department of Anesthesiology and Pain Medicine, The University of Kansas Medical Center, Kansas City, KS, USA; 2University of Kentucky, Lexington, KY, USA; 3Interventional Pain Management, Mayo Clinic, Scottsdale, AZ, USA; 4iSpine Pain Physicians, Maple Grove, MN, USA; 5Functional Neurosurgery, Neurosurgical Associates of Lancaster, Lancaster, PA, USA; 6Department of Rehabilitation Medicine, University of Kansas Medical Center, Kansas City, KS, USA; 7Comprehensive Specialty Care, Edmond, OK, USA; 8AHN Neurosurgery, Allegheny General Hospital, Pittsburgh, PA, USA; 9AHN Neurosurgery, Forbes Hospital, Monroeville, PA, USA; 10Interventional Pain Management and Pain Psychiatry, Henry Ford Health System, Detroit, MI, USA; 11Physical Medicine & Rehabilitation and Pain Medicine, Fullerton Orthopedic Surgery Medical Group, Fullerton, CA, USA; 12Rochester Regional Health System, Rochester, NY, USA; 13Department of Physical Medicine & Rehabilitation, University of Rochester, Rochester, NY, USA; 14Adena Spine Center, Adena Health System, Chillicothe, OH, USA; 15Ohio University Heritage College of Osteopathic Medicine, Athens, OH, USA; 16Anesthesiology and Pain Medicine, Pain Consultants of San Diego, San Diego, CA, USA; 17Physical Medicine and Rehabilitation, Michigan State University, East Lansing, MI, USA; 18Department of Physical Medicine and Rehabilitation, Rhode Island Hospital, Newport Hospital, Lifespan Physician Group, Providence, RI, USA; 19Comprehensive Spine Center at Rhode Island Hospital, Newport Hospital, Providence, RI, USA; 20Neurosurgery, Brown University, Providence, RI, USA; 21Interventional Pain Management, Pain Treatment Centers of America, Little Rock, AR, USA; 22Department of Neurology, University of South Florida, Tampa, FL, USA; 23Florida Spine & Pain Specialists, Riverview, FL, USA; 24Pain Management, Cleveland Clinic, Abu Dhabi, United Arab Emirates; 25Anesthesiology, Cleveland Clinic Lerner College of Medicine, Cleveland, OH, USA; 26Pain Management, Ventura County Medical Center, Ventura, CA, USA; 27Center for Regenerative Medicine, University Southern California, Los Angeles, CA, USA; 28Remedy Medical Group, San Francisco, CA, USA; 29Mount Sinai Health System, New York City, NY, USA; 30IPM Medical Group, Inc., Walnut Creek, CA, USA; 31Division of Pain Medicine, Department of Anesthesiology, University of California San Diego, San Diego, CA, USA; 32Va San Diego Healthcare, San Diego, CA, USA; 33Department of Neurosurgery, University of Arkansas for Medical Science, Little Rock, AR, USA; 34Department of Anesthesiology, Perioperative Care, and Pain Medicine, NYU Grossman School of Medicine, New York, New York, USA; 35Department of Population Health - Division of Medical Ethics, NYU Grossman School of Medicine, New York, New York, USA; 36The Spine and Nerve Center of the Virginias, Charleston, WV, USA
Correspondence: Dawood Sayed, The University of Kansas Health System, 3901 Rainbow Blvd, Kansas City, KS, 66160, USA, Tel +1 913-588-5521, Email [email protected]
Introduction: Painful lumbar spinal disorders represent a leading cause of disability in the US and worldwide. Interventional treatments for lumbar disorders are an effective treatment for the pain and disability from low back pain. Although many established and emerging interventional procedures are currently available, there exists a need for a defined guideline for their appropriateness, effectiveness, and safety.
Objective: The ASPN Back Guideline was developed to provide clinicians the most comprehensive review of interventional treatments for lower back disorders. Clinicians should utilize the ASPN Back Guideline to evaluate the quality of the literature, safety, and efficacy of interventional treatments for lower back disorders.
Methods: The American Society of Pain and Neuroscience (ASPN) identified an educational need for a comprehensive clinical guideline to provide evidence-based recommendations. Experts from the fields of Anesthesiology, Physiatry, Neurology, Neurosurgery, Radiology, and Pain Psychology developed the ASPN Back Guideline. The world literature in English was searched using Medline, EMBASE, Cochrane CENTRAL, BioMed Central, Web of Science, Google Scholar, PubMed, Current Contents Connect, Scopus, and meeting abstracts to identify and compile the evidence (per section) for back-related pain. Search words were selected based upon the section represented. Identified peer-reviewed literature was critiqued using United States Preventive Services Task Force (USPSTF) criteria and consensus points are presented.
Results: After a comprehensive review and analysis of the available evidence, the ASPN Back Guideline group was able to rate the literature and provide therapy grades to each of the most commonly available interventional treatments for low back pain.
Conclusion: The ASPN Back Guideline represents the first comprehensive analysis and grading of the existing and emerging interventional treatments available for low back pain. This will be a living document which will be periodically updated to the current standard of care based on the available evidence within peer-reviewed literature.
Keywords: back pain, intervention, clinical guideline, spinal cord stimulation, minimally invasive spine procedure, lumbar disorder, epidural steroid injection, radiofrequency ablation
Corrigendum for this paper has been published.
Introduction
Objectives, Scope, and Goals
The objective of the American Society of Pain and Neuroscience (ASPN) Evidence-Based Clinical Guideline for Interventional Treatments of low back pain (LBP) is to provide evidence-based recommendations to address the appropriate utilization of interventional treatments for LBP. This guideline is intended to represent a comprehensive review of the spectrum of interventional treatments for LBP. The guideline is based upon the highest quality of clinical evidence available at the time of publication. The goals of the guideline are to assist clinicians in delivering the highest quality evidenced back interventional treatments, as well as understanding the known risks and complications of interventional treatments. The ASPN Back Guideline is intended to be updated periodically to maintain relevance with the current treatment landscape and empirical literature. Although the guideline represents a comprehensive review of the majority of the interventional treatments for LBP, it is important to note that not all interventional techniques were included. Exclusion of any particular technique does not necessarily suggest that the omitted therapies are inappropriate clinical use. The ASPN Back Guideline does not represent a standard of care. Treatment should be based on an individual patient’s need and the physician’s professional judgement and experience. This guideline is not intended to be used as the sole reason for denial or approval of treatment or services.
ASPN Back Guideline Clinical Committee and Multidisciplinary Collaboration
The ASPN clinical guideline committee is comprised of a diverse group of physicians representing the specialties most commonly involved in the provision of interventional treatments of LBP. This includes physicians from the core specialties of anesthesiology, neurosurgery, physical medicine and rehabilitation, and radiology, as well as a pain psychologist/medical ethicist with many years of experience in consulting with interventional physicians. Committee members were selected based on clinical experience, research, and previous publication history.
Disclosures of Potential Conflicts of Interests
All participants involved in the guideline development have been required to disclose all potential conflicts of interest. All evidence grading was reviewed and validated by committee members with no potential conflict of interest for any particular therapy. Authors with conflicts of interest on subjects with grading criteria were recused from those particular items.
Methods for Literature Search, Evidence Ranking and Consensus Development
The world literature in English from 2000-present was searched using Medline, EMBASE, Cochrane CENTRAL, BioMed Central, Web of Science, Google Scholar, PubMed, Current Contents Connect, Meeting Abstracts, and Scopus to identify and compile the evidence for lower back interventional therapies for the treatment of pain. Search words were created specific to the topics for each major section pertaining to injection therapy, minimally invasive spine procedures and ablative procedures. Identified peer-reviewed literature was critiqued using the United States Preventive Services Task Force (USPSTF) criteria for quality of evidence,1 with modifications for interventional pain studies (Table 1). The hierarchy of evidence for the project considered RCT as the preeminent classification, followed by prospective observational studies, case series and finally expert opinion. Per the methodology, the process identified RCT and prospective observational studies of STROBE criteria quality in the creation of guidelines. Interventions with more than one RCT were considered to have sufficient evidence to create conclusions, and observational studies were not considered. Interventions with no RCTs or only one RCT then also utilized prospective observational studies in the creation of guideline recommendations. Should an intervention be found to have no RCTs or observational studies, case series were used. These are clearly denoted by the taxonomy of the recommendation that the predominant quality of evidence is of a classification less than RCT. For interventions where RCT and prospective observational studies are of requisite quality (STROBE) are not available, case series and/or expert opinion may be used in the creation of guidelines to fill in the current literature gap to assist the clinician in selecting care pathways. These designations follow a modified USPSTF process used previously by ASPN and NANS in the creation of guidelines. The details are listed in Table 1. After USPSTF letter grading was assigned, the working subgroup then assigned the “level of certainty regarding benefit” as described in Table 2.
 |
Table 1 Quality of Evidence Ranking Using United States Preventative Services Task Force Criteria Modified for Interventional Spine Procedures |
 |
Table 2 Levels of Certainty Regarding Net Benefit |
For each major section or topic, the ASPN Back Group formulated consensus points. Consensus points should not be confused with recommendations based on consensus alone, which were rendered as clinical guidance due to the lack of evidence-based literature (such as randomized controlled trials [RCTs], prospective observational studies, retrospective cohort/case series).
Injection Therapy
Epidural Steroid Injections
LBP has consistently been one of the most common causes of functional limitation and absence from work, as it impacts over 80% of the general population around the world.2,3 A common diagnosis of LBP is lumbar radiculopathy, with a prevalence between 9.9% and 25%.4 Lumbar radiculopathy is generally defined as LBP that radiates down below the knees to the foot and toes and can be associated with neurological findings such as paresthesia and weakness. Radiculopathy is not only secondary to mechanical compression but may also be due to the release of inflammatory mediators at the site of pathology.5 When comparing to LBP without radicular symptoms, lumbar radiculopathy is associated with more disability and pain, and thus causes decreased quality of life and increased utilization of health resources.6 Per current guidelines around the world, treatment for lumbar radiculopathy includes spinal injections, specifically lumbar epidural steroid injections.
Epidural steroid injections are generally performed with three different approaches: interlaminar (midline or parasagittal), transforaminal or caudal. The interlaminar approach is widely used, but limitations can include lack of target specificity and the injectate being distributed to the dorsal epidural space, as opposed to the ventrolateral space.7 The transforaminal approach, however, is considered to be more specific as this injection localizes the injectate into the ventrolateral epidural space, which is anatomically located in close proximity to the nerve root.7 The caudal approach can be specifically utilized and may be advantageous in patients with previous spine surgeries, such as a lumbar fusion or laminectomy, in which cases it may be unsafe or anatomically impossible to utilize the interlaminar or transforaminal approach.
Corticosteroid injectable agents are divided into two groups: non-particulate and particulate. Non-particulate corticosteroids are faster in onset but have much shorter acting anti-inflammatory properties. On the other hand, particulate corticosteroids have a slower onset with a longer anti-inflammatory effect. Particulate corticosteroids include triamcinolone, methylprednisolone and betamethasone acetate and are insoluble in saline, local anesthetic and iodinated contrast agents,8 whereas non-particulate corticosteroids such as betamethasone sodium phosphate and dexamethasone are soluble in all agents.8 Of the corticosteroids, methylprednisolone is the largest in size while betamethasone is the smallest.8
The evidence for the three types of epidural steroid injections and analysis of the literature will serve as the foundation to provide recommendations and guidelines for each type of injection. There have been 48 systematic reviews and 42 RCTs examining the efficacy of epidural steroid injections in the management of chronic spinal pain.9 These studies have suggested that epidural steroid injections have clear but often not long-lasting reduction in chronic spinal pain.9 The most recent and authoritative of these systematic reviews was performed by Manchikanti et al. This review outlined the efficacy and the evidence-based recommendations for conditions treated with epidural injection therapy. Additionally, this review comprehensively evaluated the efficacy of each epidural treatment approach (caudal, interlaminar, transforaminal) for given spinal indications (disc herniation, lumbar spinal stenosis, etc.). Given the comprehensive nature and recency of that review, we will briefly summarize the results from that manuscript as: 1) no new studies were identified in our search process and 2) there have been numerous authoritative reviews of this modality.
Interlaminar Epidural Steroid Injection
The Manchikanti review identified 13 high-quality RCTs evaluating the efficacy of interlaminar steroid injections. Ten studies were rated as high quality. The review concluded that there is Level I evidence treatment of lumbar disc herniation with interlaminar epidural steroid injections and Level II evidence for the treatment of lumbar spinal stenosis and axial/discogenic pain. The manuscript also suggests that overall the treatment effect has been rated as significant with the exception of systematic reviews with methodological flaws. These reviews were not specified. No new or additional studies were identified in our review process in the interval between publication of the Manchikanti study and the preparation of this manuscript.
Transforaminal Epidural Steroid Injection
In the Manchikanti review, there were 13 high-quality RCTs evaluating the efficacy of transforaminal epidural steroid injections. The majority of the studies examined the efficacy of transforaminal approaches in the setting of disc herniation. The evidence synthesis suggested Level I evidence for transforaminal injections in the setting of disc herniation and Level II evidence in the setting of lumbar spinal stenosis.
Caudal Epidural Steroid Injection
In the Manchikanti review, there were ten high-quality RCTs meeting inclusion criteria. Two compared caudal epidural injections to interlaminar and transforaminal injections in the management of disc herniation, while one study compared transforaminal injections to caudal injections in the management of lumbar disc prolapse. The remaining studies evaluated treatment of spinal stenosis, axial back pain or post-surgery syndrome. None of the RCTs were placebo controlled. Using the criteria methodology from that review the following conclusions were drawn concerning caudal epidural steroid injections: Level III evidence that caudal and interlaminar approaches are equivalent, Level II–III evidence for treatment of lumbar spinal stenosis with caudal approaches, Level II in post-surgery syndrome, Level III evidence that transforaminal approaches are superior to caudal approaches.9
Evidence Summary
For epidural interventions, RCTs and observational studies with functional status improvement measures were included. Short-term relief was defined as less than six months whereas greater than six months was considered long-term relief. The ASPN consensus guideline committee reviewed the 36 RCTs mentioned above as being of high quality. No additional studies were identified in our search process. For epidural interventions, there was sufficient evidence in the form of RCTs (Table 3), for the committee to make recommendations. Table 4 summarizes those recommendations.
 |
Table 3 Evidence Summary for Epidural Steroid Injections |
 |
Table 4 ASPN Back Consensus Group Recommendations for Epidural Steroid Injections |
Trigger Point Injections
For trigger point interventions, there was sufficient evidence in the form of RCTs for the committee to make recommendations. A review of RCTs regarding TPIs has revealed 25 studies investigating the efficacy of these injections for myofascial pain syndrome (MPS) with diverse medications. Over 40 RCTs were found through a PubMed literature search for “trigger point injection” that studied trigger point injections (technical variations, adjuncts for MPS treatment, and in comparison to other treatments for MPS). Given the volume of RCTs available, a focus was placed on literature published within the past five years with a focus on further studies outside this time frame to evaluate and clarify points made.
MPS is a soft tissue pain condition, characterized by a localized taut band of muscle that can cause acute or chronic pain.10 This condition is clinically diagnosed by identification of the characteristic taut bands on physical exam and a history indicative of myofascial pain, although objective means for diagnosis are often costly and not widely available. Diagnostic criteria defined by Simons et al are often referenced when describing the features of trigger points including the presence of taut bands, tenderness from taut bands, reproducibility of pain, local twitch response, restricted range of motion, autonomic symptoms, and referred pain.11 Palpation of an active trigger point can cause referred pain through activation of the central nervous system along with the distribution of the nerve innervating the muscle that is activated.12 Once diagnosed, MPS is treated by a variety of modalities including pharmacologic therapies (namely nonsteroidal anti-inflammatory drugs), therapy (including dry needling and acupuncture), and trigger point injections (TPIs).
Indications and Contraindications
TPIs should be considered in patients after thorough evaluation has ruled out other causes of back pain including muscle strain, facetogenic back pain, discogenic back pain, vertebrogenic back pain, spinal cord stenotic disease, vertebral body disease (including fracture), and radicular back pain. Once MPS has been diagnosed with the criteria outlined by Simons et al,11 patients can be trialed with conservative management, including pharmacologic therapy and physical therapy. If MPS persists and taut bands are identified, it is reasonable to perform TPIs. Contraindications for the procedure include patient refusal, infection overlying the site of injection and concurrent use of specific anticoagulants and anti-platelet medications.13
Safety/Complications
Though relatively safe as TPIs are generally performed with large gauge short needles by anatomic technique through identification of taut bands by physical examination, they are occasionally associated with complications specific to the region at which the injections are performed, namely the cervical and thoracic region. A 2004 study by Fitzgibbon et al characterized 5475 claims from the American Society of Anesthesiologists Closed Claims Project between 1970 and 1999 for chronic pain, with the authors determining that 284 pain management-specific claims (5.1%) were made with 276 of these claims (5.0% of total claims, 97.1% of pain management claims) were for invasive procedures.14 Of those claims, 138 (50%) involved injections (50%), including 17 claims for TPIs (6.1% of pain management claims, 12.3% of injection-specific claims). Interestingly, when assessed for complication type, 18 incidences of pneumothorax were reported with injections out of 59 total from all of the pain management associated claims (30.5%), of which 15 were associated with TPIs (83.3% of all injection associated pneumothoraxes; 88.2% of all TPI-associated claims).14
A review of the literature regarding complications of TPIs reveals a general dearth of publications, although a number of reports of complications associated with dry needling and acupuncture have been published. One of the first articles addressing TPI-associated complications of pneumothorax was published by Shafer in 1970.15 Subsequently, several additional case reports have been published, including one by Ahiskalioglu et al, in which a patient developed pneumothorax following cervical and thoracic TPIs.16 In their report, a 25-year-old 45 kg female received TPIs to her trapezii, supraspinatus, levator scapulae, and rhomboideus muscles with subsequent development of pneumothorax.16 Fortunately, this episode was self-resolving through conservative care and close follow-up. Paik et al published a case report in which a CT-guided aspiration was required for a 25-year-old female who developed a right-sided pneumothorax following a right trapezius TPI.17
Local anesthetics are often used for TPIs, and there is also a risk of reversible myotoxicity. In a review by Zink et al examining reports of histologic changes of skeletal muscle upon exposure to various local anesthetics (procaine, carbocaine, lidocaine tetracaine, chloroprocaine, bupivacaine) suggested that all local anesthetics studied resulted in some degree of reversible myotoxic effects in experimental models. However, few reports of clinical myotoxic reports have been published.18 No incidences of bowel perforation or pneumoperitoneum associated with TPIs were found through a thorough literature review. TPIs are considered a low-risk procedure and one should abide by the multi-specialty, multi-organizational guideline publication on peri-procedural antiplatelet and anticoagulant management for interventional spine and pain procedure when performing these injections.13
Evidence Summary
A review of RCTs regarding TPIs has revealed several studies investigating the efficacy of these injections for MPS with diverse medications. Over 40 RCTs were found through a PubMed literature search for “trigger point injection” that studied trigger point injections (technical variations, adjuncts for MPS treatment, and in comparison to other treatments for MPS). A focus was placed on literature published within the past 5 years with a focus on further studies outside this time frame to further evaluate and clarify points made by recent studies (Tables 5 and 6).
 |
Table 5 Evidence Summary for Trigger Point Injections |
 |
Table 6 ASPN Back Consensus Group Recommendations for Trigger Point Injections |
Facet Interventions
Facet interventions have a long history of clinical effectiveness, and there are multiple systematic reviews examining the efficacy of the technique. The current section will review recent efficacy studies with an eye toward answering several relevant clinical questions concerning facet intervention such as the role of articular injections vs RFA, facet intervention and medical management, risk mitigation for intra-arterial injection and prognostic value of diagnostic blocks.
Lumbar facet joint pain is one of the most common types of axial back pain. Its prevalence varies greatly in the literature, with estimates of prevalence ranging from as low as 4.8% to over 50%.19–22 Many of the studies investigating prevalence have been methodologically flawed. The wide disparity in reported prevalence demonstrates the need for standardized criteria on how to properly diagnose lumbar facet pain. In addition, there is a poor correlation between lumbar facet joint pathology on imaging and LBP.23 Numerous questions have been raised regarding the ideal cutoff for determining whether a diagnostic block is positive, how many blocks should be performed before considering radiofrequency ablation (RFA) and the volume of local anesthetic that should be injected.24–29 Lumbar facet interventions are the second most commonly performed procedures for chronic pain, yet there is still controversy regarding their effectiveness.30,31 While most reviews concluded that RFA is effective for lumbar facet joint pain,32–35 some studies dispute this.31,35 Facet blocks, including intra-articular and medial branch blocks, are frequently used prior to radiofrequency ablation. Cohen et al36 in the FACTS, RCT discussed effectiveness of lumbar facet joint blocks and predictive value prior to the procedure. This randomized study established the lack of long-term therapeutic benefit for intra-articular and medial branch facet blocks but suggested the possibility that when used as prognostic tools, these injections may provide superior outcomes prior to RFA on some measures compared to control blocks. For intra-articular injections, most reviews have concluded that the injections are ineffective,31,32,34,37,38 although some studies indicate they may provide some benefit compared to sham and conservative treatment.39–41
Consensus practice guidelines on interventions for lumbar facet joint pain developed by a multispecialty, international working group42 concluded that lumbar medial branch RFA may provide benefit to well-selected individuals, with medial branch blocks (MBB) being more predictive than intra-articular (IA) injections. More stringent selection criteria are likely to improve denervation outcomes, but at the expense of more false-negatives,42 potentially missing many patients that could benefit from RFA procedures. Physical examination signs such as tenderness over the facet joints, lumbar paraspinal tenderness and increased pain with trunk extension can help improve diagnostic accuracy. However, most reviews and guidelines do not support positive physical examination requirements for a diagnosis of lumbar facet pain,43,44 but rather favor diagnostic injections as the only reliable means for diagnosing it. Physical examination such as palpation of the lumbar spine under fluoroscopy and recognizing pain referral patterns can help determine the levels at which a diagnostic block can be performed. Regarding imaging studies such as scintigraphy, magnetic resonance imaging (MRI) and CT, there is weak or no evidence supporting the use of these imaging modalities for identifying painful lumbar facet joints prior to MBB or IA facet joint injections.45,46 Although there is insufficient evidence regarding the optimal timing of facet joint blocks for chronic LBP, or the duration of conservative treatment prior to consideration of facet injections, 3 months of conservative therapy prior to considering facet interventions is typically considered acceptable Compared with saline controls, both IA and medial branch injections with a local anesthetic (LA) provide better predictive information for medial branch RFA.36 Despite the lack of large prospective studies comparing the prognostic value of MBB and intra-articular facet injections as a screening procedure prior to RFA, some studies32,47,48 concluded that medial branch blocks are superior to intra-articular facet injections in predicting the success of RFA and should be the preferred screening method. Intra-articular injections of corticosteroids may, however, be used as a therapeutic injection for certain patients with suspected inflammatory pain, and in those who want to avoid ablative therapies, such as young athletes.49,50
The volume of the injectate for MBB and IA facet injections remains a subject of debate. Injecting excessive volumes can lead to spread of the injectate to adjacent structures such as the epidural space, spinal nerves, musculature and ligaments, undermining the specificity and positive predictive value of RFA. In addition, injecting insufficient volumes can lead to capsule distension and rupture in cases of IA injections. There are no studies evaluating the prognostic effect of the injectate volume on RFA outcomes. For MBB, there are several studies evaluating the efficacy of lumbar facet MB RFA using different volumes36,51–53 such as 0.3 mL, 0.5 mL, 0.75 mL and 1 mL with no difference in outcomes based on injectate volume. For IA injections, the joint capsule volume ranges from 1mL to 2 mL.54 Different volumes have been used in different RCTs examining the prognostic value and efficacy of IA injections. Large injectate volumes may result in rupture of the joint capsule and inadvertent spread to other potential pain generators, thereby undermining specificity. On the other hand, insufficient volumes may fail to anesthetize the joint, leading to false-negative blocks. In short, the accepted consensus is to use a volume of 0.5 mL–1.0 mL for MBB to reduce spread to adjacent structures and a volume of less than 1.5 mL for IA injections to prevent capsular rupture and spread to adjacent structures. Adding steroids to the injectate for MBB and IA injections for diagnostic purposes should be avoided. Many studies provide evidence against the use of intra-articular steroids.36,55,56
In Phase I of a three-arm double-blind study that compared IA LA and steroid lumbar facet injections, MBB with LA and steroid, and saline control blocks, Cohen et al36 found no significant differences in any outcome measure at any time point in the 6-month follow-up. Based on a review of evidence, the routine use of therapeutic facet injections is not recommended. However, there are a few exceptions, such as patients who may be at risk of complications from RFA (young athletes, older individuals on anticoagulation therapy or with implantable cardiac devices). In those cases, it is reasonable to add steroids to a block for possible intermediate-term relief. The number of diagnostic MBBs before RFA remains a subject of controversy. The American Society of Interventional Pain Physicians (ASIPP) and the Spine Intervention Society (SIS) advocate for the use of two diagnostic blocks prior to RFA19,44 to minimize placebo effects and false-positive results. False-positive results can also be contributed to spilling of the injectate into surrounding structures, use of sedation, use of copious superficial anesthesia and resting while not performing normal activities following the block.32,57 There are several reasons for false-negative blocks, including intravenous uptake, failure to anesthetize the target nerve, inability to access the joint for IA injections, aberrant anatomy, procedure-related pain such as muscle soreness and spasm and opioid-induced hyperalgesia. The decision whether to perform a single block, double block or no blocks is based on weighing false-positive versus false-negative results. There exists evidence that the success rate for medial branch RFA will increase with the number of blocks, but this will occur at the expense of missing out on some patients with false-negative results who could have benefited from the RFA. The multispecialty, international working group42 advocates for the use of a single block prior to RFA. They concluded that dual blocks result in a higher subsequent success rate for medial branch RF, but that the use of no diagnostic MBB results in the highest overall number of patients with a positive response to the RFA, thereby making a single block the “middle ground” option. They concluded that the decision to either proceed straight to RFA, performing a single block or double blocks can be tailored to the clinical scenario. Another debatable subject is the cutoff that should be used to consider a block as successful. Several studies compared outcomes of RFA based on percentage of relief from MBB, using different cutoffs including 50%, 80% and 70%.24,48,58–63 A 50% or greater cutoff is generally the most accepted model. In addition, other parameters to measure functional improvement should be considered when assessing the success of a diagnostic block.
Indications and Contraindications
Lumbar facet MBBs and intra-articular facet injections are indicated in the diagnosis and possible treatment of LBP due to lumbar facet joint pathophysiology. Chronic facet pain due to osteoarthritis (OA) has been associated with degenerative disc disease (DDD). DDD results in concomitant changes in the facet joints, and the reverse is also true: degeneration and motion abnormalities of the facet joints can accelerate disc degeneration. DDD usually precedes facet joint arthritis, and it is well noted that facet arthropathy is more prevalent at spinal levels with advanced DDD. Other conditions other than facet OA may cause facet-induced pain. Inflammatory arthropathies such as rheumatoid arthritis, ankylosing spondylitis and reactive arthritis can use lumbar facet pain. Other less common conditions such as pseudogout, synovitis, chondromalacia facetae and infection can also cause facet pain. Facet synovial pseudocysts can cause axial back pain as well as possible radicular pain due to compression of adjacent structures. Severe trauma such deceleration injuries and motor vehicle accidents can cause dislocation of the lumbar facet joints and lumbar facet pain following the trauma. Contraindications include patient refusal, ongoing active infection, and allergy to the medications used. Coagulopathy and patients on anticoagulants should be assessed prior to performing these interventions. Benefit versus risk analysis should be performed for those patients prior to proceeding with the injection.
Complications
The risks and complications from lumbar facet injections can be due to vascular penetration and injury, injection, procedure-related pain and injury to non-target neural structures. The incidence of vascular penetration and positioning of the needle intravascularly varies from 3.6% to 20%.64–69 A multispecialty, international working group42 and other societies such as SIS recommend checking for intravascular placement of the needle tip by aspirating and visualizing the spread of contrast on fluoroscopy in real-time prior to performing MBBs to reduce false-negative results. This should ideally be done in a manner such that the total injectate dose (LA and contrast) is kept as low as possible to minimize the effect on local anesthetic dispersion.42 Most societies recommend continuation of non-heparin anticoagulants prior to lumbar facet MBBs, as the risk of discontinuation of those medications such as development of thromboembolic events outweighs the benefits. Post-procedural pain can lead to false-negative results for the prognostic MBB, particularly in patients experiencing opioid-induced hyperalgesia. Manchikanti et al68 found that irritation of the nerve roots occurred in 0.1% of patients but found no long-term neural deficits out of 3162 MBBs performed. Proper use of fluoroscopic or CT guidance is recommended for MBBs and IA facet injections, although ultrasound guidance can be used by physicians highly skilled and experienced in ultrasound. Proper formal training in interventional pain procedures is recommended for physicians performing MBBs and IA facet injections to avoid complications and improve outcomes.
Evidence Summary
A review of RCTs for facet joint injections reveals several studies investigating the efficacy of these injections for LBP. A PubMed literature search yielded 11 RCTs evaluating lumbar facet injections and/or medial branch blocks for LBP during the literature review time period warranting inclusion. The focus was placed on literature published during this time period. Other landmark studies published outside of this time frame were also evaluated to clarify and support data from more recent studies. For facet interventions, there was sufficient evidence in the form of RCTs (Table 7), for the committee to make recommendations. Table 8 summarizes those recommendations.
 |
Table 7 Evidence Summary for Intra-Articular Facet Joint Injections |
 |
Table 8 ASPN Back Consensus Group Recommendations for Intra-Articular Facet Injections |
Two of the main questions regarding intra-articular facet joint injections are 1) do they replace radiofrequency ablation, and 2) do they delay the need for radiofrequency ablation.56,70 Most of the data suggests that intra-articular facet joint injections are not therapeutic, and they do not replace or delay the need for radiofrequency ablation.36,56,70 However, there are several studies that suggest otherwise. For example, Wu et al demonstrated that both autologous platelet-rich plasma and intra-articular steroid injections were effective for treating lumbar facet joint syndrome.71 In addition, Sae-Jung et al determined that methylprednisolone facet joint injections were effective for facet-mediated LBP but augmented with the addition of diclofenac.72
Intradiscal Regenerative Therapies
The intervertebral disc plays a crucial role in the health of the spine complex. Several pathologies of the disc itself, including internal disc disruption, tears, degeneration, and loss of height can all predispose patients to discogenic back pain and its sequelae. The disc is a central part of the interconnected biomechanical system of the spine, which allows for mobility and distribution of stress. Degeneration often correlates with loss of disc height that can lead to excess motion and instability. While this review will focus on treating pain originating from the disc itself, damage to the disc may lead to excess forces and subsequent damage throughout the spine.
The disc is a sensitive environment as it depends on diffusion for nutrients and waste movement due to its avascular nature at baseline. This diffusion capacity is relatively poor and worsens with both increasing age and pathology. In healthy discs, nerve endings are limited to the outer one-third of the disc and are not found in the inner annulus or nucleus pulposus region.73 In degenerated discs, nociceptive nerve fibers along with vasculature may migrate into the central disc regions.74 It is theorized that neurotransmitters together with changes within the extracellular matrix itself and the release of cytokines regulate this nerve ingrowth. In addition, pain-related peptides and proinflammatory cytokines are increased.
A common cause of disc failure is overloading in which forces may lead to desiccation of the disc and annular tears. The disc itself has a limited compression capacity which worsens with decreasing fluid content. To improve disc failure, the premise is to regain or maintain disc height to reduce the axial nerve compression and to restore the tissue dynamics (fluid content) of the annulus. A second goal is to possibly reconstitute the central nucleus with a matrix environment that can hold fluid and improve nutritional flow. Using regenerative medicine, the hope is to improve the damaged internal environment of the disc by reconstituting a matrix that may improve and return disc function.75
Indications
Intradiscal regenerative medicine has primarily been studied in patients with intractable chronic LBP for at least 3–6 months despite failure of a multi-modal treatment approach including indicated medications, physical therapy, and other interventional procedures as per recommendation guidelines. Patients should have history, physical exam, and radiologic findings consistent with their symptomatic lumbar intervertebral discogenic pain. Provocative discography can further specify the source of pain and the precise level(s) to treat.
Safety and Complications
The overall safety profile of regenerative therapies is excellent and comparable to standard intradiscal procedures. Rare adverse events may include LBP, muscle spasms, and discitis. Standard intradiscal precautions should be taken with an emphasis on sterile technique in both the preparation of the injectate and the intradiscal procedure itself. To further illustrate this significance, a case of spondylodiscitis with positive Cutibacterium acnes culture has been reported subsequent to platelet-rich plasma (PRP) intradiscal injections. The authors stressed the importance of appropriate sterile technique and risk-stratification of patients with high infection potential, as well as better understanding of intradiscal biologic therapies and the intradiscal environment.76 Traditional antibiotic therapy protocols for intradiscal interventions may benefit from further review specifically regarding regenerative medicine.
Evidence Review with Evidence Level Designation: Intradiscal Regenerative Therapies
It is important to understand that not all biologics used in regenerative medicine are equivalent. For instance, factors at a minimum that can affect the final PRP product include volume of blood aspirated, baseline platelet count, patient health status and comorbidities, patient medications, anticoagulant of choice, centrifugation parameters, and inclusion/exclusion of leukocytes. Similarly, mesenchymal stem cells (MSCs) are found in most tissues of the human body but primarily sourced for reimplantation from the bone marrow and adipose due to ease of access. Volume of aspirate, patient health status and comorbidities, patient medications, harvesting protocol parameters and technique can all affect the final MSC product. Not distinguishing this heterogeneity, we have summarized the gross clinical evidence evaluating regenerative medicine for LBP from discogenic pathology, including prolotherapy, protein-rich plasma (PRP), cellular therapy, and other intradiscal injectates (Table 9).
 |
Table 9 Evidence Summary for Intradiscal Regenerative Therapies |
Evidence Review with Evidence Level Designation: Prolotherapy and Platelet Rich Plasma
Prolotherapy is among the earliest studied regenerative medicines. There have been several prospective and retrospective trials and case reports studying PRP, although only one published RCT. A prospective, double-blind, randomized controlled trial by Tuakli-Wosornu et al in 2016 investigated intradiscal PRP for treatment of chronic moderate to severe lumbar discogenic pain unresponsive to conservative treatment and confirmed with discography. Twenty-nine patients received intradiscal PRP with the control group consisting of 18 patients who received only intradiscal contrast. Over 8 weeks of follow-up, there were significant improvements in participants who received the intradiscal PRP with regard to pain, function, and patient satisfaction compared with the controls.77 Furthermore, those who received PRP were able to maintain significant improvements in the Functional Rating Index for at least 1-year follow-up. In 2019, Cheng et al performed a 5-to-9-year follow-up on the same patients from the aforementioned RCT by Tuakli-Wosornu et al. From the PRP intervention group, 21 of the 29 original patients were able to be included in this follow-up study. Seventy-one percent were classified as successes as they demonstrated both clinical and significant improvements in pain and function. The remaining 29% of patients required spinal surgery and were classified as failures. This study further supports improvements in pain and function post-intradiscal injection of PRP sustained for follow-up periods of 5–9 years following intradiscal PRP treatment for moderate-severe lumbar discogenic pain.78
Cellular Therapy
Several case series and prospective studies have investigated the use of intradiscal autologous stem cells for lumbar discogenic pain. Overall, there is moderate evidence, including that from two relatively small size RCTs, supporting intradiscal allogeneic mesenchymal stem cells in the treatment of discogenic LBP. Regarding human umbilical cord tissue-derived mesenchymal stem cells, there is a single study of small sample size producing low evidence in its support.
In 2021, Beall et al published one-year results of the VAST RCT investigating the clinical relevance of treating painful intervertebral disc tissue by supplementary transplantation of viable cellular allograft disc matrix. This structural allograft is prepared from human nucleus pulposus allograft that contains allogeneic viable cells. A minimum of 6 × 106 cells were suspended in each allograft matrix suspension. This prospective, randomized, parallel-arm, multicenter study enrolled a total of 218 subjects who demonstrated clinical disc degeneration of 1 or 2 vertebral levels from L1 to S1 and Pfirrmann levels 3 through 6 on MRI. The cellular allograft group was compared to saline placebo or continued treatment with nonsurgical management in a 3.5:1:1 randomization. At 12 months with a total of 182 subjects completing the study, clinically meaningful improvements in mean visual analog scale of pain intensity (VASPI) and ODI scores were achieved in both the investigational allograft and saline groups. A responder analysis demonstrated a clinically meaningful reduction in ODI of ≥15 points at 12 months that was statistically significant in favor of the allograft group (76.5%) compared to the saline group (56.7%). The supplementation of the disc with viable allograft was able to produce a marked reduction in pain, an improvement of function, and a safety profile similar to traditional discography. Although the saline control placebo group also was able to demonstrate improvements, as previously suggested in prior studies, intradiscal saline may have some therapeutic advantage in itself and thus likely is an active comparator rather than a neutral placebo control.79,80
Cellular Therapy: Other Intradiscal Injectates
Methylene blue has been studied by an RCT by Peng et al in 2010. Seventy-two subjects with discogenic LBP were randomized: 36 of whom received 1 mL of 1% methylene blue followed by 1 mL of 2% lidocaine, and 36 in the placebo group received 1 mL of isotonic saline followed by 1 mL of 2% lidocaine. The authors of this single study concluded that the injection of methylene blue into the painful disc is a safe effective and minimally invasive method for the treatment of intractable and incapacitating discogenic LBP.81
Fibrin is another injectate that has been trialed to treat discogenic pain. In 2014, Yin et al reported on 15 adults with confirmed discogenic pain who underwent intradiscal injection of a fibrin sealant. Eighty-seven percent of the subjects achieved at least a 30% reduction in low back pain VAS compared with baseline at the 26-week primary end point without significant adverse events. Although this was not an RCT and only evaluated 15 patients, fibrin may provide benefits in certain patients. Fibrin is composed of purified prothrombin and fibrinogen and reconstituted with aprotinin and calcium. When injected into the annular tears, it has the ability to form a matrix sealant that protects the nucleus pulposus.82
In an attempt to further define the evidence for intradiscal treatments, a post hoc comparison in 2020 by Ju et al aggregated single-site data from 4 separate multicenter RCTs [Study A: Growth factor BMP-7 (n = 15); Study B: active fibrin sealant (n = 10); Study C: Growth Factor rhGDF-5 (n = 3); Study D: cell-based stem cell treatment MPC-06-ID in HA (n = 10); and saline control group (n = 12)]. While there was both a significant decrease in VAS pain and an improvement in patient reported disability scores, the authors concluded there was no significant difference between the investigational group of biologics and the saline control group. The authors suggested that perhaps saline injection itself has a therapeutic effect, possibly by diluting pro-inflammatory mediators within the degenerated disk, decreasing intradiscal pressure, or a combination of the placebo effect. The small sample sizes and heterogeneity of combining multiple studies make it difficult to draw conclusions from this study83 (see Table 9 for evidence summary).
Therapy Grading
Intradiscal regenerative therapy is burgeoning area of research and intervention. Different than interventions in the previous sections that have established histories with decades of experience, this intervention category is relatively recently introduced into the lexicon of therapeutic intervention. As a result, there is one RCT and several observational studies and case series which are utilized to form recommendations. Table 9 summarizes the current literature on this family of interventions and Table 10 summarizes those recommendations. There is evidence for the use of intradiscal PRP in the form of a single RCT, and several prospective observational studies and case series for both autologous bone marrow and adipose tissue-derived mesenchymal stem cells, as well as allogeneic mesenchymal stem cells and cellular allograft disc matrix for the treatment of persistent lumbar discogenic back pain. It is important to discern that the primary patient populations studied have previously failed the multidisciplinary standard of care. Regenerative Medicine holds the potential to provide an alternative intervention for these patients whose pain persists despite the recommended conservative management. In these selected patients, intradiscal biologics may improve pain and function without the need for advanced surgical treatments that can impair the spine’s native biomechanics (Table 10).
 |
Table 10 ASPN Back Consensus Group Recommendations for Regenerative Therapies |
Sacroiliac Joint Injections
The sacroiliac joint (SIJ) is a diarthrodial synovial joint with abundant innervation from the lumbosacral nerve roots.84,85 The joint itself is approximately two-thirds synovial and one-third ligamentous, with the synovial portion extending anterior and inferiorly and reinforced at its posterior and superior aspect by syndesmotic ligament.86 The sacroiliac joint is accepted as a relatively common source of low back and/or buttock pain with or without lower extremity pain. The sacroiliac joint has been implicated as the primary pain generator in 10% to 27% of low back pain cases.87,88 SIJ dysfunction more commonly occurs with degenerative conditions or with an imbalance between the two SI joints; therefore, patients at increased risk for SIJ pain include those with leg length discrepancy, advanced age, inflammatory arthritis, pregnancy, trauma, and previous spine surgery.89
There are no definite historical, physical, or radiological features to provide a definite diagnosis of sacroiliac joint pain.90–92 A systematic review by Szadek et al evaluated the diagnostic validity of the International Association for the Study of Pain (IASP) criteria for sacroiliac joint pain and concluded that the thigh thrust test, the compression test, and 3 or more positive stressing tests contain sufficient discriminative power for diagnosing sacroiliac joint pain.93
There are many therapies for SIJ dysfunction, with the most common and often first step in therapy algorithms being SIJ intra-articular injections, which can be utilized both diagnostically and therapeutically.94
Indications and Contraindications
Diagnostic intra-articular SIJ blocks and therapeutic intra-articular SIJ blocks have their own specific roles in the diagnosis and therapy of SIJ-mediated pain. A thorough history and physical examination including provocative tests are performed for an accurate diagnosis. Typically, if a patient has a positive response to 3 or more SI joint provocative tests, a positive outcome of a diagnostic SI joint block can be predicted.93 However, SIJ diagnostic injection is then indicated, as it is a true confirmatory test.95,96 In diagnostic blocks, an anesthetic is injected into the posterior SIJ under fluoroscopic guidance, and if there is a certain degree of pre-defined pain relief following the diagnostic injection for the duration of the anesthetic, then the diagnosis of SI joint dysfunction can be established.97,98
Therapeutically, a local anesthetic is combined with a corticosteroid medication to provide pain relief in the SI joint. Therapeutic SI joint injections can be intra-articular or periarticular, and a growing body of research suggests that intra-articular therapeutic injections are superior to periarticular injections.98,99 Absolute contraindications of SI joint injections include patient history of allergy to cortisone injections, and local malignancy. Relative contraindications include coagulopathy, current, uninterrupted use of blood thinning agents, pregnancy, systemic infection, septic joint, osteomyelitis, and poorly controlled diabetes.100–102
Safety and Complications
The largest study to date on SIJ adverse events indicated that there were very low numbers of adverse effects secondary to SIJ injections, with 3% (5/191) of patients experiencing immediate transient reactions and 24% (32/132) with delayed adverse reactions, the most common being increased pain.103 There are rarer but more serious complications reported in the literature including trauma to the nerves, accidental intervertebral foraminal injection, hematoma, sciatic palsy, meningitis, abscess, and systematic infection.104–106 Another study determined that 2.5% of 525 SIJ injection resulted in a vasovagal reaction, and there have been case studies illustrating very rare complications such as herpes reactivation or pyogenic sacroiliitis.107–109 Temporary sciatic palsy was reported in two studies, with 3/67 cases in one and 5/60 in the other.110,111 One of the major complications of the procedure is that many were technically unsuccessful, with rates of 10–20%.112
The most recent data on SIJ blocks, both diagnostic and therapeutic, was compiled to guide the below best practice guidelines. Image guidance for SIJ injections has been found to be very important in multiple studies.113–116 A study determined that in patients who underwent SIJ injections without image guidance, intra-articular needle placement was confirmed in only 22% in subsequent computed tomography (CT) scans.113 In another study of “blind” injections, only five of 60 needles closely approximated the joint, and none had proper intra-articular placement.114 Ultrasound and CT can also be used for image guidance.115 However, ultrasound cannot verify intra-articular placement of the injectate, and was found to be inferior to fluoroscopic guidance in a prospective, randomized, single-blinded study.116 CT guidance can also be utilized but has been found to be less effective than fluoroscopy at capturing the escape of injectate from the joint to adjacent structures, and neither ultrasound nor CT guidance can rule out concurrent intravascular flow.113
Diagnostic intra-articular SIJ blocks remain the gold standard for establishing a diagnosis of SIJ pain.114 The positive response of intra-articular diagnostic injections is a complete or near complete relief of pain. Various studies have set different levels of pain relief as the threshold needed for a positive test, ranging from >70% pain relief to >50% pain relief from the diagnostic block.93,115,117,118 The studies that utilized >70% pain relief as the threshold for an accurate diagnostic block had a smaller number of subjects and therefore were more specific for diagnosis for SIJ-mediated pain.119 The most important criteria, however, found across multiple studies, was the use of a single positive, diagnostic block versus dual positive, diagnostic blocks.109,120–126 Utilizing dual controlled blocks significantly decreases the positive response rate, with dual blocks reporting rates of positive SIJ pain diagnosis from 10 to 40% whereas single control blocks produced 29–63% positivity rates of SIJ pain.109,120–126 Therefore, it has been demonstrated that diagnostic accuracy is at Level II for dual diagnostic blocks, with at least 70% pain relief as the criterion standard and Level III for single diagnostic blocks, with at least 75% pain relief as the criterion standard.109,120–126
There have been only two randomized controlled trials, one in which therapeutic SIJ injection was completed utilizing a steroid versus utilizing saline in patients with ankylosing spondyloarthropathy. Those receiving a steroid experienced a mean VAS score decrease from 6.8 to 1.3 compared to the decrease in saline VAS score from 7.0 to 5.2, with a 50% decrease in NSAID use in the steroid group and 14% relief in the saline group, as well as 1 month pain relief sustained in 5/6 patients in the steroid group and 1/6 in the saline group.110 While of small sample size, these data demonstrated statistically and clinically significant improvements with steroid injection versus placebo. However, Kim et al, who compared prolotherapy to therapeutic SIJ injection, found that 27.2% of subjects achieved 50% pain relief in the steroid group at 6 months and 63.6% of those in the prolotherapy group achieved 50% pain relief. This was repeated at 15 months, with 10.2% in the steroid group achieving significant pain relief compared to the prolotherapy group, in which 58.7% of patients experienced sustained pain relief.127 However, the study is significantly flawed, and confounded in that many subjects received varying numbers of injections that were not reported.128 The remainder of studies focused on therapeutic SIJ injections were all observational, either prospective or retrospective. Three studies utilized the criteria of 2 positive diagnostic blocks to select patients who received the therapeutic steroid SIJ injection. In these 3 investigations, 45–67% of study participants reported at least 50% pain relief at 4 weeks.129–131 There have been numerous studies in which patients were selected for therapeutic SIJ injections after one positive diagnostic block. These results varied far more significantly likely due to these studies utilizing a heterogonous set of diagnostic criteria, follow-up times, and outcome measures. As mentioned above, patients diagnosed with SIJ pain based on the results of only a single diagnostic block demonstrated greater variability in their responses than those diagnosed via dual controlled blocks.109,120–126 The studies utilizing single blocks as diagnostic criteria reported an average duration of pain relief from their therapeutic injections ranging from 76 to 94.4 days, with the percentage of patients receiving relief from their therapeutic injections ranging from 23% to 78%.110,127–131
Evidence Summary
For sacroiliac joint literature, there was sufficient evidence in the form of 2 RCTs and several observational studies (Table 11), for the committee to make recommendations. Table 12 summarizes those recommendations. SIJ dysfunction is a complex pain process with numerous proposed therapy options ranging from physical therapy to invasive surgery on the procedural continuum, SIJ injections are usually the first line in both diagnostic and therapeutic care.
 |
Table 11 Evidence Summary for Sacroiliac Joint Injections |
 |
Table 12 ASPN Back Consensus Group Recommendations for Sacroiliac Joint Injections |
Minimally Invasive Spine Procedures
Percutaneous Image-Guided Minimally Invasive Lumbar Decompression
Lumbar spinal stenosis (LSS) is a widely prevalent condition commonly seen in the elderly population.132 These patients typically present with myriad symptoms classified as neurogenic claudication. These symptoms may include lower back and leg pain/paresthesias, worsened by walking and usually relieved after rest.133 While most patients remain asymptomatic, it is estimated that approximately 10% population over the age of 70 will suffer from symptoms secondary to LSS.134 These chronic and disabling symptoms lead to impairment of patients’ quality of life. Among the several factors that may contribute to LSS, ligamentum flavum hypertrophy (LFH) is regarded as one of the most common causes in the elderly.135 Conservative measures including physical therapy, NSAIDs, and epidural steroid injections have demonstrated limited benefit in providing long-term symptomatic relief in these patients.136–139 Therefore, the treatment of spinal stenosis historically has been limited to open laminectomy with or without fusion, which can expose the patient to increased complications and an extended hospital stay. Percutaneous image-guided lumbar decompression (PILD) for lumbar spinal stenosis is a procedure in which specially designed instruments are used to percutaneously remove a portion of the lamina and debulk the ligamentum flavum. The procedure is performed under fluoroscopic guidance without direct visualization of the surgical area.
Indications
The PILD procedure is currently only indicated for the treatment of lumbar spinal stenosis secondary to ligamentum flavum hypertrophy. The following criteria should be met before a patient is considered a candidate for PILD:
- The patient has symptomatic LSS, ie, presence of neurogenic claudication.
- Confirmation of central/foraminal LSS secondary to LFH on imaging (MRI/CT).
- LFH ≥ 2.5mm.
Safety and Complications
The PILD procedure was designed as a minimally invasive procedure for the treatment of lumbar spinal stenosis secondary to ligamentum flavum hypertrophy. The efficacy and safety of the PILD procedure has been demonstrated in several level 1 clinical studies (Table 13), with recommendations in Table 14.
 |
Table 13 Evidence Summary for PILD in Spinal Stenosis |
 |
Table 14 ASPN Back Consensus Group Recommendations for PILD Injections |
Almost all clinical studies of PILD assessed patients for procedure-related complications including dural tears, nerve root injuries, bleeding, infections, and rehospitalization post-procedure. None of the studies identified any serious procedure/device-related complications. Minor procedure-related complications that were reported included soreness at the surgical site,140 minor post-operative bleeding,141 and minor intra-operative bleeding that was controlled with gel foam.142 All clinical studies demonstrated that the safety profile of the PILD procedure was equivalent to that of epidural steroid injections. Levy et al published the results of a multicenter systematic analysis conducted to evaluate the safety of PILD procedure.143 This review included 373 patients who underwent a PILD procedure. There were no major procedure- or device-related events reported. Schomer et al published the results of a meta-analysis conducted to compare safety and efficacy of PILD procedure to open lumbar decompression in patients suffering from lumbar spinal stenosis.144 SPORT (Spine Patient Outcomes Research Trial) surgical cohort patients were analyzed for efficacy and safety of standard lumbar decompressive laminectomy and were compared to PILD patients. While no significant differences were found between the two procedures in terms of efficacy, the complication rate in surgical cohort was significantly higher. To date, there have been no reports of serious device or procedure-related complications with the PILD procedure. In contrast, the SPORT surgical cohort reported complications in 9.9% patients, which included dural tears in 9.2% of patients, 9.5% patients required intraoperative blood transfusions, and 4.9% required postoperative blood transfusions. The study concluded that as a minimally invasive alternative to decompression surgery, PILD procedures yielded comparable patient outcomes with shorter procedure times, less blood loss, shorter hospital stays, and significantly better safety.
Evidence Summary
For percutaneous image-guided lumbar decompression, there was sufficient evidence in the form of three RCTs and several prospective observational studies (Table 13), for the committee to make recommendations. Table 14 summarizes those recommendations.
Stand-Alone Interspinous Spacers, Indirect Decompression
The first interspinous implant for the lumbar spine was developed in the 1950s by Knowles. Owing to flaws in design, material, surgical technique, and applied indications, its use was abandoned. The first modern interspinous device, the Wallis system, was developed by Abbot Spine in 1986 and was used primarily in patients with recurrent disc herniation.145 Since that time, many adaptations have been introduced to the market as either combination treatment with other surgical procedures or as stand-alone approaches. Traditionally, these interspinous implants were designed to be utilized via open techniques. In 2016, a stand-alone interspinous spacer for the indirect decompression of the lumbar spine was introduced commercially. The Superion device (Vertiflex, Inc., San Clemente, CA; percutaneous interspinous process device [IPD]) is a low-profile evolution of previous IPD systems that can be implanted percutaneously between symptomatic vertebral levels on an outpatient basis. This technique has a number of potential advantages and imparts results that parallel the open technique.146 Interspinous spacers have been designed to provide an alternative to open surgical decompression surgery with minimal surgical dissection. Indirect decompression of the spinal canal using an interspinous spacer is a minimally invasive procedure that can be performed in an ambulatory surgery center and has been shown to provide comparable clinical performance to decompressive laminectomy for management of symptoms of spinal stenosis.147,148
Indications and Contraindications
The effective utilization of the interspinous spacer relies upon the appropriate diagnosis of LSS. This should begin with a proper history and physical examination to rule out other sources of back pain. Patients must report symptoms of neurogenic claudication that abate with sitting down or leaning forward, referred to as the “shopping cart sign”. To confirm clinical suspicion of LSS, MRI or CT myelogram studies are required.149 In addition, lumbar x-rays including flexion/extension views should be performed in order to assess for spondylolisthesis and segmental instability.
The initial treatment of LSS consists of various nonoperative approaches including physical therapy, pain medications (NSAIDs, mild opioids), and epidural steroid injections, referred to as conservative care.150 Conservative treatment is generally recommended for 6 months prior to initiating more invasive treatments. Patients with symptoms refractory to sustained conservative medical management warrant surgical consideration.150 As mentioned, open decompression surgery has been associated with significant post-operative complications.
Standalone lumbar interspinous spacers are indicated to treat skeletally mature patients suffering from painful walking, numbness, and/or cramping in the legs (neurogenic claudication) secondary to a diagnosis of moderate degenerative lumbar spinal stenosis, with or without Grade 1 spondylolisthesis, as confirmed by advanced radiographic imaging. They are indicated for those patients with impaired physical function who experience relief in flexion from symptoms of leg/buttock/groin pain, numbness, and/or cramping, with or without back pain, and who have undergone at least 6 months of non-operative treatment. Interspinous spacers may be implanted at one or two adjacent lumbar levels in patients in whom treatment is indicated at no more than two levels, from L1 to L5.
For this intended use, moderate degenerative lumbar spinal stenosis is defined as follows:
- 25% to 50% reduction in the central canal and/or nerve root canal (subarticular, neuroforaminal) compared to the adjacent levels on radiographic studies, with radiographic confirmation of any one of the following:
- Evidence of thecal sac and/or cauda equina compression,
- Evidence of nerve root impingement (displacement or compression) by either osseous or non-osseous elements,
- Evidence of hypertrophic facets with canal encroachment.
And associated with the following clinical signs:
- Presents with moderately impaired physical function defined as a score of ≥2.0 on the Zurich Claudication Questionnaire (ZCQ),
- Ability to sit for 50 min without pain and to walk 50 feet or more.151
The interspinous spacers may be contraindicated in the following situations:
- Severe spinal stenosis with neurological deficits
- Multilevel (more than 2 levels of spinal stenosis)
- Spinal instability (>3mm of translation)
- Osteoporosis (high risk for spinous process fracture)
- Scoliosis (Cobb angle >17 degrees)
- Baastrup's disease
- Greater than grade I spondylolisthesis
- Previous lumbar surgery at the affected level
- Symptoms not relieved with forward flexion20
Safety/Complications
The device and device-related adverse effects (AEs) as reported during the RCT, post hoc analyses, and clinical registries performed to date are quite minimal. The most commonly reported minor, self-limiting post-procedure adverse events included incisional pain and transient worsening of back pain. The following device- or procedure-related events have been reported:
- 23 spinous process fractures
- 10 wound complications
- 2 infections
- 50 reoperations/revisions
Literature Summary
A review of literature revealed that there are 28 published peer-reviewed articles and 6 clinical studies published to date with direct patient data regarding the clinical efficacy of stand-alone interspinous spacers for LSS. The clinical studies include one RCT, 2 post hoc analyses of RCTs, an open-label follow-up on RCT study arms, and 2 prospective single-arm studies.
In 2015, Patel et al152 published results from a prospective, multicenter, randomized, controlled, investigational device exemption noninferiority trial. A total of 391 randomized patients were implanted with Superion (n = 190) or control (n = 201) spacers at 29 sites in the United States between August 2008 and December 2011. These patients returned for visits at 6 weeks and 3, 6, 12, 18, and 24 months. The primary endpoint of this study was a composite treatment success outcome at the 2-year follow-up visit, defined as (1) clinically significant improvement in at least 2 of 3 ZCQs, (2) freedom from reoperation, revision, removal, or supplemental fixation at the index level, (3) freedom from epidural steroid injection or nerve block at the index level within 12 weeks of the 2-year visit, (4) freedom from rhizotomy or spinal cord stimulator at any level, and (5) freedom from major implant or procedure-related complications. Secondary outcomes included leg and back pain severity assessed on a 100-mm visual analogue scale, ODI, patient satisfaction questions and adverse events classified by seriousness and relationship to the device and/or procedure. The primary composite endpoint of this study was met, which demonstrated that the Superion spacer was noninferior to the X-Stop spacer. Leg pain, the predominant patient complaint, decreased in severity by 70% during 2 years in each group. Most (77%) patients achieved leg pain clinical success (improvement ≥20 mm) at 2 years. Back pain clinical success (improvement ≥20 mm) was 68%, with no differences between groups. ODI clinical success (≥15% point improvement) was achieved in 65% of patients. The rates of complications and reoperations were similar between groups.152
Other peer-reviewed publications include literature reviews, a clinical registry, and a cadaveric biomechanical study. The literature reviews include topics such as cost-effectiveness, use in levels adjacent to the previous surgery, and algorithms for LSS treatment. For interspinous spacers, there was sufficient evidence in the form of RCTs and prospective observational studies (Table 15), for the committee to make recommendations. Table 16 summarizes those recommendations.
 |
Table 15 Evidence Summary for Interspinous Spacers, Indirect Decompression |
 |
Table 16 ASPN Back Consensus Group Recommendations for Interspinous Spacers, Indirect Decompression |
Percutaneous and Endoscopic Disc Procedures
Lumbar intervertebral discs provide a cushion between the vertebral bodies to allow the spinal column to tolerate a particular amount of compression on a regular basis. Despite their structural benefit, lumbar disc herniations (LDH) can be particularly problematic due to their predilection for nerve root compression based on anatomic location. These often manifest as an acute radiculopathy in a sciatic distribution with or without acute LBP. The prevalence of LDH is approximately 1–3%.153 Those who undergo 6 weeks of conservative therapy without significant improvement in symptoms are recommended to undergo surgical intervention to remove the herniated portion of the disc.154 The most common procedure to accomplish this task is the classic open microdiscectomy (MD). In this procedure, the lamina of the affected levels are exposed, a small laminotomy is made and a discectomy is performed with the aid of intraoperative microscopy. This procedure produces excellent short-term outcomes in a majority of patients.155,156 However, this procedure also has its potential pitfalls. As many as 10% of patients undergoing MD will experience a re-herniation of the remaining disc material.157 In addition, approximately 30% of patients experience LBP after surgery and 20% ultimately require a revision surgery.158,159
In an effort to reduce pain and complications associated with open MD, minimally invasive procedures have been developed over the years in hopes of achieving similar results. One of the first generations of minimally invasive surgery was percutaneous laser disc decompression. While this achieved good clinical results, further developments in technology have witnessed this technology’s use reduced over time.160–162 These developments in technology have mostly been with regard to that of visualization or approach techniques. In reference to visualization, this has typically involved an endoscope as opposed to a traditional microscope. Compared to the traditional open procedure, both percutaneous and tubular approaches have been developed in an effort to spare painful muscle dissection.163–168 As these new approaches have been developed, they have been tested against the gold standard of MD for both clinical results and complications.
This section discusses the available percutaneous, endoscopic and other minimally invasive options for lumbar discectomy and how they compare to the clinical outcomes and complication rates achieved in traditional MD.
Indications and Contraindications
Lumbar discectomy, in both its minimally invasive and more traditional open forms, is a procedure which targets the removal of a portion of an intervertebral lumbar disc which is herniated through the disc annulus or causing the annulus to bulge, ultimately leading to pressure on the traversing and/or exiting nerve root at this level. In the traditional open procedure, a laminotomy is usually created at the more cranial level of the disc herniation. The thecal sac and traversing nerve root are then retracted medially, and the herniated or bulging disc fragment is removed under microscopic magnification. In the more minimally invasive techniques, bony removal is often limited, if necessary at all. Visualization is often provided by an endoscope in an effort to limit the opening needed to perform such a procedure.
Lumbar discectomy is indicated in the following situations:
- Diagnostic testing (MRI, CT myelogram) which shows a herniated/bulging lumbar disc causing compression of the traversing nerve root, exiting nerve root or cauda equina
- Significant pain, weakness, numbness or paresthesias in an expected distribution based on the compressed nerve root
- Radiculopathy symptoms that are more significant than LBP symptoms
- Symptoms have not improved with upwards of 6 weeks of conservative management (NSAIDs, oral steroids, epidural steroid injections, physical therapy, etc.)
- Symptoms consistent with cauda equina syndrome (bilateral leg weakness, sensory disturbances in the genital and saddle region, loss of bowel/bladder control)
While multiple different interventions are possible with regard to lumbar discectomy, all of these procedures and devices have received approval from the FDA. Regarding contraindications to lumbar discectomy, the most significant is related to spinal instability. In patients with evidence of underlying instability, decompression alone can lead to worsening of this instability and further morbidity. Other contraindications which have been noted in the literature include calcified discs, painless weakness and pyogenic spondylodiscitis or other severe disc space infections. Specifically, endoscopic discectomy can be contraindicated in the setting of cauda equina syndrome and severe fibrotic adhesions. Also, regarding endoscopic discectomy, tubular discectomy and other percutaneous techniques, surgeon experience and level of training must be considered prior to proceeding.169
Safety and Complications
Most studies that have compared minimally invasive techniques for discectomy to more traditional open procedures have studied rates of complications between these two techniques. While minimally invasive techniques may lead to less post-operative pain for the patient, subjecting them to increased risk as a result of that technique would potentially reduce any benefit gained. Thus, careful investigation of differences in complications between these groups is of paramount importance.
In microendoscopic discectomy techniques, a number of studies have been completed with monitoring of peri-operative complications. Two particular complications which have been carefully monitored include reherniation of the disc and dural tear. Teli et al found higher incidence of both dural tears (8.7% v. 3%) and reherniation (11.4% v. 3.5%) in microendoscopic discectomy as compared to open procedures.170 However, other studies in which microendoscopic techniques were used have not yielded such results. In these other studies, similar rates of dural tears (approximately 7% in each group) and reherniations (approximately 2% in each group) were noted between microendoscopic techniques and more traditional open discectomies.171,172
Other studies which have reviewed microendoscopic, percutaneous and open discectomy techniques have identified minimal complications that were mostly transient in nature. These include dysesthetic pain, motor weakness, paresthesias and urinary retention. In all of the studies reviewed, the individual rate of these complications did not exceed 5% with regard to any of the above techniques. In addition, no serious adverse events, such as post-operative discitis, were noted.162,173–178 Overall, based on the available data, the procedures performed for lumbar discectomy can be performed safely, regardless of the technique used.
Evidence Review with Evidence Level Designation
A number of studies have been performed assessing discectomy procedures, as well as several reviews. Some studies have compared microendoscopic discectomy to open techniques.170–172 Others have compared microendoscopic techniques to percutaneous methods.173,174 Still, others have compared percutaneous techniques to open procedures175,176,179 and tubular methods to open procedures, as well.162,177,178 A number of systematic reviews and meta-analyses have also been completed which compared the above techniques, some focusing on efficacy while others on complications.180–183 While many studies of these procedures are available, for the purposes of this guideline, we limited our use to the most recent data available in an effort to provide the most accurate and up-to-date recommendation.
In summary, percutaneous and endoscopic disc procedures have a favorable safety and efficacy profile in terms of lumbar disc herniation with persistent radicular symptoms. Further research is needed to examine complication rates in regard to dural tears and re-herniation and evaluating methods to further decrease these rates of incidence for these techniques to supplant MD as standard of care. For percutaneous and endoscopic disc procedures, there was sufficient evidence in the form of RCTs (Table 17) for the committee to make recommendations. Table 18 summarizes those recommendations.
 |
Table 17 Evidence Summary for Percutaneous and Endoscopic Procedures |
 |
Table 18 ASPN Back Consensus Group Recommendations for Percutaneous and Endoscopic Procedures |
Interspinous/Interlaminar Fusion Devices
Degenerative lumbar spinal stenosis has many etiologies that can include hypertrophied ligamentum flavum, osteophytes, facet joint hypertrophy and degeneration of the disc space.184 Lumbar spinal stenosis and lumbar degenerative disc disease are often seen in conjunction and are largely products of each other.185 Treatment options for those with spinal stenosis and degenerative changes include conservative measures such as physical therapy, medications, and epidural steroid injections.186 The most common surgical options can include open laminectomy or decompression with or without transpedicular screw fixation.187 There are several limitations to these spinal surgical procedures including extended recovery and chronic back pain associated with post-laminectomy syndrome. These surgeries have also been associated with a higher incidence of adverse events such as cerebrospinal fluid leak, nerve injury, deep wound infections, misplaced hardware, and hardware failures.188,189 Lastly, there is concern regarding adjacent segment disease from altered biomechanics.190 Many of these factors limit the use of these procedures in those patients of advanced age, those with medical comorbidities, and those with mild or moderate findings. Minimally invasive approaches with reduced procedural risks become a viable option for those patients.
Although indirect decompression with the use of interspinous process spacers (IPS) has demonstrated positive outcomes, its implementation is limited in those patients with degenerative changes, spondylolisthesis, and multiple pain generators such as disc degeneration and facet joint hypertrophy. This has led to the development of minimally invasive devices for interspinous or interlaminar fixation (ISF) which can address both the stenosis and degeneration and provide the ability to stabilize adjacent spinous processes, decompress neural structures by blocking extension, and minimize overload on adjacent spinal levels. Biomechanically, they have been demonstrated to deliver immediate flexion-extension balance and provide effective stabilization for arthrodesis while preserving motion.191,192 Advantages include small skin incisions, minimally invasive nature, minimal muscle dissection, shorter operative times, and favorable efficacy.193 It is these features that make it a suitable option to those patients not suited for pedicle screw fixation, non-surgical candidates, and those early in the treatment paradigm. This has specifically been demonstrated in an elderly cohort demonstrating significant improvement in VAS with reliable fusion rates.194
The use of ISF in isolation as a treatment was performed by Postacchini et al, who demonstrated in a prospective study that a stand-alone ISF, with minimally invasive decompression in stenotic patients with degenerative spondylolisthesis, provided fusion and highly significant improvement in all outcome measures at a two-year follow-up.195 This finding was supported in a multicenter RCT directly comparing ISF with decompression to decompression alone.196 Two-year follow-up was performed on moderate to severe spinal stenosis with the primary endpoint being superior for the ISF with decompression group, as well as patients in the decompression alone group being more likely to undergo a secondary intervention or injections. ISF with decompression vs decompression with pedicle screw fusion was also assessed in a multicenter RCT with five-year follow-up.197 The majority of ISF with decompression group patients (50.3%) met all composite endpoints, while only 44% in the pedicle screw fusion group did so. The two groups were similar in reoperation rates, as well as improvement in ODI, and VAS. This finding further supports the utility of ISF.
Chin et al performed a retrospective review of prospectively collected data on patients undergoing open decompression and distraction of the spinous processes at L4-L5 using an interspinous device. Procedures were performed in an outpatient setting with a follow-up period of over 5 years.198 There were a total of 56 patients who met criteria for inclusion. The authors found significant improvements in both VAS pain scores and ODI. There was one case that underwent the removal of the device and converted to a hemilaminectomy. Lastly, there were no complications. An additional retrospective study utilizing the same device collected data on 13 patients with a median follow-up of 19 months, demonstrating a statistically significant improvement in pain scores without reoperation or complications.199 These studies demonstrate both the safety and efficacy of ISF when used as a stand-alone device. Another study specifically looked at the use of ISF without decompression as a stand-alone device.200 The study was retrospective, with a sample of 32 patients followed for three months with the Aurora Zip (Aurora Spine, Carlsbad, CA) ISF device used at four sites to evaluate the safety and efficacy of the treatment of lumbar spinal stenosis and degenerative disease. The study determined that subjects experienced a 67% reduction in VAS pain scores while having no complications.
There are several ISF devices on the market which vary in their application and patient selection. Some of the variability is due to its use with vs without a decompression, as well as with or without coinciding anterior spinal fusion. Ultimately, the use of bone graft material is a defining factor in the labeling of ISF, as well as being able to properly decorticate and prepare bone for arthrodesis.
Evidence and Therapy Grading
For interspinous/interlaminar fusion devices, there were no RCTs to guide recommendations; however, there was sufficient evidence in the form of prospective studies (Table 19) for the committee to make recommendations. Table 20 summarizes those recommendations.
 |
Table 19 Evidence Summary for Interspinous/Interlaminar Fusion Devices |
 |
Table 20 ASPN Back Consensus Group Recommendations for Interspinous/Interlaminar Fusion Devices |
Minimally Invasive Sacroiliac Fusion
Sacroiliac joint dysfunction denotes abnormal biomechanics between the sacrum and ileum, typically as a result of hypermobility. With pathological movement or laxity of the sacral ligaments, movement may result in sacroiliitis (inflammation within the sacroiliac joint) and sacroiliac joint pain. Normal movement of the sacroiliac joint is typically limited to 2 to 4 degrees of movement due to the bony architecture and ligamentous structures surrounding the joint. However, if the anatomy is disrupted or degenerative, excessive or limited nutation and counter-nutation may occur.201 Nutation refers to the anterior-inferior movement of the sacrum, while the coccyx moves posteriorly relative to the ilium; and counter-nutation refers to the posterior-superior movement of the sacrum, while the coccyx moves anterior relative to the ilium. In established cases of SIJ dysfunction, there may be either resultant elements of ankyloses or arthrosis within the joint.
Diagnostic imaging in the form of CT scans, MRIs, and plain film radiographs may provide evidence of degenerative changes within the sacroiliac joints but does not always coincide with the joint as the etiology of pain symptoms. This eventually led to the adoption of diagnostic sacroiliac joint injections. The use of image-guidance substantially improved the accuracy of the injections. To date, diagnostic SIJ injection with image guidance is the most reliable method for diagnosing sacroiliac joint dysfunction.102
Indications
Although there is a diagnostic methodology for SIJ dysfunction, the treatment algorithm has only been more recently defined and continues to evolve.103 Conservative treatments included bracing, medications, activity modification, manual therapy, chiropractic manipulation, physical therapy, and intra-articular SIJ injections.202 In the past decade, sacroiliac joint stabilization/fusion has been presented as an option for recalcitrant cases of sacroiliac joint pain. Historically, arthrodesis was performed as an open procedure and used sparingly due to its invasive nature. Surgical stabilization and/or fusion may now be performed via a minimally invasive approach. There are multiple options for sacroiliac joint stabilization/fusion, with the most common being: 1) the lateral approach, and 2) the posterior approach. In the past decade, the use of a minimally invasive transiliac or transarticular (lateral) approach became recognized with multiple high-level studies providing empirical support.203–211 The use of the posterior approach has been recently proposed as a less invasive and safer procedure. Specifically, the posterior approach avoids the neurovascular bundle.212,213
With certain posterior sacroiliac joint systems, an allograft transfixation implant(s) are placed to stabilize the joint for arthrodesis. This is not a new concept, as it was used in a previous study by McGuire et al.214 Cranial and caudal fibular dowel grafts, harvested from the posterosuperior iliac spine, were demonstrated to be effective in successful fusion of the SIJ. Newer posterior systems include a cortical allograft and therefore negate the need for harvesting of bone. Further distinguishing it is that the procedure is performed minimally invasively, which allows it to be performed on an outpatient basis and does not require weight-bearing restrictions.215
Safety and Complications
Minimally invasive SIJ fusion is a relatively safe procedure but is not without certain risks. Shamrock et al performed a recent review on the safety of transiliac sacroiliac joint fusion. They reported on fourteen studies of a total of 720 patients (499 females/221 males) with a mean follow-up of 22 months.216 There were 91 reported procedural-related complications (11.11%) with the most common adverse event being surgical wound infection/drainage (n = 17). Twenty-five adverse events were attributed to be secondary to placement of the implant (3.05%) with nerve root impingement (n = 13) being the most common. The revision rate was 2.56%. Consistent with their report, Heiney et al reported surgical wound infection as the most common complication associated with the transiliac sacroiliac joint fusion in a systematic review of 432 subjects.217
There is evolving scientific literature studying the overall number of complications for the posterior approach for minimally invasive sacroiliac joint fusion.218 Non-union was the most common complication noted but has not been consistently tracked in the studies with post-procedure imaging. Rajpal et al reported two hematomas and one infection as a result of a posterior sacroiliac screw fixation.219 There have been no reported serious complications as a result of percutaneous posterior allograft sacroiliac joint fusion/stabilization. Sayed et al published multicenter outcomes with a novel posterior approach on 50 patients and reported a 0% serious adverse event (SAE) rate.218
Evidence Review and Therapy Grading
A prospective observational study reported on 171 patients who underwent sacroiliac arthrodesis using a hollow-threaded fusion cage (DIANA cage, Signus, Alzenau, Germany).220 There were significant improvements in ODI, SF-MPQ, and both the physical and mental components of the SF-12. VAS scores decreased from 74 to 37 mm. The rate of SI joint fusion, confirmed by CT scan, was low. However, the authors attributed the low percentage of radiographic fusion to the early (6 months) stage at which patients received CT scans; inadequate preparation of the recess or deposit of bone (substitute) material; poor positioning of the implant; and osteoporosis.
In a retrospective case series, 24 patients underwent a unilateral (22) or bilateral (2) SIJ fusion utilizing the posterior oblique approach with cylindrical-threaded implants (Medtronic, Minneapolis, Minnesota).219 A statistically significant reduction in LBP scores was noted from an average VAS baseline score of 6.6 ± 2.4 to 3.7 ± 3.3 postoperatively. Leg pain scores decreased from 4.8 ± 3.8 to 1.5 ± 2.9. The mean total satisfaction score was 79% ± 27.6%.
In a recent retrospective multicenter observational study, patients with posterior minimally invasive SIJ fusion (PainTEQ, Tampa, FL, USA) were followed for at least 12 months post-implantation.28 Based on inclusion criteria, a retrospective review was performed on 50 of 110 charts. An NRS reduction of 66.5% was noted overall. In a subanalysis, the percentage of NRS reduction was calculated in cohorts of patients that had undergone previous lumbar surgery versus those who had not done so. There was a 66.8% NRS reduction in patients with histories of lumbar fusion versus a 59.6% reduction in NRS in those without such.
The use of posterior minimally invasive SIJ fusion (SIJF) (PainTEQ, Tampa, FL, USA) was lastly studied as a means of “salvage therapy”. In a multicenter retrospective observational study, 111 patients had undergone posterior SIJ fusion for refractory SIJ-related pain following previous spinal cord stimulation (SCS), interspinous spacer (ISS), intrathecal drug delivery system (IDDS) implantation, and/or PILD. The totals for each of these prior procedures included 76 SCS (68.5%), 39 ISS (35.1%), 3 IDDS (2.7%), and 2 PILD (1.8%). Nine patients (8.1%) had undergone multiple prior procedures (7 patients had SCS+ISS, 2 patients had SCS+IDDS). The mean time between SIJ allograft implantation and the last follow-up was 290.9 ± 195.7 days. At the final follow-up, the mean overall patient reported pain relief (0–100%) was 67.6% ± 28.9%. One hundred and two patients (91.9%) reported pain relief post-operatively of ≥30%. Fifty-two patients (46.8%) reported pain relief of ≥80%.221 More recently, a prospective multicenter study on this same SI fusion approach was published on 69 patients at 6 months with an average mean improvement in VAS of 34.9, ODI reduction of 17.7 and 0 device-related adverse events.222
Minimally Invasive Lateral Sacroiliac Fusion Evidence
The lateral approach to minimally invasive SIJ fusion involves dissection through the lateral gluteus muscles down to the ilium, where a device is used to transfix the ilium to the sacrum.223 The majority of evidence for minimally invasive lateral sacroiliac fusion and the highest level of evidence – two level-I prospective studies – comes from studies of a triangular titanium implant (SI Bone iFuse system; Santa Clara, CA) (Table 21, with recommendations in Table 22). There are currently 11 published level-IV retrospective studies, two level-II prospective cohort studies, and two level-I prospective studies of this technology. The RCT of minimally invasive lateral sacroiliac fusion versus nonoperative care by Polly et al determined that 82% of surgical patients and 26% of nonoperative patients achieved success which was defined by a composite score, and surgical patients received higher clinical benefit as measured by the VAS SIJ pain scores, ODI, SF-36, and EQ-5D. A total of 148 patients were randomly assigned to surgical versus nonsurgical care, and crossover from non-surgical to surgical care was allowed after 6 months.224
 |
Table 21 Evidence Summary for Minimally Invasive Sacroiliac Fusion |
 |
Table 22 ASPN Back Consensus Group Recommendations for Minimally Invasive Sacroiliac Joint Fixation |
Complication rates for minimally invasive lateral sacroiliac fusion have been relatively low, and the most concerning complication is nerve impingement, which may require removal or repositioning of the device. In an analysis of implants from a manufacturer’s database, Miller et al reported a nerve impingement rate of 0.9% and a 1.4% rate of improper device placement.225 The lateral approach may injure the L5, S1, or S2 nerves if the implant is malpositioned, and some have argued that navigation may be useful to reduce the risk of nerve injury.223 There is also some evidence that intraoperative neuromonitoring with EMG may also reduce the risk of nerve injury during minimally invasive SIJF.226
Other technologies for minimally invasive lateral sacroiliac fusion have been studied. Rappoport et al published 24-month outcomes of patients undergoing SIJF with a hydroxyapatite coated screw (Globus Medical; Audubon, PA) and reported that leg and back pain VAS scores both statistically improved at 12 months with surgery.227 Another lateral sacroiliac fusion technology – SImmetry (Surgalign Spine Technologies; Deerfield, IL) – adds SI joint decortication and bone graft delivery steps prior to implant placement. A lone level 2 prospective study has been published. In this study, Araghi et al analyzed 50 patients who underwent SImmetry fusion and reported statistically significant reductions in SI joint pain and ODI at 6 months in addition to reduced opioid use. There was one revision (2%) for nerve impingement reported in this series.228 Finally, there are several publications utilizing hollow modular anchorage screws filled with demineralized bone matrix putty and local bone. The largest prospective study involving 55 patients determined that VAS SI joint pain, SF-36 PCS, and Majeed scores improved with surgery.229
Summary of Evidence Review and Recommendations
For minimally invasive sacroiliac fusion, there was sufficient evidence in the form of 2 RCTs and several prospective observational and case studies (Table 21) for the committee to make recommendations. Table 22 summarizes those recommendations.
Sacroiliac joint dysfunction accounts for a substantial amount of reported lower back pain. Surgical stabilization and/or fusion of the SIJ may be considered when a patient has persistent moderate to severe pain, functional impairment, and failed intensive non-operative care. Overall, the evidence for minimally invasive lateral sacroiliac fusion has been Grade B, ie, moderate level of certainty for net-benefit.
Based on the efficacy and safety of minimally invasive sacroiliac fusion in properly selected patients, the authors give this therapy a grade A, ie, high level of certainty of benefit based on multiple level 1-A and 1-B studies. The authors recognize that there is a considerable need for further research for all SIJ fusion systems regardless of type or approach as well as no current evidence to support one technique over another.218 The ASPN Back Group also applies this therapy grade only to sacroiliac fusion systems and techniques with high quality peer-reviewed studies.
Vertebral Augmentation
Vertebral compression fractures (VCFs) may be classified as osteoporotic, pathologic or traumatic. In the United States, there are approximately 1 million osteoporotic VCFs reported per year along with 160,000 neoplastic fractures and 50,000 traumatic fractures.230–238 Overall, VCFs occur in 30–50% of individuals over 50 years of age239,240 and may be associated with significant debilitating pain, poor quality of life (QOL), and decreased function and are prone to progression over time leading to worsening pain, compensatory structural changes that may predispose to adjacent fractures, worsening disability and increased morbidity and mortality.241–244 Vertebral compression fractures create a heavy financial burden in the healthcare industry with costs well over $1 billion dollars yearly, and treatment optimization is essential to improve patient outcomes and healthcare utilization reduction.245 Although some VCFs may be managed conservatively, those associated with significant vertebral height loss, kyphotic deformity, debilitating pain-limiting function, progression of vertebral height loss, evolution of symptoms and advanced imaging findings of a VCF may warrant vertebral augmentation.246,247
This section will focus on specific vertebral augmentation methods, such as percutaneous vertebroplasty (PVP), percutaneous balloon-kyphoplasty (PBK) and implantable vertebral augmentation devices for the management of symptomatic VCFs when clinically indicated as described below.
The ASPN Back Group opines that vertebral augmentation is indicated when the following criteria are present:
- Urgent/emergent/hospitalized:
- Primary metastatic neoplasia with pathological fractures associated with severe pain (conservative treatment trial not indicated);
- Non-ambulatory patient secondary to VCF with severe pain preventing ambulation for more than 24–48 hours despite aggressive medical management;
- Non-urgent/non-emergent/non-hospitalized in the following situations:
- Acute (<6 weeks) painful VCF confirmed by advanced diagnostic imaging within 30 days;
- Sub-acute (<6 months) painful VCF confirmed by advanced diagnostic imaging;
- Presence of debilitating severe pain and functional deficits related to a vertebral fracture;● Severe pain on a daily basis, defined as >6/10 on a visual analog scale or numeric pain;● Significant functional impairment and inability to perform ADLs, such as non-ambulatory or limited ambulation, limited transfers, bathing, self-care, etc.;
- Lack of satisfactory improvement with at least 4 weeks of NSM as defined above.
- Absence of alternative causes for pain, such as discitis, disc herniation, spinal cord compression, etc.
Contraindications to vertebral augmentation may be classified as relative or absolute. Safety and complications are detailed below (not an all-inclusive list; other contraindications may exist).
- Absolute contraindications
- active systemic infection
- other localized infection within the procedural field
- Relative contraindications
- coagulopathy, thrombocytopenia
- allergy to bone cement/PMMA
- retropulsion of vertebral body fragments causing central canal stenosis with neurological deficit
- spinal instability
- pregnancy
- spinal cord compression/myelopathy
- neurological deficits
However, not every contraindication should preclude the procedure. The two absolute contraindications that have been agreed upon by a multidisciplinary group of experts include the presence of active infection at surgical site or an untreated blood-borne infection. It is important to note that osteomyelitis is a strong, but not absolute, contraindication. In very rare instances, vertebral augmentation may be necessary in the setting of continuous antibiotic suppression therapy in patients with few or no other options. Relative contraindications should be approached on a case-by-case basis as some of them can be avoided (ie, substituting a non-allergic filling material for a filling material in a patient with a known allergy to it) while others cannot (ie, spinal instability). Fracture retropulsion was historically considered one of the traditional contraindications but should now no longer be a contraindication, with current recommendations suggesting that vertebral augmentation increases fracture reduction and pulls the retropulsed fracture forward via ligamentotaxis of the posterior longitudinal ligament.246,248,249
Safety and Complications
Vertebral augmentation methods have an excellent safety profile and are considered safe by numerous society guidelines and landmark review studies, with a low risk of complications, post-treatment re-fractures and adjacent fractures.250–253 It is important to consider complications of both vertebral augmentation and NSM when evaluating treatment options for patients with painful VCFs. It should be kept in mind that NSM is not without complications. In the elderly population, bed rest and limitations on activity levels can be quite detrimental especially in conjunction with concurrent opioid therapy. This was demonstrated in the safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR) trial, which showed that the NSM patient cohort was associated with more SAEs compared to the vertebroplasty cohort including a case of paralysis and another case of a patient with neurologic compromise necessitating surgical decompression.251 Neither of these patients that experienced the SAEs had substantial fracture retropulsion at the time of enrolment.251
Vertebral augmentation is a minimally invasive intervention yet does present some risks. Most of these risks, however, are not clinically significant in approximately 99% of cases.254 Perhaps, vertebroplasty has a slightly higher risk compared to the newer vertebral augmentation methods, particularly related to cement extravasation into the surrounding tissue, including leakage intradiscally or into the spinal canal or adjacent vasculature. Safety can be optimized, and complications can be reduced by proper patient preparation and careful risk factor analysis. Patients with intravertebral cleft and cortical disruption are at higher risk of cement leakage and low cement viscosity and high volume of injected cement can increase the risk of cement leakage during vertebral augmentation. These factors, therefore, should be taken into consideration when planning the patient’s vertebral augmentation. Interestingly, age, sex and fracture type, and surgical approach were not significant risk factors for significant adverse events.254–256 Reported complications included such minor issues as mild superficial tissue infection and small amounts of bleeding to more serious complications such as pneumothorax, rib fracture, cord compression, nerve root injury and pulmonary embolism from cement leakage. These more serious complications, however, are rare events. Cement leakage is a common occurrence and is even more common in malignant lesions, likely because the cortex of the vertebral body is commonly destroyed and there are frequently increased levels of vascularity and neovascularity.254,257
Taking into account all of the available data regarding the safety profile, low complication rate and relative clinical insignificance of side effects, as well as clinical efficacy compared with NSM described below, we believe that vertebral augmentation outweighs the possible risks and should be considered in selected patients that meet the above-cited criteria. It is imperative to discuss the risks and benefits of VA with the patient during the informed consent process, especially as compared to the risks and benefits of NSM.
Evidence Review
As of July 2021, more than 1800 search results on PubMed were related to vertebral augmentation studies, with at least 15 level I-A RCTs published within the past decade and numerous other level I-B well-designed, controlled clinical studies. Since the two controversial and subsequently downgraded RCT studies published in 2009, the evidentiary landscape regarding the use of vertebral augmentation has evolved, with the majority of the data demonstrating positive benefits of pain relief and improvement in function when utilized alone and when compared to sham/placebo or to NSM.250,251,258–273
Based on the body of evidence, vertebral augmentation is a safe and effective treatment with multiple level I-A studies supporting its use when the proper clinical scenario described above is met.
Since VCFs are very commonly associated with severe debilitating pain, functional impairments and increased mortality risk, based on the abundance of high-quality level I-A studies, multiple meta-analyses and systematic reviews, we favor the use of vertebral augmentation in the treatment of patients with painful VCFs. For vertebral augmentation, there was sufficient evidence in the form of 15 RCTs and several prospective observational and case studies (Table 23) for the committee to make recommendations. Table 24 summarizes those recommendations.
 |
Table 23 Evidence Summary for Vertebral Augmentation |
 |
Table 24 ASPN Back Consensus Group Recommendations for Vertebral Augmentation |
Neuromodulation
Spinal Cord Stimulation (SCS)
SCS is a well-established treatment option for patients who experience chronic refractory pain, including LBP from a multitude of etiologies. As the field of neuromodulation is rapidly evolving with new technology and programming options, it is increasingly important to perform well-designed, high-quality studies to ensure optimized patient outcomes.
The studied indications for SCS in the treatment of lumbar spine pathology include failed back surgery syndrome (FBSS), nonsurgical refractory back pain, and lumbar spinal stenosis. The quality of evidence varies for each of these indications and recommendations have been provided separately based on the specific indication.
Though SCS has been considered to be a safe and minimally invasive procedure, variable complication rates have been reported. These can be divided primarily into those that can be attributed to biologic factors and those that are device (hardware)-related. Device-related complications consist of lead migration, lead breakage, lack of effective stimulation, hardware malfunction, loose connections, battery failure, and failure to communicate with the generator. Biologic complications consist of epidural hemorrhage, seroma, CSF leakage, allergic reaction, pain over implant site, and skin breakdown.274,275
Safety: Hardware Complications
The majority of device failures are related to the hardware and more specifically the leads. Lead fractures and disconnects have been reported to occur in 5.9–9.1% of cases and are typically discovered through imaging and impedance checks.275,276 Lead migration rates have been reported anywhere between 13.2 and 22.6% based on past literature reviews.274,277 Regarding lead migration, additional issues that may arise include potential loss of efficacy with need for revision and possible replacement, all of which puts additional strain on SCS therapy delivery. Though paddle electrodes have been deemed an alternative approach to address lead migration, they also present with their own set of potential complications, including neurologic injury and possible epidural hematoma.278
Safety: Non-Hardware Complications
Though non-hardware complications occur at a lower rate than hardware complications, these can include neurologic injury, epidural hematoma, skin erosion, epidural fibrosis, dural puncture, pain, and allergic reactions to the device components.274,279 The most common site for infections has been at the pocket site, with incidence ranging between 2 and 10% of implants. This was further analyzed by Hoelzer et al in over 2737 cases in which an overall infection rate of 2.45% was identified.279,280 In their analysis, it was determined that post-operative dressings and antibiotic coverage were important in decreasing infection rates. Another low-frequency complication is epidural hematoma with an incidence of 0.25–0.3%.274,281 Another potential complication is neurologic injury (incidence of 0.03–0.25%) that can involve the motor, sensory or autonomic nervous systems and may result from direct trauma from the needle or lead, in both percutaneous and paddle variations.
The impact of neuromonitoring in reducing central nervous system (CNS) injury with various levels of periprocedural sedation is important to consider and review.282,283 Although SCS is a viable, generally safe, non-pharmacologic approach to pain management, we must keep in mind that there are potential hardware and non-hardware complications that can occur.
Evidence Review
The evidence for SCS in the treatment of FBSS is supported by six randomized, controlled trials with significant enrollment volumes over time periods greater than six months. The evidence for SCS in the treatment of nonsurgical LBP consists of two prospective case series and small cohorts of patients within larger studies. Compared to FBSS and nonsurgical LBP, there is a dearth of evidence describing the use of SCS for lumbar spinal stenosis (LSS)-related back and leg pain. For SCS, there was sufficient evidence in the form of six RCTs and several prospective observational and case studies (Table 25) for the committee to make recommendations. Table 26 summarizes those recommendations.
 |
Table 25 Evidence Summary for Spinal Cord Stimulation |
 |
Table 26 ASPN Back Consensus Group Recommendations for Spinal Cord Stimulation |
Intrathecal Drug Delivery
Given the many thousands who died of prescription opioid overdoses during the first decade of this millennium, traditional opioid analgesia has become a less comfortable mode of treatment for chronic LBP in recent years. However, IDDS is established as a safe, effective, and economical treatment option for the management of a wide range of refractory chronic pain.284–290 Yet, its clinical utility specific to back pain remains limited by the lack of high-quality RCTs.291,292 This subsection will review current literature on the role of IDDS for LBP and present clinical guidance.
Indications
Prior to discussing disease-specific indications, it is important to establish and understand the definition of refractory pain. Deer et al proposed that pain is defined as refractory, regardless of etiology, when 1) multiple evidence-based biomedical therapies used appropriately have failed to reach treatment goals or have resulted in intolerable adverse effects, and 2) psychiatric disorders and psychosocial factors that could influence pain outcomes have been optimized.293 The FDA has indicated IDDS for a variety of noncancer pain conditions in cases in which more conservative therapies have failed.294–296 The majority of patients with IDDS implanted for noncancer pain have back pain with or without leg pain, with the most common diagnosis being FBSS or post-laminectomy syndrome (PLS).297,298
Patient selection is crucial. A complete evaluation including physical examination, medication review, comorbidity assessment, and psychosocial evaluation is recommended.295,299 Patients considered for this therapy must also have a clear diagnosis and source for their chronic back pain. They must be refractory to conservative medical management or other less invasive procedures; however, it should not be considered as a salvage therapy but rather as a distinctly different therapy.295,300 The 2017 Polyanalgesic Consensus Conference (PACC) guidelines, in fact, suggest IDDS within the same line as SCS and before the escalation of long-term systemic opioid therapy (Table 27).295 Currently, it is recommended to consider IDDS for diffuse pain pattern that may not be adequately covered by SCS.295 Key considerations for patient selection are outlined in Table 28.
 |
Table 27 Disease Indications for Intrathecal Drug Delivery |
 |
Table 28 Key Considerations for Patient Selection |
The medication choice for intrathecal administration has been well established in the literature. It is based on the level of evidence and consensus with stratification based on diagnosis and pain characteristics.295,297 Morphine and ziconotide are the only two FDA-approved intrathecal medications. Ziconotide is the first-line choice for localized noncancer neuropathic or nociceptive pain in the absence of history of psychosis or renal disorder.301 Morphine is preferred in patients with diffuse pain on more than 120 morphine equivalents in daily use.295,301 Second-line agents for localized and diffuse pain are fentanyl and hydromorphone, respectively, with or without bupivacaine.295 Other agents for tertiary and quaternary uses include admixtures of first- and second-line drugs with clonidine, sufentanil, or baclofen. The 2017 PACC guidelines summarize an algorithmic approach with recommended starting doses and titration.295
Safety and Complications
Some authors have challenged the safety of IDDS.302–305 Coffey et al demonstrated higher mortality associated with IDDS compared with SCS or lumbar laminectomy and raised concerns regarding opioid overdose and critical device-related issues.303 However, there exists an abundance of literature supporting IDDS as a safe and effective treatment option for different types of chronic, noncancer back pain.284–290,306−321 The 2017 PACC guidelines also suggested that the risk-benefit profile of IDDS makes it a relatively safe therapy, especially when compared to chronic systemic opioid therapy.297 It is imperative for clinicians to not only implement risk-mitigating strategies but also understand the intrathecal physiology and anatomy, pharmacokinetic and pharmacodynamic properties of medications, and all potential complications.
IDDS complications can be technical including catheter or pump malfunction, pharmacological, or procedural (Table 29).25,60–62,297,322–324 The most common complications were drug-related (reportedly up to 77% of all complications), followed by hardware malfunctions and procedural-related issues.297,305,325 While the majority of complications are transient and minor, serious complications can occur. An increased mortality associated with intrathecal opioid therapy in noncancer patients (0.088% at 3 days after implantation, 0.39% at 1 month, and 3.89% at 1 year) has been reported.303 Other rare but serious complications include sudden drug withdrawal or overdose, epidural or spinal hematoma, meningitis, and catheter tip granulomas likely related to higher doses and concentrations of opiates except for fentanyl.297,322,326 The administration of the lowest effective drug dose and concentration is recommended to prevent granulomas.297
 |
Table 29 Complications Associated with IDDS |
Drug-related complications are most studied with intrathecal opioids, most commonly morphine. Intrathecal opioids have been associated with adverse effects including respiratory depression, nausea, vomiting, diaphoresis, pruritus, sedation or change in mental status, urinary retention, and sexual dysfunction.297,299,305 Intrathecal ziconotide has been associated with cognitive and neuropsychiatric adverse events, especially when titrated rapidly.297,327,328 It should also be avoided in patients with renal disorders due to the risk of renal toxicity and rhabdomyolysis.299,329,330 Bupivacaine may result in sensorimotor loss or cardiotoxicity in higher doses.297 Clonidine has also been associated with cardiovascular side effects, from peripheral edema to potential life-threatening hypertensive crises and stress-induced cardiomyopathy.299
Although it is largely a safe therapy especially with recent advancement in technology and understanding of intrathecal drugs, IDDS may carry a higher risk than other interventional pain procedures. Therefore, IDDS should be implanted and managed by experienced multidisciplinary teams, with expertise in patient selection, medication selection, surgical techniques, and long-term management with understanding of all potential complications.
Evidence Review with Evidence Level Designation
It is generally accepted that intrathecal delivery of medications has clinical value; therefore, the questions that confront the therapy today concern the evidence surrounding applications of medications and medication combinations as well as guidance from pan societies concerning clinical application of the therapy. For example, IDDS has been criticized regarding the lack of high-quality RCTs with long-term follow-ups for many medications, although RCTs do exist to support the use of ziconotide. Some authors such as Hayes et al stressed the lack of consistency in the clinical use of IDDS in chronic noncancer pain.331 Brown et al also highlighted the complexity of intrathecal opioid therapy.332 Their study suggested that despite some therapeutic benefit of IDDS, patients continue to suffer from substantial physical impairment.332 As a result of these suggestions, the PACC was created to fill the void regarding clinical questions that persist with consensus opinion and evidence accumulation.294,295,297 However, there exist several retrospective trials and three prospective observational trials supporting the therapy (Table 30).
 |
Table 30 Evidence Summary for Intrathecal Drug Delivery Systems |
Numerous systematic reviews of IDDS have been performed by several groups.292,314,316,324,333–335 Although review methodologies vary, all of the reviews report a gap in our current literature supporting IDDS for noncancer pain, including chronic LBP (Tables 28–30). Based on our literature search and evidence review, the evidence of IDDS for chronic noncancer back pain is moderate. Based on the USPSTF criteria1 modified for interventional spine procedures, the therapy grading for IDDS is limited to grade B for noncancer back pain. Evidence is presented in Table 30, and recommendations may be found in Table 31.
 |
Table 31 ASPN Back Consensus Group Recommendations for Intrathecal Drug Delivery Systems |
Peripheral Nerve Stimulation for Low Back Pain–Multifidus Activation via Medial Branch Nerve Stimulation
The majority of CLBP patients suffer from mechanical (musculoskeletal) pain that is predominantly nociceptive in nature; however, neuropathic or mixed patterns are also commonly seen. Patients with CLBP often endure impaired quality of life, depression, anxiety, and sleep disturbance. Patients suffering from CLBP learn to balance activity with pain on an individual level. Some will tolerate a certain amount of pain to increase their activity level. Others are less tolerant to pain and will minimize any perceived activity that may aggravate their pain, initially leading to inactivity, guarding, and kinesiophobia. Persistent back pain-induced inhibition and disruption of proprioceptive signaling has also been correlated with long-term motor cortex reorganization. Ultimately, this results in impaired neuromuscular control and functional instability from degeneration and atrophy of the lumbar multifidus muscle, the most important stabilizer muscle of the lumbar spine.
Recently, interest has been drawn to incorporating peripheral nerve stimulation (PNS) for CLBP. These treatments have been demonstrated not only to improve pain and function but also to decrease the need for multiple interventions to treat CLBP, many of which are unsuccessful.336,337 Targeting the medial branch nerve of the dorsal rami of the lumbar spine, which innervates the fascicles of the multifidus muscles, results in activation. These muscles originate at the posterior sacrum, superior iliac spine, and mammillary processes of the lumbar vertebrae. They insert on the spinous processes of the vertebrae in the lumbar spine, 2–4 bones above the origin. This muscle group plays a critical role in providing segmental stability in response to changes in posture and protection against sudden movements.
Indications
After a comprehensive history and focused neurologic and musculoskeletal physical examination, assessment of CLBP should include an individualized, phasic, comprehensive, and multi-modal treatment plan, avoiding surgery if not indicated. Initial options may include the use of adjuvant non-opioid medications to facilitate a rehabilitative paradigm focused on addressing impaired neuromuscular control from degeneration of the multifidus muscle to restore lumbar spine stability, decrease pain, and improve function. More advanced treatments such as PNS should be considered once more conservative options have failed and there is no indication for invasive surgery. Candidates for PNS therapy experience CLBP secondary to multifidus muscle dysfunction, which is often consistent with muscle atrophy. Atrophy can be confirmed via MRI and dysfunction via physical exam. The prone instability test and multifidus lift test are physical exam maneuvers used to assess weakness of the multifidi from atrophy. Currently, the literature and experience revolve around both short-term and permanently implanted techniques.
Safety and Complications
Thus far, safety and efficacy of the non-implanted 60-day system has been demonstrated in small, uncontrolled, prospective studies. In a 2019 investigation, most subjects in a small cohort of 11 patients experienced clinically significant reductions in average pain intensity, disability, as well as pain interference without any serious or unanticipated device-related adverse events. These findings are consistent with spinal cord stimulation therapies, which potentially include infection, as well as lead migration and fracture. In a 2021 study of PNS of the medial branch nerves in a cohort of patients with lack of long term relief from lumbar radiofrequency ablation, no serious adverse events where noted. The most common side effects were mild skin irritation and/or itching, and one case of superficial infection in the 15 subjects followed. A subsequent analysis of the literature revealed that percutaneous PNS leads with a coiled design had a statistically significant lower infection risk than non-coiled leads.338 Further studies of the safety and efficacy of non-implanted 60-day system are underway.
To date, safety and efficacy of the permanently implanted PNS system has been demonstrated in multiple publications. In the most recent trial, the primary safety outcome was to assess any serious device- or procedure-related adverse event at the 120-day visit following implant. All adverse events were otherwise documented and reported. This included observed rates through the one-year visit after implant; however, there were no actual statistical hypotheses tested in the safety assessment. Among the 204 randomized subjects, 8 SAEs were reported. Three occurred in the treatment group and 5 occurred in the control group for an overall related serious adverse event rate of 4% at the 120-day primary endpoint visit. There were no unanticipated SAEs related to the device or the procedure. Of the eight serious device- or procedure-related adverse events reported, all were procedure-related with the exception of one. The rates of adverse events are consistent with known SAE rates for spinal cord stimulation therapy; however, there was no finding of lead migration, an issue that affected previous design of electrodes used. This trial demonstrated clinical effectiveness as measured by substantial and durable improvements in pain, disability, and quality of life in a cohort of patients with a favorable benefit risk profile.339,340
Evidence Review with Evidence Level Designation
Thus far, evidence supporting the efficacy of the non-implanted 60-day system is developing, with an evidence level of II. The non-implanted 60-day system was studied in a 2019 case series, at which time the stimulator was granted Investigational Device Exemption status, by using a 30-day, percutaneous, non-surgical, open coil PNS array targeting the medial branch of the dorsal ramus.341,342 Data demonstrated a reduction of pain intensity as well as in use of analgesic medications.
The highest level trial of the permanently implanted PNS system was an international, multi-center, prospective, randomized, active, sham controlled, blinded trial, which generated high, level I-A evidence supporting the significance of the treatment effect.339,340 The study was conducted at 24 sites in the US, Australia, and Europe. A total enrollment of 204 subjects were implanted with the permanently implanted PNS system and randomized (1:1) to the treatment or control group. Subjects in the treatment arm had the permanently implanted PNS system programmed to deliver stimulation at a level appropriate to the individual subject. Subjects in the control group had the permanently implanted PNS system programmed to deliver low-level stimulation. The primary endpoint assessment occurred at the 120-day visit. After the 120-day visit, subjects in the control group were given the choice of having their IPG programmed to deliver individualized and appropriate stimulation (crossover group). A complete review of the available evidence for this medial branch stimulation is summarized in Table 32.
 |
Table 32 Evidence Summary for Multifidus Activation via Medial Branch Nerve Stimulation |
Therapy Grading
For PNS stimulation of medial branches, there was sufficient evidence in the form of six RCTs and several prospective observational and case studies (Table 32) for the committee to make recommendations. The ASPN Back Group recommends selectively offering the non-implanted 60-day system therapy to individual patients based on professional judgement and patient preferences. There is at least moderate certainty that the net benefit is small. The ASPN Back Group recommends offering the permanently implanted PNS system given that there is high certainty that the net benefit is substantial. Recommendations are summarized in Table 33.
 |
Table 33 ASPN Back Consensus Group Recommendations for Multifidus Activation via Medial Branch Nerve Stimulation |
Peripheral Nerve Field Stimulation
Since its initial documented use in 1965 by Drs. Wall and Sweet, peripheral nerve stimulation (PNS) has evolved dramatically. One of its derivatives known as peripheral nerve field stimulation (PNFS) is postulated to provide analgesic effects through a similar mechanism as PNS: stimulation of the Aβ afferent neurons leads to excitation of inhibitory dorsal horn interneurons, which block the potentiation of nociceptive signals from Aδ and C-fibers to wide dynamic range neurons and thus decreases the noxious signal sent to higher cortical regions.343,344 Rather than providing electrical stimulation to a specific sensory nerve, which is the goal of PNS, PNFS targets more distal and smaller sensory branches as well as subcutaneous nerve endings.345
Various studies have demonstrated that in patients with axial LBP, lead depth placement of 10–12 mm maximizes activation of Aβ fibers while not being too superficial to raise concern for superficial erosion of leads or unintentional motor activation if placed too deep.346 When considering PNFS, placement of the leads during the trial is critical as well. If the focal area of axial LBP is approximately 6 cm in diameter, then one lead is typically used with the intention of targeting the lead placement to the epicenter of this region to maximize the therapeutic effect. If the region of intense pain experienced by patients is larger, then placement of two leads at the periphery of the painful region is recommended. During this process, patients are asked to give feedback regarding the paresthesias experienced during active stimulation of the leads, and placement is adjusted to optimize pleasant paresthesias.347 These trials are performed to optimize location and programing of the leads prior to permanent subcutaneous implantation of PNFS leads with an IPG.
Indications and Complications
The general indication for the use of PNFS is in patients with severe chronic neuropathic pain, without a clearly correctable underlying pathology, that persists despite various medical treatments.348 With respect to its use in patients with LBP, PNFS can be used for treating either chronic unilateral or bilateral axial pain that may or may not be associated with failed back surgery syndrome following a multilevel spinal surgery.349 In addition, some other important criteria when selecting patients include ensuring their pain is well localized to a specific region in the low back, the pain remains uncontrolled for more than 6 months despite guideline-based management, and the intensity of the axial LBP is more severe than radicular pain in situations in which both are occurring concurrently. Much like PNFS performed in other areas of the body, imaging prior to PNFS trialing should be performed to exclude any underlying reversible spinal pathology causing the patient’s symptoms.347
The complications reported in PNFS are similar to those evidenced in PNS and include infection, lead migration, skin erosion, fracture/disconnection of the leads, and hardware malfunction. The propensity for certain complications to be more prevalent in PNFS than PNS may exist, particularly given the depth and technique utilized when anchoring the PNFS leads, but the lack of literature specifically evaluating complications of PNFS makes this distinction difficult to make.348,349 Some of the various complications and complication rates seen in PNFS studies will be discussed in the following section.
Review of Evidence
When evaluating the evidence supporting the use of PNFS for the treatment of chronic LBP, there remains a paucity of literature that evaluates solely PNFS’s role in treating LBP. Rather, some of the studies look at PNFS’s use for the treatment of various regions of pain, and they incorporate statistically significant data from patients suffering from solely chronic LBP. Here, we will incorporate these statistically significant findings in addition to studies that isolate PNFS’s role in treating solely axial chronic LBP. The literature is summarized in Table 34 and the therapy grade recommendations for PNFS for low back pain are highlighted in Table 35.
 |
Table 34 Evidence Summary for Peripheral Nerve Field Stimulation |
 |
Table 35 ASPN Back Consensus Group Recommendations for Peripheral Nerve Field Stimulation |
Ablative Therapies
Lumbar Radiofrequency Ablation Lumbar Spine
One of the most prevalent articulations of the lumbar spine is that of the zygapophyseal joint.350 This joint is formed at each level of the lumbar spine and at the lumbosacral junction by the inferior articulating process of the level above in the superior articulating process of the level below. As in other parts of the human body, this joint is subject to degeneration of both primary and secondary causes leading to joint hypertrophy, joint stiffness, synovitis and hypomobility. Lumbar facet-mediated pain may likely result from repetitive stress and trauma to the joint and/or joint capsules causing chronic inflammation and capsular distention. Nonetheless, these pathological processes often lead to progressive and significant debilitating pain.351
The use of thermal destruction of neural tissue is simply based on the premise that pain that may be otherwise refractory to oral pharmacology or physical therapy is treated by destroying the sensation delivery pathway from the site of pain. Simply speaking, the destruction of the neural signal pathway is performed as the correction of the underlying cause from a surgical standpoint cannot be performed or does not exist.352
Conventional radiofrequency ablation (C-RFA), also known as radiofrequency thermocoagulation (RFTC) and radiofrequency neurolysis (as well as simply, “neurolysis”), is a treatment method utilizing radiofrequency current to create a thermal change in a defined, non-insulated area of an otherwise insulated conductive probe or needle. The conductance of energy to the tip of a radiofrequency needle creates a well-defined area of heat used for thermal ablation of a biological tissue. Commonly in medicine, thermal destruction is used when neural signaling is either aberrant or undesirable. Radiofrequency ablation exists as traditional, constant heat and for a defined time, thermal destruction. The level of heat typically is in the range of 60–90 degree Celsius. Pulsed RFA (P-RFA) parameters are similar to conventional RFA, albeit that output of the energy is delivered in short pulses. Shorter pulses reduce tissue target temperature with interval cooling permitted, therefore allowing for the use of radiofrequency interruption of neural signaling without diffuse tissue damage. A classic use of pulsed RFA is 20 millisecond pulses every 0.5 seconds with temperature not exceeding 42 degree Celsius.353,354 Other forms of radiofrequency ablation include a “cooled” form of ablation with temperatures at or near 60 degree Celsius for a prolonged time period resulting in a larger circumference of a lesion.355
Indications
Indications for the use of lumbar RFA are largely related to intractable pain of the lumbar facet joints. Pain of nociceptive origin from the lumbar facet joints are treated using this therapy following pain for at least three months and the patient having tried and failed more conservative measures or these measures being contraindicated in that patient’s specific medical state. Conservative measures include, but are not limited to, physical therapy, manual manipulation, psychological coping strategies, medically supervised exercise regimens and pharmacological management, typically most consistent with failure of non-steroidal anti-inflammatory medication, acetaminophen, and other therapies such as opioids. The latter pharmacological management strategy has generally fallen out of favor as a treatment option given the larger societal problem of opioid abuse. Lastly, RFA is typically preceded by diagnostic medial branch nerve blocks with local anesthetic solutions such as lidocaine, bupivacaine and ropivacaine followed by reassessment of pain reduction and functional improvement, if present.35
Safety and Complications
The overall safety profile related to the use of RFA is favorable. Some small retrospective studies exist and report complications; typically, these complications are self-limited and include common postprocedural issues such as pain after injection, transient worsening of back pain, thermal injuries and infection. While complications may occur, the rate of complication is quite low,356 although care must be taken to prevent heating of lumbar instrumentation, if present.357 Similarly, the use of direct visualization through fluoroscopy and confirmation with sensory and motor testing also contributes to the low complication rate.
Review of the Evidence
There are several studies pertaining to the use of traditional RFA, pulsed RFA and cooled RFA in publication. The most substantial body of published data appears to be related to either traditional RFA in isolation or comparisons between traditional RFA and pulsed RFA.
Efficacy of Conventional, Continuous Radiofrequency Ablation
A C-RFA literature search revealed 3 randomized trials (one multicentered randomized, double blinded, sham lesion-controlled trial, two single-centered, randomized double-blind controlled trials), in addition to 1 single-centered sham-controlled trial, two large prospective observational outcome studies, 1 single-centered, prospective clinical audit, and 1 large single-center retrospective review. Table 36 presents an evidence summary, and recommendations appear in Table 37.
 |
Table 36 Evidence Summary for Lumbar Radiofrequency Ablation |
 |
Table 37 ASPN Back Consensus Group Recommendations for Lumbar Radiofrequency Ablation |
Sacroiliac Radiofrequency Ablation
Sacroiliac regional pain syndrome (SIRP) is a pain condition that is characterized by a localized pain below the posterior superior iliac spine and the buttock region. The pain arises from the densely innervated joint, joint capsule and the ligamentous structures in the posterior and the anterior aspects of the joint.358 The prevalence of the SIRP pain depends on age of the patient, typically increasing with age, as the mechanics shift the weight from the anterior elements to the posterior elements. There is also a higher incidence in patients who have undergone adjacent segment fusion at the lumbosacral level. The importance of understanding the SIRP condition is that it accounts for many instances of lower back and buttock pain currently treated by the primary care providers and specialists.
Because of the transient and inconsistent results of sacroiliac injections (with local anesthetics, steroids) and prolotherapy, more definitive treatments have been sought. Since the advent of radiofrequency neurotomy, multiple authors have deployed a variety of different approaches to denervate the joint. There has been variability historically in outcomes attributable to patient selection, target selection, and procedural technique.
Pathophysiology and Innervation of the Sacroiliac Region
The SIJ is a 1–2 mm wide diarthrodial joint with an articular cartilage, synovial fluid, and a fibrous capsule. The joint has a strong ligamentous support structure that serves to stabilize the joint. The joint still has motion in two planes. The innervation of the intra-articular portion of the joint has been vigorously contested over the years. It appears that anteriorly, there is innervation from the lumbosacral trunks, obturator nerve, and gluteal nerves, and posteriorly from the lateral branches of the S1-S3 dorsal rami. Historically, there was a belief that there is also innervation from the L4 medial branch and the L5 dorsal ramus. Sacroiliac joint complex pain emanates from the extra-articular elements in addition to or separate from the intra-articular portion of the joint. This complex includes the articular portion of the joint, the joint capsule, overlaying dorsal ligaments, regional muscles, and nerves that supply these structures.
Diagnosis Pitfalls and Precautions
Pain and tenderness above the posterior superior iliac spine is less likely to be due to SIRP, whilst that at or below the sacral sulcus is more likely to be symptomatic of SIRP. The finger Fortin sign, whereby the patient points to the medial aspect of the sacral joint in the sulcus, has the greatest likelihood to be indicative of SIRP. Laslett et al and van der Wurff et al have thus posited that if 3/5 clinical signs are positive, there is high sensitivity and specificity of an SIRP diagnosis.110,359
Optimal diagnostic criteria for the sacroiliac joint, or more accurately the sacroiliac regional pain, have not been defined, in part due to the lack of agreement of the true pathophysiology of SIRP. Pain emanates from the joint as well as the surrounding soft tissues. Thus, a provocative injection of the joint or a pain-relieving local anesthetic injection that blocks the joint pain alone but missing the blockade of the soft tissues does not suffice. Likewise, a single clinical symptom (“I have buttock pain in the region of the sacroiliac joint”) is not sufficient due to considerable overlap from other pain generators (such as annular tears, herniations, facet arthropathy, neurocompressive stenosis, spondylolisthesis) that can masquerade as “sacroiliac pain”. The importance of ruling out these other conditions is that there are definitive solutions for many of these conditions. Accurate prognostic and diagnostic information are also a prerequisite for optimal outcomes.
Imaging including sacroiliac degeneration again may suggest is the presence of pathophysiology, but this does not necessarily confirm that the joint is a painful one.
Prognostic Blockade for Radiofrequency Neurotomy
The construct of dual comparative anesthetic blocks with two separate local anesthetics as a prelude to radiofrequency neurotomy has been established for cervical and lumbar facet denervation,52,360–362 although the extension of this paradigm to sacroiliac denervation has important limitations. First, sacroiliac innervation is inconsistent, second, the sacroiliac lateral branches are not always in the same tissue planes, and third, our understanding of the sources of innervation of the sacroiliac complex has been evolving. With respect to innervation, it was believed that the joint received innervation from the L4 medial branch, L5 dorsal ramus and the lateral S1, S2, and S3 lateral branches, leading Cohen et al in 2008363 to include these nerves in their randomized prospective controlled trial. Subsequently, the L4 medial branch was believed not to contribute to the sacroiliac complex, leading Patel et al in 2012 to exclude the L4 medial branch from their RCT.364,365 In both studies, the prognostic block technique differed. In the Cohen trial,363 the patients were randomized to sham procedure or radiofrequency neurotomy if they reported >75% relief with one intra-articular corticosteroid and anesthetic injection 6 hours post-injection. In the Patel et al RCT, patients were eligible for study enrollment if they received >75% relief of their index pain with two sets of single-site, single-depth, anesthetic blocks of the L5 dorsal ramus and S1-S3 sacral lateral branches.364,365
Indications and Contraindications
Axial non-radicular pain is the most common clinical presentation in the contemporary pain clinic. Amongst this group of patients, mixed and nociceptive pain syndromes predominate with pain arising from the anterior and posterior elements, including facet joints, annular tears in the discs, and sacroiliac joints.119,127,366,367 Lower back and buttock pain without distal radicular and neuropathic features must be carefully evaluated to precisely define the primary source of pain. The presence of pain should be corroborated with at least three positive clinical signs, subsequent to which prognostic dual comparative multi-site multi-depth anesthetic blocks with >75% relief with each block of the lateral S1, S2, S3 branches are the best indication for the sacral radiofrequency denervation procedure.
The procedure is contraindicated in anyone with localized infection, refusal and/or inability to provide informed consent, and pregnancy when fluoroscopy is indicated. Relative contraindications are poorly visualized anatomy and cases in which limited visualization of the sacral foraminal precludes adequate placement of the radiofrequency cannulas.
Safety/Complications
Because the procedure involves defined bony landmarks and end points, SIRP is safe, with few if any real complications. In fact, none has been cited in the published literature. Nonetheless, transient post-procedure pain (neuritis) is a possible side effect, as is possible infection, although both are easily addressed with analgesics (gabapentin) and antibiotics, respectively.
Evidence Summary for Sacroiliac Radiofrequency Neurotomy
Many prospective studies for the treatment of SIRP exist. Three sham-controlled studies demonstrated efficacy,363–365,368 and four further pragmatic effectiveness trials, and eight observational studies have been published (Table 38). In these investigations, there was extensive variation in terms of selection criteria, targeted nerve branches, procedure techniques and technologies deployed. Table 39 contains the recommendations for SI joint lateral branch ablation.
 |
Table 38 Evidence Summary for Sacroiliac Radiofrequency Ablation |
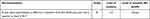 |
Table 39 ASPN Back Consensus Group Recommendations Sacroiliac Radiofrequency Ablation |
Basivertebral Radiofrequency Ablation
The basivertebral nerve (BVN) is a branch of the sinuvertebral nerve responsible for carrying nociceptive information from damaged vertebral endplates. The sinuvertebral nerve arises bilaterally from the ventral ramus of each spinal nerve immediately distal to the dorsal root ganglia and travels to join a branch of the grey ramus communicants responsible for sympathetic fibers. The nerve then takes a recurrent course and re-enters the spinal canal through the basivertebral foramen towards the midline of the vertebral body, where these fibers become the BVN. Although there is some anatomical variability, the BVN travels in a posterior to anterior direction approximately 30–50% into the vertebral body, forming a central nerve trunk, where it bifurcates towards the superior and inferior endplate. This is the anatomical target for the ablative procedure of the BVN for vertebral pain discussed in this section.369–371
Historically, other structures such as intervertebral discs, facet joints, ligaments and muscles have been studied as the source of axial LBP. Recently, a shift towards damaged vertebral endplates has been proposed as a potential contributory etiology of LBP.372,373 Numerous studies have postulated that axial LBP may have a vertebral etiology component, and there is growing evidence that damaged vertebral end plates with nociceptive pain carried by the BVN can be perceived as LBP through substance P and calcitonin gene-related peptide (CGRP), which has been confirmed with protein gene product (PGP) 9.5 positive histochemical marker visualized under microscopy.371–377
Vertebral endplates are highly vascularized and innervated structures susceptible to post-traumatic degenerative changes, inflammation, and intraosseous edema, which tend to manifest in MRIs as Modic changes (MC) which may present clinically inconsistently from other potential etiologies.373,376–382 Identifying the etiology of LBP is a common challenge in clinical practice. Eighty percent of cases are diagnosed as non-specific LBP, and only 20% of LBP cases can be attributed to a pathoanatomical entity. Jensen et al reviewed 82 studies and determined that MCs were reported in up to 43% of patients with nonspecific LBP; a positive association between MCs and nonspecific LBP was found in 7 of 10 studies. Therefore, the identification and diagnosis of this subset of patients with pathoanatomical changes is crucial to optimize patient outcomes.382–385
LBP associated with MCs presents clinically differently than other etiologies. The clinical presentation may vary widely in the population, but it is generally described as a deep, aching, midline (up to 70% of cases), burning pain of progressive nature that is potentially more severe at night. There is generally no radicular expression (in only approximately 6% of cases reported), no lower extremity weakness or sensory deficits, and symptoms tend to be worse with spinal flexion, sitting, and standing, in contrast to extension. Type I MCs are positively associated with higher LBP intensity and worse ODI scores. These patients tend to present with significant functional impairments, and those with MCs reported a greater frequency and duration of symptoms, seeking care more often than those without MCs.372,380,381,384,386 Among the three types of MCs, Type I is known to be the one strongly associated with LBP, in contrast to Type II or Type III, which have been shown to be more stable and demonstrate less refractory pain. Type I MCs are described as vertebral endplate disruptions, degeneration and fissuring with areas of granulation under histological analysis, and present as bone marrow edema, increased vascularity and inflammation within the vertebral endplates, perceived as decreased signal in T1-weighted MRI and increased signal in T2-weighted MRI.382,387,388
Treatment options for LBP associated with MCs are similar to those recommended for LBP of other etiologies, starting with a conservative approach to minimally invasive surgical options; however, conservative care is generally not effective.389 With advancements in the pathoanatomical understanding of vertebral endplate damage, the association of MCs with LBP severity, and the BVN role in providing sensory innervation to vertebral endplates described above, it is feasible to presume that RFA or neurotomy of this nerve may interrupt nociceptive signaling and potentially reduce LBP of vertebral etiology by directly targeting the potential pain generator.390
Indications and Contraindications
Intraosseous BVN ablation or neurotomy is a minimally invasive procedure performed under fluoroscopic or CT-guidance. The procedure involves unilateral transpedicular or transforaminal endoscopic extrapedicular access, with the use of bipolar electrodes to deliver high frequency alternating current, resulting in BVN neurotomy and the interruption of pain transmission from damaged vertebral endplates.85,390–393
Medical necessity to support this intervention should include a detailed history and physical exam, in addition to diagnostic studies and treatment history to support the rationale for the procedure.
BVN ablation at the L3 through S1 vertebrae is indicated when patients meet the following indication criteria:
- Chronic axial LBP (greater than 6 months of duration).
- Pain refractory to conservative nonsurgical treatment for at least 6 months of duration.
- Evidence of vertebral endplate changes on MRI as below:
- Modic Type I and/or Modic type II changes.
- Vertebral endplate changes with inflammation, edema, disruption and/or fissuring.
- Fibrovascular bone marrow changes (hypointensive signal for Modic type I changes).
- Fatty bone marrow replacement (hyperintensive signal for Modic type II changes).
BVN ablation is clinically indicated using an FDA-cleared device for the procedure when the above criteria are met.
Studies published to date on the use of BVN ablation for vertebral pain also fulfilled other inclusion criteria, which were variable based on each study. These included confirmed skeletal maturity on diagnostic images, significant limitations in function and ADLs with a minimum of at least 30 points on the ODI and of 4 cm on the VAS, and all other reasonable sources of pain have been ruled out. Regardless, the patient population of all published studies on BVN ablation has met the 3 main inclusion criteria noted above. General contra-indications to the procedure include active systemic infections, pregnancy, histories of spine surgery at the treatment level, type III MCs, tumors, metastatic disease, osteoporosis, and implantable pulse generators. Other contra-indications or exclusion criteria reported by some of these studies included compression fracture at the treatment level, symptomatic spinal stenosis, radicular pain, body mass index greater than 40, addictive behavior, three or more Waddell’s signs, Beck Depression Inventory (BDI) score greater than 24, thrombocytopenia, and coagulopathy.394,395
Safety and Complications
The device- and procedure-related AEs reported in the 473 clinical trial procedures (including 78 sham procedures) performed to date are quite low and had a median time to resolution of 66.5 days. The most commonly reported minor, self-limiting post-procedure adverse events included incisional pain and transient worsening of back pain. The following device- or procedure-related events have been reported:
- 1 case of a nerve root injury.
- 2 cases of lumbar/lumbosacral radiculopathy.
- 4 cases of motor/sensory deficits.
- 17 cases of transient radiculitis successfully treated with oral medications.
Serious AEs reported in the post-market surveillance for commercial cases FDA database through February 2021 include 1 case of vertebral compression fracture in a sham procedure in a patient undergoing hormonal therapy and 1 case of a retroperitoneal hemorrhage. Post-procedure MRIs at variable follow-up intervals did not reveal any signs of avascular necrosis, spinal cord injury or accelerated disc degeneration. In addition, there were no reports of thermal injuries, post-procedure infections, or broken devices. Although AEs are considered relatively rare in the studies published to date, future larger scale studies are needed, nonetheless, based on the studies available, BVN ablation seems to be safe and well tolerated by most patients when proper patient selection and procedural technique are applied.85,390,391,393,394,396
Evidence Review with Evidence Level Designation
There have been numerous clinical studies published to date with direct patient-data regarding the clinical efficacy of BVN ablation for axial LBP of vertebrogenic nature.370,391,392,395,397–403 In addition, clinical and systematic reviews recently have been published discussing different aspects of this intervention in chronic axial lower back pain management, analyzing common data points among similar studies, as well as published society guidelines.85,390,393,394,396,404–407 Table 40 provides a summary of available clinical studies, outcome measures utilized, level of evidence (according to USPSTF criteria1) and comments on each study. Studies published to date reported functional outcomes with the ODI and pain assessment utilizing the VAS, while quality of life measurements were reported utilizing the SF-36 and/or the EQ-5D-5L questionnaire. Patient satisfaction has been analyzed utilizing the MacNab criteria, and opioid utilization was also reported as an outcome measurement in several studies.
 |
Table 40 Evidence Summary for Basivertebral Radiofrequency Ablation |
Evidence and Therapy Grading
For basiventral nerve ablation, the evidence is summarized in Table 40. Based upon 11 studies meeting search criteria for inclusion in the review, the recommendation for basivertebral nerve ablation is Grade A with Level of Certainty 1a based upon 4 RCTs (Table 41).
 |
Table 41 ASPN Back Consensus Group Recommendations for Basivertebral Nerve Ablation |
Conclusions
The ASPN Back Guideline provides a comprehensive framework for the safe and effective utilization of interventional treatments for lumbar disorders. Interventional treatments should be utilized based on the published efficacy and relative risk data. Over the last several years, many novel techniques and procedures for lower back disorders have been developed. The authors of ASPN Back believe that this guideline will help identify gaps in the literature and provide guidance on future evidence development. Given the broad scope of interventional treatments for lower back pain, many less established interventions were not included. This represents a limitation of this guideline and provides an opportunity to make future guidelines even more robust. The ASPN Back Guideline will be updated at regular intervals to include new therapies and evidence.
Abbreviations
β-CTX, Carboxyl-terminal collagen I crosslinks; 95% CI, 95% confidence interval; ADLs, Activities of daily living; AE/SAE, Adverse event/Serious adverse event; AF, Annulus fibrosus; ANOVA, Analysis of variance; AQoL, Assessment of Quality of Life; ASA, American Society of Anesthesiologists; ASIPP, American Society of Interventional Pain Physicians; ASLR, Active straight leg raise; ASPN, American Society of Pain and Neuroscience; ASRA, American Society of Regional Anesthesia and Pain Medicine; AVBHr, Anterior vertebral body height ratio; BALP, Bone alkaline phosphatase; BDI, Beck Depression Inventory; BGP, Bone gla protein; BKP, Balloon kyphoplasty; BMC, Bone marrow concentrate; Botox, Botulinum toxin; BPI, Brief Pain Inventory; BTXA, Botulinum toxin type A; BVN, Basivertebral nerve; CDC, Centers for Disease Control; CEI, Caudal epidural injections; CGRP, Calcitonin gene-related peptide; CLPB, Chronic low back pain; CMM, Conventional medical management; CNS, Central nervous system; C-RFA, Conventional radiofrequency ablation; CRPS, Complex regional pain syndrome; CT, Computed tomography scan; DBM, Demineralized bone matrix; DDD, Degenerative disc disease; DIANA cage, Hollow threaded fusion cage for SIJ fusion; ECAP, Evoked compound action potential; ED, Emergency Department; EMG, Electromyography; EQ-5D, EuroQOL Health Questionnaire; ESI, Epidural steroid injection; FACES, Wong-Baker pain scale; FBSS, Failed back surgery syndrome; FRI, Functional Rating Index; GAS, Global Assessment of Improvement Scale; GDS-SF, Geriatric Depression Scale – Short Form; GIC/PGIC/CGIC, Global Impression of Change (patient-, clinician-); HA, Hyaluronic acid; HADS, Hospital Anxiety and Depression Scale; HCPCS, Healthcare Common Procedure Coding System; HSC, Hematopoietic stem cell; IA, Intra-articular; IASP, International Association for the Study of Pain; ICD, International Classification of Diseases; ICI, Intra-articular corticosteroid injection; IDDS, Intrathecal drug delivery; IPD, Interspinous process device; IPG, Implanted pulse generator; IPS, Interspinous process spacers; ISF, Interspinous fixation; ISS, Interspinous spacer; IT, Intrathecal; ITT, Intent to treat; IV, Intravenous; IVD, Intervertebral disc; JOA, Japanese Orthopedic Association; LA, Local anesthetic; LBP, Low back pain; LDH, Lumbar disc herniations; LFH, Ligamentum flavum hypertrophy; LFJ, Lumbar facet joint; LSS, Lumbar spinal stenosis; LTR, Localized twitch responses; MAC, Monitored anesthesia care; MBB, Medial branch blocks; MC, Modic change; MCID, Minimum clinically important difference; MCS, Mental component summary (SF-12, −36); MD, Microdiscectomy; MDA, Malondialdehyde; MED, Microendoscopic discectomy; MME, Milligram morphine equivalent; MOSS, Medical Outcomes Study-Sleep; MPC, Mesenchymal precursor cell; MPQ, McGill Pain Questionnaire; MPS, Myofascial pain syndrome; MQS, Medication Quantification Scale; MRI, Magnetic resonance imaging; MSC, Mesenchymal stem cells; MSMD, Multisite, multidepth; MVBHr, Midline vertebral body height ratio; NACC, Neurostimulation Appropriateness Consensus Committee; NASS, North American Spine Society; NCS, Numeric Categorical Scale; NDI, Neck Disability Index; NHP, Nottingham Health Profile; NICE, National Institute of Health and Clinical Excellence; NNT, Number-needed-to-treat; NP, Nucleus pulposus; NPAD, Neck Pain and Disability Scale; NPQ, Neck Pain Questionnaire; NRS, NPRS, Numeric rating scale, numeric pain rating scale; NS, Normal saline; NSAID, Nonsteroidal anti-inflammatory drug; NSM, Non-surgical management; OA, Osteoarthritis; OD, Open discectomy; ODI, Oswestry Disability Index; OMM, Optimized medical management; OPM, Optimal pain medication; PACC, Polyanalgesic Consensus Conference; PBK, Percutaneous balloon kyphoplasty; PCKP, Percutaneous curved kyphoplasty; PCS, Physical component summary (SF-12, −36); PDI, Pain Disability Index; PDQ, Pain Detect Questionnaire; PEEK, Polyether ether ketone; PELD, Percutaneous endoscopic lumbar discectomy; PFDI-20, Pelvic Floor Disability Index; PGP, Protein gene product; PILD, Percutaneous image-guided minimally invasive lumbar decompression; PKP, Percutaneous kyphoplasty; PLS, Post-laminectomy syndrome; PMMA, Polymethyl methacrylate; PNFS, Peripheral nerve field stimulation; PNS, Peripheral nerve stimulation; PPDT, Pressure pain detection thresholds; PPI, Pressure pain intensity scores; PPR, Percentage pain relief; PPT, Pressure-pain threshold; PPTT, Pressure pain tolerance thresholds; PRF, Pulsed radiofrequency; P-RFA, Pulsed radiofrequency ablation; PRGF, Plasma rich growth factor; PRP, Platelet-rich plasma; PS, Pain scale; PTED, Percutaneous transforaminal endoscopic discectomy; PTM, Pressure threshold meter; PVBHr, Posterior vertebral body height ratio; PVP, Percutaneous vertebroplasty; QoL, Quality of life; QUALEFFO, Questionnaire of the European Foundation of Osteoporosis; RCT, Randomized controlled trial; RFA, Radiofrequency ablation; RFTC, Radiofrequency thermocoagulation; rhBMP-2, Bone morphogenetic protein-2; RMQ/RMDQ, Roland-Morris Disability Questionnaire; RR, Responder rate; SANE, Single assessment numeric evaluation; SCS, Spinal cord stimulation; SD, Standard deviation; SF-12, SF-36, Short Form questionnaire; health-related quality of life (12-, 36-item); SI, Sacroiliac; SIJ, Sacroiliac joint; SIJF, Sacroiliac joint fusion; SIRP, Sacroiliac regional pain syndrome; SIS, Spine Intervention Society; SLBB, Sacral lateral branch block; SLBRFA, Sacral lateral branch radiofrequency ablation; SOD, Superoxide dismutase; SPORT, Spine Patient Outcomes Research Trial; SQS, Subcutaneous nerve stimulation; SSSD, Single site, single depth; STAI, State-Trait Anxiety Inventory; STROBE, Strengthening the Reporting of Observational Studies in Epidemiology; SVF, Stromal vascular fraction; TAC, Total antioxidant capacity; tDCS, Transcranial direct current stimulation; TFESI, Transforaminal epidural steroid injection; TIVAD, Titanium-implantable vertebral augmentation device; TPI, Trigger point injections; TRACP, Tartrate-resistant acid phosphatase; TSQ, Treatment Satisfaction Questionnaire; USPSTF, United States Preventive Services Task Force; VA, Vertebral augmentation; VAPOUR, Vertebroplasty for acute painful osteoporotic fractures; VAS, Visual analog scale; VASPI, Visual analog scale of pain intensity; VBS, Vertebral body stenting system; VCF, Vertebral compression fractures; WBC, White blood cell; WHO, World Health Organization; WHOQoL, World Health Organization quality of life health questionnaire; ZCQ, Zurich Claudication Questionnaire.
Acknowledgments
Third-party editing assistance was provided by Allison Foster, PhD, of Foster Medical Communications.
Disclosure
Prof. Dr. Dawood Sayed reports grants from Boston Scientific, during the conduct of the study; personal fees from Medtronic, Nevro, Saluda, Painteq (with options), Vertos (with options), SPR (with options), Mainstay (with options), and Surgentec, outside the submitted work. Dr Jay Grider is a stock holder of interlink spine. Dr Jonathan M Hagedorn reports personal fees for research from Abbott, Boston Scientific, Medtronic, Nevro, and Saluda, outside the submitted work. Dr Steven Falowski is a consultant and took part in research for Abbott, Aurora, CornerLoc, Medtronic, Saluda; equity from PainTeq, CornerLoc, Saluda, SPR, and Synerfuse; consultant for Vertos, outside the submitted work.
Dr Douglas Beall reports grants from Medtronic, consultant for Merit Medical, IZI (including royalty agreement), Boston Scientific, Vivex (including royalty agreement), Abbott, Cerapedics, Elliquence, Amber Implants, Avanos, Relievant, Stryker, Lenoss Medical, Piramal, ReGelTec, Kahtnu, Stratus Medical, and Genesys; consultant and research grants from Spine Biopharma, BioRestorative Therapies, and DiscGenics, during the conduct of the study. Dr Nestor D Tomycz reports consulting for SI Bone and Abbott, outside the submitted work. Dr Mark N Malinowski reports personal fees for speaking, consulting and/or medical advisory board from Abbott, Biotronik, Nalu Medical, and SI Bone, outside the submitted work. Dr Nomen Azeem reports personal fees from Boston Scientific, Vertos Medical, Spinal Simplicity, and Painteq, outside the submitted work. Dr Reda Tolba reports consulting for Medtronic and Abbott, outside the submitted work. Dr Erika Petersen reports personal fees from Abbott Neuromodulation, Biotronik, Medtronic Neuromodulation, Presidio Medical, and Vertos; research support to institution from Nalu, Mainstay Medical, Nevro, Saluda, and SPR; board of directors, stock options from SynerFuse; stock options from neuro.42, during the conduct of the study. Dr Michael E Schatman is a research consultant for Modoscript, outside the submitted work.
Dr Timothy Deer reports personal fees for consultant, research investigator, and/or stock options from Abbott, Vertos, Saluda, Mainstay, Nalu, Cornerloc, Medtronic, Boston Scientific, PainTeq, Spinal Simplicity, and Avanos, outside the submitted work; In addition, Dr Timothy Deer has a pending to Abbott. The authors report no other conflicts of interest in this work.
References
1. Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. preventive services task force: a review of the process. Am J Prev Med. 2001;20(3):21–35. doi:10.1016/S0749-3797(01)00261-6
2. Rivera CE. Lumbar Epidural Steroid Injections. Phys Med Rehabil Clin N Am. 2018;29(1):73–92. doi:10.1016/j.pmr.2017.08.007
3. van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002;16(5):761–775. doi:10.1053/berh.2002.0267
4. Van Boxem K, Cheng J, Patijn J, et al. 11. Lumbosacral radicular pain. Pain Pract. 2010;10(4):339–358. doi:10.1111/j.1533-2500.2010.00370.x
5. Shrestha P, Subba L, Agrawal P, Lohani S. Outcome of transforaminal epidural steroid injection for lumbar radiculopathy: initial three-year experience at Upendra Devkota Memorial-National Institute of Neurological and Allied Sciences, Nepal. Chin Neurosurg J. 2020;6:6. doi:10.1186/s41016-020-0184-5
6. Konstantinou K, Hider SL, Jordan JL, Lewis M, Dunn KM, Hay EM. The impact of low back-related leg pain on outcomes as compared with low back pain alone: a systematic review of the literature. Clin J Pain. 2013;29(7):644–654. doi:10.1097/AJP.0b013e31826f9a52
7. Ghai B, Bansal D, Kay JP, Vadaje KS, Wig J. Transforaminal versus parasagittal interlaminar epidural steroid injection in low back pain with radicular pain: a randomized, double-blind, active-control trial. Pain Physician. 2014;17(4):277–290.
8. Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008;9(2):227–234. doi:10.1111/j.1526-4637.2007.00341.x
9. Manchikanti L, Knezevic NN, Navani A, et al. Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines. Pain Physician. 2021;24(S1):S27–S208.
10. Gerwin RD. Diagnosis of myofascial pain syndrome. Phys Med Rehabil Clin North Am. 2014;25(2):341–355. doi:10.1016/j.pmr.2014.01.011
11. Simons DG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol. 1.
12. Mense S, Gerwin RD, editors. Central nervous system mechanisms of muscle pain: ascending pathways, central sensitization, and pain-modulating systems., in Muscle pain: understanding the mechanisms. Muscle Pain: Understanding the Mechanisms. Springer-Verlag; 2010. 105–176. doi:10.1007/978-3-540-85021-2
13. Narouze S, Benzon HT, Provenzano D, et al. Interventional Spine and Pain Procedures in Patients on Antiplatelet and Anticoagulant Medications (Second Edition): guidelines From the American Society of Regional Anesthesia and Pain Medicine, the European Society of Regional Anaesthesia and Pain Therapy, the American Academy of Pain Medicine, the International Neuromodulation Society, the North American Neuromodulation Society, and the World Institute of Pain. Reg Anesth Pain Med. 2018;43(3):225–262. doi:10.1097/AAP.0000000000000700
14. Fitzgibbon DR, Posner KL, Domino KB, et al. Chronic pain management: American Society of Anesthesiologists Closed Claims Project. Anesthesiology. 2004;100(1):98–105. doi:10.1097/00000542-200401000-00018
15. Shafer N. Pneumothorax following “trigger point” injection. JAMA. 1970;213(7):1193.
16. Ahiskalioglu E, Alici H, Dostbil A, Celik M, Ahiskalioglu A, Aksoy M. Pneumothorax after trigger point injection: a case report and review of literature. J Back Musculoskelet Rehabil. 2016;29(4):895–897. doi:10.3233/bmr-160666
17. Paik NC, Seo JW. CT-guided needle aspiration of pneumothorax from a trigger point injection. Pain Med. 2011;12(5):837–841. doi:10.1111/j.1526-4637.2010.00972.x
18. Zink W, Graf BM. Local anesthetic myotoxicity. Reg Anesth Pain Med. 2004;29(4):333–340. doi:10.1016/j.rapm.2004.02.008
19. Falco FJE, Manchikanti L, Datta S, et al. An update of the systematic assessment of the diagnostic accuracy of lumbar facet joint nerve blocks. Pain Physician. 2012;15(6):E869–907.
20. Long DM, BenDebba M, Torgerson WS, et al. Persistent back pain and sciatica in the United States: patient characteristics. J Spinal Disord. 1996;9(1):40–58.
21. Ko S, Vaccaro AR, Lee S, Lee J, Chang H. The prevalence of lumbar spine facet joint osteoarthritis and its association with low back pain in selected Korean populations. Clin Orthop Surg. 2014;6(4):385–391. doi:10.4055/cios.2014.6.4.385
22. Kalichman L, Li L, Kim DH, et al. Facet joint osteoarthritis and low back pain in the Community-based population. Spine. 2008;33(23):2560–2565. doi:10.1097/BRS.0b013e318184ef95
23. Kalichman L, Kim DH, Li L, Guermazi A, Hunter DJ. Computed tomography-evaluated features of spinal degeneration: prevalence, intercorrelation, and association with self-reported low back pain. Spine J. 2010;10(3):200–208. doi:10.1016/j.spinee.2009.10.018
24. Cohen SP, Strassels SA, Kurihara C, et al. Establishing an optimal “cutoff” threshold for diagnostic lumbar facet blocks: a prospective correlational study. Clin J Pain. 2013;29(5):382–391. doi:10.1097/AJP.0b013e31825f53bf
25. Cohen SP, Williams KA, Kurihara C, et al. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010;113(2):395–405. doi:10.1097/ALN.0b013e3181e33ae5
26. Derby R, Melnik I, Lee JE, Lee SH. Correlation of lumbar medial branch neurotomy results with diagnostic medial branch block cutoff values to optimize therapeutic outcome. Pain Med. 2012;13(12):1533–1546. doi:10.1111/j.1526-4637.2012.01500.x
27. Derby R, Melnik I, Choi J, Lee JE. Indications for repeat diagnostic medial branch nerve blocks following a failed first medial branch nerve block. Pain Physician. 2013;16(5):479–488.
28. Bogduk N, Holmes S. Controlled zygapophysial joint blocks: the travesty of cost-effectiveness. Pain Med. 2000;1(1):24–34. doi:10.1046/j.1526-4637.2000.99104.x
29. Novak S, Nemeth WC. RE: cost-effectiveness of diagnostic medial branch blocks before radiofrequency denervation. Spine J. 2008;8(2):412–413. doi:10.1016/j.spinee.2007.11.002
30. Manchikanti L, Hirsch JA, Pampati V, Boswell MV. Utilization of facet joint and sacroiliac joint interventions in Medicare population from 2000 to 2014: explosive Growth Continues! Curr Pain Headache Rep. 2016;20(10):58. doi:10.1007/s11916-016-0588-2
31. Chou R. Low back pain (chronic). BMJ Clin Evid. 2010;2010:548.
32. Cohen SP, Huang JHY, Brummett C. Facet joint pain--advances in patient selection and treatment. Nat Rev Rheumatol. 2013;9(2):101–116. doi:10.1038/nrrheum.2012.198
33. Van Kleef M, Vanelderen P, Cohen SP, Lataster A, Van Zundert J, Mekhail N. 12. Pain originating from the lumbar facet joints. Pain Pract. 2010;10(5):459–469. doi:10.1111/j.1533-2500.2010.00393.x
34. Manchikanti L, Kaye AD, Boswell MV, et al. A systematic review and best evidence synthesis of the effectiveness of therapeutic facet joint interventions in managing chronic Spinal Pain. Pain Physician. 2015;18(4):E535–582.
35. Leggett LE, Soril LJJ, Lorenzetti DL, et al. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag. 2014;19(5):e146–153. doi:10.1155/2014/834369
36. Cohen SP, Doshi TL, Constantinescu OC, et al. Effectiveness of Lumbar Facet Joint Blocks and Predictive Value before Radiofrequency Denervation: the Facet Treatment Study (FACTS), a Randomized, Controlled Clinical Trial. Anesthesiology. 2018;129(3):517–535. doi:10.1097/ALN.0000000000002274
37. Chou R, Hashimoto R, Friedly J, et al. Pain Management Injection Therapies for Low Back Pain. Agency for Healthcare Research and Quality (US); 2015. Available from: http://www.ncbi.nlm.nih.gov/books/NBK285206/.
38. Vekaria R, Bhatt R, Ellard DR, Henschke N, Underwood M, Sandhu H. Intra-articular facet joint injections for low back pain: a systematic review. Eur Spine J. 2016;25(4):1266–1281. doi:10.1007/s00586-016-4455-y
39. Ribeiro LH, Furtado RNV, Konai MS, Andreo AB, Rosenfeld A, Natour J. Effect of facet joint injection versus systemic steroids in low back pain: a randomized controlled trial. Spine. 2013;38(23):1995–2002. doi:10.1097/BRS.0b013e3182a76df1
40. Celik B, Er U, Simsek S, Altug T, Bavbek M. Effectiveness of lumbar zygapophysial joint blockage for low back pain. Turk Neurosurg. 2011;21(4):467–470. doi:10.5137/1019-5149.JTN
41. Kawu AA, Olawepo A, Salami AOO. Facet joints infiltration: a viable alternative treatment to physiotherapy in patients with low back pain due to facet joint arthropathy. Niger J Clin Pract. 2011;14(2):219–222. doi:10.4103/1119-3077.84021
42. Cohen SP, Bhaskar A, Bhatia A, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020;45(6):424–467. doi:10.1136/rapm-2019-101243
43. Boswell MV, Manchikanti L, Kaye AD, et al. A best-evidence systematic appraisal of the diagnostic accuracy and utility of facet (Zygapophysial) joint injections in chronic spinal pain. Pain Physician. 2015;18(4):E497–533.
44. Bogduk N. Interventional spine intervention society. lumbar medial branch blocks. In: Practice Guidelines for Spinal Diagnostic & Treatment Procedures.
45. Cohen SP, Hurley RW, Christo PJ, Winkley J, Mohiuddin MM, Stojanovic MP. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007;23(1):45–52. doi:10.1097/01.ajp.0000210941.04182.ea
46. Schwarzer AC, Wang SC, O’Driscoll D, Harrington T, Bogduk N, Laurent R. The ability of computed tomography to identify a painful zygapophysial joint in patients with chronic low back pain. Spine. 1995;20(8):907–912. doi:10.1097/00007632-199504150-00005
47. Van Zundert J, Vanelderen P, Kessels A, van Kleef M. Radiofrequency Treatment of Facet-related Pain: evidence and Controversies. Curr Pain Headache Rep. 2012;16(1):19–25. doi:10.1007/s11916-011-0237-8
48. Cohen SP, Moon JY, Brummett CM, White RL, Larkin TM. Medial branch blocks or intra-articular injections as a prognostic tool before lumbar facet radiofrequency denervation: a Multicenter, Case-Control Study. Reg Anesth Pain Med. 2015;40(4):376–383. doi:10.1097/AAP.0000000000000229
49. Dreyfuss P, Stout A, Aprill C, Pollei S, Johnson B, Bogduk N. The significance of multifidus atrophy after successful radiofrequency neurotomy for low back pain. PM R. 2009;1(8):719–722. doi:10.1016/j.pmrj.2009.05.014
50. Wu PB, Date ES, Kingery WS. The lumbar multifidus muscle in polysegmentally innervated. Electromyogr Clin Neurophysiol. 2000;40(8):483–485.
51. van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24(18):1937–1942. doi:10.1097/00007632-199909150-00013
52. Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine. 2008;33(12):1291–1297. doi:10.1097/BRS.0b013e31817329f0
53. Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23(6):524–529. doi:10.1097/AJP.0b013e318074c99c
54. Glover JR. Arthrography of the joints of the lumbar vertebral arches. Orthop Clin North Am. 1977;8(1):37–42.
55. Carette S, Marcoux S, Truchon R, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991;325(14):1002–1007. doi:10.1056/NEJM199110033251405
56. Kennedy DJ, Huynh L, Wong J, et al. Corticosteroid injections into lumbar facet joints: a prospective, randomized, double-blind placebo-controlled trial. Am J Phys Med Rehabil. 2018;97(10):741–746. doi:10.1097/PHM.0000000000000960
57. Ackerman WE, Munir MA, Zhang JM, Ghaleb A. Are diagnostic lumbar facet injections influenced by pain of muscular origin? Ain Pract. 2004;4(4):286–291. doi:10.1111/j.1533-2500.2004.04402.x
58. Stojanovic MP, Sethee J, Mohiuddin M, et al. MRI analysis of the lumbar spine: can it predict response to diagnostic and therapeutic facet procedures? Clin J Pain. 2010;26(2):110–115. doi:10.1097/AJP.0b013e3181b8cd4d
59. Holz SC, Sehgal N. What is the correlation between facet joint radiofrequency outcome and response to comparative medial branch blocks? Pain Physician. 2016;19(3):163–172.
60. Cohen SP, Stojanovic MP, Crooks M, et al. Lumbar zygapophysial (facet) joint radiofrequency denervation success as a function of pain relief during diagnostic medial branch blocks: a multicenter analysis. Spine J. 2008;8(3):498–504. doi:10.1016/j.spinee.2007.04.022
61. Manchikanti L, Pampati S, Cash KA. Making sense of the accuracy of diagnostic lumbar facet joint nerve blocks: an assessment of the implications of 50% relief, 80% relief, single block, or controlled diagnostic blocks. Pain Physician. 2010;13(2):133–143.
62. McCormick ZL, Marshall B, Walker J, McCarthy R, Walega DR. Long-term function, pain and medication use outcomes of radiofrequency ablation for lumbar facet syndrome. Int J Anesth Anesth. 2015;2(2). doi:10.23937/2377-4630/2/2/1028
63. Derby R, Melnik I, Lee JE, Lee SH. Cost comparisons of various diagnostic medial branch block protocols and medial branch neurotomy in a private practice setting. Pain Med. 2013;14(3):378–391. doi:10.1111/pme.12026
64. Kennedy DJ, Mattie R, Scott Hamilton A, Conrad B, Smuck M. Detection of intravascular injection during lumbar medial branch blocks: a comparison of aspiration, live fluoroscopy, and digital subtraction technology. Pain Med. 2016;17(6):1031–1036. doi:10.1093/pm/pnv073
65. Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint. A physiologic challenge. Spine. 1998;23(17):1847–1852. doi:10.1097/00007632-199809010-00008
66. Verrills P, Mitchell B, Vivian D, Nowesenitz G, Lovell B, Sinclair C. The incidence of intravascular penetration in medial branch blocks: cervical, thoracic, and lumbar spines. Spine. 2008;33(6):E174–177. doi:10.1097/BRS.0b013e318166f03d
67. Lee CJ, Kim YC, Shin JH, et al. Intravascular injection in lumbar medial branch block: a prospective evaluation of 1433 injections. Anesth Analg. 2008;106(4):1274–1278. doi:10.1213/ane.0b013e318162c358
68. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: a prospective evaluation of 7500 episodes with 43,000 nerve blocks. Pain Physician. 2012;15(2):E143–150.
69. Joo Y, Kim YC, Lee SC, et al. Impact of type of needle on incidence of intravascular injection during diagnostic lumbar medial branch block. Reg Anesth Pain Med. 2016;41(3):392–397. doi:10.1097/AAP.0000000000000381
70. Kennedy DJ, Fraiser R, Zheng P, et al. Intra-articular Steroids vs Saline for Lumbar Z-Joint Pain: a Prospective, Randomized, Double-Blind Placebo-Controlled Trial. Pain Med. 2019;20(2):246–251. doi:10.1093/pm/pny225
71. Wu J, Zhou J, Liu C, et al. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain Pract. 2017;17(7):914–924. doi:10.1111/papr.12544
72. Sae-Jung S, Jirarattanaphochai K. Outcomes of lumbar facet syndrome treated with oral diclofenac or methylprednisolone facet injection: a randomized trial. Int Orthop. 2016;40(6):1091–1098. doi:10.1007/s00264-016-3154-y
73. Buckwalter JA, Mow V, Boden S, Eyre D. Intervertebral disc structure, composition, and mechanical function. Orthopaedic Basic Sci. 2000;548–555.
74. García-Cosamalón J, Del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? J Anat. 2010;217(1):1–15. doi:10.1111/j.1469-7580.2010.01227.x
75. Ganey TM, Meisel HJ. A potential role for cell-based therapeutics in the treatment of intervertebral disc herniation. Eur Spine J. 2002;11(Suppl 2):S206–214. doi:10.1007/s00586-002-0494-7
76. Beatty NR, Lutz C, Boachie-Adjei K, Leynes TA, Lutz C, Lutz G. Spondylodiscitis due to Cutibacterium acnes following lumbosacral intradiscal biologic therapy: a case report. Regen Med. 2019;14(9):823–829. doi:10.2217/rme-2019-0008
77. Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, et al. Lumbar intradiskal platelet-rich plasma (PRP) injections: a prospective, double-blind, Randomized Controlled Study. PM R. 2016;8(1):1–10. doi:10.1016/j.pmrj.2015.08.010
78. Cheng J, Santiago KA, Nguyen JT, Solomon JL, Lutz GE. Treatment of symptomatic degenerative intervertebral discs with autologous platelet-rich plasma: follow-up at 5-9 years. Regen Med. 2019;14(9):831–840. doi:10.2217/rme-2019-0040
79. DP BEALL, GL WILSON, BISHOP R, Tally W, Clinical Trial: VAST. Safely supplementing tissue lost to degenerative disc disease. Int J Spine Surg. 2020;14(2):239–253. doi:10.14444/7033
80. Beall DP, Davis T, DePalma MJ, et al. Viable Disc Tissue Allograft Supplementation; One- and Two-level Treatment of Degenerated Intervertebral Discs in Patients with Chronic Discogenic Low Back Pain: one Year Results of the VAST Randomized Controlled Trial. Pain Physician. 2021;24(6):465–477.
81. Peng B, Pang X, Wu Y, Zhao C, Song X. A randomized placebo-controlled trial of intradiscal methylene blue injection for the treatment of chronic discogenic low back pain. Pain. 2010;149(1):124–129. doi:10.1016/j.pain.2010.01.021
82. Yin W, Pauza K, Olan WJ, Doerzbacher JF, Thorne KJ. Intradiscal injection of fibrin sealant for the treatment of symptomatic lumbar internal disc disruption: results of a prospective multicenter pilot study with 24-month follow-up. Pain Med. 2014;15(1):16–31. doi:10.1111/pme.12249
83. Ju DG, Kanim LE, Bae HW. Is there clinical improvement associated with intradiscal therapies? A Comparison Across Randomized Controlled Studies. Global Spine J. 2020;2192568220963058. doi:10.1177/2192568220963058
84. Kennedy DJ, Engel A, Kreiner DS, Nampiaparampil D, Duszynski B, MacVicar J. Fluoroscopically Guided Diagnostic and Therapeutic Intra-Articular Sacroiliac Joint Injections: a Systematic Review. Pain Med. 2015;16(8):1500–1518. doi:10.1111/pme.12833
85. Lorio M, Clerk-Lamalice O, Beall DP, Julien T. International society for the advancement of spine surgery guideline—intraosseous ablation of the basivertebral nerve for the relief of chronic low back pain. Int J Spine Surg. 2020;14(1):18–25. doi:10.14444/7002
86. Tsoi C, Griffith JF, Lee RKL, Wong PCH, Tam LS. Imaging of sacroiliitis: current status, limitations and pitfalls. Quant Imaging Med Surg. 2019;9(2):318–335. doi:10.21037/qims.2018.11.10
87. Barros G, McGrath L, Gelfenbeyn M. Sacroiliac joint dysfunction in patients with low back pain. Fed Pract. 2019;36(8):370–375.
88. Kim DK, McKenzie GA. Accessory sacroiliac joint injection for relief of buttock pain. Pain Med. 2019;20(2):412–413. doi:10.1093/pm/pny254
89. Ou-Yang DC, York PJ, Kleck CJ, Patel VV. Diagnosis and management of sacroiliac joint dysfunction. J Bone Joint Surg Am. 2017;99(23):2027–2036. doi:10.2106/JBJS.17.00245
90. Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2006;85(12):997–1006. doi:10.1097/01.phm.0000247633.68694.c1
91. Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207–218. doi:10.1016/j.math.2005.01.003
92. Szadek KM, van der Wurff P, van Tulder MW, Zuurmond WW, Perez RSGM. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J Pain. 2009;10(4):354–368. doi:10.1016/j.jpain.2008.09.014
93. Schmidt GL, Bhandutia AK, Altman DT. Management of sacroiliac joint pain. JAAOS. 2018;26(17):610–616. doi:10.5435/JAAOS-D-15-00063
94. Stanford G, Burnham RS. Is it useful to repeat sacroiliac joint provocative tests post-block? Pain Med. 2010;11(12):1774–1776. doi:10.1111/j.1526-4637.2010.00968.x
95. Spiker WR, Lawrence BD, Raich AL, Skelly AC, Brodke DS. Surgical versus injection treatment for injection-confirmed chronic sacroiliac joint pain. Evid Based Spine Care J. 2012;3(4):41–53. doi:10.1055/s-0032-1328142
96. Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013;13(1):99–116. doi:10.1586/ern.12.148
97. Thawrani DP, Agabegi SS, Asghar F. Diagnosing sacroiliac joint pain. J Am Acad Orthop Surg. 2019;27(3):85–93. doi:10.5435/JAAOS-D-17-00132
98. DePhillipo NN, Corenman DS, Strauch EL, Zalepa King LA. Sacroiliac Pain: structural Causes of Pain Referring to the SI Joint Region. Clin Spine Surg. 2019;32(6):E282–E288. doi:10.1097/BSD.0000000000000745
99. Wu L, Tafti D, Varacallo M Sacroiliac Joint Injection. StatPearls; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513245/.
100. Soto Quijano DA, Otero Loperena E. Sacroiliac Joint Interventions. Phys Med Rehabil Clin North Am. 2018;29(1):171–183. doi:10.1016/j.pmr.2017.09.004
101. Guan F, Bao R, Zhu L, et al. Risk Factors of Postoperative Low Back Pain for Low-Grade Degenerative Spondylolisthesis: an At Least 2-Year Follow-Up Retrospective Study. World Neurosurg. 2017;107:789–794. doi:10.1016/j.wneu.2017.08.109
102. Jung MW, Schellhas K, Johnson B. Use of diagnostic injections to evaluate sacroiliac joint pain. Int J Spine Surg. 2020;14(Suppl s1):S30–S34. doi:10.14444/6081
103. Falowski S, Sayed D, Pope J, et al. A review and algorithm in the diagnosis and treatment of sacroiliac joint pain. J Pain Res. 2020;13:3337–3348. doi:10.2147/JPR.S279390
104. Plastaras CT, Joshi AB, Garvan C, et al. Adverse events associated with fluoroscopically guided sacroiliac joint injections. PM R. 2012;4(7):473–478. doi:10.1016/j.pmrj.2012.02.001
105. Kokar S, Kayhan Ö, Şencan S, Gündüz OH. The role of sacroiliac joint steroid injections in the treatment of axial spondyloarthritis. Arch Rheumatol. 2021;36(1):80–88. doi:10.46497/ArchRheumatol.2021.8043
106. Kennedy DJ, Schneider B, Casey E, et al. Vasovagal rates in flouroscopically guided interventional procedures: a study of over 8000 injections. Pain Med. 2013;14(12):1854–1859. doi:10.1111/pme.12241
107. Lee MH, Byon H-J, Jung HJ, Cha Y-D, Lee DI. Pyomyositis of the iliacus muscle and pyogenic sacroiliitis after sacroiliac joint block -A case report-. Korean J Anesthesiol. 2013;64(5):464–468. doi:10.4097/kjae.2013.64.5.464
108. Meydani A, Schwartz RA, Foye PM, Patel AD. Herpes simplex following intra-articular sacroiliac corticosteroid injection. Acta Dermatovenerol Alp Pannonica Adriat. 2009;18(3):135–137.
109. Maigne J-Y, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine. 1996;21(16):1889–1892. doi:10.1097/00007632-199608150-00012
110. Van der wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87(1):10–14. doi:10.1016/j.apmr.2005.09.023
111. Chou LH, Slipman CW, Bhagia SM, et al. Inciting events initiating injection-proven sacroiliac joint syndrome. Pain Med. 2004;5(1):26–32. doi:10.1111/j.1526-4637.2004.04009.x
112. Schneider BJ, Ehsanian R, Levin J, Huynh L, Kennedy DJ, McCormick ZL. Intra-articular sacroiliac joint needle placement: ultrasound, fluoroscopy, and the criterion standard. Am J Phys Med Rehabil. 2020;99(6):e79. doi:10.1097/PHM.0000000000001288
113. Rosenberg JM, Quint TJ, de Rosayro AM. Computerized tomographic localization of clinically-guided sacroiliac joint injections. Clin J Pain. 2000;16(1):18–21. doi:10.1097/00002508-200003000-00004
114. Hansen HC. Is fluoroscopy necessary for sacroiliac joint injections? Pain Phys. 2003;6(2):155–158.
115. Jee H, Lee JH, Park KD, Ahn J, Park Y. Ultrasound-guided versus fluoroscopy-guided sacroiliac joint intra-articular injections in the noninflammatory sacroiliac joint dysfunction: a prospective, randomized, single-blinded study. Arch Phys Med Rehabil. 2014;95(2):330–337. doi:10.1016/j.apmr.2013.09.021
116. Fortin JD, Tolchin RB. Sacroiliac arthrograms and post-arthrography computerized tomography. Pain Physician. 2003;6(3):287–290.
117. Zheng P, Schneider BJ, Yang A, McCormick ZL. Image-guided sacroiliac joint injections: an evidence-based review of best practices and clinical outcomes. PM R. 2019;11(Suppl 1):S98–S104. doi:10.1002/pmrj.12191
118. Chuang CW, Hung SK, Pan PT, Kao MC. Diagnosis and interventional pain management options for sacroiliac joint pain. Ci Ji Yi Xue Za Zhi. 2019;31(4):207–210. doi:10.4103/tcmj.tcmj_54_19
119. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20(1):31–37. doi:10.1097/00007632-199501000-00007
120. Engel A, MacVicar J, Bogduk N. A philosophical foundation for diagnostic blocks, with criteria for their validation. Pain Med. 2014;15(6):998–1006. doi:10.1111/pme.12436
121. Chou R. Guideline for the Evaluation and Management of Low Back Pain: evidence Review. 2009.
122. Manchikanti L, Datta S, Derby R, et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 1. Diagnostic interventions. Pain Physician. 2010;13(3):E141–174.
123. Liliang PC, Lu K, Liang CL, Tsai YD, Wang KW, Chen HJ. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med. 2011;12(4):565–570. doi:10.1111/j.1526-4637.2011.01087.x
124. Mitchell B, MacPhail T, Vivian D, Verrills P, Barnard A. Diagnostic Sacroiliac Joint Injections: is a Control Block Necessary? Surgical Science. 2015;6(7):273–281. doi:10.4236/ss.2015.67041
125. Dreyfuss P, Henning T, Malladi N, Goldstein B, Bogduk N. The ability of multi-site, multi-depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2009;10(4):679–688. doi:10.1111/j.1526-4637.2009.00631.x
126. Laslett M, McDonald B, Tropp H, Aprill CN, Öberg B. Agreement between diagnoses reached by clinical examination and available reference standards: a prospective study of 216 patients with lumbopelvic pain. BMC Musculoskelet Disord. 2005;6(1):28. doi:10.1186/1471-2474-6-28
127. DePalma MJ, Ketchum JM, Trussell BS, Saullo TR, Slipman CW. Does the location of low back pain predict its source? Pm&r. 2011;3(1):33–39. doi:10.1016/j.pmrj.2010.09.006
128. Cohen SP, Hameed H, Kurihara C, et al. The effect of sedation on the accuracy and treatment outcomes for diagnostic injections: a randomized, controlled, crossover study. Pain Med. 2014;15(4):588–602. doi:10.1111/pme.12389
129. Scholten PM, Patel SI, Christos PJ, Singh JR. Short-term efficacy of sacroiliac joint corticosteroid injection based on arthrographic contrast patterns. PM R. 2015;7(4):385–391. doi:10.1016/j.pmrj.2014.10.007
130. Maugars Y, Mathis C, Berthelot JM, Charlier C, Prost A. Assessment of the efficacy of sacroiliac corticosteroid injections in spondylarthropathies: a double-blind study. Br J Rheumatol. 1996;35(8):767–770. doi:10.1093/rheumatology/35.8.767
131. Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16(12):1285–1290. doi:10.1089/acm.2010.0031
132. Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44(3):285–290. doi:10.1111/j.1532-5415.1996.tb00915.x
133. Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417–425. doi:10.1111/j.1533-2500.2012.00565.x
134. Ishimoto Y, Yoshimura N, Muraki S, et al. Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthritis Cartilage. 2012;20(10):1103–1108. doi:10.1016/j.joca.2012.06.018
135. Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679–686. doi:10.1007/s00586-009-0919-7
136. Jain S, Deer T, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5):331–348. doi:10.2217/pmt-2020-0037
137. Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016;19(3):E365–410.
138. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148–151. doi:10.1097/00002508-199806000-00010
139. Ammendolia C, Stuber KJ, Rok E, et al. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst Rev. 2013;1(8):CD010712. doi:10.1002/14651858.CD010712
140. Lingreen R, Grider JS. Retrospective review of patient self-reported improvement and post-procedure findings for mild (minimally invasive lumbar decompression). Pain Physician. 2010;13(6):555–560.
141. Chopko B, Caraway DL. MiDAS I (mild Decompression Alternative to Open Surgery): a preliminary report of a prospective, multi-center clinical study. Pain Physician. 2010;13(4):369–378.
142. Benyamin RM, Staats PS, MiDAS Encore I. MILD® Is an Effective Treatment for Lumbar Spinal Stenosis with Neurogenic Claudication: miDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229–242.
143. Levy RM, Deer TR. Systematic safety review and meta-analysis of procedural experience using percutaneous access to treat symptomatic lumbar spinal stenosis. Pain Med. 2012;13(12):1554–1561. doi:10.1111/j.1526-4637.2012.01504.x
144. Schomer DF, Solsberg D, Wong W, Chopko BW. mild(®) lumbar decompression for the treatment of lumbar spinal stenosis. Neuroradiol J. 2011;24(4):620–626. doi:10.1177/197140091102400419
145. Sénégas J. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J. 2002;11(Suppl 2):S164–169. doi:10.1007/s00586-002-0423-9
146. Deer TR, Sayed D, Malinowski MN, et al. A review of emerging evidence for utilization of a percutaneous interspinous process decompression device to treat symptomatic lumbar adjacent-segment degeneration. Pain Med. 2019;20(Suppl 2):S9–S13. doi:10.1093/pm/pnz247
147. Lauryssen C, Jackson RJ, Baron JM, et al. Stand-alone interspinous spacer versus decompressive laminectomy for treatment of lumbar spinal stenosis. Expert Rev Med Devices. 2015;12(6):763–769. doi:10.1586/17434440.2015.1100071
148. Nunley PD, Shamie AN, Blumenthal SL, Orndorff D, Block JE, Geisler FH. Interspinous process decompression: expanding treatment options for lumbar spinal stenosis. Biomed Res Int. 2016;2016:3267307. doi:10.1155/2016/3267307
149. Diwan S, Sayed D, Deer TR, Salomons A, Liang K. An algorithmic approach to treating lumbar spinal stenosis: an evidenced-based approach. Pain Med. 2019;20(Suppl 2):S23–S31. doi:10.1093/pm/pnz133
150. Parker SL, Anderson LH, Nelson T, Patel VV. Cost-effectiveness of three treatment strategies for lumbar spinal stenosis: conservative care, laminectomy, and the Superion interspinous spacer. Int J Spine Surg. 2015;9:28. doi:10.14444/2028
151. Tekmyster G, Sayed D, Cairns KD, Raso LJ, Kim C, Block JE. Interspinous Process Decompression With The Superion® Spacer For Lumbar Spinal Stenosis: real-World Experience From A Device Registry. Med Devices. 2019;12:423–427. doi:10.2147/MDER.S220431
152. Patel VV, Whang PG, Haley TR, et al. Superion interspinous process spacer for intermittent neurogenic claudication secondary to moderate lumbar spinal stenosis: two-year results from a randomized controlled FDA-IDE pivotal trial. Spine. 2015;40(5):275–282. doi:10.1097/BRS.0000000000000735
153. Gibson JA, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: the future ‘gold standard’ for discectomy?–A review. The Surgeon. 2012;10(5):290–296.
154. Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14(1):180–191.
155. Haines SJ, Jordan N, Boen JR, et al. Discectomy strategies for lumbar disc herniation: results of the LAPDOG trial. J Clin Neuroscience. 2002;9(4):411–417.
156. Thomé C, Barth M, Scharf J, Schmiedek P. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine. 2005;2(3):271–278.
157. Barrios C, Ahmed M, Arrótegui J, Björnsson A, Gillström P. Microsurgery versus standard removal of the herniated lumbar disc: a 3-year comparison in 150 cases. Acta Orthop Scand. 1990;61(5):399–403.
158. Silverplats K, Lind B, Zoëga B, et al. Clinical factors of importance for outcome after lumbar disc herniation surgery: long-term follow-up. Eur Spine J. 2010;19(9):1459–1467.
159. Virk SS, Diwan A, Phillips FM, Sandhu H, Khan SN. What is the rate of revision discectomies after primary discectomy on a national scale? Clin Orthopaedics Related Res. 2017;475(11):2752–2762.
160. Patel N, Singh V. Percutaneous lumbar laser discectomy: literature review and a retrospective analysis of 65 cases. Photomed Laser Surg. 2018;36(10):518–521.
161. Abrishamkar S, Kouchakzadeh M, Mirhosseini A, et al. Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J res med sci. 2015;20(12):1133.
162. Brouwer PA, Brand R, van den Akker-van Marle ME, et al. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: two-year results of a randomised controlled trial. Interventional Neuroradiol. 2017;23(3):313–324.
163. Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus. 1999;7(5):E7.
164. Kambin P. Arthroscopic microdiscectomy. J Arthroscopic Related Surgery. 1992;8(3):287–295.
165. Alvi MA, Kerezoudis P, Wahood W, Goyal A, Bydon M. Operative approaches for lumbar disc herniation: a systematic review and multiple treatment meta-analysis of conventional and minimally invasive surgeries. World Neurosurg. 2018;114:391–407.
166. Anichini G, Landi A, Caporlingua F, et al. Lumbar endoscopic microdiscectomy: where are we now? An updated literature review focused on clinical outcome, complications, and rate of recurrence. Biomed Res Int. 2015;2015:548.
167. Li X, Chang H, Meng X. Tubular microscopes discectomy versus conventional microdiscectomy for treating lumbar disk herniation: systematic review and meta-analysis. Medicine. 2018;97:5.
168. Riesenburger RI, David CA. Lumbar microdiscectomy and microendoscopic discectomy. Minimally Invasive Therapy allied Technologies. 2006;15(5):267–270.
169. Wagner R, Haefner M. Indications and Contraindications of Full-Endoscopic Interlaminar Lumbar Decompression. World Neurosurg. 2021;145:657–662. doi:10.1016/j.wneu.2020.08.042
170. Teli M, Lovi A, Brayda-Bruno M, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19(3):443–450. doi:10.1007/s00586-010-1290-4
171. Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a Prospective Randomised Study. J Orthop Surg. 2011;19(1):30–34. doi:10.1177/230949901101900107
172. Hussein M, Abdeldayem M, Mattar M Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up | springerLink. Available from: https://link.springer.com/article/10.1007/s00586-014-3296-9.
173. Chen Z, Zhang L, Dong J. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial in: journal of Neurosurgery. Spine. 2018;28(3):98.
174. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a Prospective, Randomized, Controlled Study. Spine. 2008;33(9):931–939. doi:10.1097/BRS.0b013e31816c8af7
175. Pan L, Zhang P, Yin Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surgery. 2014;12(5):534–537. doi:10.1016/j.ijsu.2014.02.015
176. Ding Z, Yong-qing TAO. Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Int Trans Med. 2017;5(1):29–33.
177. Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a Prospective Randomized Study. Neurosurgery. 2008;62(1):174–182. doi:10.1227/01.NEU.0000311075.56486.C5
178. Franke J, Greiner-Perth R, Boehm H, et al. Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J. 2009;18(7):992–1000. doi:10.1007/s00586-009-0964-2
179. Pan Z, Ha Y, Yi S, Cao K. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) Technique in Treating Lumbar Disc Herniation. Med Sci Monit. 2016;22:530–539. doi:10.12659/MSM.894870
180. Chen X, Chamoli U, Castillo JV, Ramakrishna VA, Diwan AD. Complication rates of different discectomy techniques for symptomatic lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J. 2020;29(7):1752–1770.
181. Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int J Surgery. 2016;31:86–92.
182. Gadjradj PS, Harhangi BS, Amelink J, et al. Percutaneous transforaminal endoscopic discectomy versus open microdiscectomy for lumbar disc herniation: a systematic review and meta-analysis. Spine. 2021;46(8):538.
183. Xu J, Li Y, Wang B, et al. Minimum 2-Year efficacy of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy: a meta-analysis. World Neurosurg. 2020;138:19–26.
184. Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;1(1):CD010264. doi:10.1002/14651858.CD010264.pub2
185. Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl KM, Schwab JM. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009;5(7):392–403. doi:10.1038/nrneurol.2009.90
186. Backstrom KM, Whitman JM, Flynn TW. Lumbar spinal stenosis-diagnosis and management of the aging spine. Man Ther. 2011;16(4):308–317. doi:10.1016/j.math.2011.01.010
187. Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6(6):461–472. doi:10.1097/00002517-199306060-00001
188. Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18(15):2231–2238. doi:10.1097/00007632-199311000-00015
189. Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11(6):594–598. doi:10.1007/s00586-002-0469-8
190. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(6Suppl):190S–194S. doi:10.1016/j.spinee.2004.07.007
191. Gonzalez-Blohm SA, Doulgeris JJ, Aghayev K, Lee WE, Volkov A, Vrionis FD. Biomechanical analysis of an interspinous fusion device as a stand-alone and as supplemental fixation to posterior expandable interbody cages in the lumbar spine: laboratory investigation. J Neurosurg Spine. 2014;20(2):209–219. doi:10.3171/2013.10.SPINE13612
192. Karahalios DG, Musacchio MJ. Lumbar interspinous devices: fusion and motion sparing. In: Holly LT, Anderson PA editors. Essentials of Spinal Stabilization. Springer International Publishing; 2017:321–334. doi:10.1007/978-3-319-59713-3_25
193. Kim HJ, Bak KH, Chun HJ, Oh SJ, Kang TH, Yang MS. Posterior Interspinous Fusion Device for One-Level Fusion in Degenerative Lumbar Spine Disease: comparison with Pedicle Screw Fixation - Preliminary Report of at Least One Year Follow Up. J Korean Neurosurg Soc. 2012;52(4):359–364. doi:10.3340/jkns.2012.52.4.359
194. Vokshoor A, Khurana S, Wilson D, Filsinger P. Clinical and radiographic outcomes after spinous process fixation and posterior fusion in an elderly cohort. Surg Technol Int. 2014;XXV:271–276.
195. Postacchini F, Postacchini R, Menchetti PPM, Sessa P, Paolino M, Cinotti G. Lumbar interspinous process fixation and fusion with stand-alone interlaminar lumbar instrumented fusion implant in patients with degenerative spondylolisthesis undergoing decompression for spinal stenosis. Asian Spine J. 2016;10(1):27–37. doi:10.4184/asj.2016.10.1.27
196. Schmidt S, Franke J, Rauschmann M, Adelt D, Bonsanto MM, Sola S. Prospective, randomized, multicenter study with 2-year follow-up to compare the performance of decompression with and without interlaminar stabilization. J Neurosurg Spine. 2018;28(4):406–415. doi:10.3171/2017.11.SPINE17643
197. Musacchio MJ, Lauryssen C, Davis RJ, et al. Evaluation of decompression and interlaminar stabilization compared with decompression and fusion for the treatment of lumbar spinal stenosis: 5-year follow-up of a prospective, randomized, controlled trial. Int J Spine Surg. 2016;10. doi:10.14444/3006
198. Chin KR, Pencle FJR, Benny A, Seale JA. Greater than 5-year follow-up of outpatient L4-L5 lumbar interspinous fixation for degenerative spinal stenosis using the INSPAN device. J Spine Surg. 2020;6(3):549–554. doi:10.21037/jss-20-547
199. Raikar SV, Patil AA, Pandey DK, Kumar SR. Inter spinal fixation and stabilization device for lumbar radiculopathy and back pain. Cureus. 2021;13(11):e19956. doi:10.7759/cureus.19956
200. Falowski SM, Mangal V, Pope J, et al. Multicenter retrospective review of safety and efficacy of a novel minimally invasive lumbar interspinous fusion device. JPR. 2021;14:1525–1531. doi:10.2147/JPR.S304957
201. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537–567. doi:10.1111/j.1469-7580.2012.01564.x
202. Hansen H, Manchikanti L, Simopoulos TT, et al. A systematic evaluation of the therapeutic effectiveness of sacroiliac joint interventions. Pain Physician. 2012;15(3):E247–278.
203. Dengler J, Kools D, Pflugmacher R, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Joint Surg Am. 2019;101(5):400–411. doi:10.2106/JBJS.18.00022
204. Sturesson B, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Dengler J. Six-month outcomes from a randomized controlled trial of minimally invasive SI joint fusion with triangular titanium implants vs conservative management. Eur Spine J. 2017;26(3):708–719. doi:10.1007/s00586-016-4599-9
205. Duhon BS, Bitan F, Lockstadt H, et al. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg. 2016;10:13. doi:10.14444/3013
206. Rudolf L. Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: report of the First 50 Patients and Outcomes. Open Orthop J. 2012;6:495–502. doi:10.2174/1874325001206010495
207. Cummings J, Capobianco RA. Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res. 2013;7(1):12. doi:10.1186/1750-1164-7-12
208. Sachs D, Capobianco R, Cher D, et al. One-year outcomes after minimally invasive sacroiliac joint fusion with a series of triangular implants: a multicenter, patient-level analysis. Med Devices. 2014;7:299–304. doi:10.2147/MDER.S56491
209. Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013;7(1):14. doi:10.1186/1750-1164-7-14
210. Vanaclocha V, Herrera JM, Sáiz-Sapena N, Rivera-Paz M, Verdú-López F. Minimally invasive sacroiliac joint fusion, radiofrequency denervation, and conservative management for sacroiliac joint pain: 6-year comparative case series. Neurosurgery. 2018;82(1):48–55. doi:10.1093/neuros/nyx185
211. Dengler JD, Kools D, Pflugmacher R, et al. 1-Year Results of a Randomized Controlled Trial of Conservative Management vs. Minimally Invasive Surgical Treatment for Sacroiliac Joint Pain. Pain Physician. 2017;20(6):537–550.
212. Collinge C, Coons D, Aschenbrenner J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: an anatomical cadaver study. J Orthop Trauma. 2005;19(2):96–101. doi:10.1097/00005131-200502000-00005
213. Maled I, Velez R, Lopez R, Batalla L, Caja VL. Pseudoaneurysm of the superior gluteal artery during iliosacral screw fixation. Acta Orthop Belg. 2007;73(4):544–547.
214. McGuire RA, Chen Z, Donahoe K. Dual fibular allograft dowel technique for sacroiliac joint arthrodesis. Evid Based Spine Care J. 2012;3(3):21–28. doi:10.1055/s-0032-1327806
215. Sayed D, Amirdelfan K, Naidu RK, Raji OR, Falowski S, Cadaver-Based Biomechanical A. Evaluation of a Novel Posterior Approach to Sacroiliac Joint Fusion: analysis of the Fixation and Center of the Instantaneous Axis of Rotation. MDER. 2021;14:435–444. doi:10.2147/MDER.S347763
216. Shamrock AG, Patel A, Alam M, Shamrock KH, Al Maaieh M. The safety profile of percutaneous minimally invasive sacroiliac joint fusion. Global Spine J. 2019;9(8):874–880. doi:10.1177/2192568218816981
217. Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg. 2015;9. doi:10.14444/2040
218. Sayed D, Balter K, Pyles S, Lam CM, Multicenter Retrospective A. Analysis of the long-term efficacy and safety of a novel posterior sacroiliac fusion device. J Pain Res. 2021;14:3251–3258. doi:10.2147/JPR.S326827
219. Rajpal S, Burneikiene S. Minimally invasive sacroiliac joint fusion with cylindrical threaded implants using intraoperative stereotactic navigation. World Neurosurg. 2019;122:e1588–e1591. doi:10.1016/j.wneu.2018.11.116
220. Fuchs V, Ruhl B. Distraction arthrodesis of the sacroiliac joint: 2-year results of a descriptive prospective multi-center cohort study in 171 patients. Eur Spine J. 2018;27(1):194–204. doi:10.1007/s00586-017-5313-2
221. Deer TR, Rupp A, Budwany R, et al. Pain relief salvage with a novel minimally invasive posterior sacroiliac joint fusion device in patients with previously implanted pain devices and therapies. J Pain Res. 2021;14:2709–2715. doi:10.2147/JPR.S325059
222. Calodney AK, Azeem N, Buchanan P, et al. Six month interim outcomes from secure: a single arm, multicenter, prospective, clinical study on a novel minimally invasive posterior sacroiliac fusion device. Expert Rev Med Devices. 2022;19(5):451–461. doi:10.1080/17434440.2022.2090244
223. Martin CT, Haase L, Lender PA, Polly DW. Minimally Invasive Sacroiliac Joint Fusion: the Current Evidence. Int J Spine Surg. 2020;14(Suppl 1):S20–S29. doi:10.14444/6072
224. Polly DW, Swofford J, Whang PG, et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg. 2016:10. doi:10.14444/3028
225. Miller LE, Reckling WC, Block JE. Analysis of postmarket complaints database for the iFuse SI Joint Fusion System®: a minimally invasive treatment for degenerative sacroiliitis and sacroiliac joint disruption. Med Devices. 2013;6:77–84. doi:10.2147/MDER.S44690
226. Woods M, Birkholz D, MacBarb R, Capobianco R, Woods A. Utility of intraoperative neuromonitoring during minimally invasive fusion of the sacroiliac joint. Adv Orthop. 2014;2014. doi:10.1155/2014/154041
227. Rappoport LH, Luna IY, Joshua G. Minimally Invasive Sacroiliac Joint Fusion Using a Novel Hydroxyapatite-Coated Screw: preliminary 1-Year Clinical and Radiographic Results of a 2-Year Prospective Study. World Neurosurg. 2017;101:493–497. doi:10.1016/j.wneu.2017.02.046
228. Araghi A, Woodruff R, Colle K, et al. Pain and Opioid use outcomes following minimally invasive sacroiliac joint fusion with decortication and bone grafting: the evolusion clinical trial. Open Orthop J. 2017;11:1440–1448. doi:10.2174/1874325001711011440
229. Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular Anchorage screws: a prospective outcome study. Eur Spine J. 2013;22(10):2325–2331. doi:10.1007/s00586-013-2825-2
230. Mansoorinasab M, Abdolhoseinpour H. A review and update of vertebral fractures due to metastatic tumors of various sites to the spine: percutaneous vertebroplasty. Interv Med Appl Sci. 2015;10(1):1–6. doi:10.1556/1646.10.2018.03
231. Borgen TT, Bjørnerem Å, Solberg LB, et al. High prevalence of vertebral fractures and low trabecular bone score in patients with fragility fractures: a cross-sectional sub-study of NoFRACT. Bone. 2019;122:14–21. doi:10.1016/j.bone.2019.02.008
232. Crans GG, Silverman SL, Genant HK, Glass EV, Krege JH. Association of severe vertebral fractures with reduced quality of life: reduction in the incidence of severe vertebral fractures by teriparatide. Arthritis Rheum. 2004;50(12):4028–4034. doi:10.1002/art.20671
233. Melton LJ, Kyle RA, Achenbach SJ, Oberg AL, Rajkumar SV. Fracture risk with multiple myeloma: a Population-Based Study. J Bone Mineral Res. 2005;20(3):487–493. doi:10.1359/JBMR.041131
234. Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008;7(5):459–466. doi:10.1016/S1474-4422(08
235. Quraishi NA, Gokaslan ZL, Boriani S. The surgical management of metastatic epidural compression of the spinal cord. J Bone Joint Surg Br. 2010;92(8):1054–1060. doi:10.1302/0301-620X.92B8.22296
236. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi:10.3322/caac.21254
237. Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110(8):1860–1867. doi:10.1002/cncr.22991
238. Barragán-Campos HM, Vallée JN, Lo D, et al. Percutaneous vertebroplasty for spinal metastases: complications. Radiology. 2006;238(1):354–362. doi:10.1148/radiol.2381040841
239. Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–1542. doi:10.1007/s00198-017-3909-3
240. Curtis JR, Taylor AJ, Matthews RS, et al. “Pathologic” fractures: should these be included in epidemiologic studies of osteoporotic fractures? Osteoporos Int. 2009;20(11):1969–1972. doi:10.1007/s00198-009-0840-2
241. Johnell O, Kanis JA, Odén A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15(1):38–42. doi:10.1007/s00198-003-1490-4
242. Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90(7):1479–1486. doi:10.2106/JBJS.G.00675
243. Goldstein CL, Chutkan NB, Choma TJ, Orr RD. Management of the Elderly With Vertebral Compression Fractures. Neurosurgery. 2015;77(Suppl 4):S33–45. doi:10.1227/NEU.0000000000000947
244. Ong KL, Beall DP, Frohbergh M, Lau E, Hirsch JA. Were VCF patients at higher risk of mortality following the 2009 publication of the vertebroplasty “sham” trials? Osteoporos Int. 2018;29(2):375–383. doi:10.1007/s00198-017-4281-z
245. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. doi:10.1359/jbmr.061113
246. Hirsch JA, Beall DP, Chambers MR, et al. Management of vertebral fragility fractures: a clinical care pathway developed by a multispecialty panel using the RAND/UCLA Appropriateness Method. Spine J. 2018;18(11):2152–2161. doi:10.1016/j.spinee.2018.07.025
247. Epstein NE. A Comparison of Kyphoplasty, Vertebroplasty, or Non-Surgical Treatment of Traumatic/Atraumatic Osteoporotic Vertebral Compression Fractures: a Short Review. Surg Neurol Int. 2019;10:54. doi:10.25259/SNI-123-2019
248. Beall DP. Vertebral Augmentation: The Comprehensive Guide to Vertebroplasty, Kyphoplasty, and Implant Augmentation.
249. Clerk-Lamalice O, Beall DP, Ong K, Lorio MP, Policy ISASS. 2018—Vertebral Augmentation: coverage Indications, Limitations, and/or Medical Necessity. Int J Spine Surg. 2019;13(1):1–10. doi:10.14444/5096
250. Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373(9668):1016–1024. doi:10.1016/S0140-6736(09)
251. Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10052):1408–1416. doi:10.1016/S0140-6736(16)
252. Marcia S, Muto M, Hirsch JA, et al. What is the role of vertebral augmentation for osteoporotic fractures? A review of the recent literature. Neuroradiology. 2018;60(8):777–783. doi:10.1007/s00234-018-2042-0
253. McCall T, Cole C, Dailey A. Vertebroplasty and kyphoplasty: a comparative review of efficacy and adverse events. Curr Rev Musculoskelet Med. 2008;1(1):17–23. doi:10.1007/s12178-007-9013-0
254. Saracen A, Kotwica Z. Complications of percutaneous vertebroplasty: an analysis of 1100 procedures performed in 616 patients. Medicine. 2016;95(24):e3850. doi:10.1097/MD.0000000000003850
255. Xiao H, Yang J, Feng X, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S77–85. doi:10.1007/s00590-014-1502-4
256. Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg. 2017;101:633–642. doi:10.1016/j.wneu.2017.01.124
257. Tomé-Bermejo F, Piñera AR, Duran-álvarez C, et al. Identification of risk factors for the occurrence of cement leakage during percutaneous vertebroplasty for painful osteoporotic or malignant vertebral fracture. Spine. 2014;39(11):E693–E700. doi:10.1097/BRS.0000000000000294
258. Zhu RS, Kan SL, Ning GZ, et al. Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporos Int. 2019;30(2):287–298. doi:10.1007/s00198-018-4804-2
259. Zhang B, Chen G, Yang X, Fan T, Chen Z. Percutaneous kyphoplasty versus percutaneous vertebroplasty for neurologically intact osteoporotic Kümmell’s disease: a systematic review and meta-analysis. Global Spine J. 2021;2192568220984129. doi:10.1177/2192568220984129
260. Beall DP, Chambers MR, Thomas S, et al. Prospective and Multicenter Evaluation of Outcomes for Quality of Life and Activities of Daily Living for Balloon Kyphoplasty in the Treatment of Vertebral Compression Fractures: the EVOLVE Trial. Neurosurgery. 2019;84(1):169–178. doi:10.1093/neuros/nyy017
261. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361(6):569–579. doi:10.1056/NEJMoa0900563
262. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361(6):557–568. doi:10.1056/NEJMoa0900429
263. Jha RM, Yoo AJ, Hirsch AE, Growney M, Hirsch JA. Predictors of successful palliation of compression fractures with vertebral augmentation: single-center experience of 525 cases. J Vasc Interv Radiol. 2009;20(6):760–768. doi:10.1016/j.jvir.2009.01.037
264. Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res. 2011;26(7):1627–1637. doi:10.1002/jbmr.364
265. Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011;12(3):225–235. doi:10.1016/S1470-2045(11)
266. Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J. 2012;21(9):1826–1843. doi:10.1007/s00586-012-2314-z
267. Anderson PA, Froyshteter AB, Tontz WL. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Miner Res. 2013;28(2):372–382. doi:10.1002/jbmr.1762
268. Yuan WH, Hsu HC, Lai KL. Vertebroplasty and balloon kyphoplasty versus conservative treatment for osteoporotic vertebral compression fractures: a meta-analysis. Medicine. 2016;95(31):e4491. doi:10.1097/MD.0000000000004491
269. Xie L, Zhao ZG, Zhang SJ, Hu YB. Percutaneous vertebroplasty versus conservative treatment for osteoporotic vertebral compression fractures: an updated meta-analysis of prospective randomized controlled trials. Int J Surg. 2017;47:25–32. doi:10.1016/j.ijsu.2017.09.021
270. Hoshino M, Takahashi S, Yasuda H, et al. Balloon kyphoplasty versus conservative treatment for acute osteoporotic vertebral fractures with poor prognostic factors: propensity score matched analysis using data from two Prospective Multicenter Studies. Spine. 2019;44(2):110–117. doi:10.1097/BRS.0000000000002769
271. Griffoni C, Lukassen JNM, Babbi L, et al. Percutaneous vertebroplasty and balloon kyphoplasty in the treatment of osteoporotic vertebral fractures: a prospective randomized comparison. Eur Spine J. 2020;29(7):1614–1620. doi:10.1007/s00586-020-06434-3
272. Zhang L, Zhai P. A comparison of percutaneous vertebroplasty versus conservative treatment in terms of treatment effect for osteoporotic vertebral compression fractures: a meta-analysis. Surg Innov. 2020;27(1):19–25. doi:10.1177/1553350619869535
273. Láinez Ramos-Bossini AJ, López Zúñiga D, Ruiz Santiago F. Percutaneous vertebroplasty versus conservative treatment and placebo in osteoporotic vertebral fractures: meta-analysis and critical review of the literature. Eur Radiol. 2021. doi:10.1007/s00330-021-08018-1
274. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100(3Suppl Spine):254–267. doi:10.3171/spi.2004.100.3.0254
275. Kumar K, North R, Taylor R, et al. Spinal cord stimulation vs. conventional medical management: a prospective, randomized, controlled, multicenter study of patients with failed back surgery syndrome (PROCESS Study). Neuromodulation. 2005;8(4):213–218. doi:10.1111/j.1525-1403.2005.00027.x
276. Kumar K, Hunter G, Demeria D. Spinal cord stimulation in treatment of chronic benign pain: challenges in treatment planning and present status, a 22-year experience. Neurosurgery. 2006;58(3):481–496. doi:10.1227/01.NEU.0000192162.99567.96
277. Mekhail NA, Mathews M, Nageeb F, Guirguis M, Mekhail MN, Cheng J. Retrospective review of 707 cases of spinal cord stimulation: indications and complications. Pain Pract. 2011;11(2):148–153. doi:10.1111/j.1533-2500.2010.00407.x
278. Babu R, Hazzard MA, Huang KT, et al. Outcomes of percutaneous and paddle lead implantation for spinal cord stimulation: a comparative analysis of complications, reoperation rates, and health-care costs. Neuromodulation. 2013;16(5):418–427. doi:10.1111/ner.12065
279. Eldabe S, Buchser E, Duarte RV. Complications of spinal cord stimulation and peripheral nerve stimulation techniques: a review of the literature. Pain Medicine. 2016;17(2):325–336. doi:10.1093/pm/pnv025
280. Hoelzer BC, Bendel MA, Deer TR, et al. Spinal cord stimulator implant infection rates and risk factors: a Multicenter Retrospective Study. Neuromodulation. 2017;20(6):558–562. doi:10.1111/ner.12609
281. Levy R, Henderson J, Slavin K, et al. Incidence and avoidance of neurologic complications with paddle type spinal cord stimulation leads. Neuromodulation. 2011;14(5):412–422. doi:10.1111/j.1525-1403.2011.00395.x
282. Falowski SM, Celii A, Sestokas AK, Schwartz DM, Matsumoto C, Sharan A. Awake vs. asleep placement of spinal cord stimulators: a cohort analysis of complications associated with placement. Neuromodulation. 2011;14(2):130–135. doi:10.1111/j.1525-1403.2010.00319.x
283. Hagedorn JM, Deer TR, Falowski SM, et al. An observational study of intraoperative neuromonitoring as a safety mechanism in placement of percutaneous dorsal root ganglion stimulation and spinal cord stimulation systems. J Pain Res. 2020;13:3349–3353. doi:10.2147/JPR.S289416
284. Guillemette S, Witzke S, Leier J, Hinnenthal J, Prager JP. Medical cost impact of intrathecal drug delivery for noncancer pain. Pain Med. 2013;14(4):504–515. doi:10.1111/j.1526-4637.2013.01398.x
285. Prager J, Deer T, Levy R, et al. Best practices for intrathecal drug delivery for pain. Neuromodulation. 2014;17(4):354–372. doi:10.1111/ner.12146
286. Krames ES. Intraspinal opioid therapy for chronic nonmalignant pain: current practice and clinical guidelines. J Pain Symptom Manage. 1996;11(6):333–352. doi:10.1016/0885-3924(96)
287. Tutak U, Doleys DM. Intrathecal infusion systems for treatment of chronic low back and leg pain of noncancer origin. South Med J. 1996;89(3):295–300. doi:10.1097/00007611-199603000-00007
288. Deer T, Chapple I, Classen A, et al. Intrathecal drug delivery for treatment of chronic low back pain: report from the national outcomes registry for low back pain. Pain Med. 2004;5(1):6–13. doi:10.1111/j.1526-4637.2004.04011.x
289. Deer TR, Smith HS, Cousins M, et al. Consensus guidelines for the selection and implantation of patients with noncancer pain for intrathecal drug delivery. Pain Physician. 2010;13(3):E175–213.
290. Deer TR, Abd-Elsayed A, Falowski S, et al. Practice choices in targeted intrathecal drug delivery: an online survey conducted by the polyanalgesic consensus committee. Neuromodulation. 2021;24(7):1139–1144. doi:10.1111/ner.13335
291. Dworkin RH, O’Connor AB, Kent J, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013;154(11):2249–2261. doi:10.1016/j.pain.2013.06.004
292. Manchikanti L, Abdi S, Atluri S, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013;16(2 Suppl):S49–283.
293. Deer TR, Caraway DL, Wallace MS. A definition of refractory pain to help determine suitability for device implantation. Neuromodulation. 2014;17(8):711–715. doi:10.1111/ner.12263
294. Deer TR, Prager J, Levy R, et al. Polyanalgesic Consensus Conference—2012: recommendations on Trialing for Intrathecal (Intraspinal) Drug Delivery: report of an Interdisciplinary Expert Panel. Neuromodulation. 2012;15(5):420–435. doi:10.1111/j.1525-1403.2012.00450.x
295. Deer TR, Pope JE, Hayek SM, et al. The Polyanalgesic Consensus Conference (PACC): recommendations on Intrathecal Drug Infusion Systems Best Practices and Guidelines. Neuromodulation. 2017;20(2):96–132. doi:10.1111/ner.12538
296. Pope JE. Intrathecal drug delivery indications. In: Pope JE, Deer TR, editors. Treatment of Chronic Pain Conditions: A Comprehensive Handbook.
297. Deer TR, Pope JE, Hayek SM, et al. The Polyanalgesic Consensus Conference (PACC): recommendations for Intrathecal Drug Delivery: guidance for Improving Safety and Mitigating Risks. Neuromodulation. 2017;20(2):155–176. doi:10.1111/ner.12579
298. Schultz DM, Abd-Elsayed A, Calodney A, Stromberg K, Weaver T, Spencer RJ. Targeted drug delivery for chronic nonmalignant pain: longitudinal data from the product surveillance registry. Neuromodulation. 2021;24(7):1167–1175. doi:10.1111/ner.13353
299. Capozza MA, Triarico S, Mastrangelo S, Attinà G, Maurizi P, Ruggiero A. Narrative review of intrathecal drug delivery (IDD): indications, devices and potential complications. Ann Transl Med. 2021;9(2):186. doi:10.21037/atm-20-3814
300. Pope JE, Deer TR. Intrathecal drug delivery for pain: a clinical guide and future directions. Pain Manag. 2015;5:3. doi:10.2217/pmt.15.12
301. Jain S, Malinowski M, Chopra P, Varshney V, Deer TR. Intrathecal drug delivery for pain management: recent advances and future developments. Expert Opin Drug Deliv. 2019;16(8):815–822. doi:10.1080/17425247.2019.1642870
302. Dr F, Ls S, Kl P, et al. Injury and liability associated with implantable devices for chronic pain. Anesthesiology. 2016;124:6. doi:10.1097/ALN.0000000000001122
303. Coffey RJ, Owens ML, Broste SK, et al. Mortality associated with implantation and management of intrathecal opioid drug infusion systems to treat noncancer pain. Anesthesiology. 2009;111(4):881–891. doi:10.1097/ALN.0b013e3181b64ab8
304. Coffey RJ, Owens ML, Broste SK, et al. Medical practice perspective: identification and mitigation of risk factors for mortality associated with intrathecal opioids for non-cancer pain. Pain Med. 2010;11(7):1001–1009. doi:10.1111/j.1526-4637.2010.00889.x
305. Kamran S, Wright B. Complications of intrathecal drug delivery systems. Neuromodulation. 2001;4:3. doi:10.1046/j.1525-1403.2001.00111.x
306. Hamza M, Doleys D, Wells M, et al. Prospective study of 3-year follow-up of low-dose intrathecal opioids in the management of chronic nonmalignant pain. Pain Med. 2012;13(10):1304–1313. doi:10.1111/j.1526-4637.2012.01451.x
307. Duarte RV, Raphael JH, Sparkes E, Southall JL, LeMarchand K, Ashford RL. Long-term intrathecal drug administration for chronic nonmalignant pain. J Neurosurg Anesthesiol. 2012;24(1):63–70. doi:10.1097/ANA.0b013e31822ff779
308. Kanai A. Short-term results of intrathecal injection of low-dose bupivacaine in outpatients with chronic low back and lower extremity pain. Eur Spine J. 2019;28(2). doi:10.1007/s00586-018-5801-z
309. de Lissovoy G, Brown RE, Halpern M, Hassenbusch SJ, Ross E. Cost-effectiveness of long-term intrathecal morphine therapy for pain associated with failed back surgery syndrome. Clin Ther. 1997;19(1):96–112. doi:10.1016/s0149-2918(97)80077-x
310. Rainov NG, Heidecke V, Burkert W. Long-term intrathecal infusion of drug combinations for chronic back and leg pain. J Pain Symptom Manage. 2001;22:4. doi:10.1016/s0885-3924(01)
311. Raphael JH, Southall JL, Gnanadurai TV, Treharne GJ, Kitas GD. Long-term experience with implanted intrathecal drug administration systems for failed back syndrome and chronic mechanical low back pain. BMC Musculoskelet Disord. 2002;3:17. doi:10.1186/1471-2474-3-17
312. Raphael JH, Duarte RV, Southall JL, Nightingale P, Kitas GD. Randomised, double-blind controlled trial by dose reduction of implanted intrathecal morphine delivery in chronic non-cancer pain. BMJ Open. 2013;3(7):e003061. doi:10.1136/bmjopen-2013-003061
313. Deer TR, Caraway DL, Kim CK, Dempsey CD, Stewart CD, McNeil KF. Clinical experience with intrathecal bupivacaine in combination with opioid for the treatment of chronic pain related to failed back surgery syndrome and metastatic cancer pain of the spine. Spine J. 2002;2(4):274–278. doi:10.1016/s1529-9430(02)
314. Abd-Elsayed A, Karri J, Michael A, et al. Intrathecal drug delivery for chronic pain syndromes: a review of considerations in practice management. Pain Physician. 2020;23(6):E591–E617.
315. Duse G, Davià G, White PF. Improvement in psychosocial outcomes in chronic pain patients receiving intrathecal morphine infusions. Anesth Analg. 2009;109(6):1981–1986. doi:10.1213/ANE.0b013e3181bd1da2
316. Falco FJE, Patel VB, Hayek SM, et al. Intrathecal infusion systems for long-term management of chronic non-cancer pain: an update of assessment of evidence. Pain Physician. 2013;16(2 Suppl):SE185–216.
317. Veizi IE, Hayek SM, Narouze S, Pope JE, Mekhail N. Combination of intrathecal opioids with bupivacaine attenuates opioid dose escalation in chronic noncancer pain patients. Pain Med. 2011;12(10):1481–1489. doi:10.1111/j.1526-4637.2011.01232.x
318. Roberts LJ, Finch PM, Goucke CR, Price LM. Outcome of intrathecal opioids in chronic non-cancer pain. Eur J Pain. 2001;5(4):353–361. doi:10.1053/eujp.2001.0255
319. Wallace MS, Charapata SG, Fisher R, et al. Intrathecal ziconotide in the treatment of chronic nonmalignant pain: a randomized, double-blind, placebo-controlled clinical trial. Neuromodulation. 2006;9(2):75–86. doi:10.1111/j.1525-1403.2006.00055.x
320. Wallace MS, Kosek PS, Staats P, Fisher R, Schultz DM, Leong M. Phase II, open-label, multicenter study of combined intrathecal morphine and ziconotide: addition of ziconotide in patients receiving intrathecal morphine for severe chronic pain. Pain Medicine. 2008;9(3):271–281.
321. Thimineur MA, Kravitz E, Vodapally MS. Intrathecal opioid treatment for chronic non-malignant pain: a 3-year prospective study. Pain. 2004;109(3):242–249. doi:10.1016/j.pain.2004.01.003
322. Duarte R, Raphael J, Eldabe S. Intrathecal drug delivery for the management of pain and spasticity in adults: an executive summary of the British Pain Society’s recommendations for best clinical practice. Br J Pain. 2016;10(2):67–69. doi:10.1177/2049463715587747
323. Goel V, Yang Y, Kanwar S, et al. Adverse Events and Complications Associated With Intrathecal Drug Delivery Systems: insights From the Manufacturer and User Facility Device Experience (MAUDE) Database. Neuromodulation. 2021;24(7):1181–1189. doi:10.1111/ner.13325
324. Turner JA, Sears JM, Loeser JD. Programmable intrathecal opioid delivery systems for chronic noncancer pain: a systematic review of effectiveness and complications. Clin J Pain. 2007;23(2):180–195. doi:10.1097/01.ajp.0000210955.93878.44
325. Hayek SM, Hanes MC. Intrathecal therapy for chronic pain: current trends and future needs. Curr Pain Headache Rep. 2014;18(1):388. doi:10.1007/s11916-013-0388-x
326. Deer TR, Pope JE, Hanes MC, McDowell GC. Intrathecal therapy for chronic pain: a review of morphine and ziconotide as firstline options. Pain Medicine. 2019;20(4):784–798. doi:10.1093/pm/pny132
327. Deer T, Rauck RL, Kim P, et al. Effectiveness and safety of intrathecal ziconotide: interim analysis of the patient registry of intrathecal ziconotide management (PRIZM). Pain Pract. 2018;18(2):230–238. doi:10.1111/papr.12599
328. McDowell GC, Saulino MF, Wallace M, et al. Effectiveness and safety of intrathecal ziconotide: final results of the patient registry of intrathecal ziconotide management (PRIZM). Pain Med. 2020;21(11):2925–2938. doi:10.1093/pm/pnaa115
329. Horazeck C, Huh AS, Huh BK. Acute rhabdomyolysis in a patient with long-term exposure to intrathecal ziconotide: a case report. Pain Pract. 2015;15(3):E34–39. doi:10.1111/papr.12273
330. Serrao JM, Marks RL, Morley SJ, Goodchild CS. Intrathecal midazolam for the treatment of chronic mechanical low back pain: a controlled comparison with epidural steroid in a pilot study. Pain. 1992;48(1):5–12. doi:10.1016/0304-3959(92)
331. Hayes C, Jordan MS, Hodson FJ, Ritchard L. Ceasing intrathecal therapy in chronic non-cancer pain: an invitation to shift from biomedical focus to active management. PLoS One. 2012;7(11):e49124. doi:10.1371/journal.pone.0049124
332. Brown J, Klapow J, Doleys D, Lowery D, Tutak U. Disease-specific and generic health outcomes: a model for the evaluation of long-term intrathecal opioid therapy in noncancer low back pain patients. Clin J Pain. 1999;15:2. doi:10.1097/00002508-199906000-00009
333. Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35(2):214–228. doi:10.1016/j.jpainsymman.2007.03.015
334. Patel VB, Manchikanti L, Singh V, Schultz DM, Hayek SM, Smith HS. Systematic review of intrathecal infusion systems for long-term management of chronic non-cancer pain. Pain Physician. 2009;12(2):345–360.
335. Hayek SM, Deer TR, Pope JE, Panchal SJ, Patel VB. Intrathecal therapy for cancer and non-cancer pain. Pain Physician. 2011;14(3):219–248.
336. Deckers K, De Smedt K, Mitchell B, et al. New Therapy for Refractory Chronic Mechanical Low Back Pain—Restorative Neurostimulation to Activate the Lumbar Multifidus: one Year Results of a Prospective Multicenter Clinical Trial. Neuromodulation. 2018;21(1):48–55. doi:10.1111/ner.12741
337. Cohen S, Gilmore C, Kapural L, et al. Percutaneous peripheral nerve stimulation for pain reduction and improvements in functional outcomes in chronic low back pain. Mil Med. 2019;184(Suppl 1):537–541. doi:10.1093/milmed/usy310
338. Ilfeld BM, Gabriel RA, Saulino MF, et al. Infection Rates of Electrical Leads Used for Percutaneous Neurostimulation of the Peripheral Nervous System. Pain Pract. 2017;17(6):753–762. doi:10.1111/papr.12523
339. Gilligan C, Volschenk W, Russo M, et al. An implantable restorative-neurostimulator for refractory mechanical chronic low back pain: a randomized sham-controlled clinical trial. Pain. 2021;162(10):2486–2498. doi:10.1097/j.pain.0000000000002258
340. Gilligan C, Volschenk W, Russo M, et al. Long-term outcomes of restorative neurostimulation in patients with refractory chronic low back pain secondary to multifidus dysfunction: two-year results of the reactiv8-b pivotal trial. Neuromodulation. 2021;S1094-7159(21):5418. doi:10.1016/j.neurom.2021.10.011
341. Kapural L, Gilmore CA, Chae J, et al. Percutaneous peripheral nerve stimulation for the treatment of chronic low back pain: two clinical case reports of sustained pain relief. Pain Pract. 2018;18(1):94–103. doi:10.1111/papr.12571
342. Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous Peripheral Nerve Stimulation (PNS) for the Treatment of Chronic Low Back Pain Provides Sustained Relief. Neuromodulation. 2019;22(5):615–620. doi:10.1111/ner.12854
343. Lin T, Gargya A, Singh H, Sivanesan E, Gulati A. Mechanism of peripheral nerve stimulation in chronic pain. Pain Med. 2020;21(Suppl 1):S6–S12. doi:10.1093/pm/pnaa164
344. D’Mello R, Dickenson AH. Spinal cord mechanisms of pain. Br J Anaesth. 2008;101(1):8–16. doi:10.1093/bja/aen088
345. Abejón D, Pérez-Cajaraville J. Peripheral nerve stimulation: definition. Prog Neurol Surg. 2011;24:203–209. doi:10.1159/000323052
346. Verrills P, Russo M, Peripheral nerve stimulation for back pain. Stimulation Nervous System. 2016;29:127–138.
347. Winkelmueller M, Kolodziej MA, Welke W, Koulousakis A, Martinez R. Subcutaneous peripheral nerve field stimulation for the treatment of chronic back pain: patient selection and technical aspects. J Neurol Surg a Cent Eur Neurosurg. 2016;77(1):63–67. doi:10.1055/s-0035-1547362
348. Knotkova H, Rasche D, eds. Textbook of Neuromodulation: Principles, Methods and Clinical Applications.
349. Corriveau M, Lake W, Hanna A. Nerve Stimulation for Pain. Neurosurg Clin N Am. 2019;30(2):257–264. doi:10.1016/j.nec.2018.12.008
350. Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–258. doi:10.1001/archinternmed.2008.543
351. Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106(3):591–614. doi:10.1097/00000542-200703000-00024
352. Cosman ER. A comment on the history of the pulsed radiofrequency technique for pain therapy. Anesthesiology. 2005;103(6):1312. doi:10.1097/00000542-200512000-00028
353. Sluijter ME, van Kleef M. Characteristics and mode of action of radiofrequency lesions. Curr Rev Pain. 1998;2(3):143–150. doi:10.1007/s11916-998-0011-8
354. Pangarkar S, Miedema ML. Pulsed versus conventional radio frequency ablation for lumbar facet joint dysfunction. Curr Phys Med Rehabil Rep. 2014;2(1):61–65. doi:10.1007/s40141-013-0040-z
355. Ball RD. The science of conventional and water-cooled monopolar lumbar radiofrequency rhizotomy: an electrical engineering point of view. Pain Physician. 2014;17(2):E175–211.
356. Kornick C, Kramarich SS, Lamer TJ, Todd Sitzman B. Complications of lumbar facet radiofrequency denervation. Spine. 2004;29(12):1352–1354. doi:10.1097/01.brs.0000128263.67291.a0
357. Lamer TJ, Smith J, Hoelzer BC, Mauck WD, Qu W, Gazelka HM. Safety of lumbar spine radiofrequency procedures in patients who have posterior spinal hardware. Pain Medicine. 2016;17(9):1634–1637. doi:10.1093/pm/pnv078
358. King W, Ahmed SU, Baisden J, et al. Diagnosis and treatment of posterior sacroiliac complex pain: a systematic review with comprehensive analysis of the published data. Pain Med. 2015;16(2):257–265. doi:10.1111/pme.12630
359. Laslett M, Aprill CN, McDonald B. Provocation sacroiliac joint tests have validity in the diagnosis of sacroiliac joint pain. Arch Phys Med Rehabil. 2006;87(6):874. doi:10.1016/j.apmr.2006.04.007
360. Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335(23):1721–1726. doi:10.1056/NEJM199612053352302
361. Govind J, King W, Bailey B, Bogduk N. Radiofrequency neurotomy for the treatment of third occipital headache. J Neurol Neurosurg Psychiatry. 2003;74(1):88–93.
362. MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Cervical medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2012;13(5):647–654. doi:10.1111/j.1526-4637.2012.01351.x
363. Cohen SP, Hurley RW, Buckenmaier CC, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109(2):279–288. doi:10.1097/ALN.0b013e31817f4c7c
364. Patel N, Gross A, Brown L, Gekht G. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain. Pain Med. 2012;13(3):383–398. doi:10.1111/j.1526-4637.2012.01328.x
365. Patel N. Twelve-month follow-up of a randomized trial assessing cooled radiofrequency denervation as a treatment for sacroiliac region pain. Pain Pract. 2016;16(2):154–167. doi:10.1111/papr.12269
366. Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995;20(17):1878–1883. doi:10.1097/00007632-199509000-00007
367. Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54(2):100–106. doi:10.1136/ard.54.2.100
368. van Tilburg CWJ, Schuurmans FA, Stronks DL, Groeneweg JG, Huygen FJPM. Randomized sham-controlled double-blind multicenter clinical trial to ascertain the effect of percutaneous radiofrequency treatment for sacroiliac joint pain: three-month results. Clin J Pain. 2016;32(11):921–926. doi:10.1097/AJP.0000000000000351
369. Shayota B, Wong TL, Fru D, et al. A comprehensive review of the sinuvertebral nerve with clinical applications. Anat Cell Biol. 2019;52(2):128–133. doi:10.5115/acb.2019.52.2.128
370. Kim HS, Wu PH, Jang IT. Lumbar Degenerative Disease Part 1: anatomy and Pathophysiology of Intervertebral Discogenic Pain and Radiofrequency Ablation of Basivertebral and Sinuvertebral Nerve Treatment for Chronic Discogenic Back Pain: a Prospective Case Series and Review of Literature. Int J Mol Sci. 2020;21:4. doi:10.3390/ijms21041483
371. Tzika M, Paraskevas GK, Piagkou M, Papatolios AK, Natsis K. Basivertebral foramina of true vertebrae: morphometry, topography and clinical considerations. Surg Radiol Anat. 2021;43(6):889–907. doi:10.1007/s00276-021-02690-0
372. Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15(9):1312–1319. doi:10.1007/s00586-006-0185-x
373. Lotz JC, Fields AJ, Liebenberg EC. The role of the vertebral end plate in low back pain. Global Spine J. 2013;3(3):153–164. doi:10.1055/s-0033-1347298
374. Fras C, Kravetz P, Mody DR, Heggeness MH. Substance P-containing nerves within the human vertebral body. an immunohistochemical study of the basivertebral nerve. Spine J. 2003;3(1):63–67. doi:10.1016/s1529-9430(02)00455-2
375. Bailey JF, Liebenberg E, Degmetich S, Lotz JC. Innervation patterns of PGP 9.5-positive nerve fibers within the human lumbar vertebra. J Anat. 2011;218(3):263–270. doi:10.1111/j.1469-7580.2010.01332.x
376. DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011;12(2):224–233. doi:10.1111/j.1526-4637.2010.01045.x
377. Jensen RK, Leboeuf-Yde C. Is the presence of Modic changes associated with the outcomes of different treatments? A systematic critical review. BMC Musculoskelet Disord. 2011;12(1):183. doi:10.1186/1471-2474-12-183
378. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–199. doi:10.1148/radiology.166.1.3336678
379. Weishaupt D, Zanetti M, Hodler J, et al. Painful lumbar disk derangement: relevance of endplate abnormalities at MR Imaging. Radiology. 2001;218(2):420–427. doi:10.1148/radiology.218.2.r01fe15420
380. Kuisma M, Karppinen J, Niinimäki J, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine. 2007;32(10):1116–1122. doi:10.1097/01.brs.0000261561.12944.ff
381. Mok FPS, Samartzis D, Karppinen J, Fong DYT, Luk KDK, Cheung KMC. Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. Spine J. 2016;16(1):32–41. doi:10.1016/j.spinee.2015.09.060
382. Applebaum A, Nessim A, Cho W. Modic change: an emerging complication in the aging population. Clin Spine Surg. 2021. doi:10.1097/BSD.0000000000001168
383. Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes, possible causes and relation to low back pain. Med Hypotheses. 2008;70(2):361–368. doi:10.1016/j.mehy.2007.05.014
384. Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17(11):1407–1422. doi:10.1007/s00586-008-0770-2
385. Jensen TS, Bendix T, Sorensen JS, Manniche C, Korsholm L, Kjaer P. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet Disord. 2009;10(1):81. doi:10.1186/1471-2474-10-81
386. Järvinen J, Karppinen J, Niinimäki J, et al. Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC Musculoskelet Disord. 2015;16:98. doi:10.1186/s12891-015-0540-3
387. Herlin C, Kjaer P, Espeland A, et al. Modic changes-Their associations with low back pain and activity limitation: a systematic literature review and meta-analysis. PLoS One. 2018;13(8):e0200677. doi:10.1371/journal.pone.0200677
388. Mera Y, Teraguchi M, Hashizume H, et al. Association between types of Modic changes in the lumbar region and low back pain in a large cohort: the Wakayama spine study. Eur Spine J. 2021;30(4):1011–1017. doi:10.1007/s00586-020-06618-x
389. Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Manniche C. Rest versus exercise as treatment for patients with low back pain and Modic changes. A randomized controlled clinical trial. BMC Med. 2012;10:22. doi:10.1186/1741-7015-10-22
390. Tieppo FV, Sherwood D, Twohey E. Developments in minimally invasive surgical options for vertebral pain: basivertebral nerve ablation – a narrative review and current evidence. J Pain Res. 2022;1:548.
391. Becker S, Hadjipavlou A, Heggeness MH. Ablation of the basivertebral nerve for treatment of back pain: a clinical study. Spine J. 2017;17(2):218–223. doi:10.1016/j.spinee.2016.08.032
392. Kim HS, Adsul N, Yudoyono F, et al. Transforaminal epiduroscopic basivertebral nerve laser ablation for chronic low back pain associated with Modic changes: a Preliminary Open-Label Study. Pain Res Manag. 2018;2018. doi:10.1155/2018/6857983
393. Urits I, Noor N, Johal AS, et al. Basivertebral nerve ablation for the treatment of vertebrogenic pain. Pain Ther. 2021;10(1):39–53. doi:10.1007/s40122-020-00211-2
394. Nguyen KML, Nguyen DTD. Minimally invasive treatment for degenerative lumbar spine. Tech Vasc Interv Radiol. 2020;23(4):100700. doi:10.1016/j.tvir.2020.100700
395. Macadaeg K, Truumees E, Boody B, et al. A prospective, single arm study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. North Am Spine Soc J. 2020;3:100030. doi:10.1016/j.xnsj.2020.100030
396. Conger A, Schuster NM, Cheng DS, et al. The effectiveness of intraosseous basivertebral nerve radiofrequency neurotomy for the treatment of chronic low back pain in patients with Modic changes: a systematic review. Pain Med. 2021;22(5):1039–1054. doi:10.1093/pm/pnab040
397. Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2018;27(5):1146–1156. doi:10.1007/s00586-018-5496-1
398. Truumees E, Macadaeg K, Pena E, et al. A prospective, open-label, single-arm, multi-center study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. Eur Spine J. 2019;28(7):1594–1602. doi:10.1007/s00586-019-05995-2
399. Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: 2-Year Results From a Prospective Randomized Double-Blind Sham-Controlled Multicenter Study. Int J Spine Surg. 2019;13(2):110–119. doi:10.14444/6015
400. Khalil JG, Smuck M, Koreckij T, et al. A prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. Spine J. 2019;19(10):1620–1632. doi:10.1016/j.spinee.2019.05.598
401. Markman JD, Rhyne AL, Sasso RC, et al. Association between opioid use and patient-reported outcomes in a randomized trial evaluating basivertebral nerve ablation for the relief of chronic low back pain. Neurosurgery. 2020;86(3):343–347. doi:10.1093/neuros/nyz093
402. Fischgrund JS, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925–1934. doi:10.1007/s00586-020-06448-x
403. De Vivo AE, D’Agostino G, D’Anna G, et al. Intra-osseous basivertebral nerve radiofrequency ablation (BVA) for the treatment of vertebrogenic chronic low back pain. Neuroradiology. 2021;63(5):809–815. doi:10.1007/s00234-020-02577-8
404. Tieppo Francio V, Gill B, Rupp A, Sack A, Sayed D. Interventional procedures for vertebral diseases: spinal tumor ablation, vertebral augmentation, and basivertebral nerve ablation-a scoping review. Healthcare. 2021;9(11):1554. doi:10.3390/healthcare9111554
405. Tieppo Francio V, Sherwood D, Twohey E, et al. Developments in minimally invasive surgical options for vertebral pain: basivertebral nerve ablation - a narrative review. J Pain Res. 2021;14:1887–1907. doi:10.2147/JPR.S287275
406. Tieppo Francio V, Sayed D. Basivertebral Nerve Ablation. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK572127/.
407. Michalik A, Conger A, Smuck M, Maus TP, McCormick ZL. Intraosseous basivertebral nerve radiofrequency ablation for the treatment of vertebral body endplate low back pain: current evidence and future directions. Pain Med. 2021;22(Suppl 1):S24–S30. doi:10.1093/pm/pnab117
408. Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13(4):343–355.
409. Gharibo CG, Varlotta GP, Rhame EE, Liu ECJ, Bendo JA, Perloff MD. Interlaminar versus transforaminal epidural steroids for the treatment of subacute lumbar radicular pain: a randomized, blinded, prospective outcome study. Pain Physician. 2011;14(6):499–511.
410. Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine. 2005;30(8):857–862. doi:10.1097/01.brs.0000158878.93445.a0
411. Manchikanti L, Cash KA, Pampati V, Falco FJE. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Physician. 2014;17(4):E489–501.
412. Iversen T, Solberg TK, Romner B, et al. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi:10.1136/bmj.d5278
413. Nandi J, Chowdhery A. A randomized controlled clinical trial to determine the effectiveness of caudal epidural steroid injection in lumbosacral sciatica. J Clin Diagn Res. 2017;11(2):RC04–RC08. doi:10.7860/JCDR/2017/21905.9392
414. Cohen SB, Cheng TT, Chindalore V, et al. Evaluation of the efficacy and safety of pamapimod, a p38 MAP kinase inhibitor, in a double-blind, methotrexate-controlled study of patients with active rheumatoid arthritis. Arthritis Rheum. 2009;60(2):335–344. doi:10.1002/art.24266
415. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002;27(1):11–16. doi:10.1097/00007632-200201010-00005
416. Buchner M, Zeifang F, Brocai DR, Schiltenwolf M. Epidural corticosteroid injection in the conservative management of sciatica. Clin Orthop Relat Res. 2000;1(375):149–156. doi:10.1097/00003086-200006000-00018
417. Roldan CJ, Osuagwu U, Cardenas-Turanzas M, Huh BK. Normal saline trigger point injections vs conventional active drug mix for myofascial pain syndromes. Am J Emerg Med. 2020;38(2):311–316. doi:10.1016/j.ajem.2019.158410
418. Sakalys D, Rokicki JP, Januzis G, Kubilius R. Plasma rich in growth factors injection effectiveness for myofascial pain treatment in masticatory muscles. Randomised controlled trial. J Oral Rehabil. 2020;47(7):796–801. doi:10.1111/joor.12973
419. Moon YE, Kim SH, Seok H, Lee SY. Efficacy of topical vibratory stimulation for reducing pain during trigger point injection to the gastrocnemius: a randomized controlled trial. Arch Phys Med Rehabil. 2019;100(9):1607–1613. doi:10.1016/j.apmr.2019.02.010
420. Dessie SG, Von Bargen E, Hacker MR, Haviland MJ, Elkadry E. A randomized, double-blind, placebo-controlled trial of onabotulinumtoxin A trigger point injections for myofascial pelvic pain. Am J Obstet Gynecol. 2019;221(5):
421. Ata E, Kösem M, Adiguzel E. Does kinesiotaping increase the efficacy of lidocaine injection in myofascial pain syndrome treatment? A randomized controlled study. J Back Musculoskelet Rehabil. 2019;32(3):471–477. doi:10.3233/BMR-171035
422. Pecos-Martín D, Montañez-Aguilera FJ, Gallego-Izquierdo T, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(5):775–781. doi:10.1016/j.apmr.2014.12.016
423. Kwanchuay P, Petchnumsin T, Yiemsiri P, Pasuk N, Srikanok W, Hathaiareerug C. Efficacy and Safety of Single Botulinum Toxin Type A (Botox®) Injection for Relief of Upper Trapezius Myofascial Trigger Point: a Randomized, Double-Blind, Placebo-Controlled Study. J Med Assoc Thai. 2015;98(12):1231–1236.
424. Choi YH, Jung SJ, Lee CH, Lee SU. Additional effects of transcranial direct-current stimulation and trigger-point injection for treatment of myofascial pain syndrome: a pilot study with randomized, single-blinded trial. J Altern Complement Med. 2014;20(9):698–704. doi:10.1089/acm.2013.0243
425. Seo HG, Bang MS, Chung SG, Jung SH, Lee SU. Effect of electrical stimulation on botulinum toxin a therapy in patients with chronic myofascial pain syndrome: a 16-week randomized double-blinded study. Arch Phys Med Rehabil. 2013;94(3):412–418. doi:10.1016/j.apmr.2012.09.034
426. Yoon SH, Rah UW, Sheen SS, Cho KH. Comparison of 3 needle sizes for trigger point injection in myofascial pain syndrome of upper- and middle-trapezius muscle: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(8):1332–1339. doi:10.1016/j.apmr.2009.01.028
427. Ga H, Choi JH, Park CH, Yoon HJ. Acupuncture needling versus lidocaine injection of trigger points in myofascial pain syndrome in elderly patients--a randomised trial. Acupunct Med. 2007;25(4):130–136. doi:10.1136/aim.25.4.130
428. Zaralidou AT, Amaniti EN, Maidatsi PG, Gorgias NK, Vasilakos DF. Comparison between newer local anesthetics for myofascial pain syndrome management. Methods Find Exp Clin Pharmacol. 2007;29(5):353–357. doi:10.1358/mf.2007.29.5.1075364
429. Qerama E, Fuglsang-Frederiksen A, Kasch H, Bach FW, Jensen TS. A double-blind, controlled study of botulinum toxin A in chronic myofascial pain. Neurology. 2006;67(2):241–245. doi:10.1212/01.wnl.0000224731.06168.df
430. Göbel H, Heinze A, Reichel G, Hefter H, Benecke R. Dysport myofascial pain study group. Efficacy and safety of a single botulinum type A toxin complex treatment (Dysport) for the relief of upper back myofascial pain syndrome: results from a randomized double-blind placebo-controlled multicentre study. Pain. 2006;125(1–2):82–88. doi:10.1016/j.pain.2006.05.001
431. Kamanli A, Kaya A, Ardicoglu O, Ozgocmen S, Zengin FO, Bayik Y. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25(8):604–611. doi:10.1007/s00296-004-0485-6
432. Iwama H, Ohmori S, Kaneko T, Watanabe K. Water-diluted local anesthetic for trigger-point injection in chronic myofascial pain syndrome: evaluation of types of local anesthetic and concentrations in water. Reg Anesth Pain Med. 2001;26(4):333–336. doi:10.1053/rapm.2001.24672
433. Iwama H, Akama Y. The superiority of water-diluted 0.25% to neat 1% lidocaine for trigger-point injections in myofascial pain syndrome: a prospective, randomized, double-blinded trial. Anesth Analg. 2000;91(2):408–409. doi:10.1097/00000539-200008000-00033
434. Krishnan SK, Benzon HT, Siddiqui T, Canlas B. Pain on intramuscular injection of bupivacaine, ropivacaine, with and without dexamethasone. Reg Anesth Pain Med. 2000;25(6):615–619. doi:10.1053/rapm.2000.8933
435. Wheeler AH, Goolkasian P, Gretz SS. A randomized, double-blind, prospective pilot study of botulinum toxin injection for refractory, unilateral, cervicothoracic, paraspinal, myofascial pain syndrome. Spine. 1998;23(15):1662–1666. doi:10.1097/00007632-199808010-00009
436. Tschopp KP, Gysin C. Local injection therapy in 107 patients with myofascial pain syndrome of the head and neck. ORL J Otorhinolaryngol Relat Spec. 1996;58(6):306–310. doi:10.1159/000276860
437. Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73(4):256–263. doi:10.1097/00002060-199407000-00006
438. Garvey TA, Marks MR, Wiesel SW. A prospective, randomized, double-blind evaluation of trigger-point injection therapy for low-back pain. Spine. 1989;14(9):962–964. doi:10.1097/00007632-198909000-00008
439. Hameroff SR, Crago BR, Blitt CD, Womble J, Kanel J. Comparison of bupivacaine, etidocaine, and saline for trigger-point therapy. Anesth Analg. 1981;60(10):752–755.
440. Kocak AO, Ahiskalioglu A, Sengun E, Gur STA, Akbas I. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: a prospective randomized study. Am J Emerg Med. 2019;37(10):1927–1931. doi:10.1016/j.ajem.2019.01.015
441. Snidvongs S, Taylor RS, Ahmad A, et al. Facet-joint injections for non-specific low back pain: a feasibility RCT. Health Technol Assess. 2017;21(74):1–130. doi:10.3310/hta21740
442. Karkucak M, Batmaz İ, Kerimoglu S, Ayar A. Comparison of clinical outcomes of ultrasonography-guided and blind local injections in facet syndrome: a 6-week randomized controlled trial. J Back Musculoskelet Rehabil. 2020;33(3):431–436. doi:10.3233/BMR-181447
443. Ye L, Wen C, Liu H. Ultrasound-guided versus low dose computed tomography scanning guidance for lumbar facet joint injections: same accuracy and efficiency. BMC Anesthesiol. 2018;18. doi:10.1186/s12871-018-0620-7
444. Ellard DR, Underwood M, Achana F, et al. Facet joint injections for people with persistent non-specific low back pain (Facet Injection Study): a feasibility study for a randomised controlled trial. Health Technol Assess. 2017;21(30):1–184. doi:10.3310/hta21300
445. Do KH, Ahn SH, Cho YW, Chang MC. Comparison of intra-articular lumbar facet joint pulsed radiofrequency and intra-articular lumbar facet joint corticosteroid injection for management of lumbar facet joint pain: a randomized controlled trial. Medicine. 2017;96(13):e6524. doi:10.1097/MD.0000000000006524
446. Miller MR, Mathews RS, Reeves KD. Treatment of painful advanced internal lumbar disc derangement with intradiscal injection of hypertonic dextrose. Pain Physician. 2006;9(2):115–121.
447. Akeda K, Ohishi K, Masuda K, et al. Intradiscal injection of autologous platelet-rich plasma releasate to treat discogenic low back pain: a preliminary clinical trial. Asian Spine J. 2017;11(3):380–389. doi:10.4184/asj.2017.11.3.380
448. Levi D, Horn S, Tyszko S, Levin J, Hecht-Leavitt C, Walko E. Intradiscal platelet-rich plasma injection for chronic discogenic low back pain: preliminary results from a prospective trial. Pain Med. 2016;17(6):1010–1022. doi:10.1093/pm/pnv053
449. Jain D, Goyal T, Verma N, Paswan AK, Dubey RK. Intradiscal platelet-rich plasma injection for discogenic low back pain and correlation with platelet concentration: a prospective clinical trial. Pain Med. 2020;21(11):2719–2725. doi:10.1093/pm/pnaa254
450. Navani A, Ambach MA, Navani R, Wei J. Biologics for lumbar discogenic pain: 18 month follow-up forsafety and efficacy. PMCR. 2018;111–118. doi:10.36076/pmcr.2018/2/111
451. Orozco L, Soler R, Morera C, Alberca M, Sánchez A, García-Sancho J. Intervertebral disc repair by autologous mesenchymal bone marrow cells: a pilot study. Transplantation. 2011;92(7):822–828. doi:10.1097/TP.0b013e3182298a15
452. Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016;14:253. doi:10.1186/s12967-016-1015-5
453. Pettine KA, Suzuki RK, Sand TT, Murphy MB. Autologous bone marrow concentrate intradiscal injection for the treatment of degenerative disc disease with three-year follow-up. Int Orthop. 2017;41(10):2097–2103. doi:10.1007/s00264-017-3560-9
454. Centeno C, Markle J, Dodson E, et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017;15(1):197. doi:10.1186/s12967-017-1300-y
455. Noriega DC, Ardura F, Hernández-Ramajo R, et al. Intervertebral disc repair by allogeneic mesenchymal bone marrow cells: a randomized controlled trial. Transplantation. 2017;101(8):1945–1951. doi:10.1097/TP.0000000000001484
456. Bae HW, Amirdelfan K, Coric D, et al. A Phase II study demonstrating efficacy and safety of mesenchymal precursor cells in low back pain due to disc degeneration. Spine J. 2014;14(11):S31–S32. doi:10.1016/j.spinee.2014.08.084
457. Kumar H, Ha DH, Lee EJ, et al. Safety and tolerability of intradiscal implantation of combined autologous adipose-derived mesenchymal stem cells and hyaluronic acid in patients with chronic discogenic low back pain: 1-year follow-up of a phase I study. Stem Cell Res Ther. 2017;8(1):262. doi:10.1186/s13287-017-0710-3
458. Comella K, Silbert R, Parlo M. Effects of the intradiscal implantation of stromal vascular fraction plus platelet rich plasma in patients with degenerative disc disease. J Transl Med. 2017;15. doi:10.1186/s12967-016-1109-0
459. Wolff M, Shillington JM, Rathbone C, Piasecki SK, Barnes B. Injections of concentrated bone marrow aspirate as treatment for Discogenic pain: a retrospective analysis. BMC Musculoskelet Disord. 2020;21(1):135. doi:10.1186/s12891-020-3126-7
460. Amirdelfan K, Bae H, McJunkin T, et al. Allogeneic mesenchymal precursor cells treatment for chronic low back pain associated with degenerative disc disease: a prospective randomized, placebo-controlled 36-month study of safety and efficacy. Spine J. 2021;21(2):212–230. doi:10.1016/j.spinee.2020.10.004
461. Haufe SMW, Mork AR. Intradiscal injection of hematopoietic stem cells in an attempt to rejuvenate the intervertebral discs. Stem Cells Dev. 2006;15(1):136–137. doi:10.1089/scd.2006.15.136
462. Irwin RW, Watson T, Minick RP, Ambrosius WT. Age, body mass index, and gender differences in sacroiliac joint pathology. Am J Phys Med Rehabil. 2007;86(1):37–44. doi:10.1097/phm.0b013e31802b8554
463. Hawkins J, Schofferman J. Serial therapeutic sacroiliac joint injections: a practice audit. Pain Medicine. 2009;10(5):850–853. doi:10.1111/j.1526-4637.2009.00651.x
464. Borowsky CD, Fagen G. Sources of sacroiliac region pain: insights gained from a study comparing standard intra-articular injection with a technique combining intra- and peri-articular injection. Arch Phys Med Rehabil. 2008;89(11):2048–2056. doi:10.1016/j.apmr.2008.06.006
465. Maugars Y, Mathis C, Vilon P, Prost A. Corticosteroid injection of the sacroiliac joint in patients with seronegative spondylarthropathy. Arthritis Rheum. 1992;35(5):564–568. doi:10.1002/art.1780350512
466. Visser LH, Woudenberg NP, de Bont J, et al. Treatment of the sacroiliac joint in patients with leg pain: a randomized-controlled trial. Eur Spine J. 2013;22(10):2310–2317. doi:10.1007/s00586-013-2833-2
467. Basu S. Mild procedure: single-site prospective IRB study. Clin J Pain. 2012;28(3):254–258. doi:10.1097/AJP.0b013e31822bb344
468. Deer TR, Kim CK, Bowman RG, Ranson MT, Yee BS. Study of percutaneous lumbar decompression and treatment algorithm for patients suffering from neurogenic claudication. Pain Physician. 2012;15(6):451–460.
469. Brown LL. A double-blind, randomized, prospective study of epidural steroid injection vs. the mild® procedure in patients with symptomatic lumbar spinal stenosis. Pain Pract. 2012;12(5):333–341. doi:10.1111/j.1533-2500.2011.00518.x
470. Staats PS, Chafin TB, Golovac S, et al. Long-Term Safety and Efficacy of Minimally Invasive Lumbar Decompression Procedure for the Treatment of Lumbar Spinal Stenosis With Neurogenic Claudication: 2-Year Results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43(7):789–794. doi:10.1097/AAP.0000000000000868
471. Nunley PD, Deer TR, Benyamin RM, Staats PS, Block JE. Interspinous process decompression is associated with a reduction in opioid analgesia in patients with lumbar spinal stenosis. J Pain Res. 2018;11:2943–2948. doi:10.2147/JPR.S182322
472. Nunley PD, Patel VV, Orndorff DG, Lavelle WF, Block JE, Geisler FH. Interspinous process decompression improves quality of life in patients with lumbar spinal stenosis. Minim Invasive Surg. 2018;2018:1035954. doi:10.1155/2018/1035954
473. Nunley PD, Patel VV, Orndorff DG, Lavelle WF, Block JE, Geisler FH. Five-year durability of stand-alone interspinous process decompression for lumbar spinal stenosis. Clin Interv Aging. 2017;12:1409–1417. doi:10.2147/CIA.S143503
474. Bini W, Miller LE, Block JE. Minimally invasive treatment of moderate lumbar spinal stenosis with the superion interspinous spacer. Open Orthop J. 2011;5:361–367. doi:10.2174/1874325001105010361
475. Shabat S, Miller LE, Block JE, Gepstein R. Minimally invasive treatment of lumbar spinal stenosis with a novel interspinous spacer. Clin Interv Aging. 2011;6:227–233. doi:10.2147/CIA.S23656
476. Arts MP, Brand R, van den Akker ME, et al. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. 2011;69(1):135–144. doi:10.1227/NEU.0b013e318214a98c
477. Endres S, Ludwig E. Outcome of distraction interference arthrodesis of the sacroiliac joint for sacroiliac arthritis. Indian J Orthop. 2013;47(5):437–442. doi:10.4103/0019-5413.118197
478. Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech. 2008;21(8):579–584. doi:10.1097/BSD.0b013e31815ecc4b
479. Patterson D, Wilits M, Fiks V. Pain Reduction and Functional Improvement After Posterior Approach SI Stabilization and Fusion with Specialized Graft: A Case Series. CASIPP Annual Meeting; 2018.
480. Mann D, Wilits M, Fiks V. Pain Reduction at 12 Months After Posterior Approach SI Stabilization and Fusion with Specialized Graft: 10 Case Series. ASPN Annual Meeting; 2019.
481. Pyles S, Ortiz A, Lam C, Kim D, Sayed D. LINQ SI Fusion for Pain Relief in SCS Patient: A Case Series. NANS Annual Meeting; 2020.
482. Pyles S. LINQ Fusion: 20 Patient Case Series. FSIPP Annual Meeting; 2019.
483. Kim DH, Lee MS, Lee S, et al. Comparison of the efficacy of ultrasound- vs fluoroscopy-guided genicular nerve block for chronic knee osteoarthritis. Pain Physician. 2019;22(2):139–146.
484. Lam CM, Pyles S, Balter K, Sayed D. Multicenter Outcomes in Minimally Invasive Sacroiliac Fusion. ASIPP Annual Meeting; 2020.
485. Darr E, Meyer SC, Whang PG, et al. Long-term prospective outcomes after minimally invasive trans-iliac sacroiliac joint fusion using triangular titanium implants. Med Devices. 2018;11:113–121. doi:10.2147/MDER.S160989
486. Al-Khayer A, Hegarty J, Hahn D, Grevitt MP. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech. 2008;21(5):359–363. doi:10.1097/BSD.0b013e318145ab96
487. Khurana A, Guha AR, Mohanty K, Ahuja S. Percutaneous fusion of the sacroiliac joint with hollow modular Anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br. 2009;91(5):627–631. doi:10.1302/0301-620X.91B5.21519
488. Patel V, Kovalsky D, Meyer SC, et al. Prospective trial of sacroiliac joint fusion using 3d-printed triangular titanium implants. Med Devices. 2020;13:173–182. doi:10.2147/MDER.S253741
489. Wang C, Zhang Y, Chen W, Yan SL, Guo KJ, Feng S. Comparison of percutaneous curved kyphoplasty and bilateral percutaneous kyphoplasty in osteoporotic vertebral compression fractures: a randomized controlled trial. BMC Musculoskelet Disord. 2021;22(1):588. doi:10.1186/s12891-021-04469-1
490. Noriega D, Marcia S, Theumann N, et al. A prospective, international, randomized, noninferiority study comparing an titanium implantable vertebral augmentation device versus balloon kyphoplasty in the reduction of vertebral compression fractures (SAKOS study). Spine J. 2020;20(12):2039–2040. doi:10.1016/j.spinee.2020.08.021
491. Liu Q, Cao J, Kong J. Effects of Percutaneous kyphoplasty on bone metabolism and oxidative stress in elderly patients with osteoporotic spinal fractures. J Coll Physicians Surg Pak. 2019;29(1):37–40. doi:10.29271/jcpsp.2019.01.37
492. Liu Q, Cao J, Kong JJ. Clinical effect of balloon kyphoplasty in elderly patients with multiple osteoporotic vertebral fracture. Niger J Clin Pract. 2019;22(3):289–292. doi:10.4103/njcp.njcp_8_18
493. Firanescu CE. Vertebroplasty versus sham procedure for painful acute osteoporotic vertebral compression fractures (VERTOS IV): randomised sham controlled clinical trial. BMJ. 2018;361:k1551. doi:10.1136/bmj.k1551
494. Hansen EJ, Simony A, Rousing R, Carreon LY, Tropp H, Andersen MØ. Double Blind Placebo-controlled Trial of Percutaneous Vertebroplasty (VOPE). Global Spine J. 2016;6(1_suppl):1582763. doi:10.1055/s-0036-1582763
495. Leali PT, Solla F, Maestretti G, Balsano M, Doria C. Safety and efficacy of vertebroplasty in the treatment of osteoporotic vertebral compression fractures: a prospective multicenter international randomized controlled study. Clin Cases Miner Bone Metab. 2016;13(3):234–236. doi:10.11138/ccmbm/2016.13.3.234
496. Wang B, Guo H, Yuan L, Huang D, Zhang H, Hao D. A prospective randomized controlled study comparing the pain relief in patients with osteoporotic vertebral compression fractures with the use of vertebroplasty or facet blocking. Eur Spine J. 2016;25(11):3486–3494. doi:10.1007/s00586-016-4425-4
497. Yang EZ, Xu JG, Huang GZ, et al. Percutaneous Vertebroplasty Versus Conservative Treatment in Aged Patients With Acute Osteoporotic Vertebral Compression Fractures: a Prospective Randomized Controlled Clinical Study. Spine. 2016;41(8):653–660. doi:10.1097/BRS.0000000000001298
498. Hartmann F, Griese M, Dietz SO, Kuhn S, Rommens PM, Gercek E. Two-year results of vertebral body stenting for the treatment of traumatic incomplete burst fractures. Minim Invasive Ther Allied Technol. 2015;24(3):161–166. doi:10.3109/13645706.2014.962546
499. Tutton SM, Pflugmacher R, Davidian M, Beall DP, Facchini FR, Garfin SR. KAST Study: the Kiva System As a Vertebral Augmentation Treatment-A Safety and Effectiveness Trial: a Randomized, Noninferiority Trial Comparing the Kiva System With Balloon Kyphoplasty in Treatment of Osteoporotic Vertebral Compression Fractures. Spine. 2015;40(12):865–875. doi:10.1097/BRS.0000000000000906
500. Chen D, An ZQ, Song S, Tang JF, Qin H. Percutaneous vertebroplasty compared with conservative treatment in patients with chronic painful osteoporotic spinal fractures. J Clin Neurosci. 2014;21(3):473–477. doi:10.1016/j.jocn.2013.05.017
501. Diel P, Röder C, Perler G, et al. Radiographic and safety details of vertebral body stenting: results from a multicenter chart review. BMC Musculoskelet Disord. 2013;14:233. doi:10.1186/1471-2474-14-233
502. Korovessis P, Vardakastanis K, Repantis T, Vitsas V. Balloon kyphoplasty versus KIVA vertebral augmentation--comparison of 2 techniques for osteoporotic vertebral body fractures: a prospective randomized study. Spine. 2013;38(4):292–299. doi:10.1097/BRS.0b013e31826b3aef
503. Otten LA, Bornemnn R, Jansen TR, et al. Comparison of balloon kyphoplasty with the new Kiva® VCF system for the treatment of vertebral compression fractures. Pain Physician. 2013;16(5):E505–512.
504. Werner CML, Osterhoff G, Schlickeiser J, et al. Vertebral body stenting versus kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a randomized trial. J Bone Joint Surg Am. 2013;95(7):577–584. doi:10.2106/JBJS.L.00024
505. Blasco J, Martinez-Ferrer A, Macho J, et al. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res. 2012;27(5):1159–1166. doi:10.1002/jbmr.1564
506. Vanni D, Pantalone A, Bigossi F, Pineto F, Lucantoni D, Salini V. New perspective for third generation percutaneous vertebral augmentation procedures: preliminary results at 12 months. J Craniovertebr Junction Spine. 2012;3(2):47–51. doi:10.4103/0974-8237.116537
507. Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine. 2011;14(5):561–569. doi:10.3171/2010.12.SPINE10286
508. Muto M, Greco B, Setola F, Vassallo P, Ambrosanio G, Guarnieri G. Vertebral body stenting system for the treatment of osteoporotic vertebral compression fracture: follow-up at 12 months in 20 cases. Neuroradiol J. 2011;24(4):610–619. doi:10.1177/197140091102400418
509. Klazen CAH, Lohle PNM, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085–1092. doi:10.1016/S0140-6736(10)
510. Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine. 2009;34(13):1349–1354. doi:10.1097/BRS.0b013e3181a4e628
511. Voormolen MHJ, Mali WPTM, Lohle PNM, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28(3):555–560.
512. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98–106.
513. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1–2):179–188.
514. Kumar K, Taylor RS, Jacques L, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008;63(4):762–770. doi:10.1227/01.NEU.0000325731.46702.D9
515. Kapural L, Yu C, Doust MW, et al. Novel 10-kHz High-frequency Therapy (HF10 Therapy) Is Superior to Traditional Low-frequency Spinal Cord Stimulation for the Treatment of Chronic Back and Leg Pain: The SENZA-RCT Randomized Controlled Trial. Anesthesiology. 2015;123(4):851–860.
516. Kapural L, Yu C, Doust MW, et al. Comparison of 10-kHz High-Frequency and Traditional Low-Frequency Spinal Cord Stimulation for the Treatment of Chronic Back and Leg Pain: 24-Month Results From a Multicenter, Randomized, Controlled Pivotal Trial. Neurosurgery. 2016;79(5):667–677. doi:10.1227/NEU.0000000000001418
517. De Andres J, Monsalve-Dolz V, Fabregat-Cid G, et al. Prospective, randomized blind effect-on-outcome study of conventional vs high-frequency spinal cord stimulation in patients with pain and disability due to failed back surgery syndrome. Pain Med. 2017;18(12):2401–2421. doi:10.1093/pm/pnx241
518. Deer T, Slavin KV, Amirdelfan K, et al. Success Using Neuromodulation With BURST (SUNBURST) Study: results From a Prospective, Randomized Controlled Trial Using a Novel Burst Waveform. Neuromodulation. 2018;21(1):56–66. doi:10.1111/ner.12698
519. Mekhail N, Levy RM, Deer TR, et al. Long-term safety and efficacy of closed-loop spinal cord stimulation to treat chronic back and leg pain (Evoke): a double-blind, randomised, controlled trial. Lancet Neurol. 2020;19(2):123–134. doi:10.1016/S1474-4422(19
520. Al-Kaisy A, Palmisani S, Smith TE, et al. Long-Term Improvements in Chronic Axial Low Back Pain Patients Without Previous Spinal Surgery: a Cohort Analysis of 10-kHz High-Frequency Spinal Cord Stimulation over 36 Months. Pain Med. 2018;19(6):1219–1226. doi:10.1093/pm/pnx237
521. Baranidharan G, Feltbower R, Bretherton B, et al. One-year Results of Prospective Research Study Using 10 kHz Spinal Cord Stimulation in Persistent Nonoperated Low Back Pain of Neuropathic Origin: maiden Back Study. Neuromodulation. 2021;24(3):479–487. doi:10.1111/ner.13345
522. Costantini A, Buchser E, Van Buyten JP. Spinal cord stimulation for the treatment of chronic pain in patients with lumbar spinal stenosis. Neuromodulation. 2010;13(4):275–279. doi:10.1111/j.1525-1403.2010.00289.x
523. Kamihara M, Nakano S, Fukunaga T, et al. Spinal cord stimulation for treatment of leg pain associated with lumbar spinal stenosis. Neuromodulation. 2014;17(4):340–345. doi:10.1111/ner.12092
524. Ade T, Roh J, Sharma G, et al. Comparative effectiveness of targeted intrathecal drug delivery using a combination of bupivacaine with either low-dose fentanyl or hydromorphone in chronic back pain patients with lumbar postlaminectomy syndrome. Pain Med. 2020;21(9):1921–1928. doi:10.1093/pm/pnaa104
525. Anderson VC, Burchiel KJ. A prospective study of long-term intrathecal morphine in the management of chronic nonmalignant pain. Neurosurgery. 1999;44(2):289–300. doi:10.1097/00006123-199902000-00026
526. Atli A, Theodore BR, Turk DC, Loeser JD. Intrathecal opioid therapy for chronic nonmalignant pain: a retrospective cohort study with 3-year follow-up. Pain Med. 2010;11(7):1010–1016. doi:10.1111/j.1526-4637.2010.00876.x
527. Doleys DM, Brown JL, Ness T. Multidimensional outcomes analysis of intrathecal, oral opioid, and behavioral-functional restoration therapy for failed back surgery syndrome: a retrospective study with 4 years’ follow-up. Neuromodulation. 2006;9(4):270–283. doi:10.1111/j.1525-1403.2006.00069.x
528. Galica RJ, Hayek SM, Veizi E, et al. Intrathecal trialing of continuous infusion combination therapy with hydromorphone and bupivacaine in failed back surgery patients. Neuromodulation. 2018;21(7):648–654. doi:10.1111/ner.12737
529. Grider JS, Etscheidt MA, Harned ME, et al. Trialing and Maintenance Dosing Using a Low-Dose Intrathecal Opioid Method for Chronic Nonmalignant Pain: a Prospective 36-Month Study. Neuromodulation. 2016;19(2):206–219. doi:10.1111/ner.12352
530. Hayek SM, McEwan MT, Veizi E, DeLozier SJ, Pogrebetskaya M. Effects of bupivacaine on opioid patient-controlled intrathecal analgesia in chronic pain patients implanted with drug delivery systems. Pain Med. 2021;22(1):22–33. doi:10.1093/pm/pnaa076
531. Ilias W, Le Polain B, Buchser E, Demartini L; oPTiMa study group. Patient-controlled analgesia in chronic pain patients: experience with a new device designed to be used with implanted programmable pumps. Pain Pract. 2008;8(3):164–170. doi:10.1111/j.1533-2500.2008.00187.x
532. Rauck RL, Wallace MS, Leong MS, et al. A randomized, double-blind, placebo-controlled study of intrathecal ziconotide in adults with severe chronic pain. J Pain Symptom Manage. 2006;31(5):393–406. doi:10.1016/j.jpainsymman.2005.10.003
533. Rauck R, Coffey RJ, Schultz DM, et al. Intrathecal gabapentin to treat chronic intractable noncancer pain. Anesthesiology. 2013;119(3):675–686. doi:10.1097/ALN.0b013e3182a10fbf
534. Rauck R, Deer T, Rosen S, et al. Accuracy and efficacy of intrathecal administration of morphine sulfate for treatment of intractable pain using the Prometra(®) Programmable Pump. Neuromodulation. 2010;13(2):102–108. doi:10.1111/j.1525-1403.2009.00257.x
535. Shaladi A, Saltari MR, Piva B, et al. Continuous intrathecal morphine infusion in patients with vertebral fractures due to osteoporosis. Clin J Pain. 2007;23(6):511–517. doi:10.1097/AJP.0b013e31806a23d4
536. Staats P, Whitworth M, Barakat M, Anderson W, Lilienfeld S. The use of implanted programmable infusion pumps in the management of nonmalignant, chronic low-back pain. Neuromodulation. 2007;10(4):376–380. doi:10.1111/j.1525-1403.2007.00127.x
537. Winkelmüller M, Winkelmüller W. Long-term effects of continuous intrathecal opioid treatment in chronic pain of nonmalignant etiology. J Neurosurg. 1996;85(3):458–467. doi:10.3171/jns.1996.85.3.0458
538. Thomson S, Chawla R, Love-Jones S, et al. Restorative neurostimulation for chronic mechanical low back pain: results from a prospective multi-centre longitudinal cohort. Pain Ther. 2021;10(2):1451–1465. doi:10.1007/s40122-021-00307-3
539. Verrills P, Mitchell B, Vivian D, Sinclair C. Peripheral nerve stimulation: a treatment for chronic low back pain and failed back surgery syndrome? Neuromodulation. 2009;12(1):68–75. doi:10.1111/j.1525-1403.2009.00191.x
540. Sator-Katzenschlager S, Fiala K, Kress HG, et al. Subcutaneous target stimulation (STS) in chronic noncancer pain: a nationwide retrospective study. Pain Pract. 2010;10(4):279–286. doi:10.1111/j.1533-2500.2009.00351.x
541. Yakovlev AE, Resch BE, Yakovleva VE. Peripheral nerve field stimulation in the treatment of postlaminectomy syndrome after multilevel spinal surgeries. Neuromodulation. 2011;14(6):534–538. doi:10.1111/j.1525-1403.2011.00387.x
542. Verrills P, Vivian D, Mitchell B, Barnard A. Peripheral nerve field stimulation for chronic pain: 100 cases and review of the literature. Pain Medicine. 2011. doi:10.1111/j.1526-4637.2011.01201.x
543. McRoberts WP, Wolkowitz R, Meyer DJ, et al. Peripheral nerve field stimulation for the management of localized chronic intractable back pain: results from a randomized controlled study. Neuromodulation. 2013;16(6):565–574. doi:10.1111/ner.12055
544. Kloimstein H, Likar R, Kern M, et al. Peripheral nerve field stimulation (PNFS) in chronic low back pain: a prospective multicenter study. Neuromodulation. 2014;17(2):180–187. doi:10.1111/ner.12139
545. Ishak B, Campos B, Brunn H, Unterberg AW, Ahmadi R. Feasibility, Safety, and Efficacy of Subcutaneous Peripheral Nerve Field Stimulation for the Treatment of Refractory Low Back Pain: a Two-year Single-center Study. Neuroscience. 2018;387:38–47. doi:10.1016/j.neuroscience.2017.12.011
546. Eldabe SS, Taylor RS, Goossens S, et al. A randomized controlled trial of subcutaneous nerve stimulation for back pain due to failed back surgery syndrome: the SubQStim Study. Neuromodulation. 2019;22(5):519–528. doi:10.1111/ner.12784
547. van Gorp EJJAA, Teernstra O, Aukes HJ, et al. Long-term effect of peripheral nerve field stimulation as add-on therapy to spinal cord stimulation to treat low back pain in failed back surgery syndrome patients: a 12-month follow-up of a Randomized Controlled Study. Neuromodulation. 2019;22(8):970–977. doi:10.1111/ner.12776
548. van Wijk RMAW, Geurts JWM, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21(4):335–344. doi:10.1097/01.ajp.0000120792.69705.c9
549. Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001;26(13):1411–1416. doi:10.1097/00007632-200107010-00003
550. Gofeld M, Jitendra J, Faclier G. Radiofrequency denervation of the lumbar zygapophysial joints: 10-year prospective clinical audit. Pain Physician. 2007;10(2):291–300.
551. Yadav A, Hagedorn JM, D’Souza RS, Engle AM, Deer TR. Effect of Patient characteristics on reported outcomes over 12 months following lumbar radiofrequency ablation: a retrospective review of 500 patients. Pain Practice. 2021;21(2):152–159. doi:10.1111/papr.12938
552. Kroll HR, Kim D, Danic MJ, Sankey SS, Gariwala M, Brown M. A randomized, double-blind, prospective study comparing the efficacy of continuous versus pulsed radiofrequency in the treatment of lumbar facet syndrome. J Clin Anesth. 2008;20(7):534–537. doi:10.1016/j.jclinane.2008.05.021
553. Çetin A, Yektaş A. Evaluation of the Short- and long-term effectiveness of pulsed radiofrequency and conventional radiofrequency performed for medial branch block in patients with lumbar facet joint pain. Pain Res Management. 2018;2018:e7492753. doi:10.1155/2018/7492753
554. Colini-Baldeschi G. Evaluation of pulsed radiofrequency denervation in the treatment of chronic facetjoint pain: an Observational Study. Anesth Pain Med. 2012;1(3):168–173. doi:10.5812/kowsar.22287523.2854
555. Mikeladze G, Espinal R, Finnegan R, Routon J, Martin D. Pulsed radiofrequency application in treatment of chronic zygapophyseal joint pain. Spine J. 2003;3(5):360–362. doi:10.1016/s1529-9430(03)00065-2
556. Lindner R, Sluijter ME, Schleinzer W. Pulsed radiofrequency treatment of the lumbar medial branch for facet pain: a retrospective analysis. Pain Medicine. 2006;7(5):435–439. doi:10.1111/j.1526-4637.2006.00175.x
557. McCormick ZL, Choi H, Reddy R, et al. Randomized prospective trial of cooled versus traditional radiofrequency ablation of the medial branch nerves for the treatment of lumbar facet joint pain. Reg Anesth Pain Med. 2019;44(3):389–397. doi:10.1136/rapm-2018-000035
558. Salman OH, Gad GS, Mohamed AA, Rafae HH, Abdelfatah AM. Randomized, controlled blind study comparing sacroiliac intra-articular steroid injection to radiofrequency denervation for sacroiliac joint pain. Egyptian J Anaesthesia. 2016;32(2):219–225. doi:10.1016/j.egja.2015.07.005
559. Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of radiofrequency denervation on pain intensity among patients with chronic low back pain: the mint randomized clinical trials. JAMA. 2017;318(1):68–81. doi:10.1001/jama.2017.7918
560. Smuck M, Khalil J, Barrette K, et al. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. Reg Anesth Pain Med. 2021;46(8):683–693. doi:10.1136/rapm-2020-102259
561. Koreckij T, Kreiner S, Khalil JG, et al. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 24-Month treatment arm results. N Am Spine Soc J. 2021;8:100089. doi:10.1016/j.xnsj.2021.100089
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Best Practice Guidelines on the Diagnosis and Treatment of Vertebrogenic Pain with Basivertebral Nerve Ablation from the American Society of Pain and Neuroscience
Sayed D, Naidu RK, Patel KV, Strand NH, Mehta P, Lam CM, Tieppo Francio V, Sheth S, Giuffrida A, Durkin B, Khatri N, Vodapally S, James CO, Westerhaus BD, Rupp A, Abdullah NM, Amirdelfan K, Petersen EA, Beall DP, Deer TR
Journal of Pain Research 2022, 15:2801-2819
Published Date: 14 September 2022
