Back to Journals » Orthopedic Research and Reviews » Volume 11
Systematic review of the clinical effectiveness for long-term follow-up of total hip arthroplasty
Authors Smith LK , Dures E, Beswick AD
Received 21 December 2018
Accepted for publication 21 March 2019
Published 2 July 2019 Volume 2019:11 Pages 69—78
DOI https://doi.org/10.2147/ORR.S199183
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Clark Hung
Video abstract presented by Lindsay K. Smith.
Views: 309
Lindsay K Smith,1 Emma Dures,2 AD Beswick3
1Department of Trauma and Orthopaedics, Weston Area Health NHS Trust, Weston-super-Mare, North Somerset, UK; 2Centre for Health and Clinical Research, University of the West of England, Bristol, UK; 3Musculoskeletal Research Unit, University of Bristol, Bristol, UK
Objectives: Total hip arthroplasty (THA) is highly successful but national registries indicate that average age has lowered and that younger patients are at higher risk of revision. Long-term follow-up of THA was historically recommended to identify aseptically failing THA, minimising the risks associated with extensive changes, but follow-up services are now in decline. A systematic review was conducted to search for evidence of the clinical or cost-effectiveness of hip arthroplasty surveillance.
Methods: The study was registered with PROSPERO International Prospective Register of Systematic Reviews and conducted according to PRISMA guidelines; databases included MEDLINE and Embase, and all studies were quality assessed. Original studies (2005 to 2017) reporting follow-up of adults with THA in situ >5 years were included. Researchers extracted quantitative and qualitative data from each study.
Results: For eligibility, 4,137 studies were screened: 114 studies were included in the final analysis, representing 22 countries worldwide. Data extracted included study endpoint, patient detail, loss to follow-up, revisions, scores and radiographic analysis. Six themes were derived from inductive content analysis of text: support for long-term follow-up, subgroups requiring follow-up, effect of materials/techniques on THA survival, effect of design, indicators for revision, review process. Main findings—follow-up was specifically recommended to monitor change (eg asymptomatic loosening), when outcomes of joint construct are unknown, and for specific patient subgroups. Outcome scores alone are not enough, and radiographic review should be included.
Conclusion: There were no studies directly evaluating the clinical effectiveness of the long-term follow-up of THA but expert opinions from a range of international authors advocated its use for defined subgroups to provide patient-centred care. In the absence of higher level evidence, these opinions, in conjunction with emerging outputs from the national joint registries, should be used to inform services for long-term follow-up of THA.
Keywords: hip joint, replacement, surveillance, revision, long-term, continuing
Introduction
For many people, total hip arthroplasty (THA) is successful for treating a painful, arthritic hip but national registries indicate that 10% of implants will subsequently require revision, which increases to 30% for those under 50 years old at primary surgery.1 Up to five years postoperatively, revision is predominantly undertaken for dislocation, infection or prosthetic failure,2–4 all of which present with pain. In the longer term, there is an increase in revision for aseptic loosening which can be asymptomatic and thus, surveillance offeres identification of a potential problem for these patients. This was predominantly attributed to osteolysis generated by the wear debris from the widespread use of polyethylene5 but with the change to cross-linked polyethylene, future patterns of presentation may differ.
Although there is mandatory surveillance of metal-on-metal hip arthroplasty in the UK,6 there is no mandatory requirement for follow-up of other types of THA, and concern about follow-up is widespread as arthroplasty surveillance has been reduced.7–9 Some suggest it can be conducted by general practitioners, others maintain that it should be the orthopedic team10,11 and still others are undecided about such services. In view of economic constraints on health services, plus concerns about medicalization and overdiagnosis,12 long-term follow-up of any patient group must be justified by evidence that it offers patient-centred clinical effectiveness and cost-efficiency. We conducted a systematic review of the literature to search for evidence of the clinical or cost-effectiveness of hip arthroplasty surveillance services.
Methods
The systematic review was registered with PROSPERO, International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=20517); methods were adapted from the Cochrane Handbook13 and it was conducted according to PRISMA guidelines,14 although not limited to randomized trials.
Inclusion and exclusion criteria
The selected population were adults with THA in situ for longer than five years. Studies were included if they reported any form of follow-up or surveillance or review of people with THA, whether face-to-face or by questionnaire or by virtual methods. Studies were excluded if reporting the development of an outcomes tool or a surgical, radiographic or chemical intervention, or were reporting secondary data analysis. Evaluations of interventions in randomized controlled trials were considered as cohort studies.
Literature search
We searched: MEDLINE, Embase and PsycINFO on Ovid, CINAHL on EBSCOhost, the Cochrane Library and abstracts of scientific meetings. Searches were limited by date (January 2005 to May 2017) and to English language. All types of original research study were considered, including prospective or retrospective longitudinal studies, cross-sectional studies and randomized trials. Where a report existed of an earlier study, the most recent published paper was retrieved. The search strategy was developed for MEDLINE and terms were adapted for use in other databases (Table 1).
 |
Table 1 Search strategy |
Study selection
Titles and abstracts were screened for eligibility by two reviewers before proceeding to the full text: inconsistencies between reviewers were resolved by discussion based on full text articles.
Data extraction
The records of all saved searches were downloaded into Refworks© (ProQuest L.L.C.); then transferred to a Microsoft Excel spreadsheet for cataloging decisions on inclusion and exclusion. A second spreadsheet was developed for data extraction which included: study details and period, setting and country, assessment of study endpoint, method of statistical analysis, number and age of patients, loss to follow-up, number of revisions, outcome scores and radiographic analysis, reports of asymptomatic loosening of THA and any report of costs or cost-effectiveness.
Following the registration in PROSPERO, a secondary method was employed to capture text and opinion relating to the research question as early stages of our review suggested a lack of studies that directly evaluated follow-up services. The Joanna Briggs Institute propose that inclusion of text, to which qualitative review techniques are subsequently applied, provides the opportunity to describe the insights and opinions of authors to inform the quantitative evidence.15 A summary sentence or paragraph reporting the authors’ interpretation of the findings of each study was extracted for qualitative analysis.
A check between researchers for consistency and quality of the extracted data was conducted after completion of the initial 10 studies, and a further check was completed on a random sample of 20 papers at the end of data extraction.
Methodological quality
All the included studies were assessed for quality and rigour against the methodological index for nonrandomized studies (MINORS)16 and a global score was assigned to each. The MINORS score is a summation of individual item scores (zero to two for each item), with maximum of 24 for comparative studies and 16 for noncomparative studies (Table 2).
 |
Table 2 Methodological items for nonrandomized studies (MINORS) |
Data analysis
Descriptive statistics were used to present quantitative data and a method of hybrid content analysis was used for the qualitative data.17 Primary outcome measures were the number of joints that survived, number that failed and number revised (or planned for revision) as a proportion of the number and type of hip replacements included in each study, plus any data on costs or cost-effectiveness. Secondary outcomes were the type of patient reported outcome scores and health-related quality of life incorporated in each study.
The qualitative analysis was completed in two phases: the first was to apply inductive content analysis to the data extracted from each study to inform a thematic framework that summarised the text on clinical and cost-effectiveness (primary author). The second phase was a deductive analysis, guided by the framework, to verify the inductive analysis and to further synthesize the data relating to the research question. This second phase was conducted by two co-authors and was an iterative process, during which the framework was reviewed and amended to provide a final analysis agreed by all. The results were reported with the quantitative data and a MINORS score for each study, to allow readers to assess the textual evidence as unequivocal, credible or unsupported.15
Results
Studies included
The review process identified 4,943 articles (4,137 after removal of duplicates) which were screened for eligibility. Many records were excluded because they were not THA or presented short-term follow-up, leaving 159 potentially eligible full-text articles. A further 45 were subsequently excluded after full-text review for reasons listed in Figure 1, leaving 114 studies for inclusion in the final analysis. The dates of primary surgery ranged from 1965 to 2011 and there were 22 countries of origin. Five studies utilized a case–control method, 96 were case series, 10 were randomized controlled trials (RCT) and three were cohort studies. An overview of study characteristics is shown in Table 3 and details from each study are presented in Supplementary materials.
 |
Figure 1 Flow diagram showing the results of the literature search. Abbreviation: DEXA, dual-energy X-ray absorptiometry. |
 |
Table 3 Characteristics of included studies |
Quality assessment
All studies included clear aims and outcomes, and the design was prospective in 50%. The MINORS scores can be seen in Figures 2 and 3. Three of the studies reported a sample size calculation and statistical analysis was most commonly a prosthesis survival statistic.
 |
Figure 2 Histogram showing number of studies with MINORS scores for comparative studies (zero=poor, 24=good).Abbreviation: MINORS, methodological index for nonrandomized studies. |
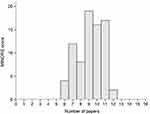 |
Figure 3 Histogram showing number of studies with MINORS scores for noncomparative studies (zero=poor, 16=good).Abbreviation: MINORS, methodological index for nonrandomized studies. |
Clinical effectiveness
The data showed a wide range in age and number of patients (Table 4). None of the studies specifically evaluated the clinical effectiveness of follow-up in terms of benefit to the patients or the providers through diagnosis of asymptomatic changes although data relevant to the clinical effectiveness of follow-up included the reporting of radiographic review of THA (86% of studies), reports of asymptomatic loosening (36% of studies) and the number of revision hip arthroplasties (Table 4). The use of patient-reported outcome measures, which are designed to capture changes in function and symptoms as perceived by the patient, increased over time. The most frequently used outcome measure was the Harris Hip Score, which became widely adopted by English-speaking orthopedic communities as a surgeon-completed score following initial publication in 1969.18 The geographical and time-related use of outcome scores can be seen in Table 5.
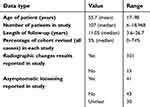 |
Table 4 Summary of extracted data |
 |
Table 5 Use of outcome scores by country and time |
Content analysis
Inductive content analysis was applied to extracted text and summarised by a representative phrase. Two of the authors deductively reviewed and revised the framework until agreement was reached between all authors that it related to the research question. Six themes emerged that encapsulate the findings. These are summarised as follows with illustrative text for each theme (Table 7) and further details in Supplementary materials.
 |
Table 6 Subgroup diagnoses in THA studies |
 |
Table 7 Themes and illustrative quotes from content analysis |
Support for long-term follow-up
Long-term follow-up was directly advocated by the authors in 41 studies, 21 to monitor changes and 20 for unknown outcomes. The reasons given were evaluation of the temporal effect on fixation and materials, continued observation of host response to implanted materials, and to provide understanding of progressive and potentially damaging changes, especially in younger patients.
Subgroups requiring follow-up over time
The outcomes of THA in specific subgroups of patients was reported in 28 studies—nine monitored changes around the prosthesis and 19 assessed the patients for unknown outcomes. The categories included age of patient (10 studies), weight (three studies), activity levels (three studies), gender (one study), and a range of diagnoses listed in Table 6. Some reported survival of the THA in the subgroup; others reported mid-term results. Many authors advocated longer follow-up (either explicitly or implicitly) due to concerns about patterns of failure of the THA in the defined subgroup of patients and the need for revision.
Effect of materials and techniques on survival of THA
Twenty studies described the effect of a range of materials and techniques for THA. Materials included titanium, hydroxyapatite coatings, ceramic-on-ceramic bearings, metal-on-metal bearings, and polyethylene (the wear reduction of highly cross-linked polyethylene was demonstrated at mid-term). Authors in 13 of the studies claimed that the results supported continuation of their practice and in the others, further long-term follow-up was advocated to assess THA survival; some emphasized the importance of follow-up into the second and third decades.
Effect of design on survival of THA
Thirteen studies examined the effect of construct design on THA survival and described outcomes and failure mechanisms related to fixation, shape of femoral stems and size of the femoral head.
Indicators for revision
Factors that might predispose to revision THA were addressed in five studies; two addressed high polyethylene wear rates (both predated the introduction of cross-linked polyethylene), one reported on primary hospital type (no effect on long-term survival) and two others reported on the use of radiographic monitoring to identify asymptomatic loosening.
Elements of the review process
Many studies described the methods of follow-up and, although most were research studies, some were reporting results from ongoing surveillance services.19–21 Radiographic assessment was widespread with 101 studies (89%) reporting radiographic results (Table 4) and most included a patient-reported outcome score (Table 5). The use of validated patient-centred outcome scores has increased over time, with some studies adding a contemporary measure to a more traditional one.19,22
Ten defined the processes that should be included in long-term follow-up of THA, predominantly the inclusion of radiographic review and the use of outcome scores. Two studies referred to loosening identified on X-ray in the absence of symptoms and highlighted the lack of correlation between the two. Both studies were of a cohort of cemented THA with polyethylene that predated the use of cross-linked polyethylene.
There were no studies on the cost-effectiveness of the review process. One paper presented data on the cost-effectiveness of the primary hip arthroplasty and the authors emphasized the importance of patient selection to maximize value for THA in the longer term.23
Discussion
There were no studies which directly evaluated the clinical or cost-effectiveness of THA surveillance and so the studies were analyzed using a combination of descriptive analysis and qualitative techniques. The summary data demonstrate the wide range of countries (22 in total) and the significant length of follow-up (up to 27 years) that have contributed to this review. In addition to the summary data, analysis of authors' opinions showed that 41 studies specifically advocated follow-up and none suggested that it should be abandoned. The reasons for continued surveillance were because the effect of time, interaction with the host body and outcome of specific techniques are unknown factors, plus the need for evidence of the outcomes of newer materials and alternative fixation methods, and most importantly, to provide patient-focussed care. In addition, the use of follow-up was advocated for subgroups of patients such as those with dysplasia or avascular necrosis, or patient characteristics such as the super-obese due to poorer long-term outcomes which predispose them to revision arthroplasty. Other studies emphasized the need for follow-up of younger or more active patients due to the increased risk of revision. These comments form a body of expert opinion for consideration in provision of long-term follow-up services.
As described earlier, long-term follow-up has often been used to identify asymptomatic failure following THA. There were 41 studies (Table 4) that specifically referred to asymptomatic failure and of these, 29 studies (70%) were of patients whose primary surgery took place before the year 2000, which is before the widespread use of cross-linked polyethylene, the long-term outcomes of which may change the pattern of presentation. Newer materials have improved the survival rates and reduced the need for surveillance in the first decade following THA,4 but surveillance in the second and third decades was still considered important by many of the authors. Although new or modified designs of THA that are introduced in the UK can now be closely monitored,24 and national joint registries provide data on the longevity of components, experiences with metal on metal hip arthroplasty have highlighted the negative effect of insufficient surveillance.25 Discoveries in relation to the failure of THA mean that the interpretation of failure is still evolving, and some long-term follow-up may still be required to assess the patterns of impending failure and to inform the future care of patients.1,26,27
The methods used in long-term follow-up have not been precisely defined9 and, although the combination of outcome scores and radiographic evaluation is common, their correlation with each other is not guaranteed.28,29 The implication is that the use of an outcome score without radiographic evaluation will not be sufficient to monitor THA.30 Some orthopedic surgeons will consider revision for radiological loosening in the absence of significant symptoms,31 as “an early revision on adequate bone stock presents more chance of success and a better functional prognosis for the patient”.32 This illustrates that the threshold for progression to revision surgery in cases of aseptic loosening is not a fixed and definable point, and that the decision-making process includes both objective and subjective elements together with patient choice.
We found no evidence of the cost-effectiveness of THA surveillance. The lack of evidence threatens the continuation of follow-up services as cost implications are unknown: can follow-up services reduce costs through simple, timely revision instead of more complicated, reconstructive surgery or emergency surgery?33 Although some studies have evaluated the cost-effectiveness of THA,34–36 they do not discuss the use of surveillance as a tool to facilitate “timely” revision. One study which evaluated the economics of three models of follow-up recommended less intensive early follow-up.37
Limitations
The strengths and weaknesses of this review are not unique and are associated with inclusion of observational cohort studies which are subject to confounding factors and bias, and impacted by loss to follow-up, particularly when the study extends over many years.38 The geographic removal of patients, development of comorbidities or death because of advanced age, are all known barriers to completion of longitudinal studies.39 In this review, 63% of studies had loss to follow-up of ≤20% and the quality was also compromised by lack of independent assessment of study outcomes; long-term, single centre studies often have a limited choice of staff available to obtain study outcomes.40
Future
The growing number of primary THA leads to a growing number of revision surgeries41 with associated costs. It is unclear if the use of long-term follow-up can lessen this burden by identifying patients in time for a relatively simple revision or reducing the number of those requiring emergency surgery for periprosthetic fracture. Currently, the provision of THA surveillance is sporadic and the cost of delivering it proves prohibitive for many hospitals, leading to consideration of alternative models of follow-up.42,43 A research programme in the UK is currently exploring the implications for disinvestment and the outcomes will be relevant for patients, health professionals and commissioners when considering future services.44 With the current emphasis on patient-centred care and long-term conditions, there may be benefit in offering selected subgroups of patients a choice for follow-up. The model of delivery of such a service should be time and cost-efficient, and responsive to change as new evidence emerges from national joint registries.
Conclusion
We systematically reviewed the literature for evidence of the clinical effectiveness of long-term follow-up of hip arthroplasty. We were unable to identify specific quantitative evidence but the evaluation of authors’ comments from a wide range of countries offers expert insight into the use of follow-up in the continuing provision of long-term, patient-centred care following total hip replacement.
Acknowledgments
This work was supported by the National Institute for Health Research and Health Education England and constitutes independent research arising from a Clinical Lectureship (CAT_CL_2013_04_005). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health & Social Care.
Disclosure
Dr Lindsay K Smith reports grants from National Institute for Health Research UK, during the conduct of the study. The other authors report no conflicts of interest in this work.
References
1. National Joint Registry. 14th annual report 2017. Available from: http://www.njrreports.org.uk.
2. The Swedish Hip Arthroplasty Register. Available from: https://shpr.registercentrum.se/shar-in-english.
3. Australian Orthopaedic Association National Joint Replacement Register. 2017 Annual report. Available from: https://aoanjrr.sahmri.com.
4. Keeney JA, Ellison BS, Maloney WJ, Clohisy JC. Is routine mid-term total hip arthroplasty surveillance beneficial? Clin Orth Relat Res. 2012;470:3220–3226. doi:10.1007/s11999-012-2411-7
5. Harris WH. Conquest of a worldwide human disease: particle-induced periprosthetic osteolysis. Clin Orth Relat Res. 2004;429:39–42. doi:10.1097/01.blo.0000149821.72760.39
6. Medicines and Healthcare products Regulatory Agency. All metal-on-metal (MoM) hip replacements: updated advice for follow-up of patients. Available from: https://www.gov.uk/drug-device-alerts/all-metal-on-metal-mom-hip-replacements-updated-advice-for-follow-up-of-patients.
7. Smith LK. Assessment of the current state of hip arthroplasty surveillance in the UK. Musculoskelet Care. 2014;12(4):232–238.
8. Lovelock TM, Broughton NS. Follow-up after arthroplasty of the hip and knee. Are we over-servicing or under-caring? Bone & Joint J. 2018;100-B(1):6–10. doi:10.1302/0301-620X.100B1.BJJ-2017-0779.R1
9. Lieberman JR, Leger RR, Tao JC, Clohisy JC, Meneghini RM. Total hip arthroplasty surveillance: when do we see our patients postoperatively? J Arthroplasty. 2011;26:1161–1164. doi:10.1016/j.arth.2011.04.035
10. Haddad FS, Ashby E, Konangamparambath S. Should follow-up of patients with arthroplasties be carried out by general practitioners? Bone & Joint J. 2007;89-B:1133–1134.
11. British Hip Society, British Orthopaedic Association, Royal College of Surgeons of England. 2017 Commissioning guide: pain arising from the hip in adults. Available from: https://www.boa.ac.uk/wp-content/uploads/2017/11/Pain-Arising-from-the-Hip-Guide-Final.pdf.
12. Wise J. Choosing Wisely: how the UK intends to reduce harmful medical overuse. BMJ. 2017;356:j370. doi:10.1136/bmj.j370
13. Cochrane handbook for systematic reviews of interventions version 5.1.0; 2011. Available from: http://training.cochrane.org/handbook.
14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemio. 2009;62:1006–1012. doi:10.1016/j.jclinepi.2009.06.005
15. Joanna Briggs Institute Reviewer‘s Manual. 2017. Available from: https://reviewersmanual.joannabriggs.org/display/MANUAL/4.1+Text+and+opinion+reviews+and+evidence-based+practice.
16. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716.
17. Dures E, Fraser I, Almeida C, et al. Patients’ perspectives on the psychological impact of inflammatory arthritis and meeting the associated support needs: open-ended responses in a multi-centre survey. Musculoskelet Care. 2016;15:175–185. doi:10.1002/msc.1159
18. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51-A:737–755. doi:10.2106/00004623-196951040-00012
19. de Kam DC, Gardeniers JW, Veth RP, Schreurs BW. Good results with cemented total hip arthroplasty in patients between 40 and 50 years of age. Acta Orthop. 2010;81:165–170. doi:10.3109/17453671003717831
20. Kang JS, Moon KH, Park SR, Choi SW. Long-term results of total hip arthroplasty with an extensively porous coated stem in patients younger than 45 years old. Yonsei Med J. 2010;51:100–103. doi:10.3349/ymj.2010.51.1.100
21. Maggs JL, Smeatham A, Whitehouse SL, Charity J, Timperley AJ, Gie GA. The exeter contemporary flanged cemented acetabular component in primary total hip arthroplasty. Bone Joint J. 2016;98-B:307–312. doi:10.1302/0301-620X.98B3.35901
22. Danesh-Clough T, Bourne RB, Rorabeck CH, McCalden R. The mid-term results of a dual offset uncemented stem for total hip arthroplasty. J Arthroplasty. 2007;22:195–203. doi:10.1016/j.arth.2006.04.006
23. Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013;95-B:115–121. doi:10.1302/0301-620X.95B1.29835
24. Beyond Compliance. Available from: http://www.beyondcompliance.org.uk.
25. Hunt L, Whitehouse MR, Beswick AD, Porter ML, Howard P, Blom AW. Implications of introducing new technology: comparative survivorship modelling of metal-on-metal hip replacements and contemporary alternatives in the national joint registry. J Bone Joint Surg Am. 2018;100:189–196. doi:10.2106/JBJS.17.00039
26. Surace MF, Monestier L, Vulcano E, Harwin SF, Cherubino P. Conventional versus cross-linked polyethylene for total hip arthroplasty. Orthopedics. 2015;38:556–561. doi:10.3928/01477447-20150902-05
27. Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J Bone Joint Surg Am. 2006;88:1183–1191. doi:10.2106/JBJS.D.02916
28. Hartofilakidis G, Karachalios T, Georgiades G, Kourlaba G. Total hip arthroplasty in patients with high dislocation: a concise follow-up, at a minimum of fifteen years, of previous reports. J Bone Joint Surg Am. 2011;93:1614–1618. doi:10.2106/JBJS.J.00875
29. Shaju KA, Hasan ST, D‘Souza LG, McMahon B, Masterson EL. The 22-mm vs the 32-mm femoral head in cemented primary hip arthroplasty long-term clinical and radiological follow-up study. J Arthroplasty. 2005;20:903–908. doi:10.1016/j.arth.2005.02.005
30. Smith LK, Cramp F, Palmer S, Coghill N, Spencer RF. Empirical support for radiographic review: a follow up study of total hip arthroplasty. Hip Int. 2013;23:80–86. doi:10.5301/HIP.2012.9912
31. Bidar R, Kouyoumdjian P, Munini E, Asencio G. Long-term results of the ABG-1 hydroxyapatite coated total hip arthroplasty: analysis of 111 cases with a minimum follow-up of 10 years. Orthop Traumatol Surg Res. 2009;95:579–587. doi:10.1016/j.otsr.2009.10.001
32. Boyer B, Philippot R, Geringer J, Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop. 2012;36:511–518. doi:10.1007/s00264-011-1289-4
33. Kamath AF, Austin DC, Derman PB, Israelite CL. Unplanned hip arthroplasty imposes clinical and cost burdens on treating institutions. Clin Orth Relat Res. 2013;471:4012–4019. doi:10.1007/s11999-013-3226-x
34. Räsänen P, Paavolainen P, Sintonen H, et al. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78:108–115. doi:10.1080/17453670610013501
35. Burns AWR, Bourne RB. Economics of revision total hip arthroplasty. Current Orthop. 2006;20(3):203–207. doi:10.1016/j.cuor.2006.02.007
36. Fordham R, Skinner J, Wang X, Nolan J; The Exeter Primary Outcome Study Group. The economic benefit of hip replacement: a 5-year follow-up of costs and outcomes in the exeter primary outcomes study. BMJ Open. 2012;2:e000752. doi:10.1136/bmjopen-2011-000752
37. Bolz KMD, Crawford RW, Donnelly B, Whitehouse SL, Graves N. The cost-effectiveness of routine follow-up after primary total hip arthroplasty. J Arthroplasty. 2010;25:191–196. doi:10.1016/j.arth.2008.12.009
38. Wylde V, Beswick AD, Dennis J, Gooberman-Hill R. Post-operative patient-related risk factors for chronic pain after total knee replacement: a systematic review. BMJ Open. 2017;7:e018105. doi:10.1136/bmjopen-2017-018105
39. Angadi DS, Brown S, Crawfurd EJ. Cemented polyethylene and cementless porous-coated acetabular components have similar outcomes at a mean of seven years after total hip replacement: a prospective randomised study. Bone Joint J. 2012;94-B:1604–1610.
40. Lainiala O, Eskelinen A, Elo P, Puolakka T, Korhonen J, Moilanen T. Adverse reaction to metal debris is more common in patients following MoM total hip replacement with a 36 mm femoral head than previously thought: results from a modern MoM follow-up programme. Bone Joint J. 2014;96-B:1610–1617. doi:10.1302/0301-620X.96B12.33742
41. Pabinger C, Geissler A. Utilization rates of hip arthroplasty in OECD countries. Osteoarthritis Cartilage. 2014;22:734–741.
42. Hacking C, Weinrauch P, Whitehouse SL, Crawford RW, Donnelly WJ. Is there a need for routine follow-up after primary total hip arthroplasty? ANZ J Surgery. 2010;80:737–740.
43. Roberts N, Mujica-Mota R, Williams D. The cost of improving hip replacement follow-up in the UK. Musculoskelet Care. 2016;14:116–120. doi:10.1002/msc.v14.2
44. Conaghan P, Smith LK, Kingsbury S, et al. Towards UK post arthroplasty follow-up recommendations: UK SAFE. Available from: https://www.journalslibrary.nihr.ac.uk/programmes/hsdr/1470146. Accessed January 24, 2018.
45. Hartofilakidis G, Georgiades G, Babis GC. A comparison of the outcome of cemented all-polyethylene and cementless metal-backed acetabular sockets in primary total hip arthroplasty. J Arthroplasty. 2009;24:217–225. doi:10.1016/j.arth.2007.11.010
46. Broeke RH, Harings SE, Emans PJ, Jutten LM, Kessels AG, Geesink RG. Randomized comparison between the cemented scientific hip prosthesis and omnifit: 2-year DEXA and minimum 10-year clinical follow-up. J Arthroplasty. 2013;28:1354–1361. doi:10.1016/j.arth.2012.09.024
47. Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. A concise follow-up, at twenty years, of previous reports. J Bone Joint Surg Am. 2011;93-A:1335–1338. doi:10.2106/JBJS.J.00448
48. Issa K, Harwin SF, Malkani AL, Bonutti PM, Scillia A, Mont MA. Bariatric orthopaedics: total hip arthroplasty in super-obese patients (those with a BMI of ≥50 kg/m2). J Bone Joint Surg Am. 2016;98-A:180–185. doi:10.2106/JBJS.O.00474
49. Chandran P, Azzabi M, Miles J, Andrews M, Bradley J. Furlong hydroxyapatite-coated hip prosthesis vs the Charnley cemented hip prosthesis. J Arthroplasty. 2010;25:52–57. doi:10.1016/j.arth.2008.10.009
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
