Back to Journals » OncoTargets and Therapy » Volume 14
Synchronous Multiple Lung Cancers with Lymph Node Metastasis and Different EGFR Mutations: Intrapulmonary Metastasis or Multiple Primary Lung Cancers?
Authors Qu R , Tu D , Ping W, Zhang N, Fu X
Received 1 December 2020
Accepted for publication 26 January 2021
Published 16 February 2021 Volume 2021:14 Pages 1093—1099
DOI https://doi.org/10.2147/OTT.S294953
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Leo Jen-Liang Su
Rirong Qu, Dehao Tu, Wei Ping, Ni Zhang, Xiangning Fu
Department of Thoracic Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430030, People’s Republic of China
Correspondence: Xiangning Fu
Department of Thoracic Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430030, People’s Republic of China
Tel +86 13607150390
Fax +86 027-83665211
Email [email protected]
Background: There is no consensus on whether patients with synchronous multiple lung cancers (SMLC) who present with lymph node metastasis (LNM) but whose epidermal growth factor receptor (EGFR) mutations are different are considered to have intrapulmonary metastases or multiple primary lung cancers. Few studies on these patients have been reported.
Methods: The electronic medical records of patients with surgically resected multiple lung cancers between February 2016 and July 2019 were retrospectively reviewed, focusing on the clinical characteristics and prognosis of patients with LNM and different EGFR mutations.
Results: A total of 125 patients were diagnosed with SMLC, and only 8 patients had LNM and different EGFR mutations. Their mean age was 61.43 ± 8.08 years (range 47– 69 years). EGFR detection suggested that 4 patients had completely different mutation types, and 4 patients had mutations in only 1 tumor. Only 1 of the 17 total lesions was squamous cell carcinoma, the rest were adenocarcinoma. All patients underwent adjuvant therapy after surgery. Except for 1 patient who underwent chemotherapy, the rest received tyrosine kinase inhibitor-targeted therapy. As at 15 October 2020, the average follow-up time was 28.68 ± 10.74 months (range 10.5– 40.5 months), and all patients were alive except 1 who died from extensive pleural metastasis.
Conclusion: The current study highlights the clinical importance of EGFR detection in SMLC, especially in patients with LNM. SMLC with LNM and different EGFR mutations should be considered multiple primary lung cancers rather than intrapulmonary metastases, and comprehensive treatment based on surgery may be preferable in these patients due to a good prognosis.
Keywords: EGFR, epidermal growth factor receptor, IPM, intrapulmonary metastasis, LNM, lymph node metastasis, MPLC, multiple primary lung cancers, SMLC, synchronous multiple lung cancers
Introduction
With the advancement of imaging technology and the enhancement of people’s health awareness, more cases of synchronous multiple lung cancers (SMLC) are being diagnosed. The incidence of SMLC in previously reported studies1 ranges from 1% to 7%, and the detection rate is rapidly increasing. The diagnosis of such patients is critical because the stage assessment and treatment options for multiple primary lung cancers (MPLC) and intrapulmonary metastasis (IPM) are completely different. MPLC is considered to be a local disease and surgery is the first choice, whereas IPM is considered to be a systemic disease and chemotherapy and other adjuvant treatments are the first choice. Differentiating between MPLC and IPM is based largely on clinicopathological features, however, there is still no definitive guideline or algorithmic approach. Therefore, distinguishing between MPLC and IPM is challenging for clinicians when tumor histology indicates similar subtypes.
The earliest criteria used to define MPLC was the Martini and Melamed standard in 1975, which stated that for patients with MPLC of similar histology, their common lymphatic drainage system must be free of tumor metastasis.2 In contrast, the Antakli criteria3 proposed in 1995 indicates that the absence of lymph node metastasis (LNM) is not a requirement for MPLC of similar histology, as long as two or more of the following five criteria are met: (1) anatomically distinct; (2) associated premalignant lesion; (3) no systemic metastases; (4) no mediastinal spread; (5) different DNA ploidy. It was mentioned there for the first time that different molecular genetic characteristics can also be used as the basis for a diagnosis of MPLC. Since then the American College of Chest Physicians (ACCP) has revised and updated the Martini and Melamed criteria in 2003, 2007, and 2013.4–6 The criteria propose that patients with the same histology must have no N2 or N3 LNM, and emphasize the importance of molecular genetic diagnosis. With the development of next-generation gene sequencing technology in recent decades, many studies7–12 have demonstrated the role of genomics in the diagnosis of MPLC. Notably however, to date no definitive consensus has been reached on the various issues related to the diagnosis, treatment, and prognosis of SMPLC.
The current study investigated patients with LNM and different EGFR mutations who had been diagnosed with SMLC and undergone surgical resection. To the best of our knowledge, there are still few reports on such patients. To address the issue of whether such patients should be diagnosed with MPLC or IPM, clinicopathological features, EGFR mutations, and follow-up observations in these patients were analyzed.
Patients and Methods
Patients
Clinical data derived from patients with SMLC who had nodal metastasis but different EGFR mutations who were treated at the department of thoracic surgery, Wuhan Tongji Hospital from February 2016 to July 2019 were retrospectively analyzed. The inclusion criteria were (1) ≥ 2 tumors, (2) acceptable cardiopulmonary function, (3) no previous history of tumors, (4) all lesions tested for EGFR and the mutations were different, and (5) no distant metastasis on preoperative examinations, including chest computed tomography (CT), abdominal CT or ultrasonography, brain CT or magnetic resonance imaging, and whole body bone scans. The exclusion criteria were (1) incomplete patient data, (2) adjuvant treatment before surgery, and (3) no LNM detected after surgery. The study was approved by the institutional review board of Tongji Medical College of Huazhong University of Science and Technology, China, and it was also conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Surgical Procedure
All surgical procedures were performed with combined intravenous-inhalation anesthesia plus double lumen endotracheal intubation. The surgery was performed using a 3-cm small single-port approach. A 3-cm incision was made between the 5th ribs in the mid-axillary line of the surgery side to place a thoracoscope, an elbow laparoscopic suction device, and electrocoagulation hooks, and a bipartite clamp was placed to hold the lung lobe if necessary. In bilateral surgery, one side of the surgery was completed then the contralateral surgery was performed in the same way. Specific procedures and strategies used to determine the extent of surgical resection were as previously described.13,14
Tissue Samples and EGFR Mutation Analysis
Genomic DNA was extracted from fresh tissues using the QIAamp DNA Tissue Kit (Qiagen, Germany). EGFR mutations were detected using commercially available kits from YZY Medical (Wuhan, China) based on amplification refractory mutation system real-time polymerase chain reaction technology. Twenty-nine different EGFR mutations in exons 18–21 were detected in the lesions of the patients in the current study.
Follow-Up
Follow-up was performed by outpatient or telephone. Follow-up times were calculated from the day after surgery, and included observations up to 15 October 2020. In the first year after surgery, chest CT, tumor markers, and abdominal ultrasound were reviewed every 3 months. In the second year after surgery the same indicators were reviewed every 6 months. Thereafter they were reviewed annually.
Results
Clinical Characteristics of Patients and Lesions
A total of 125 patients with SMLC underwent surgery at the department of thoracic surgery, Wuhan Tongji Hospital between February 2016 and July 2019, of which 8 met the inclusion criteria. They included 5 males and 3 females, and their mean age was 61.43 ± 8.08 years (range 47–69 years). All the males had a history of smoking, and 5 patients had comorbid hypertension. Of the 8 patients, 5 were found to have tumors as a result of health examination by chest CT and 3 were found to have tumors when they presented with respiratory symptoms. All patients had normal tumor markers. Cardiopulmonary function was acceptable in all patients. The 8 patients had a total of 17 lesions, with a mean diameter of 29.91 ± 12.21 mm, including 8 ground-glass opacity (GGO) lesions and 9 solid lesions. Two patients had lesions in both lungs. One patient had 3 lesions, and the rest had 2 lesions. There were 5 lesions in the right upper lobe, 4 in the right middle lobe, 3 in the left upper or lower lobe, and 2 in the right lower lobe. Only 1 patient’s lesions were located in the same lobe. The clinical characteristics of the patients and lesions are shown in Tables 1 and 2 respectively.
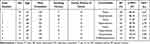 |
Table 1 Clinical Characteristics of Patients |
 |
Table 2 Clinical Characteristics of Lesions |
Surgical and Postoperative Pathology Data
All patients underwent simultaneous single-port thoracoscopic surgery, including 2 patients who underwent bilateral surgery. Three patients underwent lobectomy plus wedge resection, 2 underwent lobectomy plus segmentectomy, 2 underwent combined lobectomy, and 1 underwent single lobectomy. All operations were successful. The mean operation time was 210.76 ± 65.23 mins, the mean intraoperative blood loss was 184.78 ± 82.70 mL, and the mean postoperative hospital stay was 11.72 ± 2.38 days. No severe postoperative complications or deaths occurred. Only 3 patients had different histopathological types, including 1 with minimally invasive adenocarcinoma and invasive adenocarcinoma, 1 with squamous cell carcinoma and invasive adenocarcinoma, and 1 with adenocarcinoma in situ and invasive adenocarcinoma. Apart from the 1 squamous cell carcinoma, all the other lesions were adenocarcinomas. Of the 2 patients with bilateral lesions, 1 underwent systemic lymph node dissection on both sides, and the other only underwent lymph node sampling because the left lesion exhibited pure GGO. The remaining patients underwent systemic lymph node dissection. The mean total number of lymph nodes dissected was 26.17 ± 10.72, the mean number of N1 lymph nodes dissected was 9.59 ± 4.04, and the mean number of N2 lymph nodes dissected was 17.72 ± 7.06. Two patients had N1 metastasis, 4 had both N1 and N2 metastasis, and 2 only had N2 metastasis. Patients with bilateral lesions only had metastases in the right thoracic lymph nodes. Detailed surgical and postoperative pathology data are shown in Table 3.
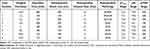 |
Table 3 Surgical and Postoperative Pathology Data |
EGFR Mutations in the 8 Paired Lesions
EGFR detection indicated that 4 patients had completely different mutation types, and 4 had mutations in only 1 tumor. Four lesions had no mutations, and 13 lesions had mutations. L858R was the most common mutation (6/13), followed by 19DEL (3/13), and the rest were rare mutations (two L861Q, one G719X, and one S768I). Details of the EGFR mutations are shown in Table 4.
 |
Table 4 Detail of EGFR Mutation in the 8 Paired Lesions |
Postoperative Treatment and Follow-Up
Details of postoperative treatment and follow-up are shown in Table 5. All 8 patients underwent adjuvant therapy after surgery. One patient underwent chemotherapy, and the rest received tyrosine kinase inhibitor-targeted therapy. As at 15 October 2020, the average follow-up time was 28.68 ± 10.74 months (range 10.5–40.5 months). Only 2 patients had distant metastasis. One patient was found to have brain metastasis 25 months after surgery, and another patient was found to have pleural metastasis 6 months after surgery. All patients remain alive except 1 who died of extensive metastases. The patient who presented with distant metastasis was the same patient who developed N2 skip metastasis.
 |
Table 5 Postoperative Treatment and Follow-Up of Patients |
Discussion
In clinical practice we encountered SMLC patients with postoperative LNM but different EGFR mutations. Such patients can easily be diagnosed with IPM in clinical practice, causing them to miss the best treatment opportunity. In the current study analysis of clinical data derived from these patients indicated that an absence of LNM may not be a necessary criterion for the diagnosis of MPLC with similar tumor pathology.
Differential histopathology remains the first criterion for the diagnosis of MPLC. From the earliest Martini-Melamed criteria2 in 1975, to the Antakli criteria3 in 1995, to the ACCP guidelines6 in 2013, different histopathology types have been used as primary criteria for the diagnosis of MPLC. In this context different histopathology types refers to completely different pathologies, and only one patient (patient 3) in the present study met this condition, with squamous cell carcinoma and adenocarcinoma. With the advancement of imaging technology and the popularization of lung cancer screening, more multiple primary lung adenocarcinomas are being diagnosed and they now account for 40.3%–91.3% of MPLC.15–18 Because there are significant differences in the biological characteristics of lung adenocarcinoma and patient survival associated with different invasive states and different invasive components, the classification of lung adenocarcinoma in 201119 and the World Health Organization classification of lung cancer in 201520 further subclassify lung adenocarcinomas into pre-invasive lesions and invasive lesions. These can be divided into five categories according to the main components of invasion; lepidic, acinar, papillary, micropapillary, and solid. Subsequently, the American Joint Committee on Cancer 8th TNM staging system included the different pathological subtypes of tumors as criteria for the diagnosis of MPLC.21 Although both patient 1 and 7 in the present study had lung adenocarcinomas, the invasive states of their lesions differed. Patient 1 had minimally invasive adenocarcinoma and invasive adenocarcinoma, and patient 7 had adenocarcinoma in situ and invasive adenocarcinoma, so they should also be considered cases of multiple primary lung adenocarcinoma.
As an auxiliary method for the diagnosis of MPLC, genetic analysis can improve the accuracy of diagnosis. Currently the most widely used technique is next-generation sequencing, which shows solid tumors with tens to hundreds of somatic chromosomal rearrangements, single nucleotide variations, and other molecular variations (eg mutations, CNVs, and fusion heterozygosity). Because it is highly sensitive and can provide genomic data even on specimens with relatively low or very low tumor cell counts, it has been widely used in routine clinical practice.22 It can be used to select people suitable for targeted therapy, and it can also identify multiple lung cancers. It is now recognized that cancers with different driver mutations in oncogenes have different clonal origins.23,24 Among them, EGFR and KRAS mutations have proved widely useful for distinguishing SMLC with similar pathological tissue from MPLC or IPM.12 In the current study, EGFR mutation testing was performed on all lesions in 6 patients with the same tumor pathology, and the EGFR mutations in each patient were different, indicating that the patients had different tumor clonal sources. Therefore, in patients with the same tumor pathology and LNM, if the tumor driver mutation is different, the metastasis may be local rather than systemic, and they should be considered to have MPLC.
Differences in the radiological appearances of tumors can be useful for distinguishing MPLC. With the application of low-dose computed tomography and positron emission tomography-computed tomography (PET-CT), more multifocal ground glass/lepidic lung cancers are being diagnosed. Multifocal ground glass/lepidic lung cancer exhibits GGO on CT scanning, or appears as lepidic cancer on pathology.21,25,26 Multifocal ground glass/lepidic lung cancers, including adenocarcinoma in situ, minimally invasive adenocarcinoma, and lepidic-predominant adenocarcinoma are all considered to be independent primary tumors.27–29 Matsunaga et al30 concluded that multifocal lung cancer with at least one GGO should be diagnosed as MPLC due to its favorable prognosis. In addition, PET-CT can distinguish MPLC from IPM based on the difference or ratio of standard uptake values between tumors in each patient.31,32 Notably however, it may not be sufficient to rely solely on PET-CT or CT to identify MPLC. Suh et al33 established a new method for the diagnosis of MPLC by combining the standard uptake value from PET-CT with the radiological features on CT, including GGO, spicule sign, and air-bronchogram. MPLCs are diagnosed when any tumor with pure GGO or GGO-dominant features in present, or when both tumors have spiculation or air-bronchogram, or when only one tumor has spiculation or air-bronchogram but tumors have more than two grades of standard uptake values. This method could have been used in the patients in the current study to verify whether they were considered to have multiple primary lung cancers. Of the 8 patients in this study 5 had at least one GGO lesion, and the 3 patients whose lesions were all solid nodules also had spiculation or air-bronchogram on CT.
Surgery is still the first choice for the treatment of MPLC. Because most MPLC is diagnosed at an early stage, surgery should be the preferred treatment.34 Targeted therapy and immunotherapy have achieved promising results in patients with advanced non-small cell lung cancer,35,36 but there is still insufficient clinical evidence on whether these two therapies can be applied in patients with MPLC. In one study approximately 45% of MPLC manifesting as GGOs had EGFR mutations.37 Therefore, targeted therapy may be a treatment option in inoperable MPLC patients with EGFR mutations. Traditional chemotherapy should be considered in patients with LNM. All the patients in the present study underwent targeted therapy after surgery. Because all patients with MPLC have EGFR mutations, targeted therapy may be more suitable for them. All patients survived except 1, who died from extensive pleural metastasis. Therefore, for MPLC with LNM, comprehensive treatment based on surgery should be the first choice.
In conclusion, the diagnosis of MPLC should be based on detailed evaluation of all available information from multiple oncology-related disciplines, rather than relying merely on clinicopathological features. EGFR mutation testing is extremely important in patients in whom MPLC is suspected, especially in patients with LNM. SPLC with LNM but with different EGFR mutations should be considered MPLC rather than IPM. Comprehensive treatment based on surgery may be preferable in these patients because it is associated with a good prognosis.
Funding
This work was supported by the Tongji Hospital Clinical Research Flagship Program (No.2019CR107).
Disclosure
None of the authors have any potential conflicts of interest.
References
1. Ferguson MK, DeMeester TR, DesLauriers J, et al. Diagnosis and management of synchronous lung cancers. J Thorac Cardiovasc Surg. 1985;89(3):378–385. doi:10.1016/S0022-5223(19)38787-2
2. Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975;70(4):606–612. doi:10.1016/S0022-5223(19)40289-4
3. Antakli T, Schaefer RF, Rutherford JE, et al. Second primary lung cancer. Ann Thorac Surg. 1995;59(4):863–867. doi:10.1016/0003-4975(95)00067-u
4. Detterbeck FC, Jones DR, Kernstine KH, et al. Special treatment issues. Chest. 2003;123(1):244S–258S. doi:10.1378/chest.123.1_suppl.244s
5. Shen KR, Meyers BF, Larner JM, et al. Special treatment issues in lung cancer - ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(3):290S–305S. doi:10.1378/chest.07-1382
6. Kozower BD, Larner JM, Detterbeck FC, et al. Special treatment issues in non-small cell lung cancer-diagnosis and management of lung cancer, 3rd ed: American College of Chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5):e369S–e399S. doi:10.1378/chest.12-2362
7. Chang YL, Wu CT, Lin SC, et al. Clonality and prognostic implications of p53 and epidermal growth factor receptor somatic aberrations in multiple primary lung cancers. Clin Cancer Res. 2007;13(1):52–58. doi:10.1158/1078-0432.CCR-06-1743
8. Arai J, Tsuchiya T, Oikawa M, et al. Clinical and molecular analysis of synchronous double lung cancers. Lung Cancer. 2012;77(2):281–287. doi:10.1016/j.lungcan.2012.04.003
9. Murphy SJ, Aubry MC, Harris FR, et al. Identification of independent primary tumors and intrapulmonary metastases using DNA rearrangements in non-small-cell lung cancer. J Clin Oncol. 2014;32(36):4050–4058. doi:10.1200/JCO.2014.56.7644
10. Asmar R, Sonett JR, Singh G, et al. Use of oncogenic driver mutations in staging of multiple primary lung carcinomas: a single-center experience. J Thorac Oncol. 2017;12(10):1524–1535. doi:10.1016/j.jtho.2017.06.012
11. Murphy SJ, Harris FR, Kosari F, et al. Using genomics to differentiate multiple primaries from metastatic lung cancer. J Thorac Oncol. 2019;14(9):1567–1582. doi:10.1016/j.jtho.2019.05.008
12. Zheng R, Shen Q, Mardekian S, et al. Molecular profiling of key driver genes improves staging accuracy in multifocal non-small cell lung cancer. J Thorac Cardiovasc Surg. 2020;160(2):e71–e79. doi:10.1016/j.jtcvs.2019.11.126
13. Wang Q, Cai YX, Deng Y, et al. Modular 3-cm uniportal video-assisted thoracoscopic left upper lobectomy with systemic lymphadenectomy. J Thorac Dis. 2016;8(8):2264–2268. doi:10.21037/jtd.2016.03.15
14. Qu R, Hao Z, Zhang Y, et al. Single-center experience of simultaneous bilateral uni-portal video-assisted thoracoscopic surgery for multiple ground-glass opacities. J Cardiothorac Surg. 2020;15(1):69. doi:10.1186/s13019-020-01107-0
15. Chang YL, Wu CT, Lee YC. Surgical treatment of synchronous multiple primary lung cancers: experience of 92 patients. J Thorac Cardiovasc Surg. 2007;134(3):630–637. doi:10.1016/j.jtcvs.2007.06.001
16. De Leyn P, Moons J, Vansteenkiste J, et al. Survival after resection of synchronous bilateral lung cancer. Eur J Cardiothorac Surg. 2008;34(6):1215–1222. doi:10.1016/j.ejcts.2008.07.069
17. Finley DJ, Yoshizawa A, Travis W, et al. Predictors of outcomes after surgical resection of synchronous primary lung cancers. J Thorac Oncol. 2010;5(2):197–205. doi:10.1097/JTO.0b013e3181c814c5
18. Tsunezuka Y, Matsumoto I, Tamura M, et al. The results of therapy for bilateral multiple primary lung cancers: 30 years experience in a single centre. Eur J Surg Oncol. 2004;30(7):781–785. doi:10.1016/j.ejso.2004.05.008
19. Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6(2):244–285. doi:10.1097/JTO.0b013e318206a221
20. Travis WD, Brambilla E, Nicholson AG, et al. The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10(9):1243–1260. doi:10.1097/JTO.0000000000000630
21. Rami-Porta RAH, Travis WD, Rusch VW. AJCC Cancer Staging Manual. Vol. 8. France: Springer International Publishing; 2017.
22. Chuang JC, Shrager JB, Wakelee HA, et al. Concordant and discordant EGFR mutations in patients with multifocal adenocarcinomas: implications for EGFR-targeted therapy. Clin Ther. 2016;38(7):1567–1576. doi:10.1016/j.clinthera.2016.06.005
23. Lau DH, Yang B, Hu R, et al. Clonal origin of multiple lung cancers: k-ras and p53 mutations determined by nonradioisotopic single-strand conformation polymorphism analysis. Diagn Mol Pathol. 1997;6(4):179–184. doi:10.1097/00019606-199708000-00001
24. Matsuzoe D, Hideshima T, Ohshima K, et al. Discrimination of double primary lung cancer from intrapulmonary metastasis by p53 gene mutation. Br J Cancer. 1999;79(9–10):1549–1552. doi:10.1038/sj.bjc.6690247
25. Detterbeck FC, Franklin WA, Nicholson AG, et al. The IASLC lung cancer staging project: background data and proposed criteria to distinguish separate primary lung cancers from metastatic foci in patients with two lung tumors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(5):651–665. doi:10.1016/j.jtho.2016.01.025
26. Detterbeck FC, Nicholson AG, Franklin WA, et al. The IASLC lung cancer staging project: summary of proposals for revisions of the classification of lung cancers with multiple pulmonary sites of involvement in the forthcoming eighth edition of the TNM classification. J Thorac Oncol. 2016;11(5):639–650. doi:10.1016/j.jtho.2016.01.024
27. Park E, Ahn S, Kim H, et al. Targeted sequencing analysis of pulmonary adenocarcinoma with multiple synchronous ground-glass/lepidic nodules. J Thorac Oncol. 2018;13(11):1776–1783. doi:10.1016/j.jtho.2018.07.097
28. Ren YJ, Huang SJ, Dai CY, et al. Germline predisposition and copy number alteration in pre-stage lung adenocarcinomas presenting as ground-glass nodules. Front Oncol. 2019;9:288. doi:10.3389/fonc.2019.00288
29. Zhang Y, Li G, Li Y, et al. Imaging features suggestive of multiple primary lung adenocarcinomas. Ann Surg Oncol. 2020;27(6):2061–2070. doi:10.1245/s10434-019-08109-w
30. Matsunaga T, Suzuki K, Takamochi K, et al. New simple radiological criteria proposed for multiple primary lung cancers. Jpn J Clin Oncol. 2017;47(11):1073–1077. doi:10.1093/jjco/hyx113
31. Dijkman BG, Schuurbiers OCJ, Vriens D, et al. The role of 18F-FDG PET in the differentiation between lung metastases and synchronous second primary lung tumours. Eur J Nucl Med Mol Imaging. 2010;37(11):2037–2047. doi:10.1007/s00259-010-1505-2
32. Liu Y, Tang Y, Xue Z, et al. SUVmax ratio on PET/CT may differentiate between lung metastases and synchronous multiple primary lung cancer. Acad Radiol. 2020;27(5):618–623. doi:10.1016/j.acra.2019.07.001
33. Suh YJ, Lee HJ, Sung P, et al. A novel algorithm to differentiate between multiple primary lung cancers and intrapulmonary metastasis in multiple lung cancers with multiple pulmonary sites of involvement. J Thorac Oncol. 2020;15(2):203–215. doi:10.1016/j.jtho.2019.09.221
34. Chen T-F, Xie C-Y, Rao B-Y, et al. Surgical treatment to multiple primary lung cancer patients: a systematic review and meta-analysis. BMC Surg. 2019;19(1):185. doi:10.1186/s12893-019-0643-0
35. Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non-small cell lung cancer: a review. JAMA. 2019;322(8):764–774. doi:10.1001/jama.2019.11058
36. Proto C, Ferrara R, Signorelli D, et al. Choosing wisely first line immunotherapy in non-small cell lung cancer (NSCLC): what to add and what to leave out. Cancer Treat Rev. 2019;75:39–51. doi:10.1016/j.ctrv.2019.03.004
37. Wu CY, Zhao C, Yang Y, et al. High discrepancy of driver mutations in patients with NSCLC and synchronous multiple lung ground-glass nodules. J Thorac Oncol. 2015;10(5):778–783. doi:10.1097/JTO.0000000000000487
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
