Back to Journals » Journal of Pain Research » Volume 16
Study of the Distribution of Lumbar Modic Changes in Patients with Low Back Pain and Correlation with Lumbar Degeneration Diseases
Received 15 July 2023
Accepted for publication 27 October 2023
Published 6 November 2023 Volume 2023:16 Pages 3725—3733
DOI https://doi.org/10.2147/JPR.S430792
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Baixing Wei, Han Wu
Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun, Jilin, People’s Republic of China
Correspondence: Han Wu, Department of Orthopedics, China-Japan Union Hospital of Jilin University, No. 126 Xi’antai Avenue, Changchun, Jilin, People’s Republic of China, Tel +86 43189876902, Email [email protected]
Purpose: To study the distribution of lumbar Modic changes (MC) in low back pain patients, and to explore the relationship between Modic changes and age, gender, segment and lumbar degeneration diseases (disc degeneration, spinal stenosis, lumbar spondylolisthesis).
Patients and Methods: Modic changes were counted and analysed in 500 randomly selected patients who visited the outpatient clinic for lumbar spine MRI for low back pain from 2019 to 2022. The relationship between Modic changes and bulging disc, protrusion, extrusion, sequestration, Schmorl’s node, spinal stenosis, and lumbar spondylolisthesis was studied. Data correlations were compared using the chi-square test, P< 0.05 was considered a statistically significant difference.
Results: Modic changes were present in 184 segments. 58 were type I, 119 were type II, and 7 were type III. The number of Modic changes segments in L1-2, L2-3, L3-4, L4-5, and L5-S1 was 10, 22, 22, 58, and 72, respectively. Modic changes by gender occurred in 44 males and 82 females, and by age grouping were 0 cases in 10– 19 years, 3 cases in 20– 29 years, 6 cases in 30– 39 years, 41 cases in 40– 49 years, 64 cases in 50– 59 years, 38 cases in 60– 69 years, 15 cases in 70– 79 years, and 5 cases in 80– 89 years, respectively. Modic changes occurred in 56 with bulging disc, 45 with Protrusion, 57 with Extrusion and Sequestration, 32 with Schmorl’s node, 32 with spondylolisthesis, and 56 with stenosis. Modic changes correlated with all of the above factors except bulging disc, and all differences were statistically significant (P< 0.05).
Conclusion: The most common type of Modic changes is type II; Modic changes have correlation with age, gender, segment, lumbar disc herniation, lumbar spondylolisthesis, and lumbar spinal stenosis, and are a very important factor in low back pain.
Keywords: low back pain, Modic changes, disc degeneration, spinal stenosis, lumbar spondylolisthesis
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Kovacs has been published for this article.
Introduction
Low back pain (LBP) is anatomically defined as pain extending from the 12th rib to the iliac crest.1 Degenerative diseases of the lumbar spine are the most common causes of low back pain. Anatomically, disc degeneration, radicular pain, facet arthropathy, and myofascial pain can be used as its pathogenesis. Etiologically, the most common is degenerative lumbar spine pathology.1 Modic changes are changes in the spinal endplate and subendplate bones on MRI and are seen as a spinal degeneration and an etiology of low back pain. It was first reported by De Roos in 1987,2 and later by Modic in 1988, who described the types of signal changes, typing criteria and pathological changes on MRI,3 The etiology of Modic changes is unknown, and most of the current studies are limited to epidemiological and clinical correlations, and there are no consistent conclusions yet. Specifically, Modic changes are pathological changes that occur when the protective effect of the cartilage endplate is weakened or lost, leading to oedema of the adjacent cancellous bone, followed by fatty infiltration of the vertebral body, and ultimately fibrosis and calcification.2 This continuous pathological process divides Modic changes into three types (I, II, III).3 The above pathologies appear to be causally related to common lumbar spine disorders (lumbar disc degeneration, lumbar spondylolisthesis, lumbar spinal stenosis, etc.). However, there have been few comprehensive studies involving large sample sizes on the relationship between the above. There is still controversy over the results of the studies. Therefore, there is a need for research on this topic.
Materials and Methods
Ethics and Patient Consent
This study was approved by the Ethics Committee of the China–Japan Union Hospital of Jilin University and was also in accordance with the Declaration of Helsinki. All the patients provided written informed consent in this study.
Materials
Outpatients who had MRI and X-ray examinations for low back pain between 2019 and 2022 were randomly selected for inclusion in the study. Patients with MRI presentation of tumor, fracture, tuberculosis, or infection were excluded.4–6
Diagnosis of Low Back Pain
Low back pain refers to nonspecific pain extending from the 12th rib to the iliac crest, with or without low leg pain.1
Definition and Typing of Modic Changes in MRI
Type 0: normal signal; type I: T1 low signal, T2 high signal; type II: T1 high signal, T2 equal signal or mild high signal; type III: T1 and T2 both low signal3 (Figure 1).
Assessment of the Type of Disc Degeneration
Degree of disk herniation according to the lumbar disk pathologic classification of the North American Spine Society.7 Bulging disc: The presence of disc tissue extending beyond the edges of the ring apophyses. Protrusion: The greatest distance between the edges of the disc material presenting outside the disc space is less than the distance between the edges of the base of that disc material extending outside of the disc space. Extrusion: The distance between the edges of the disc material outside the disc space is greater than the distance between the base edges, or when there is no continuity between the disc material within and beyond the disc space. Sequestration: The displaced disc material has lost completely any continuity with the parent disc. Schmorl’s node: Herniated discs in the vertical direction (Figure 2).
Assessment of Lumbar Spondylolisthesis
Radiologically visible anterior displacement of a vertebral body over an adjacent vertebral body without associated disruption or defect of the vertebral ring. The vertebral body is divided into four parts along the longitudinal axis and divided into four types: I, II, III, IV.8 However, only type I and II were found in our patients (Figure 3).
 |
Figure 3 Lumbar spondylolisthesis (only type I and II were found in our patients). (A) type I spondylolisthesis, (B) type II spondylolisthesis. |
Assessment of Lumbar Spinal Stenosis
Measures for central stenosis were antero-posterior diameter (<10mm) and cross-sectional area (<70mm2) of spinal canal. A lateral recess length ≤2 mm or a lateral recess angle <30° were described as diagnostic for lateral recess stenosis9 (Figure 4).
Statistical Methods
Statistical analyses were performed using SPSS 25.0 software (IBM Corporation, Armonk, New York, USA). The different variables were tabulated, and the percentage of counts was expressed as a percentage. The chi-square test was applied in determining the correlation of the categorical variables (Pearson chi-square test was used when the sample content was ≥40 and each frequency was ≥5; corrected chi-square test was used when the sample content was ≥40 and there was 1 ≤frequency <5; and Fisher’s exact test was used when the sample content was <40 or the frequency was <1). P<0.05 is considered a statistically significant difference.
Results
Fundamental Information
Of the 500 outpatients randomly selected, 25 patients with a diagnosis of lumbar spine tumor, tuberculosis, or infection were excluded, and 126 (26.5%) patients had 184 (7.7%) segment Modic changes out of 2375 disc segments in 475 patients.
Of the 184 Modic changes segments, there were 58 type I, 119 type II, and 7 type III. The number of Modic changes segments for L1-2, L2-3, L3-4, L4-5, and L5-S1 was 10, 22, 22, 58, 72, respectively. There was an increasing trend, and the difference was statistically significant (P<0.05) (Table 1).
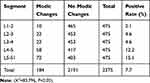 |
Table 1 Characteristics of Modic Changes Distribution |
Modic changes were not found in the 10–19 years group, 3 cases in the 20–29 years group, 6 cases in the 30–39 years group, 18 cases in the 40–49 years group, 41 cases in the 50–59 years group, 38 cases in the 60–69 years group, 15 cases in the 70–79 years group, and 5 cases in the 80–89 years group. There was also an increasing trend, and the difference was statistically significant (P<0.05) (Table 2).
 |
Table 2 Characteristics of Modic Changes in Age |
The prevalence of Modic changes was 21.1% in men and 30.8% in women, with a statistically significant difference between the two groups (P<0.05) (Table 3).
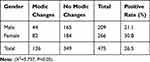 |
Table 3 Association Between Gender and Modic Change |
Relationship Between Modic Changes and Lumbar Disc Degeneration
Total lumbar disc degeneration: Bulging disc in 759 cases, protrusion in 443 cases, extrusion and sequestration in 138 cases, and Schmorl’s node in 150 cases. (Due to the too small quantity of Sequestration, we put Extrusion and Sequestration in one group for the convenience of the study) Lumbar disc degeneration combined with Modic changes: Bulging disc in 56 cases, protrusion in 45 cases, extrusion and sequestration in 57 cases, and Schmorl’s node in 32 cases (Table 4).
 |
Table 4 Distribution Characteristics of Modic Changes Combined with Spinal Degeneration |
In terms of P-value, Modic changes correlated significantly (P<0.05) with protrusion, extrusion and sequestration, and Schmorl’s node, showing that Modic changes increase the probability of the above (Tables 5–8).
 |
Table 5 Association of Bulging Disc with Modic Changes |
 |
Table 6 Association of Protrusion with Modic Changes |
 |
Table 7 Association of Extrusion and Sequestration with Modic Changes |
 |
Table 8 Association of Schmorl’s Node with Modic Changes |
Relationship Between Modic Changes and Lumbar Spondylolisthesis
There were a total of 98 segments of lumbar spondylolisthesis, of which 88 were type I, 10 were type II, and type III and IV were not found. For the convenience of the study, we had to conduct the study without typing. The number of segments with lumbar spondylolisthesis combined with Modic changes was 32 (Table 4). There is a strong correlation between lumbar spondylolisthesis and Modic changes (P<0.05) (Table 9).
 |
Table 9 Association of Spondylolisthesis with Modic Changes |
Relationship Between Modic Changes and Lumbar Spinal Stenosis
There were a total of 248 segments with lumbar spinal stenosis, and 56 segments with concurrent Modic changes (Table 4). There is a strong correlation between lumbar spinal stenosis and Modic changes (P<0.05) (Table 10).
 |
Table 10 Association of Stenosis with Modic Changes |
Discussion
Previous studies have shown that the prevalence of Modic changes in patients with low back pain ranges from 18% to 58%.3,10,11 Modic changes tend to occur more often in the discs of patients who are older, have low segments, and are most commonly type II.12 Our study is in agreement with these studies. Karchevsky11 proved that men had a greater incidence of Modic changes than women, which is different from our study.
Herlin found that Modic changes showed a strong correlation with low back pain when the grade of disc degeneration increased.13 For lumbar disc herniation, Xiao found that as the grade of L3-L5 disc degeneration increased, the probability of Modic changes in the adjacent endplates of the L3-L5 vertebral body increased.14 As for Schmorl’s node, after the cartilage endplate and adjacent bone marrow changes have caused Modic changes, there is a higher probability of the disc herniating vertically.
Arana’s study showed a strong correlation between L5-S1 spondylolisthesis and Modic changes.15 Hayashi found that disc degeneration and angular motion of lumbar spondylolisthesis were related to Modic changes, with Modic type II lumbar spondylolisthesis being the most severe and type III being the least severe. This may be related to the poor stability of the yellow bone marrow in type II and the sclerosis of the yellow bone marrow fibrosis in type III.16
Although both spinal stenosis and Modic changes can be the cause of low back pain.17 However, Carragee’s study showed that Modic changes were not strongly correlated with low back pain and lumbar spinal stenosis.18 In addition, Modic changes have no significant influence on clinical outcome parameters in patients with lumbar spinal stenosis compared to patients without MCs, independent of the chosen surgical strategy.19 Our study concluded that the two are correlated in part because it did not distinguish between hypertrophy of the ligamentum flavum and developmental stenosis of the spinal canal and stenosis due to disc herniation.
While the above are only studies of a single disease with Modic changes, or only a certain subtype of Modic changes, our study involves a large, comprehensive, and general study of a large sample. Thus, in conjunction with our conclusions, we review previous studies and propose some assumptions.
We speculated that lumbar degeneration (disc degeneration, spondylolisthesis, and stenosis), and Modic changes may be causally related, with the pathological process of Modic changes destabilising the intervertebral space and stress changes caused by degeneration exacerbating the Modic changes.
Currently, non-surgical treatments for simple Modic changes include antibiotics,20 zoledronic acid,21,22 intradiscal glucocorticoids, or lidocaine injection.23,24 Surgical treatments are common with Basivertebral Nerve Ablation,25 and rarely fusion. Studies have shown that Modic changes are a risk factor for recurrence of lumbar disc herniation after endoscopic lumbar discectomy.26,27 This is due to the simple removal of the disc without treatment of the diseased cartilaginous endplates. In addition, lumbar spine surgery may promote the development of Modic changes,28 especially nonfusion surgery.29 Therefore, in conjunction with our findings, we believe that fusion should be elevated in priority when Modic changes are combined with disc degeneration, spondylolisthesis, and stenosis.
The pathology of Modic changes is closely related to inflammation.30 In conjunction with this study, more aggressive anti-inflammatory therapy should be given to patients with simple Modic changes. This may slow or stop the development of Modic changes, thereby reducing the incidence of disc degeneration, spondylolisthesis, and stenosis, and to some extent avoiding the possibility of future fusion surgery.
In addition, Modic changes impede lumbar functional recovery from surgery and can even exacerbate postoperative related symptoms.31,32 This is because inflammation is also present in the vertebral body, so postoperative treatment targeting Modic changes deserves more attention.
The above inferences based on the results could be helpful in low back pain management. Due to the complexity of the conditions of the outpatients and the variety of treatments and duration, the inferences would have to be confirmed by selecting a new population for the study. This is a limitation of this study. In addition, a more detailed analysis of Modic changes typing in relation to degeneration and pain levels was not possible due to the different duration of disease in each individual and the difficulty of conducting retrospective follow-up.
Conclusion
The most common type of Modic changes is type II; Modic changes have correlation with age, gender, segment, lumbar disc herniation, lumbar spondylolisthesis, and lumbar spinal stenosis and are a very important factor in low back pain.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the hospital.
Acknowledgments
We would like to thank all the participants in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare no conflict of interest.
References
1. Knezevic N, Candido K, Vlaeyen J, Van Zundert J, Cohen S. Low back pain. Lancet. 2021;398(10294):78–92. doi:10.1016/s0140-6736(21)00733-9
2. de Roos A, Kressel H, Spritzer C, Dalinka M. MR imaging of marrow changes adjacent to end plates in degenerative lumbar disk disease. AJR Am J Roentgenol. 1987;149(3):531–534. doi:10.2214/ajr.149.3.531
3. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–199. doi:10.1148/radiology.166.1.3336678
4. Resnick D, Niwayama G. Intervertebral disc abnormalities associated with vertebral metastasis: observations in patients and cadavers with prostatic cancer. Invest Radiol. 1978;13(3):182–190. doi:10.1097/00004424-197805000-00002
5. Schwarz-Nemec U, Friedrich K, Stihsen C, et al. Vertebral bone marrow and endplate assessment on MR imaging for the differentiation of Modic type 1 endplate changes and infectious spondylodiscitis. J Clin Med. 2020;9(3):826. doi:10.3390/jcm9030826
6. Kuisma M, Karppinen J, Niinimäki J, et al. A three-year follow-up of lumbar spine endplate (Modic) changes. Spine. 2006;31(15):1714–1718. doi:10.1097/01.brs.0000224167.18483.14
7. Fardon D, Williams A, Dohring E, Murtagh F, Gabriel Rothman S, Sze G. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014;14(11):2525–2545. doi:10.1016/j.spinee.2014.04.022
8. Matz P, Meagher R, Lamer T, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16(3):439–448. doi:10.1016/j.spinee.2015.11.055
9. Steurer J, Roner S, Gnannt R, Hodler J. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC Musculoskelet Disord. 2011;12:175. doi:10.1186/1471-2474-12-175
10. Kuisma M, Karppinen J, Niinimäki J, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine. 2007;32(10):1116–1122. doi:10.1097/01.brs.0000261561.12944.ff
11. Karchevsky M, Schweitzer M, Carrino J, Zoga A, Montgomery D, Parker L. Reactive endplate marrow changes: a systematic morphologic and epidemiologic evaluation. Skeletal Radiol. 2005;34(3):125–129. doi:10.1007/s00256-004-0886-3
12. Jensen T, Bendix T, Sorensen J, Manniche C, Korsholm L, Kjaer P. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet Disord. 2009;10:81. doi:10.1186/1471-2474-10-81
13. Herlin C, Kjaer P, Espeland A, et al. Modic changes-their associations with low back pain and activity limitation: a systematic literature review and meta-analysis. PLoS One. 2018;13(8):e0200677. doi:10.1371/journal.pone.0200677
14. Xiao L, Ni C, Shi J, et al. Analysis of correlation between vertebral endplate change and lumbar disc degeneration. Med Sci Monit. 2017;23:4932–4938. doi:10.12659/msm.904315
15. Arana E, Kovacs F, Royuela A, et al. Modic changes and associated features in Southern European chronic low back pain patients. Spine J. 2011;11(5):402–411. doi:10.1016/j.spinee.2011.03.019
16. Hayashi T, Daubs M, Suzuki A, et al. Motion characteristics and related factors of Modic changes in the lumbar spine. J Neurosurg Spine. 2015;22(5):511–517. doi:10.3171/2014.10.Spine14496
17. van der Graaf J, Kroeze R, Buckens C, Lessmann N, van Hooff M. MRI image features with an evident relation to low back pain: a narrative review. Eur Spine J. 2023;32(5):1830–1841. doi:10.1007/s00586-023-07602-x
18. Carragee E, Alamin T, Miller J, Carragee J. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5(1):24–35. doi:10.1016/j.spinee.2004.05.250
19. Ulrich N, Burgstaller J, Gravestock I, et al. The influence of endplate (Modic) changes on clinical outcomes in lumbar spinal stenosis surgery: a Swiss prospective multicenter cohort study. Eur Spine J. 2020;29(9):2205–2214. doi:10.1007/s00586-020-06364-0
20. Albert H, Manniche C, Sorensen J, Deleuran B. Antibiotic treatment in patients with low-back pain associated with Modic changes type 1 (bone oedema): a pilot study. Br J Sports Med. 2008;42(12):969–973. doi:10.1136/bjsm.2008.050369
21. Koivisto K, Kyllönen E, Haapea M, et al. Efficacy of zoledronic acid for chronic low back pain associated with Modic changes in magnetic resonance imaging. BMC Musculoskelet Disord. 2014;15:64. doi:10.1186/1471-2474-15-64
22. Cai G, Laslett L, Aitken D, et al. Effect of zoledronic acid and denosumab in patients with low back pain and modic change: a proof-of-principle trial. J Bone Miner Res. 2018;33(5):773–782. doi:10.1002/jbmr.3376
23. Cao P, Jiang L, Zhuang C, et al. Intradiscal injection therapy for degenerative chronic discogenic low back pain with end plate Modic changes. Spine J. 2011;11(2):100–106. doi:10.1016/j.spinee.2010.07.001
24. Tavares I, Thomas E, Cyteval C, et al. Intradiscal glucocorticoids injection in chronic low back pain with active discopathy: a randomized controlled study. Ann Phys Rehabil Med. 2021;64(2):101396. doi:10.1016/j.rehab.2020.05.003
25. Schnapp W, Martiatu K, Delcroix GJ. Basivertebral nerve ablation for the treatment of chronic low back pain: a scoping review of the literature. Pain Physician. 2022;25(4):E551–E562.
26. Ono K, Ohmori K, Yoneyama R, Matsushige O, Majima T. Risk factors and surgical management of recurrent herniation after full-endoscopic lumbar discectomy using interlaminar approach. J Clin Med. 2022;11(3):748. doi:10.3390/jcm11030748
27. Luo M, Wang Z, Zhou B, et al. Risk factors for lumbar disc herniation recurrence after percutaneous endoscopic lumbar discectomy: a meta-analysis of 58 cohort studies. Neurosurg Rev. 2023;46(1):159. doi:10.1007/s10143-023-02041-0
28. El Barzouhi A, Vleggeert-Lankamp C, van der Kallen B, et al. Back pain’s association with vertebral end-plate signal changes in sciatica. Spine J. 2014;14(2):225–233. doi:10.1016/j.spinee.2013.08.058
29. Mu X, Kim SW, Uhl E, Scholler K. The effects of lumbar fusion and non-fusion surgery on the development of Modic changes. J Orthop Surg Res. 2022;17(1):89. doi:10.1186/s13018-022-02971-3
30. Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes, possible causes and relation to low back pain. Med Hypotheses. 2008;70(2):361–368. doi:10.1016/j.mehy.2007.05.014
31. Xu J, Li Y, Wang B, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation with Modic changes via a transforaminal approach: a retrospective study. Pain Physician. 2019;22(6):E601–E608.
32. Takahashi H, Aoki Y, Inoue M, et al. Characteristics of relief and residual low back pain after discectomy in patients with lumbar disc herniation: analysis using a detailed visual analog scale. BMC Musculoskelet Disord. 2021;22(1):167. doi:10.1186/s12891-021-04015-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



