Back to Journals » Infection and Drug Resistance » Volume 16
Strain Identification and Drug Resistance Analysis of Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry in Nontuberculous Mycobacterial Lung Disease
Authors Shi J, Gao G, Pan J, Wu LP, Ning H, Wu Z, Ye X, Jiang X
Received 20 January 2023
Accepted for publication 14 April 2023
Published 17 July 2023 Volume 2023:16 Pages 4635—4643
DOI https://doi.org/10.2147/IDR.S405563
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jichan Shi,1,* Gexin Gao,2,* Jing Pan,3 Lian-Peng Wu,4 Hongye Ning,1 Zhengxin Wu,1 Xinchun Ye,1 Xiangao Jiang1
1Department of Infectious Disease, The Theorem Clinical College of Wenzhou Medical University, Wenzhou Central Hospital, Wenzhou, People’s Republic of China; 2Department of Nursing, Wenzhou Medical University, Wenzhou, People’s Republic of China; 3Department of Geriatric Medicine, The Theorem Clinical College of Wenzhou Medical University, Wenzhou Central Hospital, Wenzhou, People’s Republic of China; 4Department of Laboratory, The Dingli Clinical Institute of Wenzhou Medical University, Wenzhou Central Hospital, Wenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiangao Jiang, Department of Infectious Disease, The Theorem Clinical College of Wenzhou Medical University, Wenzhou Central Hospital, 252 BaiLiDong Road, Wenzhou, Zhejiang, 325000, People’s Republic of China, Tel +86 13676788085, Email [email protected]
Objective: To evaluate the clinical value of matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) in detecting Nontuberculous mycobacteria (NTM).
Methods: The clinical data of 172 patients with suspected NTM lung disease were collected from our hospital from January 1, 2018, to December 30, 2021. The results were compared with those of BACTEC MGIT 960 in liquid culture and gene chip. This study also utilised MALDI-TOF MS to detect macrolide (MA) and amikacin (Am) mutations.
Results: One hundred thirty-seven cases of NTM pulmonary disease were confirmed by identifying the NTM gene chip in bronchoalveolar lavage fluid and/or MALDI-TOF MS detection. The positive predictive value and negative predictive value were 100% (131/131) and 85.37% (35/41), respectively, and the consistency of the two methods was high (kappa=0.899). For the drug resistance detection of MAs, the consistency rate between MALDI-TOF MS detection and drug sensitivity detection was 97.71% (128/131), the sensitivity was 81.25% (13/16) and the specificity was 100% (115/115). The positive and negative predictive values were 100% (13/13) and 93.75% (115/118), respectively. There was no coincidental consistency between the two methods, and the consistency was high (P< 0.001, kappa=0.884). For the drug resistance test of Am, the consistency rate between the MALDI-TOF MS test and the drug sensitivity test was 93.13% (122/131), the sensitivity was 93.52% (101/108), the specificity was 90.91% (21/23) and the positive predictive value and negative predictive value were 98.06% (101/103) and 75.00% (21/28), respectively. The two methods had high consistency, and the consistency was not coincidental (P< 0.001, kappa=0.781).
Conclusion: Utilising MALDI-TOF MS has a good consistency with the drug resistance gene chip method and can be a rapid and effective method to identify strains and drug resistance of NTM. Therefore, it has certain clinical application value in patients with suspected NTM lung disease.
Keywords: Nontuberculosis mycobacteria, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry, strain identification, resistance
Introduction
The name Nontuberculous mycobacteria (NTM) refers to mycobacteria other than Mycobacterium tuberculosis complex (tuberculous mycobacterium, MTBC) and Mycobacterium leprae, which are widely present in nature and belong to opportunistic pathogens.1 They can cause disease in various systems, including the respiratory tract, digestive tract, skin and mucous membranes. An infection of the human body with NTM is called NTM disease, which causes lesions of related tissues and organs.2 In recent years, global NTM disease has rapidly increased and has become a major public health problem.3 It is also one of China’s rising public health concerns, with more NTM pulmonary disease observed in south and coastal China.4 My country has not yet formed a unified scheme for identifying NTM, which mainly relies on molecular detection technology; there is a great deal of controversy over the primers used. For some rare NTMs, whole-genome sequencing is required for identification.5,6 In addition, NTM lung disease and tuberculosis are very similar in clinical and imaging manifestations,7 increasing the misdiagnosis rate. Therefore, finding new etiological detection methods, improving the identification of NTM, and the ability to diagnose drug resistance would result in earlier diagnosis and treatment, reducing the amount of damage NTM disease does to the human body.
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) was first used to identify mycobacteria in 2004. The use of MALDI-TOF MS in the analysis of oligonucleotides is a new approach and has developed rapidly in recent years. Compared with traditional identification methods, MALDI-TOF MS simplifies the identification process, shortens the identification time and has the advantages of accuracy, rapidity, sensitivity and high throughput.8 This study evaluated the clinical value of MALDI-TOF MS in detecting NTM compared with the BACTEC MGIT 960 liquid culture system and gene chip.
Materials and Methods
General Information
The clinical data of 172 patients with suspected NTM lung disease who visited Wenzhou Central Hospital, a tertiary Class A general hospital, from January 1, 2018, to December 30, 2021, were collected. All subjects met the diagnostic criteria for suspected NTM lung disease formulated by the Tuberculosis Branch of the Chinese Medical Association.9 Inclusion criteria (one of the following conditions was sufficient): (1) The sputum test for acid-fast bacilli was positive, and the clinical manifestations were inconsistent with pulmonary tuberculosis; (2) Those with positive acid-fast bacilli in sputum or other specimens and negative in molecular biology of MTBC; (3) Patients for whom regular anti-tuberculosis treatment was ineffective and repeatedly excreted bacteria; and whose lung lesions were mainly bronchiectasis, multiple small nodules or thin-walled cavities.
At the same time, two bronchoalveolar lavage fluid (BALF) specimens from each patient were collected. All patients signed informed consent forms, and the research protocol was approved by the hospital’s medical ethics committee (ethics approval ID: L2021-03-083).
Method
Flow charts provided quick access to relevant information (Figure 1).
 |
Figure 1 The flow chart of research. |
Gene Chip Testing
The BALF specimens were identified using the Boao gene chip method.10 The length of the 16S rRNA primer was about 1500 bp, the upstream primer was 5’-AGTTTGATCCTGGCTCAG-3’ and the downstream primer was 5’-GGTTACCTTGTTACGACTT-3’. The length of the hsp65 primer was 441 bp, the upstream primer was 5’-ACCAACGATGGTGT-GTCCAT-3’ and the downstream primer was 5’-CTTGTCGAACCG-CATACCCT-3’.
Mycobacterium Culture
BACTEC MGIT 960 was used for mycobacterial culture. After the BALF was thoroughly mixed, 5 mL was put into a centrifuge tube, and the digestion solution was added. It was vortexed until the digestion was complete. The supernatant was discarded after separation, and a small amount of polybutylene succinate was added to the pellet to resuspend it. The suspension was added to the MGIT tube (CAT #70937T) for culture. Culture-positive tubes were reconfirmed by acid-fast staining and subsequent identification of bacterial species.
Polymerase Chain Reaction and MALDI-TOF MS
Specimen DNA Extraction
The 50-mL collection tube was marked with the serial number and name and centrifuged at 10,000 rpm for 15 min. Then, the supernatant was discarded to keep the pellet, and 1.5–2 times the pellet volume of 4% sodium hydroxide (NaOH) was added to the corresponding 50-mL tube. This was shaken and mixed for 30s, incubated in a 45°C water bath to make it completely liquefied (the liquefaction time was controlled within 1 h). If the liquefaction had not been completed in 1 h, the clear and transparent part was taken for the experiment. The fully liquefied sample was transferred to a 1.5-mL Eppendorf (EP) tube. The sample was centrifuged at 15,000 rpm for 5 min. The supernatant was carefully aspirated after centrifugation. One mL of normal saline was added to each tube; each tube was shaken, mixed, and centrifuged at 15,000 rpm for 5 min. The supernatant was carefully aspirated after centrifugation. Next, 200–600 uL of lysis solution F5 was added to all samples according to the precipitation volume, then transferred to 1.5-mL cryopreservation tubes (if there were two tubes in one sample, they were combined into one tube), shaken and mixed well, and incubated in a metal bath at 99°C for 10 min. After the metal bath was complete, they were centrifuged briefly. All the liquid in the 1.5-mL EP tube was transferred to the first well of the reagent strip of Lab-Aid 824 Mycobacterium tuberculosis nucleic acid extraction, Maxi reagent. All samples treated with 4% NaOH had 10 ul of enhancement fluid added. The corresponding serial number of the sample was written on the edge of the tenth hole of the reagent strip. After ensuring that all reagent strips and trays were fixed on the sample rack, the magnetic rod sleeve was inserted into the groove of the magnetic rod. After the magnetic rod sleeve was locked in place, the extraction was performed, and after the extraction was completed, the liquid was aspirated from the last reaction well for subsequent polymerase chain reactions (PCRs).
Nucleic Acid Amplification
The PCR solution (prepared in advance) was added to a 96- or 384-well plate. Then 2 ul of the sample to be tested was added. The DNA extracted from the negative and positive samples was added to the reaction plate for product quality control during use. Then, the PCR product was purified. The reaction system was SAP Buffer 0.17 ul, SAP Enzyme (1.7 U/ul) 0.3 ul, and ultrapure water was added to make up 2 ul of solution. Next, 2 ul of SAP reaction solution was added to each reaction well. The reaction conditions were 37°C for 40 min and 85 °C for 5 min. After the SAP reaction, the extension reaction was carried out. The reaction system was: iPLEX Buffer 0.2 ul, iPLEX Termination mix 0.2 ul, Extend Primer Mix 0.94 ul and iPLEX Enzyme 0.041 ul. Finally, ultrapure water was added so the total volume equaled 2 ul, and 2 ul of the extension reaction solution was added to each reaction well.
3) Genotype interpretation according to the peak map of nucleic acid mass spectrometry detection by MALDI-TOF MS was performed and compared with the wild-type genotype to determine whether drug resistance occurred at the detection site as reported.11
Interpretation of results: See Table 1 for examples of the test samples.
 |
Table 1 Examples of MALDI-TOF MS Detection of Drug Resistance Genes in Nontuberculous mycobacteria |
Statistical Analysis
SPSS software version 22.0 was used for statistical analysis of the experimental data, and the enumeration data were expressed as percentages (%). The consistency between groups was compared by the kappa consistency test, and P<0.05 indicated that the consistency between different testing methods was not coincidental. The BACTEC MGIT 960 cultured gene chip drug resistance detection was used as a reference, and the efficacy of MALDI-TOF MS detection to identify NTM strains was evaluated. The agreement between the two methods was judged by the kappa test. A kappa value of 0.81–1 is almost perfect; 0.61–0.80 is highly consistent (substantial); 0.4–0.60 is moderate; 0.21–0.40 is fair; and 0.0–0.20 indicates very low consistency (slight).12
Results
General Information
Among the 172 patients with suspected NTM lung disease, ages ranged from 36 to 78 years, with an average age of 57. This included 47 males and 125 females, a body mass index of 22±5 kg/m2. Out of the 172 total patients, 108 (62.79%) had underlying lung diseases, including 54 cases (31.39%) bronchiectasis, 28 cases (16.28%) had chronic obstructive pulmonary disease; 21 cases (12.21%) had a history of pulmonary tuberculosis; 9 cases (5.23%) had silicosis; and 4 cases (2.33%) had pulmonary aspergillosis. In addition, 60 cases had comorbidities (34.88%), including 57 cases of diabetes (33.14%), 18 cases of hypertension (10.47%); 3 cases of long-term immunosuppressive therapy after kidney transplantation (1.74%); and 2 cases of rheumatoid arthritis (2.91%). Of the 172 patients, 137 cases of NTM lung disease tested positive by BALF NTM gene chip identification and/or MALDI-TOF MS.
Identification Results of NTM Strains
Among 172 patients with suspected NTM lung disease, 152 were positive for Mycobacterium in BACTEC MGIT 960 liquid culture, and 137 (79.65%, 137/172) were identified as NTM by gene chip. Thirteen isolates were identified. Mycobacterium avium complex (MAC) was the most commonly isolated strain, including Mycobacterium intracellulare, Mycobacterium avium, Mycobacterium marseillense and Mycobacterium colombiense, accounting for 70.07% (96/137), followed by Mycobacterium abscessus, accounting for 21.17% (29/137). Other NTMs only accounted for 8.76% (12/137) (Table 2).
 |
Table 2 The Bacterial Species Identification Results of 137 Patients with Confirmed NTM Lung Disease |
Efficacy Comparison of MALDI-TOF MS and BALF Culture
Among the 172 patients, 148 were positive for Mycobacterium by MALDI-TOF MS, and 131 (76.61%, 131/172) were identified as NTM. There was no coincidental consistency in the positive detection rate of Mycobacterium between MALDI-TOF MS and the BACTEC MGIT 960 liquid culture method (χ2=131.57, P<0.001). The sensitivity and specificity were 97.37% (148/152) and 100% (20/20), respectively. The positive predictive value and negative predictive value were 100% (148/148) and 83.33% (20/24), respectively, and the two detection methods were highly consistent (kappa=0.896). See Table 3.
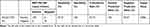 |
Table 3 Efficacy of MALDI-TOF MS Detection of Mycobacteria in BALF Specimens with the Results of Liquid Culture as the Reference Standard |
Comparison of Detection Efficiency of MALDI-TOF MS and the Gene Chip Method
There was no coincidental consistency in the positive detection rate of NTM strains detected by MALDI-TOF MS and the gene chip method (χ2=140.40, P<0.001). The sensitivity and specificity were 95.67% (131/137) and 100% (35/35), respectively. The positive predictive value and negative predictive value were 100% (131/131) and 85.37% (/35/41), respectively, and the two detection methods were highly consistent (kappa=0.899). See Table 4.
 |
Table 4 The Efficacy of MALDI-TOF MS Detection of NTM in BALF Specimens with the Results of Gene Chip Method as the Reference Standard |
Efficacy Analysis of MALDI-TOF MS for Detection of Drug Resistant Mutations
The efficacy analysis of 131 samples identified as NTM by the gene chip method and MALDI-TOF MS was performed. For the detection of drug resistance to macrolides (MAs), the consistency rate between MALDI-TOF MS detection and drug susceptibility detection was 97.71% (128/131). The sensitivity was 81.25% (13/16), the specificity was 100% (115/115) and the positive and negative predictive values were 100% (13/13) and 93.75% (115/118), respectively. There was no coincidental consistency in the detection of MA resistance rates between the two methods, and the consistency was high (χ2=94.84, P<0.001, kappa=0.884). For the drug resistance detection of amikacin (Am), the consistency rate between MALDI-TOF MS detection and drug susceptibility detection was 93.13% (122/131). The sensitivity was 93.52% (101/108), the specificity was 90.91% (21/23) and the positive and negative predictive values were 98.06% (101/103) and 75.00% (21/28), respectively. There was no coincidental consistency in the detection rate of Am resistance between the two methods, and the consistency was high (χ2=93.92, P<0.001, kappa=0.781). See Table 5.
 |
Table 5 Analysis of the Efficacy of MALDI-TOF MS for the Detection of Drug Resistance Mutations |
Discussion
The clinical data, imaging manifestations and laboratory examinations from 172 patients treated in our hospital with suspected NTM lung disease were statistically analysed. The results showed that most patients were middle-aged to elderly, and most suffered from chronic underlying lung diseases. The common clinical manifestations were cough and expectoration, night sweats, chest tightness, shortness of breath, sputum and blood haemoptysis and fatigue, with no obvious specificity; imaging manifestations showed various forms. Morphological lesions were mixed; sputum or other specimens were positive for acid-fast bacilli but negative by Xpert. Finally, 137 cases of NTM lung disease were diagnosed by BALF NTM gene chip identification and/or MALDI-TOF MS testing. When the results is positive, the NTM isolation rate is on the rise globally, and the distribution of strains varies greatly in different countries and regions.13,14 A recent meta-analysis of domestic NTM epidemiological studies showed that the NTM isolation rate was higher in the south than in the north and higher in the coastal areas than inland. The bacterial species differed in different provinces and cities.15 In this study, 137 isolates were identified as NTM by gene chip, and MAC (70.07%) was the most common isolate, including M. intracellulare, M. avium, M. marseillense and M. colombiense, followed by M. abscessus (21.17%); these findings are basically consistent with the prevalent strains in Hangzhou.16 For patients with these clinical manifestations, who are likely to have NTM lung disease, molecular diagnostic techniques should be used to confirm the diagnosis as soon as possible to reduce misdiagnosis and mistreatment.
This study showed that there was no coincidental consistency in the positive detection rate of Mycobacterium between MALDI-TOF MS detection and the BACTEC MGIT 960 liquid culture method (P<0.001). The sensitivity and specificity were 97.37% (148/152) and 100% (20/20), respectively, the positive predictive value and the negative predictive value were 100% (148/148) and 83.33% (20/24), respectively, and the kappa value was 0.896. It shows that the method has a good consistency with the detection results of the culture method and has a high detection efficiency, which is suitable for the primary screening of clinical specimens for Mycobacterium infection. There was no coincidental consistency in the positive detection rate of NTM strains detected by MALDI-TOF MS and the gene chip method (P<0.001). The sensitivity and specificity were 95.67% (131/137) and 100% (35/35), respectively, and the positive and negative predictive values were 100% (131/131) and 85.37% (35/41), respectively. The value is 0.899. It shows that MALDI-TOF MS detection and the gene chip method have high consistency in identifying NTM strains and have good application value in clinical practice, consistent with previous studies.17 In addition, four specimens in this study were positive for mycobacterial culture but negative for MALDI-TOF MS. The sequencing results showed that three were MTBC and one was M. surga. The reason for a negative MALDI-TOF MS test is that the specimen may contain no bacteria, or the bacterial content is below or close to the minimum detection limit of the reaction system, resulting in a negative result.
Global medical societies have jointly issued guidelines for the treatment of NTM, recommending that MAs and Am be used in patients with MAC lung disease and M. abscessus lung disease. Morimoto et al18 confirmed that MA-sensitive MAC lung disease is a predictor of treatment success. Drug susceptibility testing should be performed at the time of diagnosis to determine whether MA resistance can benefit patients in treatment. This study shows that the MALDI-TOF MS detection of MA and Am drug resistance is 97.71% and 93.13%, consistent with the drug susceptibility test results. The sensitivity and specificity are 81.25%, 100% and 93.52%, 90.91%, respectively. The positive predictive value and negative predictive value were 100%, 93.75% and 98.06%, 75.00%, respectively. Comparing the two detection methods, the kappa value was above 0.61, indicating that the two methods had high consistency in detecting drug resistance of MAs and Am. Due to the obvious correlation between MAs and Am, in vitro activity, and in vivo treatment results, the drug sensitivity test can be used as an important reference for the selection of treatment options.19,20
Limitations: We detected a minimal amount of types and numbers of NTM strains, while more than 170 different NTMs exist. The NTMs clinically isolated in this study are affected by regional differences, and the statistical data may be biased. In addition, this study only included clinical NTM isolates from the tuberculosis laboratory of our hospital, and the types of strains cannot cover all clinical NTM clinical isolates. Large-scale and multi-centre collaborative research is needed to enrich the evaluation of MALDI-TOF MS’s ability to identify NTM strains not covered in this paper.
Conclusion
In conclusion, MALDI-TOF MS detection is fast, sensitive, accurate and economical. It has high resolution, low requirements on the original sample and can provide accurate identification of NTM. It is highly consistent with the identification results of BACTEC MGIT 960 liquid culture and the gene chip method and can become a fast and effective way to screen for NTM.21,22 Moreover, it can provide drug resistance information to clinicians in a short time and provide an accurate, timely and effective laboratory test basis for clinical practice. It enables patients to receive timely and effective treatment, saves medical costs, improves patient prognosis and has good clinical application value for diagnosing and treating NTM lung disease.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Wenzhou Central Hospital (No.: L2021-03-083). Written informed consent was obtained from all participants.
Consent for Publication
The manuscript is not submitted for publication or consideration elsewhere.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding or sponsorship was received for this study or publication of this article.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Tuberculosis Branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of nontuberculous mycobacteriosis (2020 edition). Chin J Tuberculosis Respir Med. 2020;43(11):918–946. doi:10.3760/cma.j.cn112147-20200508-00570
2. Daley CL, Iaccarino JM, Lange C, et al. Treatment of Nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis. 2020;71(4):905–913. doi:10.1093/cid/ciaa1125
3. Ratnatunga CN, Lutzky VP, Kupz A, et al. The rise of non-tuberculosis mycobacterial lung disease. Front Immunol. 2020;11:303. doi:10.3389/fimmu.2020.00303
4. Liu CF, Song YM, He WC, et al. Nontuberculous mycobacteria in China: incidence and antimicrobial resistance spectrum from a nationwide survey. Infect Dis Poverty. 2021;10(1):59. doi:10.1186/s40249-021-00844-1
5. Tan Y, Su B, Shu W, et al. Epidemiology of pulmonary disease due to nontuberculous mycobacteria in Southern China, 2013–2016. BMC Pulm Med. 2018;18(1):168. doi:10.1186/s12890-018-0728-z
6. Liu G. Study on the Clinical Application Value of DNA Sequencing Method for Identifying Mycobacterium Species. Beijing Tuberculosis Chest Cancer Institute; 2016.
7. Ciet P, Serra G, Bertolo S, et al. Assessment of CF lung disease using motion corrected PROPELLER MRI: a comparison with CT. Eur Radiol. 2016;26(3):780–787. doi:10.1007/s00330-015-3850-9
8. Hettick JM, Kashon ML, Simpson JP, Siegel PD, Mazurek GH, Weissman DN. Proteomic profiling of intact mycobacteria by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Anal Chem. 2004;76(19):5769–5776. doi:10.1021/ac049410m
9. Basic Professional Committee of China Antituberculosis Association. Laboratory Inspection Regulations for Tuberculosis Diagnosis. Beijing: China Culture and Education Press; 2006.
10. Zhu L, Jiang G, Wang S, et al. Biochip system for rapid and accurate identification of mycobacterial species from isolates and sputum. J Clin Microbiol. 2010;48(10):3654–3660. doi:10.1128/JCM.00158-10
11. Shi J, He G, Ning H, et al. Application of matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) in the detection of drug resistance of Mycobacterium tuberculosis in re-treated patients. Tuberculosis. 2022;135:102209. doi:10.1016/j.tube.2022.102209
12. Tang W, Hu J, Zhang H, Wu P, He H. Kappa coefficient: a popular measure of rater agreement. Shanghai Arch Psychiatry. 2015;27(1):62–67. doi:10.11919/j.issn.1002-0829.215010
13. Smith GS, Ghio AJ, Stout JE, et al. Epidemiology of nontuberculous mycobacteria isolations among central North Carolina residents, 2006–2010. J Infect. 2016;72(6):678–686. doi:10.1016/j.jinf.2016.03.008
14. Koh WJ, Chang B, Jeong BH, et al. Increasing recovery of Nontuberculous mycobacteria from respiratory specimens over a 10-year period in a tertiary referral hospital in South Korea. Tuberc Respir Dis. 2013;75(5):199–204. doi:10.4046/trd.2013.75.5.199
15. Chu H, Zhao L, Xiao H, et al. Prevalence of nontuberculous mycobacteria in patients with bronchiectasis: a meta-analysis. Arch Med Sci. 2014;10(4):661–668. doi:10.5114/aoms.2014.44857
16. Yu F, Chen X, Ji Z, Xu K. Analysis of the prevalence of nontuberculous mycobacteria in Hangzhou from 2009 to 2014. Chin J Microecol. 2016;28(07):808–810, 815. doi:10.13381/j.cnki.cjm.201607015
17. Lotz A, Ferroni A, Beretti JL, et al. Rapid identification of mycobacterial whole cells in solid and liquid culture media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2010;48(12):4481–4486. doi:10.1128/JCM.01397-10
18. Morimoto K, Namkoong H, Hasegawa N, et al. Macrolide-resistant mycobacterium avium complex lung disease: analysis of 102 consecutive cases. Ann Am Thorac Soc. 2016;13(11):1904–1911. doi:10.1513/AnnalsATS.201604-246OC
19. Brown-Elliott BA, Woods GL, Kraft CS. Antimycobacterial susceptibility testing of Nontuberculous mycobacteria. J Clin Microbiol. 2019;57(10):e00834–19. doi:10.1128/JCM.00834-19
20. Huang WC, Yu MC, Huang YW. Identification and drug susceptibility testing for nontuberculous mycobacteria. J Formos Med Assoc. 2020;119 Suppl 1:S32–S41. doi:10.1016/j.jfma.2020.05.002
21. Alcaide F, Amlerová J, Bou G, et al. How to: identify non-tuberculous Mycobacterium species using MALDI-TOF mass spectrometry. Clin Microbiol Infect. 2018;24(6):599–603. doi:10.1016/j.cmi.2017.11.012
22. Buchan BW, Riebe KM, Timke M, Kostrzewa M, Ledeboer NA. Comparison of MALDI-TOF MS with HPLC and nucleic acid sequencing for the identification of Mycobacterium species in cultures using solid medium and broth. Am J Clin Pathol. 2014;141(1):25–34. doi:10.1309/AJCPBPUBUDEW2OAG
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
