Back to Journals » Journal of Pain Research » Volume 16
Skin Temperature of Acupoints in Health and Primary Dysmenorrhea Patients: A Systematic Review and Meta-Analysis
Authors Wang X , Zuo G, Liu J, Zhang J, Shi X, Fan X, Li X, Gao Y, Chen H, Liu CZ, She Y
Received 27 March 2023
Accepted for publication 1 June 2023
Published 14 June 2023 Volume 2023:16 Pages 2027—2046
DOI https://doi.org/10.2147/JPR.S411923
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Houman Danesh
Xuesong Wang,1,* Guang Zuo,1,* Jun Liu,1,2 Juncha Zhang,1,2 Xuliang Shi,1,2 Xisheng Fan,1,2 Xuxin Li,1 Yuanbo Gao,1 Hao Chen,1 Cun-Zhi Liu,3 Yanfen She1,2
1School of Acupuncture-Moxibustion and Tuina, Hebei University of Chinese Medicine, Shijiazhuang, Hebei, People’s Republic of China; 2Hebei International Joint Research Center for Dominant Diseases in Chinese Medicine and Acupuncture, Hebei University of Chinese Medicine, Shijiazhuang, Hebei, People’s Republic of China; 3School of Acupuncture-Moxibustion and Tuina, Beijing University of Chinese Medicine, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jun Liu; Yanfen She, School of Acupuncture-Moxibustion and Tuina, Hebei University of Chinese Medicine, No. 3 Xingyuan Road, Luquan Districtt, Shijiazhuang City, Hebei Province, 050200, People’s Republic of China, Email [email protected]; [email protected]
Objective: Dysmenorrhea is a common clinical condition and some studies shown that the skin temperature of some acupoints changes in primary dysmenorrhea (PD) patients. This study aimed to evaluate the changes in skin temperature at specific acupoints in PD patients and healthy subjects.
Methods: The literature for assessing skin temperature at acupoints in PD patients and healthy subjects was searched in eight databases. The literatures obtained from the search was independently screened by two authors, and the quality of the included articles was evaluated using the consensus checklist of the Thermographic Imaging in Sports and Exercise Medicine (TISEM) and the Newcastle–Ottawa Scale (NOS) scale. The skin temperature of the relevant acupoints or the difference between the left and right acupoints of the same name was used as the outcome during any period of menstruation. Finally, the meta-analysis was performed using RevMan 5.4.1 software to evaluate the changes in skin temperature in the related acupoints.
Results: Seven eligible studies were included, which included 328 patients with PD and 279 healthy subjects. The results of the meta-analysis revealed a significant difference in skin temperature around the Sanyinjiao (SP6)(MD: 0.04, 95% CI: 0.00, 0.08), Xuehai (SP 10)(MD: − 0.07, 95% CI:-0.11, − 0.02) and Taixi (KI 3)(MD: 0.06, 95% CI:0.01, 0.11) acupoints between PD and healthy subjects. PD patients also showed a difference in skin temperature at the Taixi (KI 3)(MD: 0.14, 95% CI:0.04, 0.24), Shuiquan (KI 5)(MD: 0.11, 95% CI: 0.03,0.19), Taichong (LR 3)(MD: − 0.10, 95% CI: − 0.19,-0.01), Diji (SP 8)(MD: − 0.09, 95% CI: − 0.16, − 0.01), and Xuehai (SP 10)(MD: − 0.14, 95% CI: − 0.23, − 0.06) acupoint areas at different times of menstruation compared to that of healthy subjects, as revealed by the subgroup analysis.
Conclusion: Primary dysmenorrhea patients showed some differences in the skin temperature of the special acupoints are as Sanyinjiao (SP6), Diji (SP 8), Xuehai (SP 10), Shuiquan (KI 5), Taichong (LR 3), and Taixi (KI 3) compared with healthy subjects.
Registration Number: CRD42022381387.
Keywords: acupuncture points, acupoints, acupoint sensitization, skin temperature, thermography, meta-analysis, systematic review
Introduction
Dysmenorrhoea is a common clinical disease, with cyclic pelvic pain or lumbosacral pain as the main symptom during or around the time of menstruation.1 It can be classified as primary dysmenorrhoea (PD) or secondary dysmenorrhoea according to its cause, with PD accounting for more than 90% of the incidence.2 One-third to one half of patients with dysmenorrhoea experience moderate to severe symptoms, which are consequently affecting the patient’s quality of life.3–5 Approximately 45% to 90% of women suffer from dysmenorrhea from the onset of the ovulatory cycle,6 and the prevalence of PD among female university students in China is 41.7%.7,8 In addition to the physical pain, PD increases the prevalence of chronic pelvic inflammatory disease3 affecting patients’ work, study, and quality of life.9
At present, the conventional treatment for PD consist of non-steroidal drugs and oral contraceptives, but their long-term use can lead to gastrointestinal and other adverse effects.10 Therefore, acupuncture therapy has become one of the most commonly used non-pharmacological therapies for PD thanks to the advantages in treating PD, such as precise efficacy and significant pain relief;11–13 the latest evidence-based acupuncture guidelines also recommend the use of acupuncture therapy.14
Acupoints are key areas where acupuncture exerts its curative purposes, and data mining indicated that acupoints such as Sanyinjiao (SP 6), Guanyuan (RN4), and Diji (SP8) have a high frequency of use in the treatment of PD.15 However, different studies have used different acupuncture prescriptions, and the efficacy of different combinations of acupoints has varied, and we hope to find the optimal combination of acupoints. When the body is under pathological stress (injury or disease), the relevant acupoints change their sensitivity thresholds and biophysical properties,16–20 ie, acupoints can react to disease. In other words, the status of the acupoints during the pathological process is dynamically changed from a “silent” to an “active” state, and the stimulation of the “activated” acupoints results in a better therapeutic effect, which is called acupoint sensitisation.
In recent years, some researchers have used thermographic imaging to detect the temperature of the body surface in the acupoints of PD patients and to analyse the temperature changes. However, their results were different; some studies showed that the temperature difference between the Sanyinjiao (SP 6) on the left and right sides of PD patients during menstruation is higher than that of healthy subjects,21 while others showed that the temperature difference is no significant between PD patients and healthy subjects.22
However, the methods to measure the temperature vary and involve many acupoints, making it difficult to reach a consistent conclusion. Therefore, the aim of this study was to evaluate the differences in the relevant acupoints’ skin temperature between PD patients and healthy subjects by a meta-analysis to provide some reference for further research on the temperature characteristics of acupoints.
Methods
This study was performed according to the checklist of the preferred reporting items for systematic reviews and meta-analyses (PRISMA 2020)23 (see Appendix 1). This study was registered in PROSPERO (https://www.crd.york.ac.uk/PROSPERO), with the registration number CRD42022381387.
Search Strategies
Eight databases were used to search the related articles, such as Web of Science, PubMed, EMBASE, Cochrane Library, China Biology Medicine (CBM), China National Knowledge Infrastructure (CNKI), Wanfang Data, and Chinese Scientific Journal Database (VIP). The search was performed from the date of the establishment of each database to 01 November 2022, using a combination of medical terms and free words, and retrospectively including the references of the selected literature to eventually find additional relevant articles.
Chinese search terms included ZhenJiu, ZhenCi, DianZhen, AiJiu, JingLuo, ShuXue, XueWei, WenDu, XueQv WenDu, ReMin, PiFu WenDu, TongJing, and YuanFaXingTongJing. English search terms include acupuncture, acupoints, acupoint, needle therapy, needling, meridian, needling, acupoint sensitization, moxibustion, moxibustion therapy, temperature, skin temperature, skin temperatures, heat sensitization, heat-sensitization, primary dysmenorrhea, dysmenorrhea, dysmenorrheas, menstrual pain, menstrual pains, painful menstruation, and painful menstruations. The full search strategy is shown in Appendix 2.
Inclusion Criteria
The inclusion criteria were the following: (1) Published studies on the detection of body surface temperature at the relevant acupoints in PD patients without age or gender limitation; (2) The language of the publication was limited to Chinese or English; (3) The study design was limited to a case-controlled study: the case group was represented by PD patients with clear diagnostic criteria and confirmed diagnosis as PD; the control group was represented by healthy subjects; (4) The results must include at least the relevant acupoints’ skin temperature at any period before, during or after menstruation or the temperature difference between the left and right acupoints of the same name.
Exclusion Criteria
The exclusion criteria were the following: (1) Studies that did not report clear diagnostic criteria; (2) Studies that included patients with secondary dysmenorrhoea; (3) Studies in which the control group was not represented by healthy subjects; (4) Studies in which either intervention was applied to both PD and healthy controls; (5) Studies that reported no clear original data and the authors were contacted without success; (6) Studies in which the temperature of specific acupoints in the skin were not available for the outcome indicators; (7) Duplicate studies or studies that reported the same results.
Literature Screening and Data Extraction
The literature screening and data extraction were individually carried out by two researchers and finally cross-checked. A third researcher decided in case of disagreement. The data extraction required the use of a pre-formulated form containing general information on the included literature, including name of the first author, name of the journal, and year of publication; baseline data on the subjects included in the literature including group information, sample size, age of the subjects and course of the disease; temperature information of skin acupoints including environmental measurement, measurement equipment, and data processing; temperature information of skin acupoint in pre/postmenstrual/menstrual period at any time including time point of measurement, information on the acupoints, absolute temperature of the acupoints’ skin temperature and difference in temperature between left and right acupoints of the same name.
Quality Assessment of the Bias of the Included Studies
To evaluate the rigor and credibility of the measurements of the acupoints’ skin temperature in the included study, the Thermographic Imaging in Sports and Exercise Medicine (TISEM) consensus checklist was used,24 which was performed by experts in the field of physiology and infrared thermographic imaging to standardize the collection and analysis of the skin temperature measurements, which were used as a tool to assess the bias in the thermographic studies. The TISEM checklist is composed of 15 items: individual data, previous instructions, extrinsic factors, environmental condition, environmental setup, equipment, acclimation, camera preparation, image recording, camera position, emissivity, assessment time, body position, method of drawing the skin, and image evaluation. Each item has three possible responses: yes, no, and unclear (Appendix 3). Some items in the consensus checklist are not applicable (NA) for studies that did not use infrared thermographic imaging (eg, thermocouples); thus, the NA marker was used.
Since the included studies included the comparisons of PD patients with healthy subjects, the comparisons were also assessed using the modified Newcastle-Ottawa Scale (NOS) for case-control studies.21 The NOS scale is a commonly used tool for evaluating the quality of case-control studies and allows user modification. The original scale consists of three categories: selection of cases and controls, comparability of cases and controls, and determination of the exposure. The determination of the exposure was omitted in this word since it is not relevant to our purpose. All items also had three possible responses: yes, no, and unclear. The TISEM checklist and NOS scales were evaluated independently by two researchers for each item separately, with a third researcher involved in case of disagreement.
Statistical Analysis
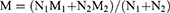
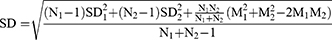
Meta-analysis was performed using RevMan 5.4.1 software. Data from subgroups where different Chinese medicine syndrome types existed were merged using the formulae (1)(2)(3), and for those who did not report the difference in skin temperature between the left and right sides of the acupoints with the same name, the formulae (4 and 5) were used for conversion.
The I2 test was used to assess the heterogeneity among the results of the included studies; the data were combined using a fixed-effects model when I2 ≤ 50% and P ≥ 0.1, indicating less heterogeneity among the included studies; conversely, the data indicating greater heterogeneity were combined using a random-effects model. The method provided by Luo25 and Wan26 was used for conversion of studies with non-normally distributed data reporting median, P25 and P75 or median (median, M), maximum (maximum, Max) and minimum (minimum, Min) values. All the acupoints’ skin temperatures were measured, and the mean difference (MD) was used as the effect indicator, with point estimates and 95% confidence intervals (CI) provided for each effect indicator. Subgroup analyses were performed due to the different time points of the measurement of the acupoints’ skin temperatures involving premenstrual, menstrual and postmenstrual periods.
Results
Study Search and Description
A total of 266 records were collected during the initial database search, with 193 remaining after removing the duplicates. A total of 134 irrelevant literature were also excluded according to the title and abstract, resulting in 59 remaining articles. After reading the full text, a total of 7 articles matching the criteria were finally included, but one of them did not report the time point of the skin temperature measurements, so we only did a descriptive analysis.27 Two of them were in English21,22 and five were in Chinese.27–31 The screening process is shown in Figure 1 (the excluded literature can be found in Appendix 4).
 |
Figure 1 Flow chart of the literature screening. |
Characteristics of the Included Articles
This study included seven articles; three were journal articles21,22,30 and four were degree theses.27–29,31 They included a total of 328 PD patients and 279 healthy subjects. All trials were conducted in China: five used infrared thermographic imaging techniques21,27–30 and two used contact thermocouple thermometry.22,31 A total of 14 acupoints’ skin temperature were reported: Sanyinjiao (SP 6), Diji (SP 8), Xuehai (SP 10), Zhongdu (LR 6), Shuiquan (KI 5), Taibai (SP 3), Taichong (LR 3), Xuanzhong (GB 39), Taixi (KI 3), GuanYuan (RN 4), ShiQiZhui (EX-B7), ZhongJi (RN 3), ZiGong (EX-CA1), and YinLingQuan (SP 9), with the nine acupoints Sanyinjiao (SP 6), Diji (SP 8), Xuehai (SP 10), Zhongdu (LR 6), Shuiquan (KI 5), Taibai (SP 3), Taichong (LR 3), Xuanzhong (GB 39) and Taixi (KI 3) reported more than four times, We have summarized all the acupoints included in the analysis into a single figure, see Figure 2. Thus, the data reporting changes in skin temperature in these nine acupuncture areas were merged. The basic characteristics of the included studies are shown in Table 1.
 |
Table 1 Characteristics of the Included Articles |
 |
Figure 2 Location of acupoints evaluated in the included studies. |
Literature Quality Assessment
Table 2 shows the results of the quality evaluation of the methods used to evaluate the skin temperature in the included studies. Five studies used infrared thermographic imaging techniques,21,27–30 and basic information, ambient temperature and humidity at the measurement location, equipment information, premeasurement adaptation period, and skin temperature measurement time were reported in all of them. However, no information was reported on the recording conditions of the temperature (such as the distance between the camera and the skin), the camera position (perpendicular to the skin), and camera emissivity, while pre-instruction,27 external factors influencing the skin temperature,27 advance camera warm-up,21 and methods for drying the skin27 were reported in only one study. Two other studies did not use infrared thermographic imaging techniques;22,31 eight items that were not related to infrared thermographic imaging techniques were evaluated, and the remaining seven were marked as NA.
 |
Table 2 Quality Assessment of the Temperature Measurement Methods of the Included Studies Based on TISEM Checklist |
Table 3 shows the quality assessment of the six factors in the case-control design of the included studies. All studies reported the validation of cases, representativeness of the cases, and selection of controls, but only two studies described the definition of controls,27,28 and four studies compared the cases with the controls regarding the duration of menstrual cycle.21,22,28,31
 |
Table 3 Quality Assessment of Case-Control Studies Based on the Modified Newcastle-Ottawa Scale |
Results of the Meta-Analysis
Sanyinjiao (SP 6) Acupoint
A total of six studies reported the changes in skin temperature in the right and left SP 6 acupoint areas, which included 288 PD patients and 269 healthy subjects, and involving three periods: premenstrual, menstrual, and postmenstrual periods. The difference in skin temperature was compared in a total of 1488 groups. A low heterogeneity among the included studies was found, as revealed by the heterogeneity test showing a value of P = 0.73 and I2 = 0%, and the fixed effects model was used to combine the effect size. The meta-analysis results showed that the difference in skin temperature between the right and left side of the SP 6 acupoint area was significantly higher in PD patients than in the healthy subjects (MD = 0.04, 95% CI = [0.00, 0.08], P= 0.03, P< 0.05). The differences in skin temperature of the SP 6 acupoints in different menstrual cycles were further explored by performing the subgroup analysis according to the different measurement time points of the menstrual cycle, in which three reported the differences in skin temperature of the SP 6 acupoints in the left and right sides in the premenstrual period, six reported them during menstruation, and four reported them in the postmenstrual period. The results showed no significant difference in temperature between the left and right sides of SP 6 during the premenstrual period (MD = 0.06, 95% CI = [−0.01,0.14], P = 0.08), and postmenstrual cycle (MD=-0.01, 95% CI = [−0.09, 0.06], P = 0.71) in PD patients compared with healthy subjects. However, PD patients during the menstrual cycle had higher skin temperature difference between the left and right sides of the SP 10 acupoint area than in healthy subject (MD =0.07, 95% CI = [0.00, 0.13], P = 0.04, P < 0.05) (Figure 3).
 |
Figure 3 Forest plot of the difference in skin temperature between PD patients and healthy people at the Sanyinjiao (SP 6) acupoint. |
DiJi (SP 8) Acupoint
A total of five studies including 282 PD patients and 263 healthy subjects reported changes in skin temperature between the right and left side of the SP 8 acupoint area, with 1476 groups comparing the difference in skin temperature of the SP 8 acupoint area. A large heterogeneity among the included studies was found using the heterogeneity test, with a P = 0.003 and I2 = 60%, and the random effects model was used to combine the effect size. The meta-analysis showed no significant difference in skin temperature between the right and left side of the SP 8 acupoint area in PD patients compared with healthy subjects (MD = 0.00, 95% CI = [−0.06,0.06], P = 0.95). A subgroup analysis was performed based on different measurement time points of the menstrual cycle to further explore the difference in skin temperature during different menstrual cycles. Three studies reported the differences in skin temperature of the SP 8 acupoint area during the premenstrual period, five reported it during the menstrual period, and four reported it during the postmenstrual period. The results showed no significant difference in skin temperature between the right and left sides of the SP 8 acupoint area during the premenstrual (MD = 0.02, 95% CI = [−0.07, 0.17], P=0.068) and menstrual (MD = 0.05, 95% CI = [−0.04,0.14], P = 0.25) periods in PD patients, while they had lower skin temperature difference between the left and right sides of the SP 8 acupoint area compared with healthy subject during the postmenstrual period (MD = −0.09, 95% CI = [−0.16, −0.01], P = 0.02, P < 0.05) (Figure 4).
 |
Figure 4 Forest plot of the difference in skin temperature between PD patients and healthy people at the DiJi (SP 8) acupoint. |
XueHai (SP 10) Acupoint
A total of five studies including a total of 282 PD patients and 263 healthy subjects reported the changes in skin temperature in the left and right side of the SP 10 acupoint area. A total of 1476 groups compared the differences among the SP 10 acupoint area. No significant heterogeneity among the included studies was found, as revealed by the heterogeneity test showing a value of P = 0.79 and I2 = 0%, and the fixed effects model was used to combine the effect size. The meta-analysis results showed that the difference in skin temperature between the right and left side of the SP 10 acupoint area was significantly lower in PD patients than in the healthy subjects (MD = −0.07, 95% CI = [−0.11, −0.02], P = 0.003, P < 0.05). A subgroup analysis was performed to further explore the differences in skin temperature between the left and right sides of the SP 10 acupoint area at different menstrual periods based on different measurement time points of the menstrual period, with three studies reporting differences in the premenstrual period, five reporting the differences in the menstrual period, and four reporting the differences in the postmenstrual period. The results showed no significant difference in skin temperature between the left and right sides of the SP 10 acupoint area in the premenstrual (MD = −0.04, 95% CI = [−0.11, 0.04], P = 0.31) and menstrual (MD = −0.03, 95% CI = [−0.11,0.04], P = 0.33) period in PD patients compared to healthy subjects. However, PD patients during the postmenstrual period had lower skin temperature difference between the left and right sides of the SP 10 acupoint area than in healthy subject (MD = −0.14, 95% CI = [−0.23, −0.06], P = 0.0006, P < 0.05) (Figure 5).
 |
Figure 5 Forest plot of the difference in skin temperature between PD patients and healthy people at the XueHai (SP 10) acupoint. |
ZhongDu (LR 6) Aupoint
A total of four studies including a total of 261 PD patients and 257 healthy subjects reported the changes in skin temperature in the right and left side of the LR 6 acupoint area, for a total of 1449 groups comparing the differences of the Zhongdu LR 6 acupoint area. A low heterogeneity among the studies was found, as revealed by the heterogeneity test showing a value of P = 0.93 and I2 = 0%, and the fixed effects model was used to combine the effect size. The meta-analysis results showed no significant difference in skin temperature between the left and right LR 6 acupoint areas in PD patients than the healthy subjects (MD = 0.02, 95% CI = [−0.01,0.05], P = 0.22). A subgroup analysis was performed according to the time points of the menstrual period to further explore the difference in skin temperature between the left and right sides of the LR 6 acupoint area during the menstrual period, with three studies reporting differences in the premenstrual period, four reporting differences in the menstrual period, and four reporting the differences in the postmenstrual period. The results showed no significant difference in skin temperature between the left and right sides of the LR 6 point area in PD patients during the premenstrual (MD = 0.03, 95% CI = [−0.02, 0.09], P=0.26), menstrual (MD = 0.04, 95% CI = [−0.01, 0.09], P=0.14) and postmenstrual (MD = −0.02, 95% CI = [−0.08, 0.04], P = 0.53), period compared to the healthy subjects (Figure 6).
 |
Figure 6 Forest plot of the difference in skin temperature between PD patients and healthy people at the ZhongDu (LR 6) acupoint. |
ShuiQuan (KI 5) Acupoint
A total of 4 studies including 261 PD patients and 257 healthy subjects reported changes in skin temperature at the left and right KI 5 acupoint area. A total of 1449 groups compared the difference of KI 5 acupoint area. Results showed that: indicating A high heterogeneity among various studies was found by the heterogeneity test, with a value of P = 0.08 and I2=40%, and the random effects model was used to combine the effect size. The meta-analysis results showed no significant difference in skin temperature between the left and right KI 5 acupoint area in PD patients compared with healthy subjects (MD = 0.02, 95% CI = [−0.05, 0.09], P = 0.51). A subgroup analysis was performed according to different measurement time points during different menstrual periods to further explore the difference in skin temperature between left and right KI 5 acupoints. Three studies reported the difference during the premenstrual period, four reported the difference during the menstrual period, and four reported the difference during the postmenstrual period. The results showed no significant difference in skin temperature between the left and right sides of KI 5 acupoint area during the premenstrual (MD = 0.04, 95% CI = [−0.10,0.18], P = 0.58), and postmenstrual period (MD = −0.07, 95% CI = [−0.16, 0.01], P = 0.10) in the in PD patients compared with healthy subjects. However, the difference in skin temperature between the left and right KI 5 acupoint area of PD patients during the menstrual period (MD = 0.11, 95% CI = [0.03,0.19], P = 0.007, P < 0.05) was higher than that of healthy people, and the difference was significant (Figure 7).
 |
Figure 7 Forest plot of the difference in skin temperature between PD patients and healthy people at the ShuiQuan (KI 5) acupoint. |
Taibai (SP 3) Acupoint
A total of 4 studies including 261 PD patients and 257 healthy subjects reported the changes in skin temperature in the left and right SP 3 acupoint area. A total of 1449 groups compared the difference of SP 3 acupoint area. A low heterogeneity was found among the included studies, as revealed by the heterogeneity test results, with a value of P = 0.57 and I2 = 0%, and the fixed-effect model was used to combine the effect size. The meta-analysis results showed no significant difference in skin temperature between the left and right SP 3 acupoint area in PD patients compared with healthy people (MD = −0.04, 95% CI = [−0.10,0.03], P=0.25). A subgroup analysis was performed according to the different measurement time points during the menstrual period to further explore the difference of skin temperature in the left and right SP 3 acupoint of different menstrual periods. Three studies reported the difference during the premenstrual period, four reported the difference during the menstrual period, and four reported the difference during the postmenstrual period. The results showed no significant difference in skin temperature between the left and right SP 3 acupoint area during the premenstrual (MD = −0.08, 95% CI = [−0.18,0.03], P = 0.15), menstrual (MD = 0.05, 95% CI = [−0.06,0.16], P = 0.40) and postmenstrual period (MD = −0.07, 95% CI = [−0.17, 0.04], P = 0.20) in PD patients compared with healthy subjects (Figure 8).
 |
Figure 8 Forest plot of the difference in skin temperature between PD patients and healthy people at the Taibai (SP 3) acupoint. |
Taichong (LR 3) Acupoint
A total of 4 studies including 261 PD patients and 257 healthy subjects reported changes in skin temperature in the left and right LR 3 acupoint area. A total of 1449 groups compared the difference in skin temperature in the left and right LR 3 acupoint area. A moderate heterogeneity among the included studies was found, as revealed by the heterogeneity test, with a value of P = 0.08 and I2 = 40%, and a fixed-effect model was used to combine the effect size. The meta-analysis results showed no significant difference in skin temperature difference between the left and right LR 3 acupoint area in PD patients compared with healthy subjects (MD = −0.01, 95% CI = [−0.07, 0.05], P = 0.75). A subgroup analysis was performed according to different measurement time points during the different menstrual periods to further explore the difference of skin temperature in the left and right LR 3 acupoint. Three studies reported the difference during the premenstrual period, four reported the differences during the menstrual period, and four reported the differences during the postmenstrual period. The results showed no significant difference in skin temperature difference between the left and right sides of the LR 3 acupoint area during the premenstrual (MD = 0.03, 95% CI = [−0.08,0.13], P = 0.62) and postmenstrual period (MD = 0.06, 95% CI = [−0.03, 0.16], P = 0.19) in PD patients compared with healthy subjects. However, the difference of skin temperature in the left and right LR 3 acupoint area of PD patients during the menstrual period (MD = −0.10, 95% CI = [−0.19,-0.01], P = 0.03, P < 0.05) was lower than that of the healthy subjects, and the difference was significant (Figure 9).
 |
Figure 9 Forest plot of the difference in skin temperature between PD patients and healthy people at the Taichong (LR 3) acupoint. |
XuanZhong (GB 39) Acupoint
A total of 4 studies including 261 PD patients and 257 healthy subjects reported changes in skin temperature at the left and right GB 39 acupoint area. A total of 1449 groups compared the difference in skin temperature in the left and right GB 39 acupoint area. A low heterogeneity among various studies was found, as revealed by the heterogeneity test results, with a value of P = 0.40 and I2 = 5%, and the fixed-effect model was used to combine the effect sizes. The meta-analysis results showed no significant difference in skin temperature between the left and right GB 39 acupoint area in PD patients compared with healthy subjects (MD = −0.00, 95% CI = [−0.04, 0.04], P = 1.00). A subgroup analysis was conducted according to the different measurement time points during the menstrual period to further explore the difference of skin temperature in the left and right GB 39 acupoint area. Three studies reported the difference during the premenstrual period, four reported the differences during the menstrual period, and four reported the differences during the postmenstrual period. The results showed no significant difference in skin temperature between the left and right GB 39 acupoint area during the premenstrual (MD = 0.07, 95% CI = [−0.01, 0.15], P = 0.10), menstrual (MD = −0.01, 95% CI = [−0.08,0.06], P = 0.76) and postmenstrual period (MD = −0.05, 95% CI = [−0.13, 0.03], P = 0.22) in the PD patients compared with healthy subjects (Figure 10).
 |
Figure 10 Forest plot of the difference in skin temperature between PD patients and healthy people at the XuanZhong (GB 39) acupoint. |
Taixi (KI 3) Acupoint
A total of 4 studies including 261 PD patients and 257 healthy subjects reported changes in skin temperature at the left and right KI 3 acupoint area. A total of 1449 groups compared the difference in skin temperature at the left and right KI 3 acupoint area. A moderate heterogeneity among the included studies was found, as revealed by the heterogeneity test results with a value of P = 0.11 and I2 = 36%, and the fixed-effect model was used to combine the effect size. The meta-analysis results showed that the difference of skin temperature in the left and right KI 3 acupoint area in PD patients was higher than that in the healthy subjects (MD = 0.06, 95% CI = [0.01, 0.11], P = 0.02, P < 0.05), and the difference was statistically significant. A subgroup analysis was performed according to the different measurement time points during the menstrual period, among which 3 studies reported the differences in s premenstrual, four reported the difference in different menstrual periods to further explore the differences in skin temperature between left and right sides of KI 3 acupoint area. Four reported the difference during the postmenstrual period. The results showed that the difference of skin temperature in the KI 3 acupoint area on both sides of PD patients was higher than that of healthy subjects during the premenstrual (MD = 0.14, 95% CI = [0.04, 0.24], P = 0.006, P < 0.05) and menstrual period (MD = 0.09, 95% CI = [0.01, 0.18], P = 0.02, P < 0.05) period, and the difference was significant. However, no significant difference in skin temperature between PD patients and healthy subjects was observed during the postmenstrual period (MD = −0.03, 95% CI = [−0.11, 0.05], P = 0.42) (Figure 11).
 |
Figure 11 Forest plot of the difference in skin temperature between PD patients and healthy people at the Taixi (KI 3) acupoint. |
Analysis of Publication Bias
Since no more than 10 studies were included for each outcome in our study, funnel plots were not performed.
Discussion
A total of 7 studies that involved 328 PD patients and 279 healthy controls were included in this study. The differences in skin temperature at the relevant acupoints in PD patients were compared with those of healthy subjects. A total of nine acupoints such as Sanyinjiao (SP 6), Diji (SP 8), Xuehai (SP 10), Zhongdu (LR 6), Shuiquan (KI 5), Taibai (SP 3), Taichong (LR 3), Xuanzhong (GB 39) and Taixi (KI 3) were considered. The skin temperature in the areas of the Diji (SP 8), Xuehai (SP 10), Shuiquan (KI 5), Taichong (LR 3) and Taixi (KI 3) acupoints was different in PD patients compared with healthy subjects. The overall results showed that the difference in skin temperature between the left and right areas of the Sanyinjiao (SP6), Xuehai (SP 10) and Taixi (KI 3) acupoints was significantly different between PD patients and healthy subjects. The results of the subgroup analysis showed that the difference of skin temperature in the acupoint area of Taixi (KI 3) was significantly different between the PD patients and the healthy subjects before menstruation; the difference of skin temperature in Sanyinjiao (SP6), Shuiquan (KI 5), Taichong (LR 3) and Taixi (KI 3) acupoints during menstruation was significantly different between PD patients and the healthy subjects; the difference of skin temperature in Digi (SP 8) and Xuehai (SP 10) acupoints after menstruation was significant between PD patients and the healthy subjects. In summary, the temperature differences of Sanyinjiao (SP6), Diji (SP 8), Xuehai (SP 10), Shuiquan (KI 5), Taichong (LR 3) and Taixi (KI 3) had a certain potential in the early diagnosis and in the evaluation of the efficacy of acupuncture in PD patients.
Some studies showed that in patients with PD and healthy subjects have an asymmetry in skin temperature at some acupoints, and this asymmetry has some significance in the early detection of the disease, early complementary diagnosis, and evaluation of the efficacy of complementary therapies.32 Some acupoints show certain thermal characteristics of the skin, presenting an imbalance in skin temperature in the left and right specific acupoints in pathological processes such as chronic bronchial asthma,33 chronic hepatitis,34 breast hyperplasia,35–37 infertility,38 intracranial hypertension,39 obesity,40 and PD.22,41 The imbalance in body surface temperature also has diagnostic value for a variety of pathological statuses, such as breast disease,42 diabetic foot,43 acute stroke,44 and facial palsy.45
Acupoints are special areas where the Qi (气, ie, vital energy) from the Zang-Fu (脏腑) organs and meridians is transferred and infiltrated, and they are special areas on the body surface that are interconnected with the related parts of the Zang-Fu (脏腑) organs. Acupoints adjust the function of the Zang-Fu (脏腑) organs and are the key of the acupuncture treatment of diseases. They are also special areas that reflect the function of the Zang-Fu (脏腑) organs and play a role in assisting the diagnosis of diseases. Acupoint sensitization occurs with the development of Zang-Fu (脏腑) diseases and disappears with the disappearance of these diseases, indicating that acupoint sensitization on the body surface is closely related to the development of Zang-Fu (脏腑) diseases in the body. The functional status of acupoints strongly influences the effects of acupuncture, and the dynamic change from “silence” to “awakening” of the acupoints enhances their acupuncture function and produce a “small stimulus with a large effect”. The mechanism is related to central and peripheral nervous system sensitization mechanisms.46 The asymmetry in the temperature of specific acupoints on the body’s surface in a disease status falls into the category of thermal sensitization. Numerous studies showed that the selection of sensitised acupoints to be used for intervention is more effective than the use of traditional acupuncture points. The study of asymmetries in skin temperature at specific acupoints during a disease status helps disease diagnosis and increases effectiveness. Infrared thermographic imaging techniques can use sensors to receive infrared radiation from the human body surface without any external factors, and after processing, infrared thermograms of the human body surface can be obtained, which can reflect the real-time thermal metabolic status of the body and play a significant role in the prevention and diagnosis of diseases. Various methods of detecting body surface temperature are available besides infrared thermographic imaging techniques, such as thermistor thermometers and semiconductor thermometers.47 Infrared thermographic imaging techniques offer images of the temperature distribution in the body surface with greater accuracy, sensitivity and resolution than contact thermometry, being objective, accurate, simple, convenient, and reproducible.48–50
Overall, this is the first study that systematically evaluates the difference in skin temperature of specific acupoints in patients with PD and healthy subjects achieving certain findings. This study summarized the current clinical evidence and found that some acupoints showed some temperature specificity in the menstrual cycle of PD patients, and detecting these acupoints with changed temperature, could contribute to the early diagnosis of PD and the development of portable devices; in addition, stimulation of these acupoints with changed skin temperature could achieve better efficacy. Although identifying some problems: (1) We limited the language of the included literature to Chinese or English, and the authors of the included studies were from China, so there may be publication bias considering the influence of Chinese culture; (2) The TISEM consensus checklist is recommended to assess the quality of the study when using infrared thermographic imaging techniques to ensure more reliable results that ensure the rigor and credibility of the skin temperature measurements of the acupoints; (3) Different ways of averaging multiple measurements and averaging consecutive measurements are available in the measure of skin temperature, which need to be standardized in future studies; (4) Since skin temperature is influenced by circadian rhythms, the time points of skin temperature measurement should be as consistent as possible within the same study; (6) The time points of measurement in PD involve the premenstruation, menstruation and postmenstruation periods. For example, as regard the premenstrual period, some studies choose 1 day before menstruation while others choose 3 days before it; thus, the timing of the premenstrual period is often difficult to understand; (6) all the included studies used acupoints as the areas of temperature measurement, and their choice was mostly based on clinical experience. However, it is not known whether skin temperature changes in other areas (other unselected acupoints or non-acupoints) compared to these acupoints. Thus, the focus of future studies will be to establish whether changes in skin temperature during a pathological status are always specific to acupoints; (7) the majority of the included studies evaluated the absolute value of the difference between the skin temperature of the left and right homonymous acupoints (ie, the degree of imbalance) as an outcome indicator, while some studies reported the absolute skin temperature of the left and right homonymous acupoints. Some other studies selected a point on another part of the body as a reference (eg, theYingtang(GV24+) acupoint) and then they measured the temperature of the target acupoint and compare the change in acupoint temperature. Overall, it seems more appropriate to use the degree of imbalance to evaluate the temperature changes of the acupoints.
Conclusion
Primary dysmenorrhoea patients showed some differences in skin temperature in some acupoint areas, such as Sanyinjiao (SP6), Diji (SP 8), Xuehai (SP 10), Shuiquan (KI 5), Taichong (LR 3) and Taixi (KI 3) compared with healthy subjects. These acupoints are specific in the early diagnosis and evaluation of the efficacy of acupuncture in primary dysmenorrhoea patients.
Acknowledgments
We would like to thank MogoEdit (https://www.mogoedit.com) for its English editing during the preparation of this manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81973755), and the Project on Hebei Administration of Traditional Chinese Medicine (No. 2022091).
Disclosure
All authors declare that they have no potential conflicts of interest.
References
1. Lefebvre G, Pinsonneault O, Antao V, et al. Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2005;27:1117–1146.
2. Burnett M, Lemyre M. No. 345-primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2017;39:585–595. doi:10.1016/j.jogc.2016.12.023
3. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21:762–778. doi:10.1093/humupd/dmv039
4. Sharghi M, Mansurkhani SM, Larky DA, et al. An update and systematic review on the treatment of primary dysmenorrhea. JBRA Assist Reprod. 2019;23:51. doi:10.5935/1518-0557.20180083
5. Vincenzo De Sanctis M, Soliman A, Bernasconi S, et al. Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev. 2015;13:465–473.
6. Rencz F, Péntek M, Stalmeier PF, et al. Bleeding out the quality-adjusted life years: evaluating the burden of primary dysmenorrhea using time trade-off and willingness-to-pay methods. Pain. 2017;158:2259–2267. doi:10.1097/j.pain.0000000000001028
7. Hu Z, Tang L, Chen L, Kaminga AC, Xu H. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a cross-sectional study. J Pediatr Adolesc Gynecol. 2020;33:15–22. doi:10.1016/j.jpag.2019.09.004
8. Meng W, Wang N, Li P, et al. Epidemiological investigation of primary dysmenorrhea of female college students and its influencing factors. J Shandong First Med Univ Shandong Acad Med Sci. 2013;2013:579–583.
9. Unsal A, Ayranci U, Tozun M, Arslan G, Calik E. Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Ups J Med Sci. 2010;115:138–145. doi:10.3109/03009730903457218
10. Furniss LD. Nonsteroidal anti-inflammatory agents in the treatment of primary dysmenorrhea. Clin Pharm. 1982;1:327–333.
11. Zhang F, Sun M, Han S, et al. Acupuncture for primary dysmenorrhea: an overview of systematic reviews. Evid Based Complement Alternat Med. 2018;2018:1–11. doi:10.1155/2018/8791538
12. Y-P Y, Ma L-X, Ma Y-X, et al. Immediate effect of acupuncture at Sanyinjiao (SP6) and Xuanzhong (GB39) on uterine arterial blood flow in primary dysmenorrhea. J Altern Complement Med. 2010;16:1073–1078. doi:10.1089/acm.2009.0326
13. Dong G, Tian Y, Han C, Li T. Advances in the study on acupuncture therapy for primary dysmenorrhea. Chin Med Pharm. 2020;10:33–35.
14. Zhang JJ, Wang J, Bai P, et al. Evidence-based clinical practice guideline of acupuncture and moxibustion for primary dysmenorrhea: development and characteristics. Zhongguo Zhen Jiu. 2019;39:1343–1346.
15. Jia X, Lijian P, Chuang L, Haoyang Z, Xiaodong L. Study on acupoint selection rule of primary dysmenorrhea and its mechanism by data mining. Modern Tradit Chin Med Mater Med World Scie Technol. 2017;19:804–810.
16. Lin M, Wei H, Zhao L, et al. Review on infrared temperature characteristics of acupoints in recent 10 years. Zhongguo Zhen Jiu. 2017;37:453–456.
17. Lin L-M, Wang S-F, Lee R-P, Hsu B-G, Tsai N-M, Peng T-C. Changes in skin surface temperature at an acupuncture point with moxibustion. Acupunct Med. 2013;31:195–201. doi:10.1136/acupmed-2012-010268
18. Pearson S, Colbert AP, McNames J, Baumgartner M, Hammerschlag R. Electrical skin impedance at acupuncture points. J Altern Complement Med. 2007;13:409–418. doi:10.1089/acm.2007.6258
19. Luo Y-N, Zhou Y-M, Zhong X, et al. Observation of pain-sensitive points in patients with knee osteoarthritis: a pilot study. Eur J Integr Med. 2018;21:77–81. doi:10.1016/j.eujim.2018.06.006
20. Ding N, Jiang J, Liu X, Xu Y, Hu J, Li Z. Laser speckle imaging of sensitized acupoints. Evid Based Complement Alternat Med. 2018;2018:1–9. doi:10.1155/2018/7308767
21. Xisheng F, Xiaoyi D, Lijia P, et al. An infrared thermographic analysis of the sensitization acupoints of women with primary dysmenorrhea. J Tradit Chin Med. 2022;42:825. doi:10.19852/j.cnki.jtcm.20220707.004
22. Yanfen S, Liangxiao M, Jiang Z, et al. Comparative study on skin temperature response to menstruation at acupuncture points in healthy volunteers and primary dysmenorrhea patients. J Tradit Chin Med. 2017;37:220–228. doi:10.1016/S0254-6272(17)30048-1
23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
24. Moreira DG, Costello JT, Brito CJ, et al. Thermographic imaging in sports and exercise medicine: a delphi study and consensus statement on the measurement of human skin temperature. J Therm Biol. 2017;69:155–162. doi:10.1016/j.jtherbio.2017.07.006
25. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–1805. doi:10.1177/0962280216669183
26. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:1–13. doi:10.1186/1471-2288-14-135
27. Li Z. Application of Low Frequency Electrical Stimulation in the Treatment of Primary Dysmenorrhea [Master’s thesis]. Jianghan University; 2022.
28. Du X. Evidence-Based Study on the Thermal Characteristics of Different Meridian Acupoints in the Same Spinal Cord Segment of Primary dysmenorrhea [Master’s thesis]. Hebei Medical University; 2018.
29. Wu G. Effect of Acupuncture at Sanyinjiao (SP6) on Infrared Temperature of Meridian Points in Patients with Primary Dysmenorrhea of Cold Coagulation Syndrome [Master’s thesis]. Beijing University of Chinese Medicine; 2016.
30. Wu G, Zhang P, Li J, et al. Effect of acupuncture at Sanyinjiao (SP6) on the infrared temperature of Guanyuan (CV4) and Sanyinjiao in dysmenorrhea patients. Shanghai J Acupunct Moxibust. 2016;35:631–635.
31. Zhang J. The acupoint surface temperature reaction the specificity research of menstrual cramps and primary dysmenorrhea [Master’s thesis]. Hebei Medical University; 2016.
32. Zhang D. Application of infrared thermography in studies of acupuncture mechanisms and meridians. Chin Acupunct Moxibust. 2004;24:37–42.
33. Fu Y, J-x N, Marmori F, Zhu Q, Tan C, Zhao J-P. Infrared thermal imaging-based research on the intermediate structures of the lung and large intestine exterior-interior relationship in asthma patients. Chin J Integr Med. 2016;22(11):855–860. doi:10.1007/s11655-016-2102-4
34. Arichi S, Arichi H, Toda S, Ihara N. Clinical observations on several meridian loci in chronic hepatitis and liver cirrhosis in comparison with those in female neurovegetative disorder, pregnancy, and the steroid side-effects syndrome. Am J Chin Med. 1979;7:157–170. doi:10.1142/S0192415X79000131
35. Li H, Shen X, Ying J, et al. Patients with clinical/radiological hyperplasia of mammary glands show pathological persistence of temperature of skin points. Anticancer Res. 2009;29:4697–4702.
36. Wang Y, Shen X, Ying J, et al. Pathologic analysis on hyperplasia of mammary gland with different syndromes based on infrared radiation temperature of acupoints. J Tradit Chin Med. 2012;32:382–387. doi:10.1016/S0254-6272(13)60042-4
37. Zheng J, Zhao Y, Wang Y, Hu S, Lu P, Shen X. The infrared radiation temperature characteristic of acupoints of mammary gland hyperplasia patients. Evid Based Complement Alternat Med. 2013;2013. doi:10.1155/2013/567987
38. Jo J, Kim H. Comparison of abdominal skin temperature between fertile and infertile women by infrared thermography: a diagnostic approach. J Therm Biol. 2016;61:133–139. doi:10.1016/j.jtherbio.2016.09.009
39. Ovechkin A, Kim K-S, Lee J-W, Lee S-M. Thermo-visual evaluation of the Yin-Tang acupuncture point for intracranial hypertension syndrome. Am J Chin Med. 2003;31:455–466. doi:10.1142/S0192415X03001041
40. Kwon YD, Lee JH, Lee MS. Increased temperature at acupuncture points induced by weight reduction in obese patients: a preliminary study. Int J Neurosci. 2007;117:591–595. doi:10.1080/00207450600773731
41. Jun E-M, Chang S, Kang D-H, Kim S. Effects of acupressure on dysmenorrhea and skin temperature changes in college students: a non-randomized controlled trial. Int J Nurs Stud. 2007;44:973–981. doi:10.1016/j.ijnurstu.2006.03.021
42. Williams KL. Temperature measurement in breast disease. Ann N Y Acad Sci. 1964;121:272–281. doi:10.1111/j.1749-6632.1964.tb13703.x
43. Ghosh A, Ray S, Garg M, Chowdhury S, Mukhopadhyay S. The role of infrared dermal thermometry in the management of neuropathic diabetic foot ulcers. Diabet Med. 2021;38:e14368. doi:10.1111/dme.14368
44. Stokholm J, Birkmose LKH, Csillag C, Kjær TW, Christensen T. Facial skin temperature in acute stroke patients with delirium-A pilot study. J Neurol Sci. 2021;431:120036. doi:10.1016/j.jns.2021.120036
45. Liu X, Feng J, Zhang R, Luan J, Wu Z. Quantitative assessment of bell’s palsy-related facial thermal asymmetry using infrared thermography: a preliminary study. J Therm Biol. 2021;100:103070. doi:10.1016/j.jtherbio.2021.103070
46. Tan H, Tumilty S, Chapple C, et al. Understanding acupoint sensitization: a narrative review on phenomena, potential mechanism, and clinical application. Evid Based Complement Alternat Med. 2019;2019:6064358. doi:10.1155/2019/6064358
47. Yang E, Lu W, Muñoz-Vergara D, et al. Skin temperature of acupoints in health and disease: a systematic review. J Integr Complement Med. 2022;28:552–568. doi:10.1089/jicm.2021.0437
48. Wang Y, Deng P, Li H. The research review of the infrared imaging technology in the field of traditional Chinese medicine. Infrared Technol. 2017;39:14.
49. Kang J, Lee N, Ahn Y, Lee H. Study on improving blood flow with Korean red ginseng substances using digital infrared thermal imaging and Doppler sonography: randomized, double blind, placebo-controlled clinical trial with parallel design. J Tradit Chin Med. 2013;33:39–45. doi:10.1016/S0254-6272(13)60098-9
50. Huang T, Huang X, Zhang W, Jia S, Cheng X, Litscher G. The influence of different acupuncture manipulations on the skin temperature of an acupoint. Evid Based Complement Alternat Med. 2013;2013. doi:10.1155/2013/905852
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.