Back to Journals » Nature and Science of Sleep » Volume 15
Secular Trends in Sleep Conditions in Chinese Elderly Individuals: A National Population-Based Study
Authors Pan XB, Wang HX, Cao YJ, Liu YY
Received 6 April 2023
Accepted for publication 30 June 2023
Published 7 July 2023 Volume 2023:15 Pages 555—566
DOI https://doi.org/10.2147/NSS.S416084
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Xing-Bing Pan,1,* Hong-Xia Wang,2,* Ya-Jing Cao,3 Yan-Yu Liu4
1Performance Appraisal Office, Children’s Hospital of Hebei Province, Shijiazhuang, People’s Republic of China; 2Department of Obstetrics and Gynecology, The Fourth Hospital of Hebei Medical University/The Tumour Hospital of Hebei Province, Shijiazhuang, People’s Republic of China; 3Institutes for Non-Communicable Chronic Diseases Control and Prevention, Hebei Provincial Centre for Disease Control and Prevention, Shijiazhuang, People’s Republic of China; 4Cancer Institute, The Fourth Hospital of Hebei Medical University/The Tumour Hospital of Hebei Province, Shijiazhuang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yan-Yu Liu, Cancer Institute, The Fourth Hospital of Hebei Medical University/The Tumour Hospital of Hebei Province, No. 12 Jiankang Road, Shijiazhuang, 050017, People’s Republic of China, Tel/Fax +86-311-8591-1878, Email [email protected]
Purpose: As one of the most rapidly aging countries in the world, the elderly population is expected to reach over 400 million in China by 2032. Many studies have suggested a positive association between sleep duration and adverse health events among elderly individuals. This study aimed to investigate the sleep conditions of Chinese elderly individuals between 2005 and 2018.
Patients and methods: Data for 53,013 elderly individuals were taken from five cycles of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) during 2005– 2018. Sex- and age-specific means and 95% confidence intervals (95% CIs) were used to estimate sleep duration trends. Changes in sleep patterns were explored during this period. The prevalence of short and long sleep durations was assessed and age-standardized by the 2010 census. Finally, self-reported sleep quality was used to determine sleep conditions from another perspective among elderly individuals.
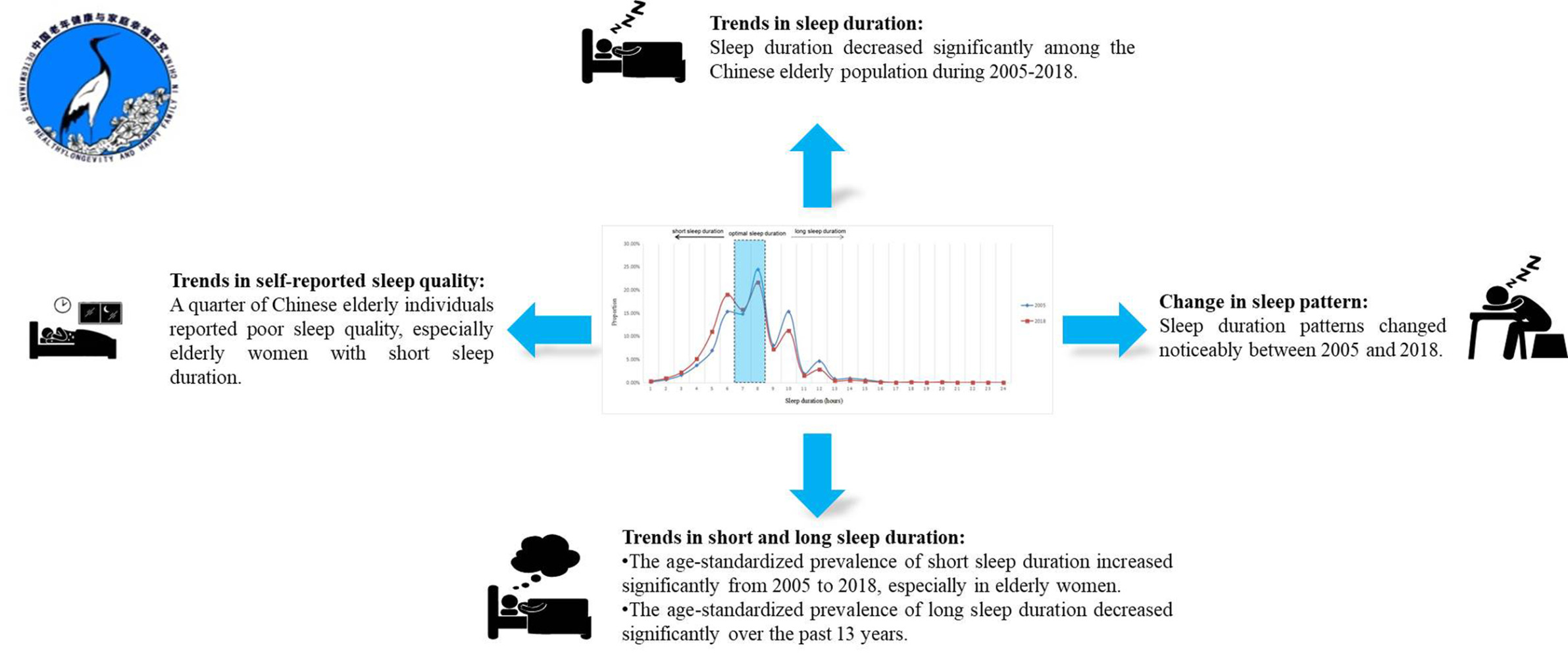
Results: The mean sleep duration decreased from 7.87 (95% CI: 7.83– 7.91) to 7.29 (95% CI: 7.25– 7.33) hours between 2005 and 2018. Changes in sleep duration patterns were found during the study period. The proportion of the elderly population who slept ≤ 6 hours increased and that of those who slept ≥ 9 hours decreased noticeably over the past 13 years. The age-standardized prevalence of short sleep duration increased from 32.7% (95% CI: 32.7– 32.9%) to 38.4% (95% CI: 38.3– 38.5%). A significant decrease was observed in the prevalence of long sleep duration.
Conclusion: Sleep conditions are gradually shifting toward a shorter sleep duration and poorer sleep quality among Chinese elderly individuals.
Keywords: trends, elderly population, sleep duration, sleep patterns, Chinese longitudinal healthy longevity survey
Graphical Abstract:
Introduction
World Health Statistics reported that people continued to live longer and lived more years in good health in 2022, leading to a rise in life expectancy across all national income groups.1 According to figures from the United Nations, there will be 2 billion elderly individuals aged ≥60 years and 1.5 billion elderly individuals aged ≥65 years around the world by 2050.2 Recent data reported by the National Bureau of Statistics of China showed that the elderly population aged ≥60 years and ≥65 years will be 280 million and 209 million accounting for 19.8% and 14.9% of the total population, respectively, by 2022. With this rate of growth, there will be 400 million elderly individuals aged ≥60 years and 300 million elderly individuals aged ≥65 years in China by 2032.3 China is only 0.2 percentage points from reaching the classification of a moderately aging country. Hence, it will be a vital public health task to focus on health conditions and relative risk factors among the Chinese elderly population in future years.
Sleep duration is an important indicator of sleep health. Secular trends in sleep duration are critical and helpful for understanding the latest sleep characteristics and changes in sleep patterns of the overall population or a specific population. However, the latest sleep characteristics and long-term changes in sleep patterns are unclear among the Chinese population, including the elderly population. There were 13 countries reporting trends in sleep duration among adults from the 1960s to 2000s: the self-reported average sleep duration of adults decreased in Japan, Russia, Finland, Germany, Belgium and Austria and increased in Bulgaria, Poland, Canada, France, Britain, Korea and the Netherlands.4 A recent study reported that sleep duration also increased among American adults between 2005 and 2018.5
The Healthy China Action Plan (2019–2030) advocated that a sleep duration between 7 and 8 hours per day is the optimal amount of sleep for Chinese adults. Meanwhile, the plan reminds us that short sleep duration is associated with an increased risk of cardiovascular disease, depression, diabetes and obesity.6 A large amount of evidence has also suggested that short sleep duration or insomnia is significantly associated with adverse health outcomes including stroke,7 hypertension,8 diabetes and diabetes-related complications,9 metabolic syndrome,10,11 dyslipidemia,12 cardiometabolic disease,13 neoplasms,14,15 fall risk,16 depression,17 premature death,18 and mental disorders that are susceptible to elderly individuals, including dementia,19,20 Alzheimer’s disease,21 and cognitive decline.22 In addition to short sleep duration, many reports of long sleep duration are concerning as long sleep has been linked with a number of adverse health outcomes including mortality, diabetes mellitus, cardiovascular disease, stroke, coronary heart disease, and obesity.23 Recently discovered evidence suggested that long sleep was also problematic for chronic kidney disease.24 However, the frequencies of short and long sleep durations are still unknown in the Chinese population, including the elderly population.
The aim of our study was to investigate the current sleep duration conditions and trends among the Chinese elderly population. Second, our study explored the changes in sleep patterns among the Chinese elderly population over the past 13 years. Third, we also investigated the prevalence and trends of short and long sleep duration by sex and age. Finally, we assessed the sleep conditions of the Chinese elderly population using self-reported sleep quality measures.
Methods
Study Design
The CLHLS is one of the world’s largest surveys on centenarians, nonagenarians and octogenarians, and it included 8 waves of in-depth surveys by the Research Center for Healthy Aging and Development, Peking University/National Development Academy between 1998 and 2018, using internationally compatible questionnaires. The first round of the CLHLS was conducted in 1998 and was followed by subsequent rounds in 2000, 2002, 2005, 2008, 2011, 2014, and 2018. The survey randomly selected 50% of the counties and cities in 23 provinces, accounting for 85% of the total population in China (approximately 1.1 billion people). The goal of the survey is to determine which factors, out of a large set of social, behavioral, and environmental risk factors, play an important role in healthy longevity. A detailed description of the CLHLS procedures has been published elsewhere.25,26 Ethical approval in this study was obtained from the Institutional Review Board (IRB) of Peking University (IRB00001052-11015), and written informed consent was obtained from all participants during the survey. All procedures involving human subjects were conducted in accordance with the guidelines laid down in the Declaration of Helsinki. Our study qualified for an exemption of ethical review of a local ethics committee according to Chinese legislation (http://www.gov.cn/zhengce/zhengceku/2023-02/28/content_5743658.htm).
Study Population
Our study used the definition of the elderly of World Health Organization (WHO) and defined the individuals aged ≥60 years old as the elderly. Participants aged 60–99 years old who reported sleep duration and quality were included for analysis in this study.
Definition of Sleep Duration and Quality
The CLHLS initially investigated the sleep duration and quality using the questionnaires in 2005. Two similar questions were utilized in the surveys. From 2005 to 2014, the questions “how long do you sleep normally?” and “how about the quality of your sleep?” were used to obtain their sleep duration and quality. However, the questions “how many hours do you usually sleep each day?” and “how is your sleep quality now?” were used to estimate their sleep duration and quality in 2018. Sleep hours were recorded in an integer. Self-reported sleep quality was categorized as “very good”, “good”, “so so”, “bad” and “very bad”.
Definition of Short Sleep and Long Sleep
At present, there is no consensus definition of short and long sleep for the Chinese elderly population. The American Academy of Sleep Medicine (AASM), the Sleep Research Society (SRS), and the American National Sleep Foundation recommended a sleep duration between 7 and 8 hours per day as appropriate for optimal health in older adults aged more than 65 years.27,28 The Healthy China Action Plan (2019–2030) also recommended a sleep duration between 7 and 8 hours per day as the optimal sleep duration for Chinese adults.6 However, this plan did not provide a concrete optimal sleep duration for elderly adults or cutoff values for short and long sleep durations. Taken together, sleep durations of ≤6 hours and ≥9 hours per day were regarded as short and long sleep durations under comprehensive consideration in this study. Previous studies have widely used the above definitions of short and long sleep durations.29,30 To explore whether there is a natural decrease in sleep duration with aging among elderly individuals, we also estimated the prevalence of short sleep duration defined as ≤5 hours. A previous study also used this definition to explore the association of short sleep duration and health outcome.31
Definition of Covariates
Sociodemographic characteristics and some diseases may influence sleep conditions in real life. Our study also collected sociodemographic information, including age, sex, smoking status, drinking status, education level, marital status, and urbanization. Smoking status was categorized as smoker and non-smoker according to smoke or not at present and smoked or not in the past. Drinking status was categorized as drinker and non-drinker according to drink or not at present and drank or not in the past. Education level was categorized as low level (no education, primary school but not graduated and primary school), middle level (middle school and high school) and high level (college or above). Marital status was categorized as currently married and not living with spouse (including separated, divorced, widowed and never married). Urbanization was categorized as urban and rural. According to the criteria of the Working Group on Obesity in China (WGOC), general obesity was defined as body mass index (BMI)≥28.0 kg/m2 and normal weight was defined as BMI <24.0 kg/m2.32 Abdominal obesity was defined as a WC ≥85 cm for men and WC ≥80 cm for women based on WHO recommendations for Asians.32 Hypertension was defined as self-reported hypertension and medicine use history as well the joint results of measurement (systolic blood pressure ≥140 mmHg, or diastolic blood pressure ≥90 mmHg). We also defined some diseases that are common to the elderly by their self-report and medicine use history, including diabetes, heart diseases, stroke and bronchitis.
Statistical Analyses
All statistical analyses were conducted using Stata software, version 15.0. Two-sided p values <0.05 indicated statistical significance. All analyses were stratified by sex and age. To understand the sleep situation of the elderly in each age group in detail, age was grouped into 60–64 years, 65–69 years, 70–74 years, 75–79 years, 80–84 years, 85–89 years, 90–94 years, and 95–99 years and according to sex in this study.
Trends in sleep duration were estimated and graphed using 2005–2018 CLHLS data. The proportion of individuals per sleep duration was developed to assess the changes in sleep duration patterns. Trends in the prevalence of short and long sleep were estimated among participants from 2005 to 2018 and were also assessed by linear-by-linear trend testing. Taking into account unequal probabilities of selection, the prevalence of short and long sleep durations was adjusted by the direct method for the 2010 census of the Chinese elderly population using the corresponding age groups. Multiple logistic regression models were utilized to further assess the changes in the prevalence of short and long sleep durations throughout the five waves of the CLHLS. Adjusted odds ratios (ORs)/age-specific ORs and their 95% CIs were used as measurements of changes in the prevalence of short and long sleep durations. OR and 95% CIs were adjusted by variables of sociodemographic characteristics and some diseases that may influence the sleep condition. In addition, 95% CI was calculated using robust clustered standard error at the provincial level to reduce the effect of intracluster correlation.33 Self-reported sleep quality was used to explore the sleep condition of Chinese elderly individuals from another perspective. In further studies, we compared the sleep quality in different sleep durations.
Results
Number of Participants
The detail selection of the study sample is shown in Supplementary Figure 1. Total of 65,428 participants were enrolled to attend an in-person follow-up visit from 2005 to 2018 CLHLS. Of 53,013 participants with data available, our study excluded 21 individuals aged less than 60 years old, and 10,901 individuals aged more than 100 years old, 1468 individuals with missing data on sleep duration and quality, and 25 individuals with extreme value of sleep duration and quality. Characteristics of Chinese elderly in the 2005–2018 CLHLS are presented in Supplementary Table 1.
Trends in Sleep Duration
Figure 1A shows weighted mean of sleep duration and 95% CI stratified by age and sex between 2005 and 2018. The weighted mean of sleep duration is estimated to be 7.69 (95% CI: 7.67–7.71) hours during 13-year period. The sleep duration decreased from 7.87 (95% CI: 7.83–7.91) to 7.29 (95% CI: 7.25–7.33) hours during the study period. The similar results were found among elderly men and elderly women, but a decrease of sleep duration among elderly women was higher than that among elderly men. Figure 1B presents the age-specific mean of sleep duration of overall elderly participants. Age-specific mean of sleep duration decreased in each age groups, especially elderly individuals in 85–89-year group. Figure 1C and D provided the age-specific mean of sleep duration of male and female elderly participants, respectively. However, the largest decrease happened in 85–89-year elderly men and 95–99-year elderly women.
Changes in Patterns of Sleep Duration
Figure 2 presents the proportion of individuals at each sleep duration group between 2005 and 2018. The unevenness of the curve reflected digital preference. Approximately 95% of Chinese elderly individuals slept between 4 and 12 hours per day. The proportion of the elderly individuals with sufficient sleeping (7–8 hours per day) decreased from 39.2% in 2005 to 37.3% in 2018, and the proportion of long sleep duration also decreased in this period. However, the proportion of elderly individuals with short sleep duration (≤6 hours per day) increased significantly over the past 13 years. But fortunately is the peak sleep duration did not shift and it was still 8 hours per day. To better exhibition the detail process of the evolution of sleep pattern, our study presented the distribution of the proportion of sleep duration among Chinese elderly individuals from 2005 to 2018 in Supplementary Figure 2.
 |
Figure 2 Distribution of the proportion of sleep duration among Chinese elderly between 2005 and 2018. |
Trends in Short and Long Sleep Duration
Table 1 shows the age-standardized and age-specific prevalence of short sleep duration striated by sex in Chinese elderly individuals from 2005 to 2018. After the standardization of the 2010 census, the age-standardized overall prevalence of short sleep duration increased from 32.7% (95% CI: 32.7–32.9%) in 2005 to 38.4% (95% CI: 38.3–38.5%) in 2018 (p < 0.001). In the analyses stratified by sex, the changes in the age-standardized prevalence of short sleep duration among elderly women were more striking than that among elderly men, with an increase from 32.2% (95% CI: 32.1–32.3%) to 42.3% (95% CI: 42.1–42.4%) among elderly women (p < 0.001) and from 33.0% (95% CI: 32.9–33.1%) to 34.6% (95% CI: 34.5–34.7%) among elderly men (p < 0.001). Similar figures were observed in overall participants except for individuals who are 60–64 year old. The highest prevalence of short sleep duration was in the group of 80–84 years old. Supplementary Table 2 provides the changes between the prevalence of short sleep duration (≤6 hours/day) and survey year from multiple logistic regression models. In further analyses, we re-estimated the prevalence of short sleep duration (≤5 hours per day) and the changes of this prevalence during the study period (Supplementary Tables 3 and 4).
 |
Table 1 Age-Standardized and Age-Specific Prevalence of Short Sleep Duration (≤6 Hours/Day) Striated by Sex in Chinese Elderly Population: CLHLS 2005–2018 |
Table 2 presents the age-standardized and age-specific prevalence of long sleep duration (≥9 hours/day) striated by sex in Chinese elderly population from 2005 to 2018. Age-standardized prevalence of long sleep duration decreased from 24.8% (95% CI: 24.7–24.9%) in 2005 to 15.9% (95% CI: 15.8–16.0%) in 2018 (p < 0.001), which decreased 31.8% during 13-year period (adjusted OR = 0.682, 95% CI: 0.645–0.721, p < 0.001). Supplementary Table 5 provides the results of changes in long sleep prevalence by multiple logistic models and reported a higher decrease among elderly women than that among elderly men.
 |
Table 2 Age-Standardized and Age-Specific Prevalence of Long Sleep Duration (≥9 Hours/Day) Striated by Sex in Chinese Elderly Population: CLHLS 2005–2018 |
Trends in Self-Reported Sleep Quality
Figure 3 presents the trends in proportion of self-reported sleep quality in accordance with sex and age during 2005–2018. Figure 3A is for elderly men and Figure 3B is for elderly women. The proportions of good sleep quality (“very good” and “good”) decreased from 63.9% to 51.0%, but poor sleep quality (“bad” and “very bad”) increased from 10.8% to 15.2%. Supplementary Figure 3 presents the comparison of the sleep quality striated by sleep duration in further study. The proportion of poor sleep quality was noticeably higher in individuals with short sleep duration, and it among elderly women was higher than that among elderly men.
 |
Figure 3 Percentage of sleep quality by age among elderly men (A) and elderly women (B) in China during 2005–2018. |
Discussion
A downward trend in sleep duration was observed among Chinese elderly individuals between 2005 and 2018. Sleep duration patterns changed noticeably during the study period. The age-standardized prevalence of short sleep duration among elderly women was higher than that among elderly men, and a higher increase in sleep duration was found among elderly women. The highest prevalence of short and long sleep was found in the 80-84-year and 95-99-year age groups, respectively. However, the largest increase in short sleep duration prevalence and the largest decrease in long sleep duration prevalence were found in the 85-89-year-old group. Finally, self-reported sleep quality among elderly men was better than that among elderly women.
Trends in Sleep Duration
Few studies have focused on sleep duration in Chinese elderly population. The White Book on Sleep in China initiated by the Chinese Sleep Research Society (CSRS) annually reported sleep conditions among Chinese individuals starting in 2014. In 2022, the book reported that the mean sleep duration was 6.5085 hours among Chinese elderly individuals aged ≥61 years and the proportion of sleep duration ≥6 hours per day was 59.7%.34 However, the White Book interviewed participants through self-report questionnaires via the internet. For this reason, only approximately 272 (3%) elderly individuals aged ≥61 years participated in this survey in 2022, thus demonstrating that many elderly participants may be ignored due to barriers to internet use. Hence, the results of the White Book may not reflect the real sleep conditions of Chinese elderly individuals.
In contrast, our study used a household survey and an in-person follow-up visit and collected a large sample size of elderly individuals. The CLHLS included sufficient sample sizes for the oldest old with all age groups including 80+ and 90+ years to explore the real sleep condition among Chinese elderly individuals. The results from this study showed that sleep duration decreased among the Chinese elderly population between 2005 and 2018. Contrary to common sense, our study found that sleep duration in elderly individuals did not decrease with aging alone, and sleep duration among elderly individuals aged ≥85 years was longer than that among elderly individuals aged ≤85 years. Sleep duration even increased in the elderly aged 85–99 years old according to the survey. Many studies in other countries have provided the trends in sleep duration, but few studies have focused on sleep duration in the elderly population, especially the oldest old, who are the most susceptible to sleep disorders.4,5 Our study filled in the data gap for the characteristics and change law of sleep duration among the elderly population and provided evidence of sleep conditions in a large sample size among oldest old individuals.
Changes in Patterns of Sleep Duration
Sleeping patterns changed dramatically in Chinese elderly individuals during 2005–2018. Sleep duration in the Chinese elderly individuals was shifting toward a trend of shorter sleep durations. A similar trend was also found in American adults aged 18–85 during 2005–2017, but this trend changed more slowly than in the Chinese elderly population due to the modified effect of young adults in this study.35 It is worth emphasizing that changes in sleep duration, especially a decrease in sleep duration, may be associated with higher risks of negative health outcomes such as hypertension.36,37 The latest study found new evidence and suggested that sleep irregularity, particularly sleep duration irregularity, was associated with an increased risk of several measures of subclinical atherosclerosis and that sleep regularity may be a modifiable target for reducing atherosclerosis risk.38 Therefore, sufficient and regular sleep duration were both vital factors for maintaining good sleep health.
Trends in Short and Long Sleep Duration
Age-standardized prevalence reached 38.4% (95% CI: 38.3–38.5%) in 2018. The prevalence of short sleep duration among Chinese elderly individuals was noticeably higher than that among American elderly individuals in a similar period. However, conclusions regarding trends in short sleep prevalence among American adults are controversial. The age-adjusted prevalence of short sleep in the National Health Interview Survey (NHIS) increased from 28.6% in 2004 to 32.9% in 2017, but the age-adjusted prevalence of short sleep in the National Health and Nutrition Examination Survey (NHANES) decreased from 35.7% in 2005 to 35.1% in 2014.5,35 A high prevalence of short sleep duration, a trend which has continually increased during the past 13 years, should be given more attention by healthcare providers.
It was fortunate that the prevalence of long sleep duration decreased from 24.8% in 2005 to 15.9% in 2018 among Chinese elderly individuals over the past 13 years. According to the NHIS, the age-adjusted prevalence of long sleep decreased from 8.5% in 2005 to 7.4% in 2017.35 Although the lower prevalence in America may be attributed to including young adults in the analysis, the prevalence of 15.9% still meant that there will be 63.6 million Chinese elderly individuals aged ≥60 with long sleep duration in 2032. Our study found that the prevalence of long sleep duration among elderly men was higher than among elderly women, but the decreasing rate was faster among elderly women. The highest prevalence of long sleep durations was found in the age group of 95–99 years, and a trend of increasing prevalence with age was observed in all age groups. Disparities in the prevalence of long sleep durations between elderly men and women were another concerning point for health care providers.
Trends in Self-Reported Sleep Quality
Self-reported sleep quality is an intuitive and comprehensive index for reflecting sleep quality and another commonly used index of sleep condition in addition to sleep duration. Previous studies have shown that poor sleep quality is associated with an increased risk of adverse health outcomes.29 In 2022, the White Book on Sleep in China reported that a total of 21% of the elderly population reported “frequent insomnia”.34 Among American elderly individuals, 36.4% (95% CI: 30.9–41.8%) reported trouble sleeping in 2018.5 In our study, the prevalence of poor sleep quality was 15.2% in 2018 and was higher in elderly women (18.4%) than in elderly men (12.7%). A misunderstanding of sleep duration may occur when viewed under the impression that sufficient sleep duration is equal to a total sleep time of 7–8 hours per day. Many elderly individuals have napping habits in the daytime due to poor sleep quality at night. In fact, this sleep pattern may be bad for health although they slept for 7–8 hours per day. Available evidence suggested that significant dose response associations were found between daytime napping and higher odds of diabetes, dyslipidemia, metabolic syndrome, and mortality among older adults aged >60 years.39 The White Book on Sleep in China provided some advice for improving the sleep quality of elderly individuals in the nighttime to avoid habitual napping in the daytime, such as sleep medication, listening to music, accompanying sleep, changing beddings, sharing sleep knowledge and reminding elderly individuals to go to sleep on time.34 Taken together, good sleep should not be defined only as a total of 7–8 hours of sleep duration per day; it needs to include good sleep quality at night and a stable sleep pattern as well.
Strengths and Limitations
The present study first provides the secular trends in sleep duration and quality in large samples of Chinese elderly individuals over a period of 13 years which, notably, included a large number of oldest old individuals in the analyses. In fact, the proportional sampling design has resulted in insufficient sample sizes for the oldest old population in the few elderly population surveys that have been conducted. Almost all census tabulations in China and other developing countries grouped 85+, 80+, or even 65+ as one category, which suppresses the heterogeneous characteristics of the oldest old population. Hence, CLHLS provided a great opportunity to explore the sleep conditions of oldest old individuals. However, there were also some potential limitations. First, sleep duration and quality were self-reported, which may misestimate the results due to the use of retrospective questions. On the one hand, many elderly participants aged 80–99 were included in our study, who may have been more strongly subjected to information and recall bias than younger participants. The survey was actively coordinated by the interviewees and their families. Additionally, a previous study in America showed that self-reported habitual sleep duration is moderately correlated with objectively measured sleep duration.40 On the other hand, participants are more likely to recall even numbers (6, 8 and 10) than odd numbers (7, 9 and 11). However, such sleep duration recall bias would not influence the analysis of sleep trends and patterns of our study because this occurred in all waves of surveys.41 Finally, we were unable to include some covariates that could potentially affect sleep health, such as stress and depression, in the analyses.42
Conclusions
Our study filled in the data gap for the characteristics and change law of sleep duration among the elderly population and provided evidence of sleep conditions in a large sample size among oldest old individuals. A downward trend in sleep duration was observed among Chinese elderly individuals between 2005 and 2018. Their sleep duration patterns have changed noticeably over the past 13 years. Sleep duration in elderly individuals did not decrease with aging alone. Sleep conditions in Chinese elderly individuals, especially elderly women and oldest old individuals, more attention should be paid to.
Ethics Approval and Consent to Participate
Ethical approval in this study was obtained from the Institutional Review Board (IRB) of Peking University (IRB00001052-11015). All participants agreed to participate in this study and provided informed written consent.
Acknowledgments
Thanks for the data derived from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), which was supported by United States Department of Health and Human Services. National Institutes of Health, National Institute on Aging (R01AG023627), National Natural Science Foundation of China (71233001), National Basic Research Program of China (2013CB530700).
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. World health statistics 2022: monitoring health for the SDGs, sustainable development goals. Available from: www.who.int/.
2. United Nations. World population prospects; 2022. Available from: https://population.un.org/.
3. National Bureau of Statistics of China. Demographic bulletin; 2022. Available from: www.stats.gov.cn/.
4. Bin YS, Marshall NS, Glozier N, et al. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 2012;16(3):223e230. doi:10.1016/j.smrv.2011.07.003
5. Wang S, Rossheim ME, Nandy RR. Trends in prevalence of short sleep duration and trouble sleeping among US adults, 2005–2018. Sleep. 2023;46(1). doi:10.1093/sleep/zsac231
6. Chen P, Li F, Harmer P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. 2019;4(9):e447. doi:10.1016/S2468-2667(19)30160-4
7. Eguchi K, Hoshide S, Ishikawa S, et al. Short sleep duration is an independent predictor of stroke events in elderly hypertensive patients. J Am Soc Hypertens. 2010;4:255–262. doi:10.1016/j.jash.2010.09.001
8. Bock JM, Vungarala S, Covassin N, et al. Sleep duration and hypertension: epidemiological evidence and underlying mechanisms. Am J Hypertens. 2022;35(1):3–11. doi:10.1093/ajh/hpab146
9. Schipper SBJ, Van Veen MM, Elders PJM, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia. 2021;64(11):2367–2377. doi:10.1007/s00125-021-05541-0
10. Xie J, Li Y, Zhang Y, et al. Sleep duration and metabolic syndrome: an updated systematic review and meta-analysis. Sleep Med Rev. 2021;59:101451. doi:10.1016/j.smrv.2021.101451
11. Che T, Yan C, Tian D, et al. The association between sleep and metabolic syndrome: a systematic review and meta-analysis. Front Endocrinol. 2021;12:773646.
12. Du S, Su Y, Zhang D, et al. Joint effects of self-reported sleep and modifiable physical activity on risk of dyslipidaemia in women aged 45–55 years: a cross-sectional study. BMJ Open. 2022;12(1):e049351. doi:10.1136/bmjopen-2021-049351
13. Kwok CS, Kontopantelis E, Kuligowski G, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. 2018;7(15):e008552. doi:10.1161/JAHA.118.008552
14. Wong ATY, Heath AK, Tong TYN, et al. Sleep duration and breast cancer incidence: results from the million women study and meta-analysis of published prospective studies. Sleep. 2021;44(2):zsaa166. doi:10.1093/sleep/zsaa166
15. Stone CR, Haig TR, Fiest KM, et al. The association between sleep duration and cancer-specific mortality: a systematic review and meta-analysis. Cancer Causes Control. 2019;30(5):501–525. doi:10.1007/s10552-019-01156-4
16. Han C, An J, Chan P. The influence of probable rapid eye movement sleep behavior disorder and sleep insufficiency on fall risk in a community-dwelling elderly population. BMC Geriatr. 2021;21(1):606. doi:10.1186/s12877-021-02513-2
17. He C, Xiao L, Xu J, et al. Effect of sleep deprivation plus existing therapies on depression: a systematic review and meta-analysis of randomized controlled trials. Int J Psychophysiol. 2023;184:1–11. doi:10.1016/j.ijpsycho.2022.11.016
18. Wang H, Sun J, Sun M, et al. Relationship of sleep duration with the risk of stroke incidence and stroke mortality: an updated systematic review and dose-response meta-analysis of prospective cohort studies. Sleep Med. 2022;90:267–278. doi:10.1016/j.sleep.2021.11.001
19. Sabia S, Fayosse A, Dumurgier J, et al. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun. 2021;12(1). doi:10.1038/s41467-021-22354-2
20. Fan L, Xu W, Cai Y, et al. Sleep duration and the risk of dementia: a systematic review and meta-analysis of prospective cohort studies. J Am Med Dir Assoc. 2019;20(12):1480–7.e5. doi:10.1016/j.jamda.2019.06.009
21. Zhang Y, Ren R, Yang L, et al. Sleep in Alzheimer’s disease: a systematic review and meta-analysis of polysomnographic findings. Transl Psychiatry. 2022;12(1):136. doi:10.1038/s41398-022-01897-y
22. Wu L, Sun D, Tan Y. A systematic review and dose-response meta-analysis of sleep duration and the occurrence of cognitive disorders. Sleep Breath. 2018;22:805–814. doi:10.1007/s11325-017-1527-0
23. Jike M, Itani O, Watanabe N, et al. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev. 2018;39:25–36. doi:10.1016/j.smrv.2017.06.011
24. Zhang F, Wang H, Huang L, et al. Effect of exercise interventions for sleep quality in patients with chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol. 2022;55(5):1193–1204. doi:10.1007/s11255-022-03413-z
25. Gu D, Feng Q, Zeng Y. Chinese Longitudinal Healthy Longevity Study. Singapore: Springer; 2017.
26. Yi Z, Vaupel JW, Zhenyu X, et al. Chinese Longitudinal Healthy Longevity Survey (CLHLS), 1998–2005; 2009.
27. Watson NF, Badr MS, Belenky G, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. J Clin Sleep Med. 2015;11(8):931–952.
28. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–243. doi:10.1016/j.sleh.2015.10.004
29. Gao C, Guo J, Gong TT, et al. Sleep duration/quality with health outcomes: an umbrella review of meta-analyses of prospective studies. Front Med. 2021;8:813943.
30. Itani O, Jike M, Watanabe N, et al. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017;32:246–256. doi:10.1016/j.sleep.2016.08.006
31. Ren LH, Wu Y, Zhao YX, Zhao X. Correlation between sleep duration and hypertension: a dose-response meta-analysis. J Hum Hypertens. 2019;33(3):218–228. doi:10.1038/s41371-018-0135-1
32. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
33. Simcoe T. XTPQML: Stata Module to Estimate Fixed-Effects Poisson (Quasi-ML) Regression with Robust Standard Errors. Statistical Software Components; 2007.
34. Chinese Sleep Research Society. White book on sleep in China; 2022. Available from: http://www.zgsmyjh.org/.
35. Connor M, Sheehan Stephen E, Frochen Katrina M, et al. Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National health interview survey, 2004–2017. Sleep. 2019;42(2):zsy221. doi:10.1093/sleep/zsy221
36. Huang L, Long Z, Lyu J, et al. The associations of trajectory of sleep duration and inflammation with hypertension: a longitudinal study in China. Nat Sci Sleep. 2021;13:1797–1806.
37. Wang Y, Hou W, Siddiqi SM, Sun C, Han T, Yang J. Association of sleep trajectory in adulthood with risk of hypertension and its related risk factors: the China health and nutrition survey. J Clin Sleep Med. 2020;16(4):515–521. doi:10.5664/jcsm.8254
38. Full KM, Huang T, Shah NA, et al. Sleep irregularity and subclinical markers of cardiovascular disease: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2023;12(4):e027361. doi:10.1161/JAHA.122.027361
39. Sun JH, Ma CW, Zhao M, et al. Daytime napping and cardiovascular risk factors, cardiovascular disease, and mortality: a systematic review. Sleep Med Rev. 2022;65:101682. doi:10.1016/j.smrv.2022.101682
40. Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. doi:10.1097/EDE.0b013e318187a7b0
41. Kirkegaard EOW. What exactly is age heaping and what use is it? Clear language. Clear Mind. 2015;2015:1.
42. Lu L, Geng Q, Wang JA, et al. Expert consensus on the diagnosis and treatment of insomnia with depression and anxiety in Chinese adults. Chin J Neurol. 2022;8(53):564–574.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

