Back to Journals » Journal of Pain Research » Volume 16
Scientific Knowledge Graph of Dysmenorrhea: A Bibliometric Analysis from 2001 to 2021
Authors Fang X , Liu H, Wang M , Wang G
Received 16 May 2023
Accepted for publication 5 August 2023
Published 22 August 2023 Volume 2023:16 Pages 2883—2897
DOI https://doi.org/10.2147/JPR.S418602
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ellen M Soffin
Xiaoting Fang,1,* Haijuan Liu,1,* Mina Wang,1 Guohua Wang2
1Graduate School, Beijing University of Chinese Medicine, Beijing, China; 2Gynecology, Beijing University of Chinese Medicine Third Affiliated Hospital, Beijing, China
*These authors contributed equally to this work
Correspondence: Guohua Wang; Mina Wang, Email [email protected]; [email protected]
Purpose: This study aims to help researchers master the most active hotspots and trends quickly through bibliometric analysis in the field of dysmenorrhea.
Methods: We retrieved literature on Web of Science from 2001 to 2021, and bibliometric analysis software CiteSpace was used in combination with VOSviewer.
Results: We finally acquired 944 papers and an upward trend in articles continued in this field overall. Through the map, China contributed the most, followed by the USA and Turkey. For institutions, Beijing University of Chinese Medicine in China contributed the most, followed by National Yang-Ming University in Taiwan, China. Hsieh JC and Hellman KM were both the most prolific authors with 14 articles. Five major research groups, respectively, with Hsieh JC, Hellman KM, Zhu J, Liang F and Dun W were the key group. Dawood MY was the most dominant author and most frequently cited author. The Cochrane Database of Systematic Reviews Journal was the most productive, and the Fertility and Sterility Journal was the most cited. Advances in pathogenesis and management for primary dysmenorrhea written by Dawood MY was most cited and influential. Pathophysiology, the potential central mechanism, syndrome, evaluation index, diagnosis of adenomyosis-associated dysmenorrhea, treatment, etc., were the main trends and hotspots.
Conclusion: Dysmenorrhea research has received a lot of attention from scholars. Strengthening international cooperation may promote the development of this field. The pathophysiology of dysmenorrhea, its impact on public health and its treatment are current research hotspots and are likely to be the focus of future study.
Keywords: scientific knowledge graph, dysmenorrhea, bibliometric analysis, trends, hotspots
Introduction
Dysmenorrhea, including primary and secondary, is characterized by pain in the lower abdomen that occurs before or during menstruation. Patients with primary dysmenorrhea (PDM) report suffering from menstrual pain without organic causes,1 while secondary dysmenorrhea is related to organic diseases of the pelvic cavity, such as pelvic inflammatory disease or adenomyosis.2 Due to the different definitions of dysmenorrhea and differences in countries and cultures, the prevalence of dysmenorrhea reported was inconsistent. A systematic review published in 2013 highlighted that among the limited studies identified, the prevalence of dysmenorrhea ranged from 16% to 91%. Among them, 2–28% of women reported severe pain or pain restricting daily life.3 It was also reported that menstrual cramps cost 600 million hours of lost work time and $2 billion in lost productivity each year, which has affected national economy.4
The etiology of primary dysmenorrhea is not well defined, but the most recognized explanation attaches dysmenorrhea to the increase of prostaglandins (PGs), particularly PGF2α,5 which causes a uterine contraction to limit blood flow and results in cramps.6 In addition to PGs, vasopressin has also been implicated in the etiology of primary dysmenorrhea, but the involvement of vasopressin remains controversial. Besides, menstrual pain may lead to the development of central sensitivity to pain. PDM was found to be associated with abnormal metabolic changes in several areas of the brain involved in pain processing.7 Recently, researchers have even suggested that dysmenorrhea may put women in a state of chronic pain and the chronic pain may lead to an effect on the central nervous system, and then causes pathological changes in brain anatomy structure and function, further aggravating PDM.6
Dysmenorrhea has a direct negative impact on the quality of life of the patients, especially during menstruation. Menstrual pain is not only a sensory experience, but also affects the emotional state of the patients, causing psychological distress or emotional problems; and these psychological stresses can in turn exacerbate the level of pain in dysmenorrhea patients. Also, depression and anxiety are closely associated with menstrual pain. Dysmenorrhea can also have an impact on sleep. Indeed, women who experience severe PDM may have worse sleep quality.8,9
The most prescribed medications for the treatment of dysmenorrhea are nonsteroidal anti-inflammatory drugs (NSAIDs) which are prostaglandin synthase inhibitors. The efficacy of various formulations of NSAIDs for dysmenorrhea is comparable, with 64–100% of women experiencing successful pain relief. However, 15% of women of all ages with dysmenorrhea do not respond to or are intolerant of PG inhibitors. For these women, oral contraceptives are often used as second-line therapy. The synthetic hormones in oral contraceptives inhibit ovulation and reduce endometrial thickness, thereby reducing menstrual flow, PG synthesis, and dysmenorrhea. Other current treatments for dysmenorrhea include percutaneous electrical nerve stimulation, transdermal nitroglycerin patches, and surgical interventions such as laparoscopic uterosacral nerve ablation procedures. However, these treatments are not considered effective enough to be widely used in clinical practice. Many women also use other non-pharmacologic therapies to manage menstrual discomfort, including the use of heating pads to relieve cramps, extra bed rest or sleep, physical activity, and so on. However, most non-pharmacologic therapies have been reported to have an average effectiveness rate of less than 40%. The wide variation in the efficacy of various non-pharmacological treatments suggests that the efficacy of these approaches varies from person to person.7
Dysmenorrhea is an important public health issue, and in the 21st century, the rapid accumulation of knowledge makes it increasingly difficult to identify key information and keep up with the latest research hotspots, especially for those new to the field. Researchers often need to review a large amount of literature to grasp the state of research in the field. Although research on dysmenorrhea has been widely conducted, various scientific issues related to dysmenorrhea still require continuous academic exploration. Therefore, it is necessary to comprehensively assess and summarize the research findings in this field to prepare for further studies. Bibliometrics analysis has developed rapidly in recent years, which provides convenience for literature reading and effectively solves the abovementioned problems. Bibliometric analysis software CiteSpace and VOSviewer are commonly used in bibliometrics.10 This study collected the papers on dysmenorrhea published in Web of Science database in the past more than 20 years and made a bibliometric analysis based on the literature. Our study aims to systematically comb through the literature, help researchers quickly grasp the current state of research, provide scholars and clinicians with important information in the field of dysmenorrhea, and help them understand the most active hotspots and trends.
Methods
Source of Literature
To search for comprehensive literature, we gained the subject words of “dysmenorrhea” by searching the MeSH Database in PubMed. Considering that the Web of Science Core Collection (WOSCC) is one of the most suitable database collections for bibliometrics,11 we retrieved literature on WOSCC. The search and screening were conducted by 2 researchers, and the search strategy was formulated in consultation. We entered the Web of Science (WOS) database from the Peking University Library database in China. Then, we searched WOSCC as the most comprehensive database, selecting Science Citation Index Expanded (SCI-Expanded) as well as Social Sciences Citation Index (SSCI), using its advanced search function with keywords and MeSH terms: TS=“Dysmenorrhea” OR “Menstrual Pain” OR “Menstruation, Painful” OR “Menstrual Pains” OR “Pains, Menstrual” OR “Menstruations, Painful” OR “Painful Menstruation” OR “Painful Menstruations” OR “Dysmenorrheas” OR “Pain, Menstrual”. Without language limitation, the literature ranged from Jan 1st, 2001 to Dec 31st, 2021 in time. Initially, we obtained 5316 records, and screened them through the document type filter. With only original research articles and review articles included, we retrieved 4999 records. In order to analyze highly relevant literature, we manually read the titles and abstracts one by one, and removed literature that was unrelated to the research topic. The literature was screened back-to-back, and when we encountered disagreement, we reached agreement after discussion with a third party. After CiteSpace removed duplication, we finally acquired 944 records (Figure 1), which was the whole data for analysis. The included articles were exported in the RefWorks format to a plain text file.
Analysis Software
Commonly used software for bibliometric analysis includes CiteSpace and VOSviewer. VOSviewer has more advantages in visualization, and can make more beautiful visual graphs, while CiteSpace is better at keyword analysis, and can detect research hotspots and research trends.12 For functional complementarity, CiteSpace is used in combination with VOSviewer in this study. The used software versions are CiteSpace 6.1.R3 and VOSviewer 1.6.18.
Data Analysis
The RefWorks file was imported into VOSviewer 1.6.18 software for bibliometric visualization analysis, involving countries, institutions, authors, and co-cited authors, cited references as well as keywords, and was also imported into the CiteSpace 6.1.R3 software for keyword detection with the strongest citation bursts and keyword cluster analysis. The CiteSpace software parameters were set as follows: Time slicing (from 2001–01 to 2021–12), Years Per Slice (1 year), Node types (choosing keyword), Pruning (pruning sliced networks, pathfinder and pruning the merged networks), and other parameters were set according to the initial software settings. It should be noted that Scimago Graphical mapping software was used to better present the global research geographically when drawing the international cooperation network visualization map.
Research Ethical Review
An ethical review is not required because all the data used in the study were downloaded from public databases, so the study did not involve direct interactions with animals or humans.
Results
Analysis of Total Number of Publications
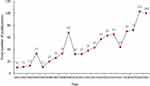
The research trend over the last 21 years in dysmenorrhea can be evaluated through the number of papers each year. As shown in Figure 2, although the publications increased suddenly in 2004 and 2009, and reduced suddenly in 2017, an upward trend in articles continued in this field overall, and since 2019, the annual output showed explosive growth and reached the highest publications of 103 papers in 2020.
Analysis of Countries
Articles on Dysmenorrhea came from 68 countries. Through the map (Figure 3), China contributed the most, with 197 articles (20.9%), followed by The United States with 163 papers (17.3%) and Turkey with 84 papers (8.9%), while other countries mainly Europe and the Middle East. China had some cooperation with The United States but not so close, and had research cooperation relationships with many other countries, like Australia, Japan, Brazil and so on, while Turkey cooperated only with Iran. Also, through the map, we can find that most European countries conducted close cooperation with each other in this field, which may be the result of the same or nearby region. Through the map, it is indicated that more collaboration in research on dysmenorrhea occurs between countries with higher economic power.
Analysis of Institutions
In this study, 1203 institutions are researching dysmenorrhea in total. The cooperation relationship between institutions is shown in Figure 4. Beijing University of Chinese Medicine (BUCM) in China contributed the most with 29 articles, followed by National Yang-Ming University (NYMU) in Taiwan, China with 21 articles, and Chengdu University of Traditional Chinese Medicine (CDUTCM) in China, with 18 papers. The top 12 most prolific institutions are shown in Table 1, from which we can find that most institutions are universities with abundant scientific research resources, mostly in China and the USA. Colleges from the same country conducted relatively close cooperation, for example, BUCM, at the core, had close cooperation with CDUTCM, Xi ‘an Jiaotong University (XJTU), Jiangxi University of Traditional Chinese Medicine (JXUTCM) and Tianjin University of Traditional Chinese Medicine (TJUTCM) in Dysmenorrhea. However, international cooperation was limited. We found CDUTCM had cooperation with Charite-Medical University of Berlin (Germany), University of Otago (New Zealand), University of Maryland (The United States), and so on. However, a large-scale transnational cooperative research network was not found, which suggested the leading influence of universities in China is prominent in this field, while on the other hand, transnational cooperation among institutions is lacking.
 |
Table 1 Top 12 Institutions in Dysmenorrhea |
Analysis of Authors and Co-Cited Authors
There are 3805 authors researching dysmenorrhea in total. Top 10 authors are presented in Table 2. Hsieh JC and Hellman KM were both the most prolific author with 14 articles. Through the author cooperation relationship map shown in Figure 5, we can find 5 major research groups, respectively with Hsieh JC, Hellman KM, Zhu J, Liang F and Dun W, as the core of the group. Each group had close research on dysmenorrhea, but the cooperation between groups was not so close. There was cooperation between the groups with Smith CA, Zhu J, Liang F as the core.
 |
Table 2 Top 10 Authors and Co-Cited Authors of Dysmenorrhea |
When the papers of two authors are cited by another author at the same time, there is a co-citation relationship between the two authors. The more frequently these two authors are cited, the closer their academic relationship is. The higher the citation of co-cited authors, the greater their contribution to the field is. The top 10 co-cited authors can also be seen in Table 2 and Figure 6 displays a cooperative network map of co-cited authors. We found that Dawood MY with 488 citations was cited most frequently so he was the most dominant author.
Analysis of Journals and Co-Cited Journals
A total of 957 journals published articles about dysmenorrhea and the visualization map is shown in Figure 7. We listed the top 10 journals of dysmenorrhea in Table 3. According to the 2023 Journal Citation Reports, we found that among these journals, the Cochrane Database of Systematic Reviews Journal was with the highest impact factor (IF), which was 8.4. The average IF of the top 10 journals was 4.36. Otherwise, the Cochrane Database of Systematic Reviews Journal was also the most productive journal with 73 articles, followed by the Fertility and Sterility Journal with 69 articles and the Pediatric and Adolescent Gynecology Journal with 66 articles. The cited references were published in 15, 821 journals and the cooperation visualization map are shown in Figure 8. We also listed the top 10 co-cited journals in Table 4. It is easy to find through this table that the most cited journal is Fertility and Sterility (IF 6.7, Q1) with 5479 citations, indicating that this journal was representative and persuasive in this research field and could provide strong evidence for our research in this field.
 |
Table 3 Top 10 Journals of Dysmenorrhea |
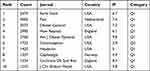 |
Table 4 Top 10 Co-Cited Journals of Dysmenorrhea |
Analysis of Cited References
A total of 19,058 references were cited in the 944 included articles. The 10 most cited papers, including 5 reviews and 5 clinical studies, are shown in Table 5. The reviews covered prevalence, risk factors, diagnosis, treatment and so on, and the studies focused on epidemiology, mainly about prevalence and risk factors. Since the prevalence of dysmenorrhea is difficult to determine because of different definitions, in women of childbearing age, the prevalence of dysmenorrhea varies between 16% and 91%, which may account for the high citation of the epidemiological researches.3 Advances in pathogenesis and management for primary dysmenorrhea written by Dawood MY was most cited of 197 citations and most influential, which indicates the importance of pathogenesis and management in dysmenorrhea.
 |
Table 5 Top 10 Cited References of Dysmenorrhea |
Analysis of Keywords
In this study, there are 2966 keywords extracted in total. As shown in Figure 9, “dysmenorrhea” appears most frequently, followed by “women” “primary dysmenorrhea” “pain” “prevalence” “management” “menstrual pain” “endometriosis” “impact” “symptoms”. All the extracted keywords formed a total of 12 clusters (Figure 10) according to similarity, showing the knowledge structure of this field to a certain extent. Based on the 12 clusters, it can be found that the research hotspots of dysmenorrhea can be divided into several aspects: pathophysiology (nitric oxide), the potential central mechanism (functional connectivity), syndrome (menstrual cycle, menstrual pain, pelvic pain, and premenstrual syndrome), evaluation index (severity, intrauterine pressure), diagnosis to adenomyosis-associated dysmenorrhea (annexin a2), treatment (complementary therapies, Xuanzhong [GB39]). Figure 11 shows top 25 keywords with the strongest citation bursts, which display changes in the research hotspots over time visually. Focuses of researchers in recent five years are “population”, “herbal medicine”, “functional connectivity” “clinical trial” “chronic pain” “systematic review” “quality of life” “pain management” and “medicine”.
 |
Figure 10 Keyword cluster map. A color represents a cluster, and 12 clusters were formed to show the knowledge structure of dysmenorrhea. |
Discussion
Dysmenorrhea is a common disease, affecting daily activities of childbearing-age women as well as reducing quality of life. Besides, most patients with dysmenorrhea may suffer from symptoms such as nausea and vomiting. Moreover, severe pain may trigger psychological problems, such as anxiety or depression.13
An upward trend in articles continued in this field overall in the past 21 years, which indicates that dysmenorrhea continues to receive the attention of researchers. Based on the upward trend, we hypothesized that dysmenorrhea will remain an important topic with great potential in the future. This trend may be related to the high prevalence of dysmenorrhea and the increased awareness of modern women’s health care. Studies on dysmenorrhea have been carried out in many countries, China, USA and Turkey contributed most, and China was the most productive country and performed well in cooperative networks. A survey in Changsha, China, reported that the incidence of PDM was as high as 41.7% among Chinese female college students.14 Another survey studied 706 Hispanic female adolescents at a local urban high school in USA, and 85% reported dysmenorrhea.15 In Turkey, a cross-sectional survey of 658 students was conducted at a health sciences university, and the reported prevalence was 79.7%.16 The prevalence of the three countries is high, which may also account for their great number of scientific research. The USA had very close links with almost all other regions, which showed high academic influence. Countries with high GDP per capita will receive more international collaborations, which suggests that economic power is an important factor influencing scientific activities and rich countries will invest more in scientific research and produce more scientifically influential results. However, international scientific research cooperation is still limited due to time and space limits. Therefore, it is necessary to strengthen international exchanges and cooperation. In the future, researchers can increase focus on collaboration with the help of network platforms to achieve breakthrough progress. As for institutions, most are universities with abundant scientific research resources, mostly in China and the United States. Colleges from the same country conducted close cooperation, while transnational cooperation among institutions is lacking, which calls for international cooperation in scientific research.
Hsieh JC and Hellman KM were both the most prolific author with 14 articles. The group of Hsieh JC mainly focused on the neuroimaging studies of dysmenorrhea, especially on structural alterations in the brain, BDNF Val66Met Polymorphism, and functional connectivity of pain modulatory systems;1,17–29 the group of Hellman KM mainly focused on the research of bladder pain sensitivity and spontaneous pain in dysmenorrhea women.30–43 Dawood MY is the most dominant author and the most frequently cited author, which is a medical doctor of the Department of Obstetrics and Gynecology, West Virginia University School of Medicine, writing a great number of reviews on dysmenorrhea, mainly about the nonsteroidal anti-inflammatory drugs like Ibuprofen.5,44–57 The team notes that once primary dysmenorrhea is diagnosed, the most effective treatments are NSAID and oral contraceptives.5 Our study found that nine of the ten most productive journals belonged to JCR Q1 and one belonged to JCR Q2. In addition, the journal co-citation network identified several major clusters of journals, including obstetrics and gynecology, pain and neuroscience, reproductive biology, and endocrinology, which indicated that there was close interdisciplinary communication in the study of dysmenorrhea.
More importantly, bibliometric analysis can help us gain insight into disciplinary development. Our study revealed the current research topics focus on three primary areas: (1) pathophysiology, such as “nitric oxide”, “functional connectivity”, “annexin a2” and “intrauterine pressure” and (2) public health impacts, such as “prevalence”, “quality of life”, and “severity” and (3) treatment, such as “herbal medicine”, “complementary therapies”, “Xuanzhong GB39”, and “pain management”.
The study on the pathological mechanism of dysmenorrhea has been paid much attention, especially in “nitric oxide” and “functional connectivity”, according to Figures 9 and 10. It is well-recognized that an increase in endometrial prostaglandin during menstruation can cause pelvic pain. Nitric oxide (NO) has relaxant effects on myometrial cells, contrary to prostaglandins, so NO donor drugs were used to relieve uterine contractions caused by endometrial prostaglandin, thus relieving menstrual cramps.58 The potential central mechanism of PDM has been noticed recently. It has been found that the state of chronic recurrent pain affects the central nervous system (CNS), leading to pathological changes in the brain, worsening menstrual pain in turn. Functional connectivity (FC) in human brain is within the realm of modern cognitive neuroscience. FC analysis can explore changes in brain functional activity associated with PDM, by analyzing the strength of the FC relationship between a particular brain region and other brain regions, from a functional integration perspective.6 The cluster map showed a special protein (annexin a2, ANXA2), relevant to the diagnosis of dysmenorrhea caused by adenomyosis. ANXA2 is a kind of calcium-binding cytoskeleton protein, existing in a variety of cell types, with diverse cellular functions, including angiogenesis, proliferation, apoptosis and cell growth regulation. It can be used as a diagnostic sign and provide a new diagnostic method for PDM caused by adenomyosis. In addition, ANXA2, a biological target for gene therapy applications, can offer a new way to relieve menstrual cramps in patients with adenomyosis-associated dysmenorrhea.59 “Intrauterine pressure” can be used to assess myometrium activity, which increases in women with dysmenorrhea. A double-blind RCT was conducted to show that a kind of oral drug, blocking the effect of vasopressin and relieving intrauterine pressure in consequence, can reduce menstrual pain when given before the onset of symptoms.60
Keyword analysis shows that “prevalence” was also one of the hotspots in the research of dysmenorrhea. There were lots of epidemiological surveys focusing on prevalence, however, owing to differences in countries and cultures, the prevalence reported was inconsistent. We found two systematic reviews published in 2013 and 2019, one of which highlighted that among the limited studies identified, the prevalence of dysmenorrhea ranged from 16% to 91%, and 2–28% of women reported severe pain or pain restricting daily life.3 Another review was based on meta-analysis, reporting that the prevalence of dysmenorrhea was high, with more than two-thirds (70.8%) of young women suffering from dysmenorrhea, regardless of the country’s economic status or geographic location.61 Dysmenorrhea negatively affects patients’ quality of life and sometimes results in activity restriction. Thus, “quality of life” is another hotspot. Women with PDM are weak in physical and social functioning and so on, reducing the quality of life (QoL) during menstruation. Also, women with PDM may have some emotional distress and may suffer from sleep disturbances and distress.7 Some evaluation indexes for dysmenorrhea are important, like the “severity” of the pain. The severity of dysmenorrhea varies from person to person, and the impact on different patients is also different, so focusing on the severity of dysmenorrhea in patients, like using the visual analogue scale may also be worth attention.
Given the negative effects of dysmenorrhea, it is essential to prevent and treat dysmenorrhea. To reduce the impact of dysmenorrhea, research in the future should focus on strategies that improve pain and symptom management.61 Keywords like “herbal medicine” “complementary therapies” “Xuanzhong GB39” “pain management” are all related to treatment. There are lots of medical approaches for treating primary dysmenorrhea, including oral contraceptives and NSAIDS, which have been reported to have some side effects and complications. Thus, the study of complementary therapies has been highlighted for effectiveness and low adverse reactions. Dysmenorrhea can be treated with alternative therapies such as essential oils, acupuncture, aromatherapy, and exercise, which can decrease the intensity and duration of pain and reduce the need for medication. In a recent study, researchers used inhalation of rose essential oil with NSAID for dysmenorrhea treatment, finding that the combination was more effective in reducing pain in PDM rather than NSAID alone, suggesting that inhalation of rose essential oil can be used as an alternative treatment to relieve pain. However, the importance of looking for new approaches should be highlighted to relieve pain. Besides, more study on possible effective treatments is demanded because of the existing limited research.13
However, the limitation of this study must be considered. The study was based on WOS database, not including all the related papers in this field, so the literature is incomplete. Nevertheless, due to the high quality of the papers included in WOS, we believe that the research results have a certain guiding significance.
Conclusion
Our study analyzed global dysmenorrhea research hotspots and trends over the past 21 years, which can guide scholars in exploring new research directions. An upward trend in articles continued in this field overall. Through the map, China contributed the most, followed by the USA and Turkey. For institutions, BUCM in China contributed the most, followed by NYMU in Taiwan, China. Hsieh JC and Hellman KM were both the most prolific authors with 14 articles. We found 5 major research groups, respectively with Hsieh JC, Hellman KM, Zhu J, Liang F and Dun W, as the core. Dawood MY was the most dominant author and most frequently cited author. Advances in pathogenesis and management for primary dysmenorrhea written by Dawood MY was most cited and most influential. The Cochrane Database of Systematic Reviews Journal was the most productive and the Fertility and Sterility Journal was the most cited. Advances in pathogenesis and management for primary dysmenorrhea written by Dawood MY was most cited and influential. Pathophysiology, the potential central mechanism, syndrome, evaluation index, diagnosis of adenomyosis-associated dysmenorrhea, treatment, etc., were the main trends and hotspots.
Acknowledgments
All the authors deserve credit for their contributions.
Funding
This work was not supported by any funding.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Wei SY, Chao HT, Tu CH, et al. Changes in functional connectivity of pain modulatory systems in women with primary dysmenorrhea. Pain. 2016;157:92–102. doi:10.1097/j.pain.0000000000000340
2. Unsal A, Ayranci U, Tozun M, et al. Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Upsala J Med Sci. 2010;115:138–145. doi:10.3109/03009730903457218
3. Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36:104–113. doi:10.1093/epirev/mxt009
4. Tsonis O, Gkrozou F, Barmpalia Z, et al. Integrating lifestyle focused approaches into the management of primary dysmenorrhea: impact on quality of life. Int J Womens Health. 2021;13:327–336. doi:10.2147/IJWH.S264023
5. Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108:428–441. doi:10.1097/01.AOG.0000230214.26638.0c
6. Yang H, Li X, Guo XL, et al. Moxibustion for primary dysmenorrhea: a resting-state functional magnetic resonance imaging study exploring the alteration of functional connectivity strength and functional connectivity. Front Neurosci Switz. 2022;16:969064. doi:10.3389/fnins.2022.969064
7. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21:762–778. doi:10.1093/humupd/dmv039
8. Iacovides S, Avidon I, Bentley A, et al. Diclofenac potassium restores objective and subjective measures of sleep quality in women with primary dysmenorrhea. Sleep. 2009;32:1019–1026. doi:10.1093/sleep/32.8.1019
9. Baker FC, Driver HS, Rogers GG, et al. High nocturnal body temperatures and disturbed sleep in women with primary dysmenorrhea. Am J Physiol. 1999;277:E1013–E1021. doi:10.1152/ajpendo.1999.277.6.E1013
10. Romanini E, Schettini I, Torre M, et al. The rise of registry-based research: a bibliometric analysis. Acta Orthop. 2021;92:628–632. doi:10.1080/17453674.2021.1937459
11. Larivière V, Desrochers N, Macaluso B, et al. Contributorship and division of labor in knowledge production. Soc Stud Sci. 2016;46:417–435. doi:10.1177/0306312716650046
12. Zhu G, Fu Z, Su S, et al. Global trends and hotspots in trigeminal neuralgia research from 2001 to 2021: a bibliometric analysis. Front Neurol. 2022;13:894006. doi:10.3389/fneur.2022.894006
13. Dias S, Pereira L, Oliveira AP, et al. Scientific and technological prospection on transdermal formulations and complementary therapies for the treatment of primary dysmenorrhea. Expert Opin Ther Pat. 2019;29:115–126. doi:10.1080/13543776.2019.1562547
14. Hu Z, Tang L, Chen L, et al. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a cross-sectional study. J Pediatr Adol Gynec. 2020;33:15–22. doi:10.1016/j.jpag.2019.09.004
15. Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000;154:1226–1229. doi:10.1001/archpedi.154.12.1226
16. Ozder A, Salduz Z. The prevalence of dysmenorrhea and its effects on female university students’ quality of life: what can we do in primary care? Int J Clin Exp Med. 2020;9:6496.
17. Chan HL, Low I, Chen LF, et al. A novel beamformer-based imaging of phase-amplitude coupling (BIPAC) unveiling the inter-regional connectivity of emotional prosody processing in women with primary dysmenorrhea. J Neural Eng. 2021;18:046074. doi:10.1088/1741-2552/abed83
18. Tu CH, Niddam DM, Chao HT, et al. Abnormal cerebral metabolism during menstrual pain in primary dysmenorrhea. Neuroimage. 2009;47:28–35. doi:10.1016/j.neuroimage.2009.03.080
19. Lee LC, Tu CH, Chen LF, et al. Association of brain-derived neurotrophic factor gene Val66Met polymorphism with primary dysmenorrhea. PLoS One. 2014;9:e112766. doi:10.1371/journal.pone.0112766
20. Tu CH, Niddam DM, Chao HT, et al. Brain morphological changes associated with cyclic menstrual pain. Pain. 2010;150:462–468. doi:10.1016/j.pain.2010.05.026
21. Wu TH, Tu CH, Chao HT, et al. Dynamic changes of functional pain connectome in women with primary dysmenorrhea. Sci Rep-Uk. 2016;6:24543. doi:10.1038/srep24543
22. Lee PS, Low I, Chen YS, et al. Encoding of menstrual pain experience with theta oscillations in women with primary dysmenorrhea. Sci Rep-Uk. 2017;7:15977. doi:10.1038/s41598-017-16039-4
23. Low I, Kuo PC, Tsai CL, et al. Interactions of BDNF Val66Met polymorphism and menstrual pain on brain complexity. Front Neurosci Switz. 2018;12:826. doi:10.3389/fnins.2018.00826
24. Tu CH, Niddam DM, Yeh TC, et al. Menstrual pain is associated with rapid structural alterations in the brain. Pain. 2013;154:1718–1724. doi:10.1016/j.pain.2013.05.022
25. Low I, Wei SY, Lee PS, et al. Neuroimaging studies of primary dysmenorrhea. Adv Exp Med Biol. 2018;1099:179–199. doi:10.1007/978-981-13-1756-9_16
26. Li WC, Chao HT, Lin MW, et al. Neuroprotective effect of Val variant of BDNF Val66Met polymorphism on hippocampus is modulated by the severity of menstrual pain. Neuroimage-Clin. 2021;30:102576. doi:10.1016/j.nicl.2021.102576
27. Wei SY, Chao HT, Tu CH, et al. The BDNF Val66Met polymorphism is associated with the functional connectivity dynamics of pain modulatory systems in primary dysmenorrhea. Sci Rep-Uk. 2016;6:23639. doi:10.1038/srep23639
28. Wei SY, Chen LF, Lin MW, et al. The OPRM1 A118G polymorphism modulates the descending pain modulatory system for individual pain experience in young women with primary dysmenorrhea. Sci Rep-Uk. 2017;7:39906. doi:10.1038/srep39906
29. Lee LC, Chen YH, Lin CS, et al. Unaltered intrinsic functional brain architecture in young women with primary dysmenorrhea. Sci Rep-Uk. 2018;8:12971. doi:10.1038/s41598-018-30827-6
30. Oladosu FA, Tu FF, Hellman KM. Nonsteroidal antiinflammatory drug resistance in dysmenorrhea: epidemiology, causes, and treatment. Am J Obstet Gynecol. 2018;218:390–400. doi:10.1016/j.ajog.2017.08.108
31. Hellman KM, Roth GE, Dillane KE, et al. Dysmenorrhea subtypes exhibit differential quantitative sensory assessment profiles. Pain. 2020;161:1227–1236. doi:10.1097/j.pain.0000000000001826
32. Hellman KM, Oladosu FA, Garrison EF, et al. Circulating sex steroids and bladder pain sensitivity in dysmenorrhea. Mol Pain. 2021;17:794236497. doi:10.1177/17448069211035217
33. Zuckerman RM, Silton RL, Tu FF, et al. Somatic symptoms in women with dysmenorrhea and noncyclic pelvic pain. Arch Women Ment Hlth. 2018;21:533–541. doi:10.1007/s00737-018-0823-4
34. Hellman KM, Datta A, Steiner ND, et al. Identification of experimental bladder sensitivity among dysmenorrhea sufferers. Am J Obstet Gynecol. 2018;219:81–84. doi:10.1016/j.ajog.2018.04.030
35. Tu FF, Datta A, Atashroo D, et al. Clinical profile of comorbid dysmenorrhea and bladder sensitivity: a cross-sectional analysis. Am J Obstet Gynecol. 2020;222:591–594. doi:10.1016/j.ajog.2019.12.010
36. Oladosu FA, Tu FF, Garfield LB, et al. Low serum oxytocin concentrations are associated with painful menstruation. Reprod Sci. 2020;27:668–674. doi:10.1007/s43032-019-00071-y
37. Oladosu FA, Hellman KM, Ham PJ, et al. Persistent autonomic dysfunction and bladder sensitivity in primary dysmenorrhea. Sci Rep-Uk. 2019;9:2194. doi:10.1038/s41598-019-38545-3
38. Westling AM, Tu FF, Griffith JW, et al. The association of dysmenorrhea with noncyclic pelvic pain accounting for psychological factors. Am J Obstet Gynecol. 2013;209:421–422. doi:10.1016/j.ajog.2013.08.020
39. Hellman KM, Kuhn CS, Tu FF, et al. Cine MRI during spontaneous cramps in women with menstrual pain. Am J Obstet Gynecol. 2018;218:501–506. doi:10.1016/j.ajog.2018.01.035
40. Kantarovich D, Dillane KE, Garrison EF, et al. Development and validation of a real-time method characterizing spontaneous pain in women with dysmenorrhea. J Obstet Gynaecol Re. 2021;47:1472–1480. doi:10.1111/jog.14663
41. Oladosu FA, Tu FF, Farhan S, et al. Abdominal skeletal muscle activity precedes spontaneous menstrual cramping pain in primary dysmenorrhea. Am J Obstet Gynecol. 2018;219:91. doi:10.1016/j.ajog.2018.04.050
42. Tu FF, Epstein AE, Pozolo KE, et al. A noninvasive bladder sensory test supports a role for dysmenorrhea increasing bladder noxious mechanosensitivity. Clin J Pain. 2013;29:883–890. doi:10.1097/AJP.0b013e31827a71a3
43. Oladosu FA, Tu FF, Garrison EF, et al. Low serum naproxen concentrations are associated with minimal pain relief: a preliminary study in women with dysmenorrhea. Pain Med. 2020;21:3102–3108. doi:10.1093/pm/pnaa133
44. Chan WY, Dawood MY, Fuchs F. Relief of dysmenorrhea with the prostaglandin synthetase inhibitor ibuprofen: effect on prostaglandin levels in menstrual fluid. Am J Obstet Gynecol. 1979;135:102–108. doi:10.1016/S0002-9378(79)80026-5
45. Chan WY, Dawood MY, Fuchs F. Prostaglandins in primary dysmenorrhea. Comparison of prophylactic and nonprophylactic treatment with ibuprofen and use of oral contraceptives. Am J Med. 1981;70:535–541. doi:10.1016/0002-9343(81)90576-3
46. Collins SB, Taylor DL, Thomas KK, et al. Cyclic perimenstrual pain and discomfort: the scientific basis for practice. Jognn J Obst Gyn Neo. 2002;31:637–649. doi:10.1177/088421702129005272
47. Dawood MY. Ibuprofen and dysmenorrhea. Am J Med. 1984;77:87–94. doi:10.1016/s0002-9343(84)80025-x
48. Dawood MY. Current concepts in the etiology and treatment of primary dysmenorrhea. Acta Obstet Gynecol Scand Suppl. 1986;138:7–10. doi:10.3109/00016348509157059
49. Dawood MY. Nonsteroidal anti-inflammatory drugs and changing attitudes toward dysmenorrhea. Am J Med. 1988;84:23–29. doi:10.1016/0002-9343(88)90473-1
50. Dawood MY. Dysmenorrhea. Clin Obstet Gynecol. 1990;33:168–178. doi:10.1097/00003081-199003000-00023
51. Dawood MY. Nonsteroidal antiinflammatory drugs and reproduction. Am J Obstet Gynecol. 1993;169:1255–1265. doi:10.1016/0002-9378(93)90292-q
52. Dawood MY, Khan-Dawood FS. Differential suppression of menstrual fluid prostaglandin F2a, prostaglandin E2, 6-keto prostaglandin F1a and thromboxane B2 by suprofen in women with primary dysmenorrhea. Prostag Oth Lipid M. 2007;83:146–153. doi:10.1016/j.prostaglandins.2006.10.009
53. Dawood MY, Khan-Dawood FS. Clinical efficacy and differential inhibition of menstrual fluid prostaglandin F2alpha in a randomized, double-blind, crossover treatment with placebo, Acetaminophen, and ibuprofen in primary dysmenorrhea. Am J Obstet Gynecol. 2007;196:31–35. doi:10.1016/j.ajog.2006.06.091
54. Dawood MY, Ramos J. Transcutaneous electrical nerve stimulation (TENS) for the treatment of primary dysmenorrhea: a randomized crossover comparison with placebo TENS and ibuprofen. Obstet Gynecol. 1990;75:656–660.
55. Fuchs F, Chan WY, Dawood MY. Suppression of menstrual prostaglandins and relief of dysmenorrhea with ibuprofen. Acta Obstet Gynecol Scand Suppl. 1979;87:91–92. doi:10.3109/00016347909157798
56. Milsom I, Minic M, Dawood MY, et al. Comparison of the efficacy and safety of nonprescription doses of naproxen and naproxen sodium with ibuprofen, Acetaminophen, and placebo in the treatment of primary dysmenorrhea: a pooled analysis of five studies. Clin Ther. 2002;24:1384–1400. doi:10.1016/s0149-2918(02)80043-1
57. Ylikorkala O, Dawood MY. New concepts in dysmenorrhea. Am J Obstet Gynecol. 1978;130:833–847. doi:10.1016/0002-9378(78)90019-4
58. Dmitrovic R, Kunselman AR, Legro RS. Sildenafil citrate in the treatment of pain in primary dysmenorrhea: a randomized controlled trial. Hum Reprod. 2013;28:2958–2965. doi:10.1093/humrep/det324
59. Liu F, Liu L, Zheng J. Expression of annexin A2 in adenomyosis and dysmenorrhea. Arch Gynecol Obstet. 2019;300:711–716. doi:10.1007/s00404-019-05205-w
60. Liedman R, Grant L, Igidbashian S, et al. Intrauterine pressure, ischemia markers, and experienced pain during administration of a vasopressin V1a receptor antagonist in spontaneous and vasopressin-induced dysmenorrhea. Acta Obstet Gyn Scan. 2006;85:207–211. doi:10.1080/00016340500495082
61. Armour M, Parry K, Manohar N, et al. The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. J Womens Health. 2019;28:1161–1171. doi:10.1089/jwh.2018.7615
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.