Back to Journals » Drug Design, Development and Therapy » Volume 17
Safety, Tolerability, and Pharmacokinetics of Benralizumab: A Phase 1, Randomized, Single-Blind Study of Healthy Chinese Participants
Authors Cheung TT, Mai TH, Chia YL, Yap DYH, Lee CH, Chen CC, Huang Y, Jin Y, Johnston J, Werkström V, Yao Y, Ge X, Zheng W
Received 4 October 2022
Accepted for publication 27 December 2022
Published 26 January 2023 Volume 2023:17 Pages 209—218
DOI https://doi.org/10.2147/DDDT.S392155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Tommy Tsang Cheung,1,* Tu H Mai,2,* Yen Lin Chia,2 Desmond YH Yap,1 Chi-Ho Lee,1 Cecil Chi-Keung Chen,2 Ying Huang,3 Yuwen Jin,3 James Johnston,4 Viktoria Werkström,5 Yuhui Yao,6 Xiaoyun Ge,7 Wenying Zheng8
1Department of Medicine, Queen Mary Hospital, The University of Hong Kong, Hong Kong, People’s Republic of China; 2Clinical Pharmacology and Quantitative Pharmacology, Clinical Pharmacology & Safety Sciences, BioPharmaceuticals R&D, AstraZeneca, South San Francisco, CA, USA; 3Clinical Pharmacology, R&D China, AstraZeneca, Shanghai, People’s Republic of China; 4Late-stage Development, Respiratory & Immunology, BioPharmaceuticals R&D, AstraZeneca, Cambridge, UK; 5Late-Stage Development, Respiratory & Immunology, BioPharmaceuticals R&D, AstraZeneca, Gothenburg, Sweden; 6Respiratory & Immunology, R&D China, AstraZeneca, Shanghai, People’s Republic of China; 7Clinical Safety, R&D China, AstraZeneca, Shanghai, People’s Republic of China; 8Biometrics, R&D China, AstraZeneca, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yen Lin Chia, Clinical Pharmacology and Quantitative Pharmacology, Clinical Pharmacology & Safety Sciences, BioPharmaceuticals R&D, AstraZeneca, 701 Gateway Blvd, South San Francisco, CA, 9408, USA, Tel +1 425 5272574, Email [email protected]
Purpose: Biological therapies targeting eosinophils have been shown to be effective in treating patients with severe eosinophilic asthma. Benralizumab (Fasenra®, AstraZeneca) is a humanized monoclonal antibody binding to the alpha subunit of the interleukin-5 receptor, which rapidly depletes eosinophils via antibody-dependent cellular cytotoxicity. The aim of this Phase 1 study was to assess the safety, tolerability, and pharmacokinetics of benralizumab in healthy Chinese individuals.
Materials and Methods: In this randomized, single-blind study (NCT03928262), healthy Chinese adult participants aged 18 to 45 years, weighing 50 to 100 kg, were randomized 1:1:1 to receive a single subcutaneous (SC) injection of benralizumab 10 mg, 30 mg, or 100 mg in the upper arms on Day 1. Safety was monitored throughout the study (up to Day 85), and blood samples were taken to determine serum benralizumab concentrations and for detection of anti-drug antibody. A non-compartmental analysis was conducted to estimate the pharmacokinetic parameters.
Results: Thirty-six healthy participants were enrolled, 12 in each dose group (mean [SD] age 26 [6] years). Following a single SC injection of benralizumab, 13 adverse events were reported by 10 participants (28%), with one mild injection-site reaction assessed as related. The mean serum benralizumab concentrations increased in a dose proportional manner, followed by exponential decreases. The mean terminal half-lives were 15.1 days for the 10 mg dose, 14.4 days for the 30 mg dose, and 15.4 days for the 100 mg dose. All doses resulted in near-complete depletion of eosinophils on Day 2, which was maintained throughout the study to Day 85.
Conclusion: A single SC injection of benralizumab was well tolerated by healthy Chinese participants, with no new or unexpected safety findings. The pharmacokinetics of benralizumab in Chinese participants was dose-proportional and consistent with those of non-Chinese participants observed in previous studies.
Clinical Trial Registration: NCT03928262 (https://clinicaltrials.gov/ct2/show/NCT03928262)
Keywords: benralizumab, pharmacokinetics, healthy Chinese
Introduction
Eosinophils are multifunctional leukocytes implicated in the inflammatory processes of a wide variety of diseases. Dysregulation of eosinophil activation and/or recruitment result in increased levels of eosinophils in the blood and tissues. In patients with eosinophilic asthma, elevated levels of eosinophils are found both in the blood and the airways. Over 80% of all severe asthma patients are of the eosinophilic phenotype,1 and biological therapies targeting eosinophils have been shown to be effective in this population.2–4
Benralizumab (Fasenra®, AstraZeneca) is a fully humanized afucosylated monoclonal antibody (mAb) that binds with high affinity and specificity to the alpha subunit of the human interleukin-5 receptor (IL-5Rα), which is predominantly expressed on human eosinophils and basophils. Benralizumab induces direct, rapid, and near-complete depletion of eosinophils and basophils via antibody-directed cellular cytotoxicity (ADCC).5,6
Benralizumab was first approved for the treatment of severe eosinophilic asthma (SEA) in the US in 2017 and is currently licenced in more than 70 countries, including the European Union, Japan, and South Korea. Results from multiple clinical trials and real-world studies have demonstrated that, as an add-on to maintenance therapy, benralizumab reduces the occurrence of asthma exacerbations and use of oral corticosteroids and improves lung function, asthma control,7–9 and health-related quality of life in patients with SEA.10 Finally, while the efficacy and safety of benralizumab were previously demonstrated in East Asian populations, including Japanese11 and Korean12 patients, they had not been evaluated in China. The aim of this Phase 1 study was to assess the safety and pharmacokinetics of a single dose of benralizumab in healthy Chinese participants. A Phase 3 efficacy and safety study in Chinese patients with severe asthma is ongoing.
Materials and Methods
Study Design, Participants, and Procedures
This was a Phase 1, randomized, single-blind study investigating the safety, tolerability, and pharmacokinetics after a single subcutaneous (SC) injection of benralizumab in healthy Chinese participants (NCT03928262). The study was conducted at the Queen Mary Hospital in Hong Kong between 2 April and 12 August 2019.
Healthy male and female Chinese participants, aged 18 to 45 years inclusive, were recruited. They also needed to be Han Chinese, born in China with Han Chinese parents and grandparents also born in China (including Hong Kong for all generations). Furthermore, their body weight had to be at least 50 kg and no more than 100 kg and their body mass index (BMI) between 19 and 24 kg/m2 inclusive. An upper-weight limit was set up to control pharmacokinetic variability, as the apparent clearance of benralizumab is dependent on body weight.13 Participants who had any condition requiring the regular use of any medication, a history immune system disorders, a helminth infection within 24 weeks, or with a condition resulting in an increased eosinophil count at screening were excluded from the study. Other exclusion criteria included receipt of any marketed or investigational biologic agents (monoclonal or polyclonal antibody) within 4 months or five half-lives, whichever was longer, prior to the date of informed consent (or planned usage during the study period); having taken part in any other study of an investigational medicinal product within 30 days or 5 half-lives (if known), whichever was longer, prior to the first study visit; receipt of a live attenuated vaccine 30 days prior to the date of informed consent; and pregnant, breastfeeding, or lactating at screening.
The full list of inclusion and exclusion criteria can be found in Supplementary Materials. All participants were required to provide a signed and dated informed consent prior to the start of the study, in compliance with the Declaration of Helsinki, Good Clinical Practice, and applicable regulatory requirements.
Participants were randomized into three study doses in a 1:1:1 ratio using consecutive randomization codes. They received a single SC injection of either 10 mg, 30 mg, or 100 mg of benralizumab on Day 1 of the study. Benralizumab was presented as a sterile liquid solution in an accessorized prefilled syringe (APFS) for SC injection. Each syringe contained either 10 mg of benralizumab in a 0.5 mL volume (nominal) or 30 mg/100 mg of benralizumab in a 1.0 mL volume (nominal), which was injected in the upper arm.
The study was single-blind in regard to dose level: the participants, the investigator, and the majority of the study staff did not know the dose. All personnel involved with the data analysis remained blinded until the database was unlocked.
Blood samples for pharmacokinetic analysis were collected on Day 1 (pre-dose) and then on Day 2, 4, 5, 6, 8, 15, 29, 43, 57, and 85. Blood samples used to assess the immunogenicity of benralizumab (ie the development of anti-drug antibodies [ADA] in response to treatment) were assessed on Day 1 (pre-dose) and on Days 29, 57, and 85.
Study Objectives and Endpoints
The primary objective was to investigate the safety and tolerability of SC administration of benralizumab in healthy Chinese participants. The primary endpoints were the number of treatment-emergent adverse events (AEs) and serious adverse events (SAEs) occurring within the duration of the study (85 days) for each dose. Laboratory variables (haematology, clinical chemistry, and urinalysis), measurements of vital signs, 12-lead electrocardiograms (ECG), and physical examinations were also assessed.
Secondary objectives included the assessment of single-dose pharmacokinetics of SC administration of benralizumab. Serum concentrations were determined using a validated electrochemiluminescent ligand-binding method with a lower limit of quantification (LLOQ) of 3.86 ng/mL. The pharmacokinetic endpoints assessed were serum concentration–time profiles of benralizumab following single SC injection, maximum observed concentration (Cmax), time to maximum observed concentration (tmax), area under the concentration–time curve from 0 to the last measurable time point (AUC0-t), area under the concentration–time curve from 0 to infinity (AUC0-∞), apparent clearance (CL/F), apparent volume of distribution at terminal phase (Vz/F) and the terminal half-life (t1/2). Another secondary objective was to assess the immunogenicity of benralizumab. ADA and, in ADA positive samples, neutralizing antibodies (nAb) were also determined by a validated electrochemiluminescent ligand-binding method.
Statistical Analyses
The safety analysis set, which comprised all participants who received any dose of benralizumab, was used to analyse the demographic and baseline characteristics, prior and concomitant medications, as well as safety and immunogenicity data. The pharmacokinetic analysis set was used to summarize the pharmacokinetic data and encompassed all the participants who received any dose of benralizumab and had at least one measurable post-dose serum pharmacokinetic observation from a pharmacokinetic blood sample, which is assumed not to be affected by factors such as important protocol deviations.
For all evaluations, participants were classified according to the dose they actually received. The analysis of the primary and secondary endpoints considered all data captured during the study. Statistical hypotheses were not evaluated based on formal statistical tests, instead descriptive statistics are presented for relevant data and parameters. Unless otherwise specified, no algorithm for missing data imputation has been employed.
Continuous variables were summarized by dose level, using the following descriptive statistics (used when applicable): the number of non-missing observations, arithmetic mean, standard deviation (SD), and quartiles. Coefficient of variation expressed in percentage (CV%), geometric mean, geometric SD, and geometric CV% were also presented in the pharmacokinetic summaries. Categorical data were summarized by dose level using frequency counts and percentages. Percentages were calculated using the number of participants within each dose level as the denominator, unless otherwise specified. When assessing minimum/maximum during the study, all assessments, including unscheduled/repeated assessments, were used. For analyses assessing changes from baseline, only participants with both baseline and at least one post-baseline measurement were included.
The pharmacokinetic parameters of benralizumab were estimated via non-compartmental analysis (NCA) methods using Phoenix WinNonlin (Princeton, New Jersey, US) version 7.0. All other data analyses were conducted using the SAS® System 9.4 (SAS Institute Inc., Cary, North Carolina, US).
The sample size of 36 participants was based on Chinese technical guidance and practical considerations (eg, dropouts) in order to have 8 to 12 evaluable participants at each dose level for the evaluation of PK and preliminary safety. Additionally, a minimum of 8 evaluable participants at each dose level that met specific NCA criteria were required for the AUC0-∞ calculation.
Post Hoc Comparison of Pharmacokinetics Between Chinese and Non-Chinese Participants
A post hoc comparison of the pharmacokinetic results from this study and those from a previous pharmacokinetic study of benralizumab, conducted with participants from Western countries, was performed. The AMES study (NCT02968914)14 was conducted in Germany and the UK and included a total of 180 healthy adult participants weighing 55–100 kg. Benralizumab was administered by APFS to 90 participants, 30 of which received a single 30 mg SC injection in the upper arm, and is the group with which the results of this current study is compared to. The sampling schedules for both studies were similar, however sampling ended at Day 57 for AMES.
Results
Participant Demographics
The demographic and baseline characteristics of the 36 healthy Chinese participants are given in Table 1. Ten (83.3%) of the 12 participants who received 10 mg of benralizumab completed the study, as did 11 (91.7%) of the 12 in the 30 mg and 100 mg benralizumab groups, respectively (Figure 1). Three participants decided to withdraw from the study, while one participant was lost to follow-up; none were linked to adverse events.
 |
Table 1 Demographics and Baseline Subject Characteristics (Safety Analysis Set) |
 |
Figure 1 Study flow design. |
All participants received the planned dose of benralizumab to which they were randomized. Four participants (11.1%) took 12 disallowed concomitant medications during the study (Supplementary Table 1). No single medication (by generic term) was taken by more than one participant, and none was thought to have influenced the clearance or pharmacokinetics of benralizumab, or to have had an impact on the study outcomes.
Safety and Tolerability
During the study, 13 adverse events were reported by 10 participants (27.8%): 3 (25%) in the 10 mg group, 5 (41.7%) in the 30 mg group, and 2 (16.7%) in the 100 mg group. The most common adverse event was influenza-like illness, which was reported by 6 participants (16.7% of all participants): 2 (16.7%) in the 10 mg group, 3 (25%) in the 30 mg group and 1 (8.3%) in the 100 mg group. All adverse events were mild except for one serious adverse event in the 100 mg group (a cervical vertebral fracture 52 days after the injection), which was assessed as not related to benralizumab by the investigator, and did not lead to withdrawal from the study. One drug-related adverse event (a mild injection site swelling which resolved within 3 days) was reported by a participant in 30 mg group and did not lead to withdrawal from the study (Table 2).
 |
Table 2 Summary of Adverse Events Reported During the On-Study Period (Safety Analysis Set) |
Clinical Laboratory Measurements, Vital Signs, and ECG Outcomes
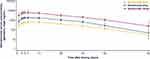
There were no clinically relevant changes or trends in most laboratory measurements. As expected, based on the mechanism of action of benralizumab, all doses resulted in near-complete depletion of eosinophils on Day 2 (mean counts <10 cells/μL for all doses), which was maintained throughout the study to Day 85 (mean counts <5 cells/μL for all doses) (Figure 2).
There were no clinically meaningful changes or trends in vital sign measurements (systolic/diastolic blood pressure, pulse rate, or temperature) nor in the assessed ECG variables (heart rate, QRS duration, PR, QT, QTcB, QTcF, and RR intervals) during the study.
Pharmacokinetic Results
In line with the pharmacokinetics observed in previous benralizumab studies, after a single SC injection, the mean serum benralizumab concentrations increased through to Day 7 or 14 in a dose proportional manner, followed by exponential decreases at a similar rate for all doses (Figure 3). At Day 85 serum benralizumab remained above LLOQ (3.86 ng/mL) for all but two participants, one each in the 10 mg and 30 mg groups.
The pharmacokinetic parameters of benralizumab are summarized in Table 3. Following a single SC administration of 10 mg, 30 mg, or 100 mg, the geometric mean Cmax, AUC0-t, and AUC0-∞ increased-proportionally to the dose given. The median time to maximum observed concentration (tmax) was 7.0 days for both the 30 mg and 100 mg doses and 9.5 days for the 10 mg dose. As for the terminal half-lives (t1/2), the geometric means were 15.1 days for the 10 mg, 14.4 days for the 30 mg, and 15.4 days for the 100 mg doses. Similar values were observed across the three doses for the apparent clearance (CL/F) and the apparent volume of distribution at terminal phase (Vz/F).
 |
Table 3 Pharmacokinetic Parameters of Benralizumab Following Single SC Dose Administration on Day 1 (PK Analysis Set) |
Anti-Drug Antibody (ADA) Response
Five of the 36 participants were positive for anti-drug antibodies (ADA) at post-baseline time points only and hence were classified as treatment-emergent. Thus, both the ADA prevalence and ADA incidence were 13.9%. All five participants tested positive for neutralising antibodies (Table 4). Four participants (across all groups) tested positive at only Day 85, but one in the 30 mg group also tested positive at Day 57. Serum benralizumab concentrations were numerically lower in ADA-positive participants after detection of ADA, compared with that of ADA-negative participants at the same time points (Figure 4). No temporally associated adverse events were observed with ADA-positive status, nor did any of the ADA-positive participants report hypersensitivity events. The interpretation of these results is limited due to the single-dose design and the small number of ADA-positive participants.
 |
Table 4 Anti-Drug Antibody Response (Safety Analysis Set) |
Post Hoc Comparison of Pharmacokinetics with a Non-Chinese Population in AMES
Post hoc analyses showed that the pharmacokinetics of a single SC administration of 30 mg benralizumab in the upper arm were consistent between healthy Chinese participants and a similar population of healthy participants from Germany and the UK recruited into the AMES study14 (Supplementary Table 2 and Supplementary Figure 1).
Discussion
This Phase 1 study indicates that a single SC injection of benralizumab at doses up to 100 mg was well tolerated by healthy Chinese participants, with no new or unexpected safety findings. The only adverse event that was assessed as related to benralizumab was a mild injection site reaction, which resolved within 3 days. Furthermore, consistent with the pharmacokinetic properties of benralizumab observed in previous studies,8,11,12 the mean serum benralizumab concentration increased in a dose-proportional manner following a single SC administration in healthy Chinese participants.
The mean terminal half-life of benralizumab seen in this study was approximately 15 days for the three dose levels, consistent with the estimated terminal half-life of 15.5 days in the population pharmacokinetic model global benralizumab studies.15 The serum concentrations and pharmacokinetic parameters for the benralizumab 30 mg group are also in line with the results of a previous single-dose SC injection study involving healthy Western volunteers with a similar bodyweight range (upper arm injection group).14 This indicates that there are no apparent ethnic differences in the pharmacokinetics of benralizumab between healthy Chinese and Western participants.
Consistent with the mechanism of action for benralizumab,6 all doses resulted in near-complete depletion of eosinophils through ADCC, which was evident by the first assessment (Day 2) and maintained throughout the study (to Day 85). This is also consistent with the expected pharmacodynamic effect of benralizumab.8,9
The overall incidence of ADA was 13.9% (5/36 participants) in this single-dose study, and there were no temporally associated adverse events observed with ADA positive status. However, the limited number of participants enrolled in this study and the low incidence of ADA-positive participants do not allow a definitive conclusion on ADA response to be made.
The results from this study support continued investigation of benralizumab, which is currently being evaluated in a Phase 3 study assessing the efficacy and safety of benralizumab in Asian patients (mainly from China) with uncontrolled severe asthma on medium-to-high dose inhaled corticosteroid plus long-acting β2-agonist (MIRACLE, NCT03186209).
Data Sharing Statement
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB), reference number: UW 18-623.
All participants were required to provide a signed and dated informed consent prior to the start of the study, in compliance with the Declaration of Helsinki, Good Clinical Practice, and applicable regulatory requirements.
Acknowledgments
This manuscript was supported by AstraZeneca. The authors would like to thank the health-care providers, research staff, and participants who took part in this study. We also thank Nicola Truss and Lise Magnollay of InScience Communications, Springer Healthcare Ltd, UK, for providing medical writing support, which was funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by AstraZeneca.
Disclosure
TTC: has received grants and non-financial support from AstraZeneca. TM, YLC, and YH were employees of AstraZeneca at the time when the study was conducted. TM is currently an employee of Genentech, and YLC is currently an employee of Seagen. YH is currently an employee of Zai Lab. CCC, XG, YJ, JJ, VW, YY, and WZ are employees of AstraZeneca, and may own stock/stock options. The authors report no other conflicts of interest in this work.
References
1. Heaney LG, Perez de Llano L, Al-Ahmad M, et al. Eosinophilic and noneosinophilic asthma: an expert consensus framework to characterize phenotypes in a global real-life severe asthma cohort. Chest. 2021;160(3):814–830. doi:10.1016/j.chest.2021.04.013
2. Dragonieri S, Carpagnano GE. Biological therapy for severe asthma. Asthma Res Pract. 2021;7(1):12. doi:10.1186/s40733-021-00078-w
3. McCracken JL, Tripple JW, Calhoun WJ. Biologic therapy in the management of asthma. Curr Opin Allergy Clin Immunol. 2016;16(4):375–382. doi:10.1097/ACI.0000000000000284
4. Patel SS, Casale TB, Cardet JC. Biological therapies for eosinophilic asthma. Expert Opin Biol Ther. 2018;18(7):747–754. doi:10.1080/14712598.2018.1492540
5. Kolbeck R, Kozhich A, Koike M, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125(6):1344–1353 e1342. doi:10.1016/j.jaci.2010.04.004
6. Ghazi A, Trikha A, Calhoun WJ. Benralizumab--A humanized mAb to IL-5Ralpha with enhanced antibody-dependent cell-mediated cytotoxicity--A novel approach for the treatment of asthma. Expert Opin Biol Ther. 2012;12(1):113–118. doi:10.1517/14712598.2012.642359
7. Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376(25):2448–2458. doi:10.1056/NEJMoa1703501
8. Bleecker ER, FitzGerald JM, Chanez P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting beta2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2115–2127. doi:10.1016/S0140-6736(16)31324-1
9. FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–2141. doi:10.1016/S0140-6736(16)31322-8
10. Kavanagh JE, Hearn AP, Dhariwal J, et al. Real-world effectiveness of benralizumab in severe eosinophilic asthma. Chest. 2021;159(2):496–506. doi:10.1016/j.chest.2020.08.2083
11. Ohta K, Adachi M, Tohda Y, et al. Efficacy and safety of benralizumab in Japanese patients with severe, uncontrolled eosinophilic asthma. Allergol Int. 2018;67(2):266–272. doi:10.1016/j.alit.2017.10.004
12. Park HS, Lee SH, Lee SY, et al. Efficacy and safety of benralizumab for Korean patients with severe, uncontrolled eosinophilic asthma. Allergy Asthma Immunol Res. 2019;11(4):508–518. doi:10.4168/aair.2019.11.4.508
13. Yan L, Wang B, Chia YL, Roskos LK. Population pharmacokinetic modeling of benralizumab in adult and adolescent patients with asthma. Clin Pharmacokinet. 2019;58(7):943–958. doi:10.1007/s40262-019-00738-4
14. Martin UJ, Fuhr R, Forte P, et al. Comparison of autoinjector with accessorized prefilled syringe for benralizumab pharmacokinetic exposure: AMES trial results. J Asthma. 2021;58(1):93–101. doi:10.1080/02770903.2019.1663428
15. AstraZeneca. Fasenra (benralizumab) summary of product characteristics; 2022. Available from: https://www.medicines.org.uk/emc/product/8918/smpc#gref.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.