Back to Journals » Cancer Management and Research » Volume 14
Role of Olaparib in the Management of Metastatic Castration-Resistant Prostate Cancer: A Japanese Clinician’s Perspective
Authors Matsumoto T, Shiota M , Blas L, Eto M
Received 19 June 2022
Accepted for publication 1 August 2022
Published 8 August 2022 Volume 2022:14 Pages 2389—2397
DOI https://doi.org/10.2147/CMAR.S326114
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Takashi Matsumoto, Masaki Shiota, Leandro Blas, Masatoshi Eto
Department of Urology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
Correspondence: Masaki Shiota, Department of Urology, Graduate School of Medical Sciences, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka, 812-8582, Japan, Tel +81 92 642 5603, Fax +81 92 642 5618, Email [email protected]
Abstract: Several studies have identified various targetable genomic alterations in prostate cancer, which accumulate during carcinogenesis and cancer progression. Genomic alterations in genes involved in DNA damage repair by homologous recombination repair may predict increased sensitivity to poly-ADP ribose polymerase (PARP) inhibitors. The Phase 3 PROfound trial has shown that treatment with the PARP inhibitor olaparib was associated with an improved radiographic progression-free survival and overall survival among patients with homologous recombination repair-deficient metastatic castration-resistant prostate cancer (mCRPC) after the treatment with androgen receptor targeting therapy, especially in men with BRCA1 or BRCA2 mutation. In Japan, olaparib was approved in December 2020 for the treatment of mCRPC with BRCA1 or BRCA2 mutation. In addition, genetic tests to detect BRCA1 or BRCA2 mutation to select patients who are likely to benefit from olaparib were also approved. This review summarizes the status of olaparib treatment for mCRPC, focusing on the situation in Japan.
Keywords: olaparib, metastatic castration-resistant prostate cancer, Japanese, BRCA, companion diagnosis, genomic profile
Introduction
Prostate cancer (PCa) is an androgen-sensitive disease that requires testosterone for its development and proliferation.1 Standard treatment for metastatic PCa is androgen deprivation therapy, which suppresses androgen receptor (AR) signaling.2 These interventions result in low testosterone levels and initially are highly effective in the relief of cancer-related symptoms, tumor marker decline, and tumor shrinking. However, the disease inevitably progresses to castration-resistant PCa (CRPC).3
Recent studies for molecular profiling, including the Stand Up to Cancer-PCF (SU2C-PCF) for metastatic CRPC (mCRPC) project and The Cancer Genome Atlas (TCGA) for primary localized PCa study, have identified various genomic alterations in PCa, which accumulate during carcinogenesis and cancer progression.4–6 Interestingly, some of them were potentially targetable alterations that occur somatically as well as in the germline.4–6 In particular, genomic alterations in genes involved in DNA damage repair by homologous recombination repair (HRR) may predict increased sensitivity to platinum-based therapy and poly-ADP ribose polymerase (PARP) inhibitors.7,8 The PROfound trial has shown that treatment with the PARP inhibitor olaparib was associated with an improved radiographic progression-free survival (rPFS) among patients with HRR-deficient mCRPC before treatment with AR axis-targeting therapy (ARAT), especially in men with BRCA1 or BRCA2 mutation.9,10 Accordingly, the Food and Drug Administration (FDA) approved olaparib, in the United States (US) in May 2020, for the treatment of mCRPC with HRR gene mutations (HRRm). In Japan, olaparib was approved by the Pharmaceutical and Medical Devices Agency (PMDA) in December 2020 for the treatment of mCRPC with BRCA1 or BRCA2 mutation, and companion diagnostic tools for the indication of olaparib in PCa have also been approved accordingly. This review summarizes the status of olaparib treatment for mCRPC, focusing on the situation in Japan.
PCa Incidence and Mortality in Japan
PCa is the most frequently diagnosed cancer in 112 countries and the leading cause of cancer death in 48 of them.11 The number of PCa cases diagnosed in the US in 2020 was 209,512, with an age-standardized incidence rate of 72 per 100,000, and the number of PCa deaths was 32,438, with an age-standardized mortality rate of 8.2 per 100,000. On the other hand, in Japan, the number of PCa cases was 106,139 with an age-standardized incidence rate of 51.8 per 100,000, and the number of deaths was 13,426 with an age-standardized mortality rate of 4.5 per 100,000.12 Thus, morbidity and mortality rates in Japan are lower than those in the US, as race in addition to age and family history of PCa are well-known risk factors for PCa. In addition, total energy intake, obesity, and intake of dairy products have also been suggested as risk factors, which may affect different morbidity and mortality rates between the US and Japan.13–15
HRR Genes and PCa Risk
As the disease progresses from hormone-sensitive PCa to mCRPC, various genomic alterations accumulate, including pathways related to AR signaling, PI3K/AKT, cell cycle, and DNA repair.5,16–19 Single-strand breaks are repaired by several mechanisms involving PARP, while two systems including HRR or non-homologous end joining (NHEJ) repair a DNA double-strand break (DSB).20,21
Tumor suppressor genes BRCA1, BRCA2, and ATM are involved in HRR, which can repair DSB accurately with few errors. However, when there is a HRR deficiency due to HRRm, the DSB is repaired by the NHEJ, which is prone to make compensatory repair errors.21 Therefore, genetic mutations in BRCA1 and BRCA2 lead to accumulating genomic abnormalities, making them susceptible to a variety of cancers, including breast, ovarian, prostate, and pancreatic cancer.22–24
So far, retrospective studies have shown the association between BRCA mutation and PCa incidence rate.25 In addition, the prospective EMBRACE study from the United Kingdom and Ireland has recently reported that germline BRCA1 and BRCA2 mutations were associated with an accumulative risk of developing PCa. The risk comorbid with PCa by age 85 years was 29% and 60% in germline BRCA1 and BRCA2 mutations, respectively.26 Another study found that in Japanese with pathogenic variants (PVs) of the BRCA2 gene, the accumulative risk of developing PCa was 24.5% by age 85 years, suggesting relative lower risk of PCa incidence related to BRCA mutation in Japanese, compared with Caucasian.27
Olaparib Treatment Outcomes in Japanese
PARP inhibitors block PARP-mediated repair of single-strand breaks, leading to the generation of more deleterious DNA.5,28–32 During DNA replication, cancer cells attempt precise repair of DSBs by HRR. However, in the presence of HRR deficiency, NHEJ repairs DSBs caused by PARP inhibition, resulting in intolerable genomic alterations, ultimately leading to cancer cell death.33
The PROfound trial, a randomized, open-label, phase 3 study, evaluated the efficacy and safety of olaparib (n=256) compared to enzalutamide or abiraterone acetate (n=131) as alternative ARAT, in patients with HRRm-deficient mCRPC who had failed ARAT.10 The median rPFS as the primary endpoint was 7.4 months (95% CI, 6.2–9.3 months) and 3.6 months (95% CI, 1.9–3.7 months) in the olaparib and alternative ARAT arms among men harboring BRCA1/2 or ATM mutation (cohort A, HR 0.34; 95% CI, 0.25–0.47; p<0.001), respectively. Moreover, a significantly longer rPFS was also observed in all HRRm (cohort A+B, HR 0.49; 95% CI, 0.38–0.63; p<0.001). The incidence of grade ≥3 adverse events was higher with olaparib than with alternative ARAT. The most common adverse events of any grade with olaparib were anemia, nausea, and fatigue or asthenia, while those with alternative ARAT were fatigue or asthenia.
Based on these results, the FDA approved olaparib for patients with 11 HRRm in addition to BRCA1/2 and ATM in May 2020, where the FDA excluded PPP2R2A gene, a regulator of phosphorylation of ATM, among 15 HRR genes due to unfavorable risk-benefit.34,35 Meanwhile, the HR of rPFS in the olaparib arm was 0.41 (95% CI, 0.13–1.39) in BRCA1-mutated subgroup and 0.21 (95% CI; 0.13–0.32) in BRCA2–mutated subgroup. However, no benefit was observed in ATM–mutated subgroup (HR, 1.04; 95% CI, 0.61–1.87).10 Based on these results, in December 2020, olaparib was approved only for mCRPC with BRCA1 or BRCA2 mutation in Japan by the PMDA,36 and also by the European Medicines Agency.37
Additional reports of the PROfound trial showed a median overall survival (OS) of 19.1 months with olaparib and 14.7 months with alternative ARAT (HR, 0.69; 95% CI, 0.50–0.97; p=0.02) in cohort A. When adjusting for crossover to olaparib, the HR for OS was 0.42 (95% CI, 0.19–0.91) in cohort A, 0.83 (95% CI, 0.11–5.98) in cohort B, and 0.55 (95% CI, 0.29–1.06) in the overall cohort.9 Thus, the patients initially assigned to olaparib with BRCA1-, BRCA2-, or ATM–mutated mCRPC after disease progression during prior treatment with AR significantly had longer OS than those assigned to enzalutamide or abiraterone acetate plus prednisone, despite significant crossover from control therapy to olaparib. In addition, the objective response rate (ORR) was higher in the olaparib group (43.9% vs 0%), with a PSA response rate of 56.9%.10 Olaparib therapy was also associated with reduced pain burden and maintenance of the health-related quality of life.38
An subgroup analysis of 101 Asians (including 57 Japanese) in the PROfound study showed the greatest improvement of rPFS (9.3 vs 3.5 months; HR, 0.17; 95% CI 0.06–0.49; p=0.0003) with olaparib in patients with BRCA1 or BRCA2 mutation, and similar trend of OS improvement (26.8 vs 14.3 months; HR, 0.62; 95% CI, 0.24–1.79; p=0.34) was shown.39 In patients with BRCA1, BRCA2, or ATM mutation, rPFS was longer in the olaparib arm than in the alternative ARAT arm (7.2 vs 4.5 months, HR, 0.58; 95% CI, 0.29–1.21, p=0.14) although statistical significance was not obtained due to less statistical power. Thus, in Asians with mCRPC accompanied with BRCA1 or BRCA2 mutation and disease progression during prior ARAT, rPFS was significantly longer with olaparib than with enzalutamide or abiraterone acetate and prednisone.
In addition, Phase 2 TRITON2 study (NCT02952534), an ongoing multicenter, single-arm clinical trial, evaluated the efficacy and safety of the PARP inhibitor rucaparib in men with mCRPC harboring a BRCA1 or BRCA2 gene alteration.30,40 The confirmed ORR by independent radiology review was 44% (95% CI, 31–57%), and safety profile was favorable. Based on the results, the FDA announced in 2020 the expedited approval of the PARP inhibitor rucaparib for advanced PCa with germline or somatic BRCA mutation and a history of ARAT and taxane-based therapy. However, rucaparib has not been approved in Japan.
Frequency of HRR Gene Mutations
As genetic variations differ among ethnics, the frequency of germline and somatic mutations in HRR gene can vary. Actually, it has recently been reported that Black men with prostate cancer exhibited a lower frequency and narrower spectrum of germline PVs and a higher frequency of variants of uncertain significance (VUS) in DNA repair genes compared with White men.41
The frequency of BRCA1 and BRCA2 mutations in advanced PCa globally was 0.9% and 8.6% in germline mutation, and 0.9% and 7.7% in somatic mutation, respectively (Table 1).42 Meanwhile, in the study from Japan on the frequency of germline BRCA1 and BRCA2 PVs in 7636 PCa cases and 12,366 non-carcinoma patients, 64 (1.3%) had germline BRCA1 or BRCA2 PVs, accounting for 0.2% and 1.1% of the prevalence rate among patients with PCa, respectively.24 In another study from Japan germline BRCA1 or BRCA2 mutation rates were 0% and 3.4% in advanced PCa (n=562), respectively.43 Thus, the frequency of germline mutation of BRCA1 and BRCA2 seems higher in Caucasians than Asians, which may be attributable to the frequency of VUS, at least in part. Since few genetic studies have been conducted in Asians, abnormalities in BRCA1 and BRCA2 genes among this population are associated with a high frequency of VUS.44 Functional assays to determine the pathological value of VUS are needed to provide clinical guidance regarding cancer risk and treatment options.45 As well, further studies on the clinical significance of genetic abnormalities unique to Asians, including Japanese are needed.
 |
Table 1 Comparison of Germline and Somatic Mutations of BRCA1/2 Between Overseas and Japan |
In addition, several results were reported on somatic mutations of BRCA1 or BRCA2. In the ZENSHIN study, the mutation rates of BRCA1 or BRCA2 including germline and somatic mutation in Japanese patients with mCRPC were 0.7% or 12.6%, respectively, and the rate of the 15 HRRm genes was 35.7% in total.46 Consistently, the frequency of HRRm in the PROfound study in global population and Japanese showed that the frequency of BRCA1 or BRCA2 mutation was comparable between global population (1.3% or 9.7%) and Japanese subset (2% or 8.3%), respectively (Table 2).39,47 Furthermore, comparable frequency of BRCA1 somatic mutation was observed among Asian, White, and Black men, despite differences of genomic alteration signatures, including HRR genes in PCa among ethnics.48 Thus, accumulating evidence suggested no large difference in the frequency of somatic mutation in BRCA1 and BRCA2 genes between global population and Japanese with mCRPC.
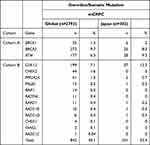 |
Table 2 Comparison of Homologous Recombination Repair Mutation Between Global and Japan in PROfound Trial |
BRCA Mutations in Tissue and Liquid Biopsy
A biopsy from soft tissues may be difficult in most cases with mCRPC, where a blood-based liquid biopsy using circulating tumor DNA (ctDNA) may detect the mutations. When comparing ctDNA alterations with tumor DNA from matched tissue, all somatic mutations identified in the tumor were simultaneously present in the ctDNA.49 Furthermore, variant allele frequencies and copy number profiles of common mutations showed a high correlation between ctDNA and tissue.49 Therefore, those data support that ctDNA-based genomic profiling is useful as DNA biomarkers in mCRPC.
The rates of BRCA1 and BRCA2 mutations in circulating tumor DNA (ctDNA) among 3334 men with mCRPC in the US were 1.4% and 7.5%, respectively.50 Although the concordance rate of gene alterations between tumor tissue and ctDNA was 93%, ctDNA contained several BRCA1 and BRCA2 alterations that were not identified in tumor tissues.50 This inconsistent detection between tumor tissue and ctDNA may be due to spatiotemporal heterogeneity or clonal hematopoiesis of indeterminate potential (CHIP).51 Meanwhile, a study among 100 Japanese with CRPC treated with abiraterone acetate or enzalutamide found 1% and 6% of somatic BRCA1 and BRCA2 mutations in ctDNA, respectively.52 Similarly, a preliminary analysis from the SCRUM-JAPAN MONSTER SCREEN project demonstrated 6% of BRCA2 mutation in ctDNA among 95 patients with unresectable PCa at pretreatment.53 Therefore, the rates of BRCA1 and BRCA2 mutations in ctDNA were comparable between the residents in the US and Japan, but less frequent compared with those in tissues.
However, there is a concern that liquid biopsy may detect CHIP of leukocytes with genetic abnormalities.54 Analysis of ctDNA from 69 advanced PCa cases detected four BRCA1 and BRCA2 mutations, and one of them was derived from CHIP.55 Therefore, current ctDNA testing has a high risk of misdiagnosis as an indication for PARP inhibitor therapy, and a test using genomic DNA from white blood cells that distinguish between CHIP mutants and PCa is ideal.
Companion Diagnostics and Comprehensive Genome Profiling
Companion diagnostics is a clinical test to predict the efficacy and side effects of treatment. Conventional genetic or genomic testing can detect alterations in a single gene, while comprehensive genome profiling test can reveal the alterations in hundreds of genes using next-generation sequencer. In Japan, on 31 May 2022, BRACAnalysisⓇ, FoundationOneⓇ CDx Cancer Genome Profile (F1CDx), and FoundationOneⓇ Liquid CDx Cancer Genome Profile (F1L) are available for reimbursement as companion diagnostics (Table 3). In addition, F1CDx, F1L, and OncoGuideTM NCC OncoPanel System (NCC OncoPanel) are also available as comprehensive genome profiling (CGP) test. BRACAnalysisⓇ is a test for germline mutations in BRCA1 and BRCA2 genes using leukocyte-derived DNA. F1CDx and F1L are CGP tests using tumor tissue and ctDNA in the blood, respectively, and provide gene alteration profiles in 324 genes without distinguishing between germline and somatic mutations. The NCC OncoPanel, which uses DNA derived from cancer tissue and leukocytes to distinguish germline from somatic mutations and detect alterations in 124 genes has been approved as CGP by insurance in Japan. As well, Guardant360Ⓡ, which tests for germline and somatic mutations using ctDNA in blood, has been approved as CGP by PMDA in Japan.
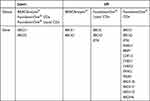 |
Table 3 Companion Diagnosis Devices in the US and Japan |
In the US, companion diagnostics for olaparib include BRACAnalysisⓇ, F1CDx, and F1L.56 Similarly, F1CDx, F1L, and Guardant360Ⓡare approved by the FDA as CGP. In addition, the FDA approved F1CDx as companion diagnostic for rucaparib based on TRITON2 trial results.30 Thus, although there are a few differences in the availability of diagnostic tests for BRCA1 and BRCA2 mutations, similar tests are available in the US and Japan.
Issues related to olaparib treatment in Japan and beyond
Olaparib is expected to show high efficacy in Japanese patients, as shown by the results from the Asian subgroup in the PROfound trial. However, in Japan, olaparib is approved only for BRCA1 and BRCA2 mutations, in contrast to the FDA’s approval for 14 HRRm. Although the frequency of somatic BRCA1 and BRCA2 mutations is comparable between Japan and worldwide, the frequency of germline BRCA1 and BRCA2 PVs in Japanese is suggested to be lower than other races. Therefore, the number of patients who can be treated with olaparib for mCRPC could be relatively limited in Japan compared to the US.
The phase 3 PROpel trial (NCT03732820) compared the effect of olaparib plus abiraterone acetate versus placebo plus abiraterone acetate in patients with untreated mCRPC.57 An interim analysis showed that olaparib treatment improved the rPFS compared to abiraterone acetate alone in the HRRm group (HR 0.54, 95% CI 0.36–0.79) and the non-HRRm group (HR 0.76, 95% CI 0.59–0.97). On the other hand, the MAGNITUDE phase 3 trial (NCT03748641) compared the PARP inhibitor niraparib plus abiraterone acetate (combination therapy) versus placebo plus abiraterone acetate in mCRPC, in which study up to 4 months of prior abiraterone plus prednisone for mCRPC was allowed. The HRRm group showed an improvement in rPFS with the combination therapy, whereas no benefit was observed in the HRR-nonmutant group.32 Thus, the results of PARP inhibitors combined with ARAT for non-HRR deficiency are conflicting, which might be due to the difference of eligibility whether prior abiraterone plus prednisone was allowed or not. It is necessary to discuss the optimal use of PARP inhibitor, depending on the results from further investigations.
In addition, phase 3 TALAPRO-3 (NCT04821622) is currently testing the effect of enzalutamide plus the PARP inhibitor talazoparib versus enzalutamide plus placebo in patients with metastatic castration-sensitive PCa carrying DNA damage response gene mutation.58 Moreover, phase 3 AMPLITUDE (NCT04497844)59 is testing the effect of abiraterone acetate plus the PARP inhibitor niraparib, in metastatic castration-sensitive PCa with HRRm.
As well, platinum-based anticancer drugs, radioisotope radium-223, and bipolar androgen therapy have also been suggested to be effective for PCa with HRR deficiency, including BRCA1 and BRCA2 mutations.60–63 Then, HRR deficiency may be a predictive biomarker of efficacy with those treatments.
Conclusion
Olaparib treatment is currently available for treatment of mCRPC in Japan although there are several differences such as frequency of BRCA gene mutation and the genes for olaparib indication between the US and Japan. Despite some challenges, there is no doubt that olaparib has opened the door to precision medicine for PCa. Several PARP inhibitors are also under investigation, and further clinical applications in PCa are expected based on the results of future clinical trials.
Disclosure
Masaki Shiota received honoraria from Janssen Pharmaceutical, AstraZeneca, Astellas Pharma, Sanofi, and Bayer Yakuhin and research funding support from Daiichi Sankyo. Masatoshi Eto received honoraria from Ono Pharmaceutical, Takeda Pharmaceutical, Novartis Pharma, Pfizer, Bristol-Myers Squibb, Janssen Pharmaceutical, MSD, Merck Biopharma, AstraZeneca, and Eisai and research funding support from Sanofi, Bayer Yakuhin, Astellas Pharma, Ono Pharmaceutical, and Takeda Pharmaceutical. The authors report no other conflicts of interest in this work.
References
1. Huggins C. Prostatic cancer treated by orchiectomy: the five year results. J Am Med Assoc. 1946;131(7):576–581. doi:10.1001/jama.1946.02870240008003
2. Ryan CJ, Tindall DJ. Androgen receptor rediscovered: the new biology and targeting the androgen receptor therapeutically. J Clin Oncol. 2011;29(27):3651–3658. doi:10.1200/JCO.2011.35.2005
3. Galletti G, Leach BI, Lam L, Tagawa ST. Mechanisms of resistance to systemic therapy in metastatic castration-resistant prostate cancer. Cancer Treat Rev. 2017;57:16–27. doi:10.1016/j.ctrv.2017.04.008
4. Abeshouse A, Ahn J, Akbani R, et al. The molecular taxonomy of primary prostate cancer. Cell. 2015;163(4):1011–1025. doi:10.1016/j.cell.2015.10.025
5. Robinson D, Van Allen EM, Wu YM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161(5):1215–1228. doi:10.1016/j.cell.2015.05.001
6. Grasso CS, Wu YM, Robinson DR, et al. The mutational landscape of lethal castration-resistant prostate cancer. Nature. 2012;487(7406):239–243. doi:10.1038/nature11125
7. Mateo J, Carreira S, Sandhu S, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373(18):1697–1708. doi:10.1056/NEJMoa1506859
8. Mateo J, Cheng HH, Beltran H, et al. Clinical outcome of prostate cancer patients with germline DNA repair mutations: retrospective analysis from an international study. Eur Urol. 2018;73(5):687–693. doi:10.1016/j.eururo.2018.01.010
9. Hussain M, Mateo J, Fizazi K, et al. Survival with olaparib in metastatic castration-resistant prostate cancer. N Engl J Med. 2020;383(24):2345–2357. doi:10.1056/NEJMoa2022485
10. de Bono J, Mateo J, Fizazi K, et al. Olaparib for metastatic castration-resistant prostate cancer. N Engl J Med. 2020;382(22):2091–2102. doi:10.1056/NEJMoa1911440
11. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
12. Wang L, Lu B, He M, Wang Y, Wang Z, Du L. Prostate cancer incidence and mortality: global status and temporal trends in 89 countries from 2000 to 2019. Front Public Heal. 2022;10:176.
13. López-Plaza B, Bermejo LM, Santurino C, Cavero-Redondo I, Álvarez-Bueno C, Gómez-Candela C. Milk and dairy product consumption and prostate cancer risk and mortality: an overview of systematic reviews and meta-analyses. Adv Nutr. 2019;10(suppl_2):S212–S223. doi:10.1093/advances/nmz014
14. Aune D, Navarro Rosenblatt DA, Chan DSM, et al. Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am J Clin Nutr. 2015;101(1):87–117. doi:10.3945/ajcn.113.067157
15. Mikami K, Ozasa K, Miki T, et al. Dairy products and the risk of developing prostate cancer: a large-scale cohort study (JACC Study) in Japan. Cancer Med. 2021;10(20):7298–7307. doi:10.1002/cam4.4233
16. Cooper CS, Eeles R, Wedge DC, et al. Analysis of the genetic phylogeny of multifocal prostate cancer identifies multiple independent clonal expansions in neoplastic and morphologically normal prostate tissue. Nat Genet. 2015;47(4):367–372. doi:10.1038/ng.3221
17. Boutros PC, Fraser M, Harding NJ, et al. Spatial genomic heterogeneity within localized, multifocal prostate cancer. Nat Genet. 2015;47(7):736–745. doi:10.1038/ng.3315
18. Fraser M, Sabelnykova VY, Yamaguchi TN, et al. Genomic hallmarks of localized, non-indolent prostate cancer. Nature. 2017;541(7637):359–364. doi:10.1038/nature20788
19. Ku SY, Gleave ME, Beltran H. Towards precision oncology in advanced prostate cancer. Nat Rev Urol. 2019;16(11):645–654. doi:10.1038/s41585-019-0237-8
20. Zhang W, van Gent DC, Incrocci L, van Weerden WM, Nonnekens J. Role of the DNA damage response in prostate cancer formation, progression and treatment. Prostate Cancer Prostatic Dis. 2019;23(1):24–37. doi:10.1038/s41391-019-0153-2
21. Lozano R, Castro E, Aragón IM, et al. Genetic aberrations in DNA repair pathways: a cornerstone of precision oncology in prostate cancer. Br J Cancer. 2021;124(3):552–563. doi:10.1038/s41416-020-01114-x
22. Momozawa Y, Iwasaki Y, Parsons MT, et al. Germline pathogenic variants of 11 breast cancer genes in 7051 Japanese patients and 11,241 controls. Nat Commun. 2018;9(1):4083. doi:10.1038/s41467-018-06581-8
23. Enomoto T, Aoki D, Hattori K, et al. The first Japanese nationwide multicenter study of BRCA mutation testing in ovarian cancer: cHARacterizing the cross-sectionaL approach to Ovarian cancer geneTic TEsting of BRCA (Charlotte). Int J Gynecol Cancer. 2019;29(6):1043LP.
24. Momozawa Y, Iwasaki Y, Hirata M, et al. Germline pathogenic variants in 7636 Japanese patients with prostate cancer and 12 366 controls. JNCI J Natl Cancer Inst. 2020;112(4):369–376. doi:10.1093/jnci/djz124
25. Oh M, Alkhushaym N, Fallatah S, et al. The association of BRCA1 and BRCA2 mutations with prostate cancer risk, frequency, and mortality: a meta-analysis. Prostate. 2019;79(8):880–895. doi:10.1002/pros.23795
26. Nyberg T, Frost D, Barrowdale D, et al. Prostate cancer risks for male BRCA1 and BRCA2 Mutation carriers: a prospective cohort study. Eur Urol. 2020;77(1):24–35. doi:10.1016/j.eururo.2019.08.025
27. Momozawa Y, Sasai R, Usui Y, et al. Expansion of cancer risk profile for BRCA1 and BRCA2 pathogenic variants. JAMA Oncol. 2022;8:871. doi:10.1001/jamaoncol.2022.0476
28. Mateo J, Boysen G, Barbieri CE, et al. DNA repair in prostate cancer: biology and clinical implications. Eur Urol. 2017;71(3):417–425. doi:10.1016/j.eururo.2016.08.037
29. Mateo J, Porta N, Bianchini D, et al. Olaparib in patients with metastatic castration-resistant prostate cancer with DNA repair gene aberrations (TOPARP-B): a multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2020;21(1):162–174. doi:10.1016/S1470-2045(19)30684-9
30. Abida W, Bryce AH, Vogelzang NJ, et al. Preliminary results from TRITON2: a Phase II study of rucaparib in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC) associated with homologous recombination repair (HRR) gene alterations. Ann Oncol. 2018;29:viii272. doi:10.1093/annonc/mdy284.002
31. Smith MR, Scher HI, Sandhu S, et al. Niraparib in patients with metastatic castration-resistant prostate cancer and DNA repair gene defects (GALAHAD): a multicentre, open-label, phase 2 trial. Lancet Oncol. 2022;23(3):362–373. doi:10.1016/S1470-2045(21)00757-9
32. Chi KN, Rathkopf DE, Smith MR, et al. Phase 3 MAGNITUDE study: first results of niraparib (NIRA) with Abiraterone acetate and prednisone (AAP) as first-line therapy in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC) with and without homologous recombination repair (HRR) gene alterations. Int J Med. 2022;40(6_suppl):12.
33. O’Connor MJ. Targeting the DNA damage response in cancer. Mol Cell. 2015;60(4):547–560. doi:10.1016/j.molcel.2015.10.040
34. Kalev P, Simicek M, Vazquez I, et al. Loss of PPP2R2A inhibits homologous recombination DNA repair and predicts tumor sensitivity to PARP inhibition. Cancer Res. 2012;72(24):6414–6424. doi:10.1158/0008-5472.CAN-12-1667
35. FDA. LYNPARZA (olaparib) prescribing information; 2020. Available from: www.accessdata.fda.gov/drugsatfda_docs/label/2020/208558s014lbl.pdf.
36. PMDA. LYNPARZA (olaparib) summary of product characteristics; 2020. Available from https://www.pmda.go.jp/files/000242574.pdf.
37. EMA. LYNPARZA (olaparib) summary of product characteristics; 2020. Available from: www.ema.europa.eu/en/documents/product-information/lynparza-epar-product-information_en.pdf.
38. Thiery-Vuillemin A, de Bono J, Hussain M, et al. Pain and health-related quality of life with olaparib versus physician’s choice of next-generation hormonal drug in patients with metastatic castration-resistant prostate cancer with homologous recombination repair gene alterations (PROfound): an open-lab. Lancet Oncol. 2022;23(3):393–405. doi:10.1016/S1470-2045(22)00017-1
39. Matsubara N, Nishimura K, Kawakami S, et al. Olaparib in patients with mCRPC with homologous recombination repair gene alterations: pROfound Asian subset analysis. Jpn J Clin Oncol. 2022;52(5):441–448. doi:10.1093/jjco/hyac015
40. Abida W, Patnaik A, Campbell D, et al. Rucaparib in men with metastatic castration-resistant prostate cancer harboring a BRCA1 or BRCA2 gene alteration. J Clin Oncol. 2020;38(32):3763–3772. doi:10.1200/JCO.20.01035
41. Giri VN, Hartman R, Pritzlaff M, Horton C, Keith SW. Germline variant spectrum among African American men undergoing prostate cancer germline testing: need for equity in genetic testing. JCO Precis Oncol. 2022;1(6):e2200234. doi:10.1200/PO.22.00234
42. Abida W, Armenia J, Gopalan A, et al. Prospective genomic profiling of prostate cancer across disease states reveals germline and somatic alterations that may affect clinical decision making. J Med. 2017;1(1):1–16.
43. Kimura H, Mizuno K, Narita S, et al. Analysis of genetic rare variants in Japanese advanced prostate cancer patients.
44. Li H, LaDuca H, Pesaran T, et al. Classification of variants of uncertain significance in BRCA1 and BRCA2 using personal and family history of cancer from individuals in a large hereditary cancer multigene panel testing cohort. Genet Med. 2020;22(4):701–708. doi:10.1038/s41436-019-0729-1
45. Jimenez-Sainz J, Jensen RB. Imprecise medicine: BRCA2 Variants of Uncertain Significance (VUS), the challenges and benefits to integrate a functional assay workflow with clinical decision rules. Genes. 2021;12:5. doi:10.3390/genes12050780
46. Uemura H, Oya M, Kamoto T, et al. A domestic multicenter observational study on the prevalence of homologous recombination repair-related gene mutations and prognosis in patients with metastatic castration-resistant prostate cancer in the real world: zENSHINStudy.
47. de Bono JS, Fizazi K, Saad F, et al. Central, prospective detection of homologous recombination repair gene mutations (HRRm) in tumour tissue from >4000 men with metastatic castration-resistant prostate cancer (mCRPC) screened for the PROfound study. Ann Oncol. 2019;30:v328–v329. doi:10.1093/annonc/mdz248.004
48. Mahal BA, Alshalalfa M, Kensler KH, et al. Racial differences in genomic profiling of prostate cancer. N Engl J Med. 2020;383(11):1083–1085. doi:10.1056/NEJMc2000069
49. Wyatt AW, Annala M, Aggarwal R, et al. Concordance of circulating tumor DNA and matched metastatic tissue biopsy in prostate cancer. JNCI J Natl Cancer Inst. 2017;109(12):djx118. doi:10.1093/jnci/djx118
50. Tukachinsky H, Madison RW, Chung JH, et al. Genomic analysis of circulating tumor DNA in 3334 patients with advanced prostate cancer identifies targetable BRCA alterations and AR resistance mechanisms. Clin Cancer Res. 2021;27(11):3094–3105. doi:10.1158/1078-0432.CCR-20-4805
51. Haffner MC, Zwart W, Roudier MP, et al. Genomic and phenotypic heterogeneity in prostate cancer. Nat Rev Urol. 2021;18(2):79–92. doi:10.1038/s41585-020-00400-w
52. Mizuno K, Sumiyoshi T, Okegawa T, et al. Clinical impact of detecting low-frequency variants in cell-free DNA on treatment of castration-resistant prostate cancer. Clin Cancer Res. 2021;27(22):6164–6173. doi:10.1158/1078-0432.CCR-21-2328
53. Matsubara N, Kato T, Fujisawa T, et al. Landscape of genomic alterations of circulating tumor DNA in advanced genitourinary cancer patients: SCRUM-Japan MONSTAR SCREEN Project. J Clin Oncol. 2021;39(6_suppl):152. doi:10.1200/JCO.2021.39.6_suppl.152
54. Abbosh C, Swanton C, Birkbak NJ. Clonal haematopoiesis: a source of biological noise in cell-free DNA analyses. Ann Oncol off J Eur Soc Med Oncol. 2019;30(3):358–359. doi:10.1093/annonc/mdy552
55. Jensen K, Konnick EQ, Schweizer MT, et al. Association of clonal hematopoiesis in DNA repair genes with prostate cancer plasma cell-free DNA testing interference. JAMA Oncol. 2021;7(1):107–110. doi:10.1001/jamaoncol.2020.5161
56. FDA. List of Cleared and Approved Companion Diagnostic Devices; 2022, Available from https://www.fda.gov/media/119249/download.
57. Saad F, Armstrong AJ, Thiery-Vuillemin A, et al. PROpel: Phase III trial of olaparib (ola) and Abiraterone (abi) versus placebo (pbo) and abi as first-line (1L) therapy for patients (pts) with metastatic castration-resistant prostate cancer (mCRPC). J Med. 2022;40(6_suppl):11.
58. Agarwal N, Azad A, Fizazi K, et al. Talapro-3: a phase 3, double-blind, randomized study of enzalutamide (ENZA) plus talazoparib (TALA) versus placebo plus enza in patients with DDR gene mutated metastatic castration-sensitive prostate cancer (mCSPC). J Clin Oncol. 2022;40(6_suppl):TPS221. doi:10.1200/JCO.2022.40.6_suppl.TPS221
59. Rathkopf DE, Chi KN, Olmos D, et al. AMPLITUDE: a study of niraparib in combination with Abiraterone acetate plus prednisone (AAP) versus AAP for the treatment of patients with deleterious germline or somatic homologous recombination repair (HRR) gene-altered metastatic castration-sensitive. J Clin Oncol. 2021;39(6_suppl):TPS176. doi:10.1200/JCO.2021.39.6_suppl.TPS176
60. Chatterjee P, Schweizer MT, Lucas JM, et al. Supraphysiological androgens suppress prostate cancer growth through androgen receptor–mediated DNA damage. J Clin Invest. 2019;129(10):4245–4260. doi:10.1172/JCI127613
61. Cheng HH, Pritchard CC, Boyd T, Nelson PS, Montgomery B. Biallelic inactivation of BRCA2 in platinum-sensitive metastatic castration-resistant prostate cancer. Eur Urol. 2016;69(6):992–995. doi:10.1016/j.eururo.2015.11.022
62. van der Doelen MJ, Isaacsson Velho P, Slootbeek PHJ, et al. Impact of DNA damage repair defects on response to radium-223 and overall survival in metastatic castration-resistant prostate cancer. Eur J Cancer. 2020;136:16–24. doi:10.1016/j.ejca.2020.05.001
63. Isaacsson Velho P, Qazi F, Hassan S, et al. Efficacy of radium-223 in bone-metastatic castration-resistant prostate cancer with and without homologous repair gene defects. Eur Urol. 2019;76(2):170–176. doi:10.1016/j.eururo.2018.09.040
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
