Back to Journals » Journal of Pain Research » Volume 16
Robot-Assisted Percutaneous Balloon Compression in Elderly Patients with Trigeminal Neuralgia
Authors Tan K , Li J, Peng Y, Wu W, Yang Z, Wang Y, Wang Y
Received 18 November 2022
Accepted for publication 22 March 2023
Published 6 April 2023 Volume 2023:16 Pages 1161—1168
DOI https://doi.org/10.2147/JPR.S396680
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Natalie Strand
Video abstract of "Robot-assisted PBC in elderly patients with TG" [ID 396680].
Views: 164
Ke Tan, Jinping Li, Yutao Peng, Wenqian Wu, Ziwen Yang, Yu Wang, Yang Wang
Department of Neurosurgery, BeiJing ChaoYang Hospital, Capital Medical University, Beijing, 100020, People’s Republic of China
Correspondence: Ke Tan, Email [email protected]
Objective: To investigate the clinical effects of percutaneous balloon compression (PBC) for trigeminal neuralgia in elderly patients with the assistance of a neurosurgical navigation and positioning planning system (referred to hereafter as the robot).
Methods: We performed a retrospective analysis of 11 patients with trigeminal neuralgia. Preoperative TOF MRA, T2WI-SPACE, and thin-slice CT scans were performed, and the volume of Meckel’s Cave was calculated by multi-modal image fusion on a workstation. Surgical planning involved two paths. Path A was the actual puncture path, the target point was the anterior inner quadrant of the inner opening of the foramen ovale; Path B represented a virtual path for measurement, and was used to plan the depth of balloon placement. The foramen ovale puncture for path A was completed under the guidance of a robotic arm adapter, while path B was completed under lateral X-ray fluoroscopy with a DSA machine. The balloon was placed at a predetermined depth, and filled to a “pear” shape to complete the operation. Preliminary follow-up results were obtained by considering VAS score and BNI classification.
Results: The foramen ovale was successfully punctured in all 11 patients and entered Meckel’s Cave, the balloon was then filled to create a “pear shape”. Immediate complete healing was achieved in 10 patients and delayed healing was achieved in one patient by the 5th postoperative day. No serious complications were identified that were related to surgery, and over a follow-up time of 1– 12 months, there was no recurrence of pain, and a BNI numbness grade of 2– 3 points. The appropriate ratio of the balloon inflated volume to the preoperative Meckel’s Cave volume was approximately 1.7.
Conclusion: Preliminary clinical application and short-term follow-up showed that robot-assisted PBC surgery is a safe and effective surgical method for elderly patients with trigeminal neuralgia.
Keywords: trigeminal neuralgia, robotics, percutaneous balloon compression, stereotactic neurosurgery, technique
Introduction
Trigeminal neuralgia (TN) is a common clinical cranial nerve disease with a population prevalence of 0.16%-0.3%. TN mostly occurs in adults and the elderly with a mean age of onset of 53–57 years.1 As the course of this disease is prolonged, the number of elderly patients with TN is increasing. Microvascular decompression (MVD) is the first-line choice of surgery for TN and has definite short-term and long-term effects. However, for recurrent cases of MVD, secondary TN such as tumor or multiple sclerosis,2 for cases without evidence of neurovascular conflict with poor drug tolerance, percutaneous minimally invasive therapy including percutaneous balloon compression (PBC) is a good indication. Moreover, for many elderly patients, their infirm physical conditions are not resistant to posterior fossa craniotomy. Concerns, and the fear of craniotomy itself, restrict the willingness of elderly patients to undergo MVD surgery. Therefore, percutaneous minimally invasive therapy including PBC is generally accepted by elderly patients.3 Traditional PBC surgery is performed with a surgeon’s bare hands under X-ray fluoroscopy; however, this may be affected by the experience of the operator and the stability of the operation. There are risks associated with this procedure such as the inaccurate positioning of the puncture needle, deviation of the direction and depth of balloon placement, and even serious neurovascular complications.4 New neuronavigational methods including robot-assisted techniques have been reported for PBC surgery.5,6 Beijing Chaoyang Hospital Affiliated to Capital Medical University completed 11 cases of PBC surgery in elderly patients with TN (≥65 years-of-age) between August 2021 and August 2022, by deploying neurosurgery navigation and positioning planning system (referred to hereafter as the robot). During these surgeries, we achieved clinical results with good curative effects. Here, we provide a retrospective analysis of our results.
Materials and Methods
Clinical Data
Of the 11 patients, 5 were male and 6 were female. Age ranged from 65 to 82 years and the disease course ranged from 8 months to 13 years. All patients presented with typical trigeminal neuralgia with recurrent, transient and severe pain in the area of one or more trigeminal nerves on one side of the face. There was 1 case of pain in one branch of I, 4 cases of one branch of II, 2 cases of one branch of III, 2 cases of branch II+III, and 2 cases of branch I+II. In total, 10 patients had a history of carbamazepine treatment for more than half a year; the maximum dose was 1200 mg/day, and the efficacy decreased, or could not be tolerated due to adverse reactions. Another case was allergic to carbamazepine, oral pregabalin (150mg/day) was ineffective. Nine cases in this group were initial cases, one case had experienced the recurrence of PBC, and one case had experienced the recurrence of MVD. Preoperative head MRI examination revealed no space-occupying lesions in the cerebellopontine angle, except for secondary trigeminal neuralgia. If there was a contraindication to MVD surgery, or the patients and their families refused craniotomy, they were given informed consent to PBC surgery assisted by the robot and provided signed and the informed consent. The clinical data are shown in Table 1.
 |
Table 1 Summary of Patient Characteristics |
Pre-Operative Preparation
All patients underwent magnetic resonance examination: three-dimensional time-of-flight magnetic resonance angiography (3D-TOF-MRA) and trigeminal nerve three-dimensional T2 weighted imaging-sampling perfection with application optimized contrasts using different flip angle evolutions (3D-T2WI-SPACE), and a layer thickness of 0.65mm. Prior to surgery and under local anesthesia, bone screws (Sinovation, Beijing, China.) were inserted in 2 cases, or scalp markers in 7 cases (Remebot, Beijing, China, type MK-06A) were attached to the forehead of the patient. The thin-slice CT scan ranged from the mandible to the top of the head, and the slice thickness was 1 mm without intervals. The MRI and CT imaging data were then transferred to the robot navigation workstation (RM-200, Remebot, Beijing, China or SR1, Sinovation, Beijing, China) to perform image fusion, and generate a 3D model. In the 3D T2WI-SPACE sequence, the morphological modeling of Meckel’s Cave was outlined in surgical plan software, and the volume of Meckel’s Cave was calculated.
Surgical Plan
Two trajectories were used for surgery. Trajectory A was the actual puncture path; the entry point was approximately 2.5 cm lateral to the angle of the mouth on the ipsilateral side. The target point was the anterior and inner quadrant of the inner orifice of the foramen ovale. The entry point of trajectory B was the target point of trajectory A; the target point was located near the trigeminal foramen in Meckel’s Cave; the lengths of the two paths were recorded respectively (Figure 1). Trajectory A was guided by the robotic arm to complete the puncture, while trajectory B was guided by lateral X-ray fluoroscopy (UNIQ FD20, Philips) to place the balloon catheter and confirm that the position, depth and shape of the balloon were correct.
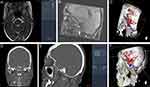
The Surgical Procedure (Figure 2)
The surgery was performed under general anesthesia with the patient in the supine position with the head tilted slightly back. The first case was fixed with a Mayfield head frame; the other 10 cases were fixed with a shaping pillow. The surgical plan and was loaded and we connected and fixed the connecting arm of the robot with the head frame or the bottom of the operating bed. We used bone screws or scalp markers for the robotic arm and patient registration; this was verified to ensure that the registration error was < 0.3mm. The face was sterilized with alcohol and the robotic arm was automatically navigated and positioned. We connected the adapter, and adjustments were made with regards to the predetermined depth of the puncture needle (CTZ-14; Qingyuan Shenzhen China). The puncture needle cannula was placed in the direction of trajectory A under the guidance of the robotic arm until the tail of the needle tail reached the adapter; and the needle was located at the inner port of the foramen ovale at the target point of trajectory A. We confirmed the needle position again under lateral X-ray fluoroscopy (FD20, Philips Medical Systems, Best, the Netherlands). A 5F Fogarty balloon catheter kit (QK08S50, Qingyuan, Shenzhen, China) was then inserted. When the catheter passed the first scale line, there was generally a sense of breakthrough. The needle was inserted according to the length of trajectory B to the predetermined depth. The tip of the balloon catheter was located at the target point of trajectory B. The position of the balloon was then reconfirmed under lateral X-ray fluoroscopy, and 0.3 mL of contrast agent (iohexol) was injected for exploratory filling; the bottom of balloon is strengthened to a volume of 0.5–0.8 mL. The balloon was “pear” shaped. (Figure 3) Individualized balloon inflation compression time ranged from 120–480 seconds, with longer time for recurrent cases. (Table 2) After compression was completed, the contrast agent was withdrawn, the balloon catheter and the puncture needle cannula were completely withdrawn, the puncture point was compressed for ten minutes, and the surgery was finally completed.
 |
Table 2 Surgery Results |
Efficacy Evaluation and Follow-Up
Preoperative and postoperative visual analog scale (VAS) was used to evaluate the degree of pain, and Barrow Neurological Institute (BNI) grading was used to evaluate the degree of facial numbness after surgery. Follow-up results were obtained from 1 month to 12 months after surgery by non-surgical doctors via the outpatient service, telephone or video call.
Results
The Relationship Between Balloon Filling Volume and Meckel’s Cave Volume
There were individual differences in the volume of Meckel’s Cave. The volume of Meckel’s Cave was determined to be 0.32–0.46mL prior to surgery. During surgery, the balloon was inflated to a “pear” shape and filling was stopped when significant resistance was felt. There was a certain proportional relationship between the volume of the capsule, see Table 2. After calculating the mean value, we found that the appropriate ratio between the balloon filling volume and the volume of Meckel’s Cave was approximately 1.7:1.
Balloon Insertion Depth
If the balloon was placed too deep, it can easily to protrude into the posterior cranial fossa, and form a “dumbbell shape” after filling or breaking through the dura at the base of the skull, thus increasing the risk of additional neurovascular injury. The insertion depth of the balloon catheter generally did not exceed the third scale line (25mm). Intraoperative X-ray lateral fluoroscopy was used to monitor the depth of balloon insertion in real time. Generally, when the first branch was painful, the implantation position was relatively deep, while the third branch disease was placed slightly shallower. During preoperative planning, by observing the location of the target point of the setting trajectory B, the ideal implantation depth could be determined individually. In this group, the implantation depth was 15.9–23.8mm; the shallowest case was a pain in the third branch and chronic occlusion of the contralateral internal carotid artery was found during the preoperative examination. To reduce the risk of vascular injury, a shallower implantation depth was planned.
Surgical Outcomes and Complications
For all 11 patients we successfully punctured the foramen ovale and entered Meckel’s Cave; the balloon was then filled to adopt a “pear” shape. Two cases of balloon rupture occurred during surgery and the operation was completed by low-volume stepped compression and prolonged time. The trigeminal neuralgia in 10 cases was completely relieved immediately after surgery, and the pain in one case was delayed relieved by day 5 post-surgery. The VAS score decreased from 8 to 10 points before surgery to 0 points post-surgery. All patients had obvious numbness after surgery, and the BNI score was 3 points. There were 4 cases of weak masticatory muscle strength and 2 cases of dry eyes. In our cases, we did not observe any incidences of vascular injury, reduced visual acuity, diplopia, ocular hyperemia or infection. Herpes simplex virus reactivation is another not so rare PBC related complication. We routinely use Acyclovir after surgery and have not seen it yet in all these cases.7
Follow-Up Results
The 11 patients were followed up for 1–12 months; there was no recurrence of pain, and the VAS was 0 points. Eight cases of numbness recovered to a BNI of 2 points, 3 cases remained on 3 points; 4 cases involving weak masticatory muscles recovered; one case of dry eyes recovered. The clinical results are shown in Table 2.
Discussion
Compared with traditional MVD surgery, PBC surgery is relatively shorter and less invasive and is especially suitable for the elderly, infirm, or those with severe systemic diseases who cannot tolerate craniotomy.1,3 Mullan was the first to report PBC surgery in the early 1980s, this type of surgery is now widely performed worldwide8 and is included and recommended in the guidelines on trigeminal neuralgia.9 Long-term clinical practice has shown that if the quality of PBC surgery and effective “pear formation” is ensured, then better pain relief rates and lower recurrence rates can be obtained.10–12
Traditional PBC surgery is performed under the guidance of X-ray or CT,13–17 although lateral X-ray alone can only provide two-dimensional non-sectional images and cannot fully display the complex skull base bony structure and foramen ovale. However, using various improved CT-guided techniques18,19 or surgery under electromagnetic navigation20,21 still relies on the operator’s free-hand operation and lacks the constraints of a fixed frame. The first cases of robotic-guided procedures for PBC were reported in August 2022, compared to other neuronavigational methods, robotics offers distinct advantages including increased precision, dexterity, durability, and resilience to fatigue that ultimately may result in improved safety and accuracy.5,6 Consequently, this procedure has a certain learning curve and that is more dependent on the experience of the surgeon, especially when there are anatomical variations in a patient, this may lead to uncontrollable surgical risks.
In comparison, robot-assisted PBC surgery has several advantages. First, robot-assisted PBC surgery uses robotic arm-assisted positioning and has a high puncture success rate. Using robot-assisted technology, the registration errors of this group of cases were all < 0.3 mm. A successful one-time foramen ovale puncture avoids the secondary injury and radiation exposure caused by repeated operations, and can significantly shorten the surgical learning curve for novices. Secondly, the depth and direction of the puncture are strictly constrained by the robotic arm to avoid damage to the intracranial structure. A special adapter is used, and the robotic arm is automatically positioned to the predetermined depth to avoid the serious vascular and nerve injury complications caused by an overly deep puncture or direction deviation during manual operation. Third, preoperative planning and multimodal image navigation guide the balloon from the best position to enter Meckel’s Cave. The success rate with regards to forming a “pear” is high, and the surgical effect is significantly improved; with this respect, our results are consistent with those published previously.6 With the inherent anatomical position and direction of the foramen ovale, the puncture direction from the foramen ovale into Meckel’s Cave and the direction of the puncture path from the outer skin of the corner of the mouth to the foramen ovale has a certain downwards and outwards angle. If the plan is to puncture from the outer corner of the mouth to Meckel’s Cave, the skin puncture point will be too low. During manual surgery, the head is tilted back, and it is necessary to adjust the height of the needle tail after reaching the foramen ovale and continuing to puncture Meckel’s Cave or make a secondary adjustment of the path during robot-assisted surgery. Our choice was to target the puncture route in the anterior medial quadrant of the foramen ovale, but without entering the center of Meckel’s Cave The target was close to the anterior and lower part of Meckel’s Cave. The dura at the base of the skull could not be peeled off easily due to the transition of the foramen ovale. When entering with a balloon catheter, there was often a clear sense of breakthrough; this can be used as an effective sign for entering Meckel’s Cave. In fact, successful punction of foramen ovale did not always mean successful entry into Meckel’s Cave, and in few cases adjustment of trajectory was required. In these cases, after completing trajectory A, the robot arm was adjusted to follow trajectory B with target point puncture a little deeper confirmed by X-ray lateral fluoroscopy, sometimes requiring more attempts and patience. During preoperative planning, the depth of balloon placement should be determined by specific measurements avoid deep damage to the cavernous sinus or temporal lobe or crossing of the petrosal ridge into the posterior cranial fossa.
The pain of the 11 elderly patients in this group was completely relieved immediately after robot-assisted PBC in 10 cases; the pain in one case completely disappeared 5 days after surgery. The mechanism underlying this delayed healing remains unclear. The balloon was inserted in place accurately and the effective formation of a “pear” was the key to ensuring good surgical effect.22 None of the patients experienced pain recurrence during the follow-up period of 1–12 months after surgery, and there were no serious complications such as vascular injury, ulcerative keratitis, vision loss, diplopia, or infection. Preliminary studies have shown that robot-assisted PBC surgery has good safety and efficacy; however, the long-term effects of this type of surgery need to be evaluated with longer follow-ups.
Four patients in this group developed mild weakness of the masticatory muscle on the same side after surgery; this was relieved when assessed 3-month follow-up. All patients developed obvious ipsilateral facial numbness after the operation; the BNI score was 3 points. To balance the relationship between recurrence and numbness after PBC surgery, and to improve the surgical experience and quality of life of patients, it is necessary to individualize, quantitative and perform precise surgical operations, such that we can reasonably reduce the compression time, and select a reasonable balloon filling pressure and volume.23–25 Considering the individual differences in Meckel’s Cave volume, there should be a certain proportional relationship between the ideal balloon filling volume and Meckel’s Cave volume. When the balloon was filled to a satisfactory “pear” shape and there was significant resistance during the operation, it is necessary to stop the filling. We calculated the ratio of the balloon filling volume to the Meckel’s Cave volume measured prior to surgery. After considering mean values, we found that the appropriate ratio was approximately 1.7. Moreover, considering that the patients in this group were all elderly patients who received surgery for the first time, there was brain tissue atrophy and the structure around Meckel’s Cave which may be relatively loose. Further studies are needed to investigate the appropriate volume ratio for all age groups and recurrent patients.
Compared with conventional X-ray-guided PBC surgery, robot-assisted technology preparations are more tedious. Furthermore, procedures such as surgical planning and robotic arm registration and adjustment will prolong the operation time. Our study identified some improvements and explorations with regards to the surgical procedure. The first 2 patients were marked with bone screws; this caused additional trauma pain; the last 9 patients were marked with scalp markers; this met the needs for registration accuracy, and should be investigated further in the future. The registration process is further optimized by avoiding the use of markers for structured light registration and other methods. Secondly, except for the first case which was fixed with a Mayfield head frame, the last 10 cases were all fixed with a plastic pillow. Shaped pillows can provide better occipital neck support, are more suitable for maintaining stability during oral and facial puncture procedures, and also improve postoperative comfort for patients.
In conclusion, the preliminary clinical application and follow-up of robot-assisted PBC surgery in elderly patients with trigeminal neuralgia indicate that it is a safe and effective new surgical method. In addition to assisting in the precise positioning of the foramen ovale and shortening the initial learning curve, multi-modal image navigation can determine the appropriate balloon filling volume and insertion depth according to Meckel’s Cave volume. This individualized form of precision surgery can improve the surgical effect. Although the immediate pain relief rate was high in this group of cases, the number of cases reported here is small. Further follow-up studies are required with larger case numbers.
Statement of Ethics
The studies involving human participants were reviewed and approved by Medical Ethics Committee of BeiJing ChaoYang Hospital, Capital Medical University. The patients provided their written informed consent prior to the procedure to participate in this surgery and to view their medical records. Data reported in the study have been completely anonymized. The confidentiality of patient data is in accordance with the Declaration of Helsinki.
Funding
This research was funded by the Innovation Technology Project, Beijing Chao-Yang Hospital, Capital Medical University (Reference: 22KCJJYB-4) in the preparation of data and the manuscript.
Disclosure
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Lambru G, Zakrzewska J, Matharu M. Trigeminal neuralgia: a practical guide. Pract Neurol. 2021;21(5):392–402. doi:10.1136/practneurol-2020-002782
2. Berra LV, Armocida D, Mastino L, et al. Trigeminal Neuralgia Secondary to Intracranial Neoplastic Lesions: a Case Series and Comprehensive Review. J Neurol Surg a Cent Eur Neurosurg. 2021;82(2):118–124. doi:10.1055/s-0040-1718708
3. Li MW, Jiang XF, Niu CS. Efficacy of and risk factors for percutaneous balloon compression for trigeminal neuralgia in elderly patients. Br J Neurosurg. 2021;35(3):280–284. doi:10.1080/02688697.2020.1787341
4. Texakalidis P, Xenos D, Tora MS, Wetzel JS, Boulis NM. Comparative safety and efficacy of percutaneous approaches for the treatment of trigeminal neuralgia: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2019;182:112–122. doi:10.1016/j.clineuro.2019.05.011
5. Graciolli Cordeiro J, Assumpcao de monaco B, Theodotou CB, et al. Robotic-assisted stereotactic percutaneous balloon compression for trigeminal neuralgia treatment. Clin Neurol Neurosurg. 2022;221:107412. doi:10.1016/j.clineuro.2022.107412
6. Liu QQ, Wang JJ, Wang CQ, et al. Robot-Assisted Percutaneous Balloon Compression for Trigeminal Neuralgia: technique Description and Short-Term Clinical Results. Front Surg. 2022;9(3):869223. doi:10.3389/fsurg.2022.869223
7. Berra LV, Armocida D, Pesce A, et al. Herpes Simplex Reactivation After Surgical Treatment of Trigeminal Neuralgia: a Retrospective Cohort Study. World Neurosurg. 2019;127:e16–e21. doi:10.1016/j.wneu.2019.01.226
8. Cruccu G, Di Stefano G, Truini A. Trigeminal Neuralgia. N Engl J Med. 2020;383(8):754–762. doi:10.1056/NEJMra1914484
9. Bendtsen L, Zakrzewska JM, Abbott J, et al. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol. 2019;26(6):831–849. doi:10.1111/ene.13950
10. Bendtsen L, Zakrzewska JM, Heinskou TB, et al. Advances in diagnosis, classification, pathophysiology, and management of trigeminal neuralgia. Lancet Neurol. 2020;19(9):
11. Zheng S, Yuan R, Ni J, et al. Long-term recurrence-free survival and complications of percutaneous balloon compression and radiofrequency thermocoagulation of Gasserian ganglion for trigeminal neuralgia: a retrospective study of 1313 cases. Pain Pract. 2022;22(5):532–540. doi:10.1111/papr.13114
12. Noorani I, Lodge A, Vajramani G, et al. Comparing Percutaneous Treatments of Trigeminal Neuralgia: 19 Years of Experience in a Single Centre. Stereotact Funct Neurosurg. 2016;94(2):75–85. doi:10.1159/000445077
13. Mendes PD. Percutaneous foramen ovale puncture: usefulness of intraoperative CT control, in the eventuality of a narrow foramen. Stereotact Funct Neurosurg. 2021;99(1):75–78. doi:10.1159/000509821
14. Xiao X, Wei Z, Ren H, et al. Comparison of effectiveness and safety between intraoperative 3D-CT-guided and C-arm-guided percutaneous balloon compression for idiopathic trigeminal neuralgia: a multi-center retrospective study. Pain Res Manag. 2021;2021:9306532. doi:10.1155/2021/9306532
15. Scranton RA, Shah K, Cohen-Gadol AA. Alternative customized instrumentation and technique for percutaneous balloon compression rhizotomy for trigeminal neuralgia. J Neuro surg. 2019;132(6):1938–1941. doi:10.3171/2019.2.JNS182896
16. Barlas O, Unal TC. A technique to facilitate the cannulation of the foramen ovale for balloon compression. Br J Neurosurg. 2021;30:1–4. doi:10.1080/02688697.2021.1907308
17. Sandwell S, Montoya S, Towner JE, et al. Anatomical Study of Percutaneous Trigeminal Compressive Balloon Positioning on Merged 3-D Rotational X-Ray and Preprocedural Magnetic Resonance Imaging. Stereotact Funct Neurosurg. 2018;96(3):182–189. doi:10.1159/000489947
18. Arishima H, Kawajiri S, Arai H, et al. Percutaneous Glycerol Rhizotomy for Trigeminal Neuralgia Using a Single-Plane, Flat Panel Detector Angiography System: technical Note. Neurol Med Chir (Tokyo). 2016;56(5):257–263. doi:10.2176/nmc.tn.2015-0286
19. Peng Y, Xie Z, Chen S, et al. Evaluation of the effects of personalized 3D-printed jig plate-assisted puncture in trigeminal balloon compression. Br J Neurosurg. 2021;19:1–7. doi:10.1080/02688697.2021.1886241
20. Wiggins A, Lonie M, Pimentil I, et al. Electromagnetic neuronavigation for the percutaneous treatment of trigeminal neuralgia with balloon compression: technical note and cadaveric validation study. Acta Neurochir. 2018;160(7):1337–1341. doi:10.1007/s00701-018-3548-2
21. Aydoseli A, Akcakaya MO, Aras Y, et al. Neuronavigation-assisted percutaneous balloon compression for the treatment of trigeminal neuralgia: the technique and short-term clinical results. Br J Neurosurg. 2015;29(4):552–558. doi:10.3109/02688697.2015.1019418
22. Lv W, Hu W, Chi L, et al. Factors that may delay disappearance of trigeminal neuralgia after percutaneous balloon compression. Neurol Neurochir Pol. 2022;56(2):156–162. doi:10.5603/PJNNS.a2022.0017
23. Wang Q, Chen C, Guo G, et al. A prospective study to examine the association of the foramen ovale size with intraluminal pressure of pear‐shaped balloon in percutaneous balloon compression for trigeminal neuralgia. Pain Ther. 2021;10(2):
24. Kourilsky A, Palpacuer C, Rogers A, et al. Multivariate models to predict pain recurrence and sensitive complications after percutaneous balloon compression in trigeminal neuralgia. J Neurosurg. 2022:1–10. doi:10.3171/2022.2.JNS212644
25. Lv W, Hu W, Chi L, Zhang L. Factors that may affect recurrence of trigeminal neuralgia after percutaneous balloon compression. J Clin Neurosci. 2022;99(5):248–252. doi:10.1016/j.jocn.2022.03.022
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.