Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
RETRO-POPE: A Retrospective, Multicenter, Real-World Study of All-Cause Mortality in COPD
Authors Koblizek V , Milenkovic B , Svoboda M, Kocianova J , Holub S, Zindr V, Ilic M, Jankovic J, Cupurdija V , Jarkovsky J, Popov B, Valipour A
Received 21 June 2023
Accepted for publication 9 November 2023
Published 17 November 2023 Volume 2023:18 Pages 2661—2672
DOI https://doi.org/10.2147/COPD.S426919
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 7
Editor who approved publication: Dr Richard Russell
Vladimir Koblizek,1,2 Branislava Milenkovic,3,4 Michal Svoboda,5,6 Jana Kocianova,7 Stanislav Holub,8 Vladimir Zindr,9 Miroslav Ilic,10,11 Jelena Jankovic,3,4 Vojislav Cupurdija,12,13 Jiri Jarkovsky,6 Boris Popov,14 Arschang Valipour15
1Department of Pneumology, University Hospital, Hradec Kralove, Czech Republic; 2Faculty of Medicine Hradec Kralove, Charles University, Hradec Kralove, Czech Republic; 3Clinic for Pulmonary Diseases, Clinical Center of Serbia, Belgrade, Serbia; 4Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 5Institute of Biostatistics and Analyses Ltd., Brno, Czech Republic; 6Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno, Czech Republic; 7Outpatient Department of Pneumology Alveolus, APRO MED, Ostrava, Czech Republic; 8Outpatient Chest Clinic, Plicni Stredisko Teplice Ltd., Teplice, Czech Republic; 9Outpatient Chest Clinic, PNEUMO KV Ltd., Karlovy Vary, Czech Republic; 10Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia; 11Clinic for Tuberculosis and Interstitial Lung Diseases, PolyClinic Department, Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica, Serbia; 12Department of Internal Medicine, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia; 13Clinic for Pulmonology, University Clinical Center Kragujevac, Kragujevac, Serbia; 14Medicine Department, Boehringer Ingelheim Serbia d.o.o. Beograd, Belgrade, Serbia; 15Karl Landsteiner Institute for Lung Research and Pulmonary Oncology, Klinik Floridsdorf, Vienna Health Care Group, Vienna, Austria
Correspondence: Vladimir Koblizek, Email [email protected]
Purpose: The Phenotypes of COPD in Central and Eastern Europe (POPE) study assessed the prevalence and clinical characteristics of four clinical COPD phenotypes, but not mortality. This retrospective analysis of the POPE study (RETRO-POPE) investigated the relationship between all-cause mortality and patient characteristics using two grouping methods: clinical phenotyping (as in POPE) and Burgel clustering, to better identify high-risk patients.
Patients and Methods: The two largest POPE study patient cohorts (Czech Republic and Serbia) were categorized into one of four clinical phenotypes (acute exacerbators [with/without chronic bronchitis], non-exacerbators, asthma–COPD overlap), and one of five Burgel clusters based on comorbidities, lung function, age, body mass index (BMI) and dyspnea (very severe comorbid, very severe respiratory, moderate-to-severe respiratory, moderate-to-severe comorbid/obese, and mild respiratory). Patients were followed-up for approximately 7 years for survival status.
Results: Overall, 801 of 1,003 screened patients had sufficient data for analysis. Of these, 440 patients (54.9%) were alive and 361 (45.1%) had died at the end of follow-up. Analysis of survival by clinical phenotype showed no significant differences between the phenotypes (P=0.211). However, Burgel clustering demonstrated significant differences in survival between clusters (P< 0.001), with patients in the “very severe comorbid” and “very severe respiratory” clusters most likely to die. Overall survival was not significantly different between Serbia and the Czech Republic after adjustment for age, BMI, comorbidities and forced expiratory volume in 1 second (hazard ratio [HR] 0.80, 95% confidence interval [CI] 0.65– 0.99; P=0.036 [unadjusted]; HR 0.88, 95% CI 0.7– 1.1; P=0.257 [adjusted]). The most common causes of death were respiratory-related (36.8%), followed by cardiovascular (25.2%) then neoplasm (15.2%).
Conclusion: Patient clusters based on comorbidities, lung function, age, BMI and dyspnea were more likely to show differences in COPD mortality risk than phenotypes defined by exacerbation history and presence/absence of chronic bronchitis and/or asthmatic features.
Plain Language Summary: People with COPD have difficulty breathing and can have a greater risk of death (mortality) than people without COPD. However, the mortality risk of a person with COPD depends on their individual clinical profile. Previous studies have shown that grouping patients into different “phenotypes” based on their respiratory symptoms or into “clusters” based on additional characteristics, including their age, body mass index and illnesses they have alongside COPD, can help to predict mortality.
There is limited data on COPD-related mortality in Central and Eastern Europe (CEE). In 2014– 2015, a large, cross-sectional study conducted across 11 countries in CEE (the POPE study) analyzed the prevalence of different patient phenotypes but did not assess mortality. In this retrospective analysis of the POPE study, we assessed mortality in 801 patients with COPD in two countries (the Czech Republic and Serbia) over a 7-year follow-up period. We grouped patients by clinical phenotypes and clusters to see which method provided significant differences between the groupings when it came to patient survival.
We found that most patients with COPD died due to diseases related to their airways and lungs. However, when grouping patients into clinical phenotypes based on respiratory symptoms alone, differences in risk of death between groups were only seen in one country. Grouping patients into clusters showed differences in risk of death between clusters for both countries. Patients with worse lung function and who were more breathless had a higher risk of death, along with those with other severe diseases alongside their COPD.
Keywords: COPD, survival, mortality, Central and Eastern Europe, respiratory, clinical phenotype, cluster
Introduction
COPD represents a major health concern in Central and Eastern Europe (CEE) due to the high prevalence of smoking in the region.1 Alongside this, there is an increasing prevalence of COPD in non-smokers, due in part to environmental exposure to airborne pollutants.2
In 2014–2015, the Phenotypes of COPD in Central and Eastern Europe (POPE) study (NCT02119494) assessed the prevalence of four clinical phenotypes according to predefined clinical criteria (acute exacerbators [with/without chronic bronchitis], non-exacerbators [NON-AE] and those with asthma–COPD overlap syndrome [ACOS]).3,4 In the POPE study, the majority of patients (63%) were non-exacerbators, and statistically significant differences in disease severity, comorbidities and prescribed therapy were seen between the four phenotypes.4
Clinical phenotyping has previously been shown to be useful in predicting mortality in patients with COPD. For example, longitudinal studies conducted in Spain and the Czech Republic have consistently shown a higher mortality risk in patients with an exacerbation phenotype (with or without chronic bronchitis), compared with NON-AE and those with ACOS.5–7 Other studies have shown that a clustering approach, which groups patients based on clinical features such as comorbidities, dyspnea, and lung function, is also a useful predictor of mortality.8–12 In one study, cluster analysis was found to be significantly superior to the 2017 Global Initiative for Chronic Obstructive Lung Disease (GOLD) 1–4 spirometry classification system for predicting mortality, with similar predictive ability to other systems such as the body mass index (BMI), obstruction, dyspnea and exercise (BODE) index and the GOLD ABCD classification.10 However, to our knowledge, no study has compared clustering to clinical phenotyping for predicting mortality in patients with COPD.
In this retrospective analysis of the POPE study (RETRO-POPE), we investigated the association between different COPD clinical phenotypes or clusters12 and mortality in patients from two countries (Czech Republic and Serbia).
Methods
Study Design
The POPE study was an international, observational, cross-sectional cohort study that included 11 CEE countries (Austria, Bulgaria, Croatia, Czech Republic, Hungary, Latvia, Poland, Russia, Serbia, Slovakia and Slovenia). It was conducted between April 2014 and July 2015.3,4 This retrospective post hoc analysis (RETRO-POPE) assessed survival over a 7-year follow-up period in patients with COPD from seven sites across the Czech Republic and Serbia, the two countries that enrolled the most patients in the POPE study.
Inclusion/Exclusion Criteria
Patients were recruited consecutively into the POPE study if they were >40 years of age, had a clinical diagnosis of COPD confirmed by their pulmonary physician, post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity <0.7, and stable disease (no evidence of exacerbations) within 4 weeks prior to study entry.3 Patients could either have a current smoking burden of ≥10 pack-years, be former smokers with a history of ≥10 smoking pack-years or be non-smokers if they met the remaining inclusion criteria but had another documented risk factor for COPD, such as an environmental or professional exposure to air pollution, as determined by the physician. Patients must have been outpatients and were required to provide informed consent to participate. In addition, patients were required to have a minimum of 1 year’s follow-up from their pulmonary physician before enrollment in order to accurately assess exacerbation history over the previous 12 months.3,4 Patients were excluded from the POPE study if they had an unstable comorbid condition at the time of enrollment, were hospitalized <1 month prior to enrollment for any reason or if they were not able or willing to participate.3,4
Definitions of Phenotypes and Clusters
RETRO-POPE used the same clinically defined phenotypes that were used in the original POPE study;3,4,13 these were NON-AE (0 or 1 exacerbation per year), ACOS, and frequent exacerbators (≥2 exacerbations per year) with chronic bronchitis (AE CB) or without chronic bronchitis (AE NON-CB). Chronic bronchitis was defined as self-reported cough with sputum production that occurred every day and lasted for ≥3 months of the year over 2 consecutive years.3,4
Patients were also grouped according to the clustering methodology proposed by Burgel et al.12,14 Five Burgel clusters were defined based on age, cardiovascular comorbidities and/or diabetes, dyspnea (modified Medical Research Council [mMRC] score), BMI and lung function (FEV1): cluster 1, very severe comorbid; cluster 2, moderate-to-severe respiratory; cluster 3, moderate-to-severe comorbid/obese; cluster 4, very severe respiratory; and cluster 5, mild respiratory (Supplementary Figure 1).
Data Collection
For each patient originally included in the POPE study, baseline demographics, information on prescribed medications and survival data were collected up to January 2022 (Czech Republic) or July 2022 (Serbia) (approximately 7 years after initial inclusion in the study). In the Czech Republic, all patients were traced by the Institute of Health Information and Statistics of the Czech Republic via the National Health Information System, whereas in Serbia, data were collected from individual hospital departments (local data from outpatient clinics) and the national death register. This was also the case for analysis of cause of death, for which the Czech Republic sites used the International Classification of Diseases 10th Revision classification codes on the deceased examination sheet, and sites in Serbia used locally collected data, which were later categorized by cause of death.
Data from RETRO-POPE were entered into a database system (Trial DB, Yale Center for Medical Informatics, New Haven, CT, USA). Each patient’s identity was replaced with a number to prevent backward identification. The identity of each patient was only known to the attending physician or to an authorized healthcare professional.
Outcomes
Survival status was assessed retrospectively for subjects enrolled in the POPE study (2014–2015) from seven sites across the Czech Republic and Serbia. For patients who died, their causes of death were collected and grouped. Deaths under the term “respiratory diseases” included those related to COPD, COPD exacerbation, pneumonia, respiratory failure, respiratory arrest or if the primary cause of death included any other respiratory disease.
Associations between clinical phenotypes (POPE definitions) or Burgel clusters and mortality were carried out in the pooled overall cohort and by country. Long-term survival was compared between patients from the Czech Republic and Serbia (overall, by clinical phenotype and by Burgel cluster).
Statistical Analyses
Patients with incomplete follow-up data (missing survival status or date of death, if deceased), or insufficient data from the POPE study to allow for phenotype and/or cluster classification according to Burgel criteria were excluded from RETRO-POPE. Descriptive statistical methods were used for data analysis. Absolute and relative frequencies were used for the description of categorical parameters; differences between categorical parameters were tested by Fisher’s exact test. Continuous patient characteristics (for example, age) were described by mean (standard deviation [SD]); statistically significant differences between groups were assessed using Mann–Whitney or Kruskal–Wallis tests. A statistical level of P<0.05 was used to indicate significance. In cases of statistical significance, multiple comparisons were applied to identify homogeneous groups.
Analysis of long-term survival was conducted. Hazard ratios (HRs) were calculated from Cox models, and Kaplan–Meier estimates of survival function were used to illustrate patient survival times. The statistical significance of differences in survival time between groups was tested by log-rank test. Statistical tests were conducted using SPSS Statistics version 28 (IBM, Armonk, NY, USA) software.
Ethical Approval
The POPE study was approved by the multicenter Ethics Committee of the University Hospital Hradec Kralove (Charles University Prague, Czech Republic, reference number 201404 S12P, date of approval Apr 8, 2014) and conducted according to the ethical principles of the Declaration of Helsinki. RETRO-POPE was approved by the multicenter Ethics Committee of the University Hospital Hradec Kralove (Charles University Prague, Czech Republic, reference number 201605 I78ZP, date of approval May 10, 2016). As a retrospective analysis of POPE, informed patient consent was not required for RETRO-POPE (all patients in the original POPE study provided informed consent).3
Results
Patient Selection
A total of 1,003 patients from the Czech Republic and Serbia were eligible for inclusion, of whom 801 patients had complete information and were included in these analyses; 202 of the 1,003 were excluded as they had incomplete information. Of the included patients, 55.3% (n=443) were from the Czech Republic and 44.7% (n=358) were from Serbia (for numbers by site and patient disposition, see Supplementary Figures 2 and 3). The mean (SD) follow-up period was 68.1 (28.8) months for patients from the Czech Republic and 74.1 (28.0) months for patients from Serbia (Mann–Whitney test P<0.001).
Baseline Characteristics
Baseline characteristics by clinical phenotype and Burgel cluster are shown in Table 1 and Table 2, respectively. Clinical phenotyping showed that the majority of patients (63.5%) were NON-AE; 18.5% of patients were AE CB, 9.9% were AE NON-CB, and 8.1% had a diagnosis of ACOS at baseline. Burgel clustering showed that most patients (37.7%) were in cluster 2 (moderate-to-severe respiratory). Cluster 1 (very severe comorbid) and cluster 3 (moderate-to-severe comorbid/obese) were less prevalent, with 26.8% and 26.0% of patients, respectively. The lowest number of patients were in cluster 5 (mild respiratory) and cluster 4 (very severe respiratory), with 6.9% and 2.6% of patients, respectively.
 |
Table 1 Baseline Demographics by Patient Clinical Phenotype |
 |
Table 2 Baseline Demographics by Burgel Cluster |
A significant relationship was seen between phenotypes and Burgel clusters, with exacerbating patients most prevalent in Burgel clusters 1 and 2. For additional information on the relationships between phenotypes and clusters, see Supplementary Tables 1 and 2. When assessing the proportion of patients from the different clinical phenotypes who met the criteria for the different Burgel clusters, we identified differences between the groups. In three of the clinical phenotypes, Burgel cluster 2 was the most common (mMRC and FEV1 combination other than mMRC ≥3 and FEV1 ≤35% or mMRC ≤1 and FEV1 ≥60%), with AE CB having Burgel cluster 1 as the most common cluster (mMRC 3–4 and FEV1 <50%). The least common cluster in three of the clinical phenotypes was Burgel cluster 4 (mMRC ≥3 and FEV1 ≤35%), with AE CB having Burgel cluster 5 as the least common (mMRC ≤1 and FEV1 ≥60%).
Patients in the Czech Republic were older and had higher BMI, whereas patients in Serbia had worse lung function and higher mean smoking-pack years. Significant differences between patients in the Czech Republic versus Serbia were also observed for comorbidities and prescribed medications. The most commonly prescribed medication was triple combination therapy with long-acting muscarinic antagonist (LAMA) plus long-acting β2-agonist (LABA) plus inhaled corticosteroids in both the Czech Republic (30.2%) and in Serbia (47.8%). The pattern of medication use then differed between these two countries, with LABA monotherapy being the second-most common in the Czech Republic (20.1%) and LAMA monotherapy in Serbia (19.3%). For additional information on differences between the countries, see Supplementary Figure 4 and Supplementary Tables 3–9.
Survival
At the time of data collection, 440 patients were alive (54.9%) and 361 had died (45.1%).
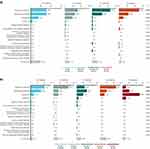
No significant differences in long-term overall survival were seen between the different phenotypes (log-rank test P=0.211; Figure 1a). Overall survival was highest in ACOS patients and lowest in frequent exacerbators; however, when using the ACOS phenotype as the reference group, there were no significant differences in HR compared with any of the other phenotypes.
 |
Figure 1 Overall cohort survival by (a) clinical phenotype and (b) Burgel clusters. Abbreviations: ACOS, asthma–COPD overlap syndrome; AE CB, frequent exacerbators with chronic bronchitis; AE NON-CB, frequent exacerbators without chronic bronchitis; NON-AE, non-exacerbators. Notes: Cluster 1, very severe comorbid; cluster 2, moderate-to-severe respiratory; cluster 3, moderate-to-severe comorbid/obese; cluster 4, very severe respiratory; cluster 5, mild respiratory (Supplementary Figure 1). |
In contrast to the analysis by clinical phenotype, a statistically significant association was identified between Burgel clusters and survival (log-rank test P<0.001; Figure 1b). Patients in cluster 5 (mild respiratory) had the highest survival rate, followed by patients in the moderate clusters (ie, cluster 2 [moderate-to-severe respiratory] and cluster 3 [moderate-to-severe comorbid/obese]). Patients in the severe clusters (ie, cluster 1 [very severe comorbid] and cluster 4 [very severe respiratory]) had the lowest survival rate. When using cluster 5 as the reference group, significant differences in HR were seen between clusters. For additional information on survival comparisons, see Supplementary Figure 5 and Supplementary Tables 10–12.
Considering the countries separately, patients in Serbia had longer survival than patients in the Czech Republic (HR 0.8, 95% confidence interval [CI] 0.6–1.0; P=0.036; Figure 2). After correcting for age, BMI, FEV1% predicted and Charlson Comorbidity Index, the survival difference was no longer significant (HR 0.88, 95% CI 0.70–1.10; P=0.257). In the Czech Republic, significant separation was seen in the survival plots for both clinical phenotypes (P=0.009) and Burgel clusters (P<0.001). In Serbia, survival was more independent of phenotype (P=0.479), but Burgel clusters showed significant separation (P<0.001). For additional information on countries, see Supplementary Figure 4 and Supplementary Tables 3–9.
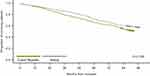 |
Figure 2 Survival by country. |
Cause of Death
Among the 361 patients who died, the most frequent cause of death was respiratory disease (36.8%), followed by cardiovascular causes (25.2%) and neoplasms (15.2%). For 41 patients (11.4%), the cause of death was unknown. For additional information on causes of death, see Supplementary Figure 6.
Analysis by clinical phenotype showed that respiratory diseases represented 30.8% of deaths in patients with ACOS, 31.7% of deaths in the NON-AE group, 45.2% in the AE NON-CB group and 50.0% of deaths in the AE CB group (P=0.023 between all groups). The proportion of deaths according to neoplasms was highest in the NON-AE group (19.0%) and lowest in the AE NON-CB group (2.4%), with a significant difference between the four clinical phenotypes (P=0.019). For all other causes of death, no significant difference was seen between clinical phenotypes. A full breakdown of the causes of death by clinical phenotype is shown in Figure 3a.
Analysis by Burgel cluster showed significant differences in the proportion of deaths caused by respiratory diseases (highest in cluster 4 [46.7%] and lowest in cluster 5 [10.0%]; P=0.004), cardiovascular disease (highest in cluster 1 [30.9%] and lowest in clusters 4 and 5 [20.0%]; P=0.040) and neoplasms (highest in cluster 5 [50.0%] and lowest in cluster 1 [10.3%]; P=0.019). For all other causes of death, no significant difference was seen between clusters. A full breakdown of the causes of death by Burgel cluster is shown in Figure 3b.
Discussion
RETRO-POPE was a post hoc analysis of all-cause mortality and cause of death in patients from the Czech Republic and Serbia who were originally enrolled in the real-world, observational POPE study. The key finding from RETRO-POPE was that grouping patients with COPD into Burgel clusters based on age, dyspnea, BMI, FEV1 and comorbidities (cardiovascular/diabetes) was more effective at predicting mortality than grouping by clinical phenotypes defined by exacerbation history and presence/absence of chronic bronchitis and/or asthmatic features.
In the clinical phenotyping analysis, patients with a frequent exacerbator phenotype (≥2 exacerbations in the previous year) had the lowest survival rate. This is consistent with previous real-world studies conducted in Spain and the Czech Republic, which had a similar duration of follow-up (4–6 years) and analyzed mortality using the same clinical phenotypes as used in RETRO-POPE.5–7 In our analysis, respiratory diseases accounted for a significantly higher proportion of deaths versus other causes in patients with an exacerbator phenotype. This is consistent with two Spanish real-world studies, in which COPD exacerbators with chronic bronchitis or emphysema had a higher risk of death.5,7 Golpe et al5 concluded that the observed mortality differences were less attributable to classification into phenotypes, and more to differences in COPD severity and comorbidity burden between groups. Similarly, worse lung function and comorbidity burden (specifically, chronic heart failure and cachexia) were also considered the major drivers of significantly higher mortality in patients with an exacerbation phenotype in a Czech real-world study.6 In contrast to the Spanish and Czech studies, our analysis showed no significant separation between clinical phenotypes in the survival plots in the overall cohort. Of note, when analyzed by country, the separation between clinical phenotypes in the survival plot was stronger in the Czech Republic than in Serbia, suggesting that the hypothesis that clinical phenotypes can predict survival may not be applicable to all country cohorts.
Unlike the phenotyping analysis by respiratory disease, the cluster analysis in the overall cohort showed significant separation between clusters in the survival plots, with similar results seen in both countries (though this was less clear in Serbia). In our analysis, patients in cluster 1 (very severe comorbid) and cluster 4 (very severe respiratory) had the lowest overall survival. This is consistent with cluster-based analysis studies from other countries, which have shown that patients with the highest comorbidity burden (cardiovascular, diabetes and other) have the lowest survival rates.8–10 When looking at the overall proportion of clinical phenotypes by Burgel cluster, our analysis showed that 44.6% of AE CB patients were in cluster 1 (54.9% in the Czech Republic and 39.2% in Serbia). This suggests that many bronchitic exacerbators had concomitant cardiovascular disease/diabetes, and were typically older, more dyspneic and had lower FEV1, which could have contributed to the higher mortality rate (43 out of 66 patients with this exacerbation phenotype [65.2%] died). Most deaths in the overall cohort were patients from Burgel cluster 1 (37.7%).
To assess whether lung function or dyspnea alone (excluding comorbidities) was effective in predicting mortality, we conducted further analyses comparing survival in patients with FEV1% predicted <50% versus ≥50% and an mMRC score of 0–2 versus 3–4. Patients with worse lung function (FEV1 <50%) and higher dyspnea (mMRC score 3–4) had significantly lower survival (P<0.001 for both; data not shown). However, analysis by Burgel cluster was significantly more effective in predicting mortality than analysis by either mMRC or FEV1 alone (P<0.001 for both), demonstrating the prognostic value of assessing BMI and comorbidities alongside lung function and dyspnea.
Few studies have compared methods for predicting mortality in COPD. Aramburu et al compared various methods of predicting mortality, and concluded that cluster analysis was significantly superior to the 2017 GOLD 1–4 spirometry classification system, with similar predictive ability to other systems such as the BODE index and the GOLD ABCD classification.10 However, to our knowledge, this retrospective analysis of the POPE study is the first to show that Burgel clustering may be a more sensitive tool for predicting mortality than clinical phenotyping by respiratory symptoms alone.
The observed difference in mortality between the two countries may partly be explained by differences in baseline characteristics. Compared with patients in Serbia, patients from the Czech Republic were significantly older and had a higher mean BMI, but they also had higher FEV1 and fewer smoking pack-years. In the unadjusted analysis, there was a significantly lower risk of mortality in Serbia versus the Czech Republic (HR 0.8, 95% CI 0.65–0.99; P=0.036); however, when corrected for age, BMI, FEV1% predicted and Charlson Comorbidity Index, this difference was no longer significant (HR 0.88, 95% CI 0.70–1.10; P=0.257).
One strength of RETRO-POPE is that it recruited patients with COPD irrespective of their smoking habits, including non-smokers with COPD, who are routinely excluded from clinical trials and are therefore of increasing interest.2,15–18 Air pollution in the CEE region has been reported to be higher than in Western Europe,19 which may contribute to the number of non-smokers with COPD in this region. Another strength of the study is that patients were recruited in a strictly consecutive manner, whereby each patient with COPD who contacted the participating institution at the time of project enrollment was asked for informed consent and, after signing it, was committed to the study. Additionally, the follow-up period in RETRO-POPE was longer than that of previous research in the CEE region (96 months vs 60 months),6 providing longer-term mortality data from this region.
Patients included in RETRO-POPE are representative of the COPD populations from both CEE countries. In the Czech Republic and Serbia, there is a different healthcare system for respiratory patients than in Western Europe. Most people with COPD are seen by pulmonologists and not general practitioners. General practitioners conduct initial visits, and patients are then referred to pulmonologists.19 There was a higher level of mortality data completeness in the Czech Republic, due to the government death registry, in which it is obligatory to capture the clinical causes of death. The completeness of data in Serbia varied as data had to be collected from individual hospital facilities.
One limitation of this study is the lack of standardization regarding the cause of death analysis. In some areas, the causes of death were based on the review of the clinical physician and did not always include a pathologic assessment. Grouping deaths under the term “respiratory diseases”, which encompasses a plethora of diseases, limits any specific conclusions related to the proportions of deaths attributed to a specific disease. Other potential limitations relate to the longitudinal nature of the analysis, as patients may have been grouped under a different clinical phenotype between the beginning of the trial and the end of the follow-up period (this information was not captured). The number of patients in each individual clinical phenotype group may also have been too low to identify a statistical difference. When assessing deaths by Burgel cluster and by phenotype, conclusions from the relative proportion of deaths observed in each group may be limited due to the small population size in some categories. Furthermore, there were methodologic differences between the two countries; for example, the follow-up period was slightly shorter in the Czech Republic than in Serbia due to the predefined data collection periods. This may partly explain some of the differences noted between the two countries.
The cohorts from the Czech Republic and Serbia had a large number of NON-AE patients (73% and 52%, respectively). This may not be true for all regions; for example, a study in Malaysia suggested that the proportion of NON-AE in Malaysia was only 29%,20 whereas a study in Spain found that the NON-AE phenotype was present in 52% of patients.21 However, it should be noted that in the RETRO-POPE analysis, patients who were included in the NON-AE clinical phenotype may have exacerbated during the follow-up period (this information was not captured). Finally, we excluded 202 patients of the 1,003 patients from the Czech Republic and Serbia due to incomplete data. As such, we do not know the clinical phenotypes/Burgel clusters for the excluded patients or whether these have an impact on the proportions of each Burgel cluster within each of the clinical phenotypes.
As COPD is a heterogeneous disease with both pulmonary and extrapulmonary features,22,23 phenotyping of patients can be problematic. Despite this heterogeneity, previous studies have suggested that by phenotyping or clustering patients, it is possible to identify groups with different prognoses.7–11 Dividing patients into clinical phenotypes or clusters seems to be the first step toward personalized medicine in the COPD field.24 However, the next decade will certainly bring a better understanding of cellular/molecular (endotypes) and genetic (genotypes) bases for new practical classification of patients.25 This analysis is the first “head-to-head” comparison of clinical phenotyping and Burgel clustering in an international multicenter study, which may prompt comparisons between other countries in the future. Findings from RETRO-POPE could help in identifying patients at a higher risk of mortality earlier, or more confidently, based on clinical and personal factors including age, BMI, level of dyspnea and comorbidities. In doing so, better personalization of patient care may be possible.
Conclusion
This 7-year longitudinal assessment of all-cause mortality in patients with COPD from two countries in the CEE region showed that clusters based on comorbidities, lung function and dyspnea were more likely to show significant differences in terms of mortality than clinical phenotypes according to exacerbation history and presence/absence of chronic bronchitis and/or asthmatic features.
Abbreviations
ACOS, asthma–COPD overlap syndrome; AE CB, frequent exacerbators with chronic bronchitis; AE NON-CB, frequent exacerbators without chronic bronchitis; BMI, body mass index; BODE, body mass index, obstruction, dyspnea and exercise; CEE, Central and Eastern Europe; CI, confidence interval; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; GOLD, Global Initiative for Chronic Obstructive Lung Disease; HR, hazard ratio; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; mMRC, modified Medical Research Council; NON-AE, non-exacerbators; POPE, Phenotypes of COPD in Central and Eastern Europe; RETRO-POPE, retrospective analysis of the POPE study; SD, standard deviation.
Data Sharing Statement
Data are available from the corresponding author upon request.
Acknowledgments
This publication was supported by a research fund from the Czech Pneumological and Phthisiological Society, Czech Republic. Data collection in the Czech Republic and analysis of all data was supported by an institutional research project of Charles University (Cooperatio Program, research area INDI).
Medical writing assistance, in the form of the preparation and revision of the manuscript, was supported financially by Boehringer Ingelheim International GmbH and provided by Paul Todd, PhD, at Meditech Media, under the authors’ conceptual direction and based on feedback from the authors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The RETRO-POPE post hoc analysis was supported by the Cooperatio Program of Charles University, Czechia - EU, research area INDI, and UHHK, 00179906 and Boehringer Ingelheim, RCV GmbH & Co KG.
Disclosure
VK reports non-financial support from Meditech Media, UK, Boehringer Ingelheim RCV Vienna, AUT, Charles University, Czechia, and Ministry of the Health, Czechia, during the conduct of the study. He gave presentations at symposia and sponsored and received fees for advisory board participation and travel grants from Angelini, AstraZeneca, Berlin-Chemie, Boehringer Ingelheim, Chiesi and Menarini. He received research grants from Angelini, AstraZeneca, Boehringer Ingelheim and Chiesi. BM has received honoraria for consulting and presenting from AstraZeneca, Berlin-Chemie, Boehringer Ingelheim and Novartis. BM also reports grants from Company Providens, Serbia, non-financial support for Advisory Board for COPD from AstraZeneca, Serbia and Boehringer Ingelheim, outside the submitted work; and President of Respiratory Society of Serbia and President of Republic Expert Commission for Pulmonology (by Ministry of Health Republic of Serbia). MS, JK, SH, VZ, MI, JJank and JJark have nothing to disclose. VC has received honoraria for consulting and presenting from AstraZeneca, Berlin-Chemie, Boehringer Ingelheim and Teva. BP is an employee of Boehringer Ingelheim Serbia d.o.o Beograd. AV has received speaker and/or consultancy fees, as well as research grants from AstraZeneca, Boehringer Ingelheim, Chiesi, GSK, Menarini and Novartis.
References
1. World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025, third edition; 2019. Available from: https://www.who.int/publications/i/item/who-global-report-on-trends-in-prevalence-of-tobacco-use-2000-2025-third-edition.
2. Yang IA, Jenkins CR, Salvi SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. 2022;10(5):497–511. doi:10.1016/S2213-2600(21)00506-3
3. Zbozinkova Z, Barczyk A, Tkacova R, et al. POPE study: rationale and methodology of a study to phenotype patients with COPD in Central and Eastern Europe. Int J Chron Obstruct Pulmon Dis. 2016;11:611–622. doi:10.2147/COPD.S88846
4. Koblizek V, Milenkovic B, Barczyk A, et al. Phenotypes of COPD patients with a smoking history in Central and Eastern Europe: the POPE study. Eur Respir J. 2017;49(5):1601446. doi:10.1183/13993003.01446-2016
5. Golpe R, Suárez-Valor M, Martín-Robles I, et al. Mortality in COPD patients according to clinical phenotypes. Int J Chron Obstruct Pulmon Dis. 2018;13:1433–1439. doi:10.2147/COPD.S159834
6. Brat K, Svoboda M, Zatloukal J, et al. The relation between clinical phenotypes, GOLD groups/stages and mortality in COPD patients–a prospective multicenter study. Int J Chron Obstruct Pulmon Dis. 2021;16:1171–1182. doi:10.2147/COPD.S297087
7. Hernández Vázquez J, Ali García I, Jiménez-García R, et al. COPD phenotypes: differences in survival. Int J Chron Obstruct Pulmon Dis. 2018;13:2245–2251. doi:10.2147/COPD.S166163
8. Rennard SI, Locantore N, Delafont B, et al. Identification of five chronic obstructive pulmonary disease subgroups with different prognoses in the ECLIPSE cohort using cluster analysis. Ann Am Thorac Soc. 2015;12(3):303–312. doi:10.1513/AnnalsATS.201403-125OC
9. Tiew PY, San Ko FW, Narayana JK, et al. “High-risk” clinical and inflammatory clusters in COPD of Chinese descent. Chest. 2020;158(1):145–156. doi:10.1016/j.chest.2020.01.043
10. Aramburu A, Arostegui I, Moraza J, et al. COPD classification models and mortality prediction capacity. Int J Chron Obstruct Pulmon Dis. 2019;14:605–613. doi:10.2147/COPD.S184695
11. Pikoula M, Quint JK, Nissen F, Hemingway H, Smeeth L, Denaxas S. Identifying clinically important COPD sub-types using data-driven approaches in primary care population based electronic health records. BMC Med Inform Decis Mak. 2019;19(1):86. doi:10.1186/s12911-019-0805-0
12. Burgel P-R, Paillasseur J-L, Janssens W, et al. A simple algorithm for the identification of clinical COPD phenotypes. Eur Respir J. 2017;50(5):1701034. doi:10.1183/13993003.01034-2017
13. Miravitlles M, Soler-Cataluna JJ, Calle M, Soriano JB. Treatment of COPD by clinical phenotypes: putting old evidence into clinical practice. Eur Respir J. 2013;41(6):1252–1256. doi:10.1183/09031936.00118912
14. Gagatek S, Wijnant SRA, Stallberg B, et al. Validation of clinical COPD phenotypes for prognosis of long-term mortality in Swedish and Dutch cohorts. COPD. 2022;19(1):330–338. doi:10.1080/15412555.2022.2039608
15. Kaur M, Chandel J, Malik J, Naura AS. Particulate matter in COPD pathogenesis: an overview. Inflam Res. 2022;71(7–8):797–815. doi:10.1007/s00011-022-01594-y
16. Lamprecht B, McBurnie MA, Vollmer WM, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011;139(4):752–763. doi:10.1378/chest.10-1253
17. Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9691):733–743. doi:10.1016/S0140-6736(09)61303-9
18. Agusti A, Vogelmeier C, Faner R. COPD 2020: changes and challenges. Am J Physiol Lung Cell Mol Physiol. 2020;319(5):L879–L883. doi:10.1152/ajplung.00429.2020
19. Valipour A, Aisanov Z, Avdeev S, et al. Recommendations for COPD management in Central and Eastern Europe. Expert Rev Respir Med. 2022;16(2):221–234.
20. Chai C-S, Liam C-K, Pang Y-K, et al. Clinical phenotypes of COPD and health-related quality of life: a cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2019;14:565–573. doi:10.2147/COPD.S196109
21. Miravitlles M, Roman-Rodriguez M, Ribera X, Ritz J, Izquierdo JL; Opti Investigator's Group. Inhaled corticosteroid use among COPD patients in primary care in Spain. Int J Chron Obstruct Pulmon Dis. 2022;17:245–258. doi:10.2147/COPD.S342220
22. Han MK, Agusti A, Calverley PM, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182(5):598–604. doi:10.1164/rccm.200912-1843CC
23. Lange P, Halpin DM, O’Donnell DE, MacNee W. Diagnosis, assessment, and phenotyping of COPD: beyond FEV1. Int J Chron Obstruct Pulmon Dis. 2016;11(Spec Iss):3–12. doi:10.2147/COPD.S85976
24. Dal Negro RW, Carone M, Cuttitta G, et al. Prevalence and clinical features of most frequent phenotypes in the Italian COPD population: the CLIMA Study. Multidiscip Respir Med. 2021;16(1):790. doi:10.4081/mrm.2021.790
25. Marques A, Souto-Miranda S, Machado A, et al. COPD profiles and treatable traits using minimal resources: identification, decision tree and stability over time. RespirRes. 2022;23(1):30.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.