Back to Journals » Cancer Management and Research » Volume 16
Resumption of Intravenous Anti-Cancer Therapy in Breast Cancer: A Real-World Experience During the SARS-CoV-2 Pandemic
Authors Yang F , Li C, Qiu Y, Chen X, Zheng K, Kang D, Zhang Y, Liu B, Yao Y, Xie L
Received 14 October 2023
Accepted for publication 15 December 2023
Published 3 January 2024 Volume 2024:16 Pages 1—9
DOI https://doi.org/10.2147/CMAR.S444783
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Fang Yang,1,* Cong Li,2,* Yuling Qiu,1 Xinjie Chen,3 Kelin Zheng,4 Donglin Kang,5 Yin Zhang,2 Baorui Liu,1 Yongzhong Yao,2 Li Xie1
1The Comprehensive Cancer Center of Drum Tower Hospital, Medical School of Nanjing University & Clinical Cancer Institute of Nanjing University, Nanjing, People’s Republic of China; 2Department of Breast Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, People’s Republic of China; 3The Comprehensive Cancer Center, China Pharmaceutical University Nanjing Drum Tower Hospital, Nanjing, People’s Republic of China; 4Department of the Comprehensive Cancer Center, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Nanjing, People’s Republic of China; 5Department of the Comprehensive Cancer Center, Nanjing Drum Tower Hospital Clinical College of Nanjing Medical University, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Xie, The Comprehensive Cancer Center of Drum Tower Hospital, Medical School of Nanjing University & Clinical Cancer Institute of Nanjing University, Nanjing, People’s Republic of China, Email [email protected] Yongzhong Yao, Department of Breast Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, People’s Republic of China, Tel/Fax +86-025-83106666, Email [email protected]
Purpose: The coronavirus disease-2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, has delayed medical consultations, especially for patients receiving intravenous anti-cancer therapy. We aim to investigate alterations in immune function among breast cancer patients who experience delayed intravenous therapy due to SARS-CoV-2 infection.
Patients and Methods: We performed an observational investigation of breast cancer patients in Nanjing Drum Tower Hospital from December 27, 2022, to January 20, 2023. Patients who recovered from SARS-CoV-2 infection were eligible for enrollment. Peripheral blood samples were taken prior to the restart of intravenous anti-cancer therapy to examine hematologic parameters.
Results: A total of 131 patients were included in the final analysis. Cough (74.0%), fever (62.6%), and expectoration (46.6%) were identified as the most presenting symptoms of SARS-CoV-2 infection in breast cancer. The average nucleic acid conversion time and delayed treatment time was 13.4 days and 13.9 days, respectively. The patients > 60 years old experienced prolonged nucleic acid conversion time (P = 0.017) and delayed treatment time (P = 0.028) compared to those <= 60 years old. Dysregulated lymphocyte subsets and cytokines were found post-SARS-CoV-2 infection. Treatment-related adverse events of grade 3 or 4 occurred in 7.6% after resuming intravenous anti-cancer therapy.
Conclusion: Our findings reveal that the SARS-CoV-2 infection led to imbalanced immune responses and postponed intravenous anti-cancer therapy in breast cancer. The safety report encourages timely resumption of intravenous anti-cancer therapy after adequately weighing the risks and benefits.
Keywords: COVID-19 pandemic, SARS-CoV-2 infection, breast cancer, immune responses, anti-cancer therapy
Introduction
The coronavirus disease-2019 (COVID-19) epidemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, has led to widespread global changes to patterns of health care and cancer treatment. Malignant tumors, as well as aggressive anti-cancer treatment, can affect multiple organs and weaken the immune system, leaving cancer patients more susceptible to acquiring SARS-CoV-2 infection and worse outcomes than patients without cancer.1 Initial studies suggested that COVID-19 was lethal for human. Many hospitals had been converted into health-care facilities for the treatment of patients with COVID-19, resulting in a reduction in the management of cancer patients. There was no robust guideline on whether to initiate or delay anti-cancer therapy, especially for patients with early-stage cancers.2 Numerous breast cancer patients suffered from a delay in terms of diagnosis and treatment at the start of the COVID-19 pandemic, from December 2019 to February 2020.3 Patients weighed the benefits of attending medical care versus the risks of potential exposure to the virus, resulting in over 40% treatment delays in breast cancer.4 The initial pandemic-related disruptions in breast cancer care were demonstrated to have a small long-term cumulative impact on breast cancer mortality.5 A recent study showed no association between chemotherapy or other anti-cancer therapies and mortality in COVID-19 patients with cancers.6 Multiple studies have demonstrated no obvious delay in breast cancer treatment initiation during the COVID-19 pandemic.7–10 These data suggest that it is crucial to timely resume anti-cancer therapy for post-COVID-19 breast cancer patients. However, evidence on the optimal time for cancer treatment resumption, as well as the safety of chemotherapy and/or targeted therapy in post-COVID-19 patients is scarce.
From December 2022 to January 2023, the number of patients infected with SARS-CoV-2 quickly increased due to the modification in the policy of lockdown in preventing the spread of COVID-19 in China. The COVID-19 epidemic has led to broad disruptions in breast cancer treatment. We characterized the clinical symptoms and course of SARS-CoV-2 infection in breast cancer patients and reported our experiences in successfully resuming intravenous anti-cancer therapy post-SARS-CoV-2 infection. This study also aims to analyze the immune status of post- SARS-CoV-2 breast cancer patients and seek risk factors associated with COVID-19 disease severity. We hope the results can promote a comprehensive understanding of safe resumption of intravenous anti-cancer therapy and inform the optimal allocation of health-care resources and services during and after the pandemic.
Materials and Methods
Study Population and Variables
Patients meeting the criteria were eligible for enrollment: i) pathologically diagnosed with breast cancer and had previously received intravenous chemotherapy and/or targeted therapy in Nanjing Drum Tower Hospital; ii) infected with COVID-19 and had recovered before restarting anti-cancer treatment between December 27, 2022, to January 20, 2023. Due to the modification in the policy of lockdown started in December 2022, the number of patients infected with COVID-19 increased sharply during that period. After that, the number of new cases of COVID-19 infection sharply decreased, and nucleic acid testing was no longer mandatory for admission. Patients were deemed to be infected with SARS-CoV-2 if a real-time reverse transcription polymerase chain reaction (rRT-PCR) assay or rapid antigen detection test from a throat or nose swab was positive for SARS-CoV-2. The rRT-PCR assay should be negative at least twice with an interval of more than 24 h before they resume intravenous chemotherapy and/or targeted therapy. Nucleic acid conversion time was defined as the days from the onset of infection to the negative detection of SARS-CoV-2 by rRT-PCR. The delayed time of treatment was defined as the time gap between the estimated and actual treatment time. The average nucleic acid conversion time and the average delayed time of treatment were calculated using the average values of all enrolled patients.
Demographics, clinical manifestations, comorbidities, and adverse events were collected on admission or after the resumption of treatment. We used the National Cancer Institute Common Toxicity Criteria (CTCAE version 4.0) to grade adverse events. Adverse events were categorized into mild-to-moderate severity (grade 1–2) and severe severity (grade 3–4). Peripheral blood samples were collected to test laboratory parameters before the resumption of treatment. Absolute counts of lymphocyte subsets were assessed, and the proportion of lymphocytes represented the percentage of one lymphocyte subset for all lymphocyte counts. The normal reference ranges were 59.4–84.6% (CD3+), 28.5–60.5% (CD3+CD4+), 11.1–38.3% (CD3+CD8+), 6.4–22.6% (B cell), 5.6–30.9% (NK cell), 0.9–3.6 (CD3+CD4+/CD3+CD8+). Apart from the patients’ need to evaluate the efficacy of anti-cancer therapy, chest computed tomography (CT) was also performed if the patient was over 60 years old, or presented with symptoms of viral pneumonia on admission. To analyze the impact of COVID-19 on the immune system, we compared the differences in lymphocyte subsets and cytokines between the patients with and without pneumonia. Written informed consent was obtained from all patients. Our study complied with the World Medical Association Declaration of Helsinki recommendations and was approved by the Medical Ethics Committee of Nanjing Drum Tower Hospital.
Statistical Analysis
Fisher’s exact tests were used to test the differences in categorical variables, and Mann–Whitney U-test and Kruskal–Wallis test were applied for quantitative variables. Statistical tests were conducted with significance set at P < 0.05 two-sided. All analyses were performed using SPSS, version.
Results
Baseline Clinical Characteristics
We identified a total of 131 patients with breast cancer who received intravenous anti-cancer therapy between December 27, 2022, to January 20, 2023 (Table 1). All the patients were female, with a median age of 54 years, range 32 to 77. Among them, 30.5% (40/131) received neoadjuvant therapy, 55.7% (73/131) received adjuvant therapy, and 13.7% (18/131) received systemic treatment for stage IV or recurrent metastatic disease; 33.6% (44/131) had comorbidities, hypertension (25.2%), diabetes (8.4%), and other cardiovascular diseases (6.1%) were the most frequent (Figure 1A).
 |
Table 1 The Association of Clinicopathologic Variables with SARS-CoV-2 Nucleic Acid Conversion Time and Delayed Treatment Time |
Clinical Manifestations of SARS-CoV-2 Infection
The most frequently experienced clinical symptomatology during the SARS-CoV-2 infection included cough (74.0%), fever (62.6%), expectoration (46.6%), fatigue (40.5%), and loss of smell and taste (34.4%) (Figure 1B). The average nucleic acid conversion time was 13.4 days, which was almost identical to the average delayed time of treatment 13.9 days (Table 1). Patients > 60 years old had significantly prolonged nucleic acid conversion time (P = 0.017) and prolonged delayed time of treatment (P = 0.028) than those <= 60 years old. Conversely, no significant differences were observed between the patients grouped by stage, cancer subtype, treatment strategy, comorbidities, and COVID-19 vaccination history (Table 1). A total of 32 patients performed chest CT scans, with 23 patients <= 60 years old and 9 patients > 60 years old. The risk of developing viral pneumonia was higher in patients > 60 years old than those <= 60 years old, but the difference was not significant (44.4% vs 13.0%, P = 0.076) (Table 2).
 |
Table 2 The Association of Age with Pneumonia Presented on Chest CT (n=32) |
Immune Responses After Recovery from SARS-CoV-2 Infection
We evaluated lymphocyte subsets and inflammatory factor levels before the resumption of intravenous anti-cancer therapy. In most patients, the proportions of CD3+/CD4+ T cells and B cells and CD3+CD4+/CD3+CD8+ ratio were decreased, while the percent of CD3+CD8+ T cells was increased (Figure 2). Elevated levels of cytokines, including IL4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-17, and IFN-γ were observed in most patients (Figure 2). The average number of elevated cytokines in patients with pneumonia was higher than that in patients without pneumonia, but there was no statistical difference (7 vs 5, P = 0.127) (Figure 2). Notably, compared to patients free of viral pneumonia, the percentage of B cells in those who developed pneumonia was significantly higher (P = 0.048) (Table 3). No significant differences in other lymphocyte subsets or inflammatory factors were observed between patients who developed viral pneumonia or not (Table 3).
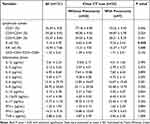 |
Table 3 Lymphocyte Subsets and Inflammatory Factors of Patients with SARS-CoV-2 Infection |
Safety of Resuming Intravenous Anti-Cancer Therapy
Adverse events after the resumption of anti-cancer therapy that were considered by the investigators to be related to treatment were reported in 53.4% of the patients. The most common select adverse events of any grade were anemia and leukocytopenia, which occurred in 28.2% and 14.5% of the patients, respectively (Table 4). The most common select adverse events of grade 3 were neutropenia and leukocytopenia, which occurred in 7.6% and 4.6% of the patients, respectively (Table 4). No treatment-related deaths occurred.
 |
Table 4 AEs After Resumption of Intravenous Anti-Cancer Therapy (n=131) |
Discussion
The COVID-19 pandemic has led to widespread global changes to patterns of patient management in multiple fields. Cancer patients have a highly susceptible immune system as a result of the cancer itself and its treatments (eg, chemotherapy, radiotherapy, and chemoradiotherapy) that they are undergoing. Individuals with cancer may be at higher risk for developing COVID-19 and have inferior outcomes compared with those without cancer.11,12 There has been a considerable reduction in breast cancer screening activities and identification of new breast cancer patients during the COVID-19 pandemic.13 Although the occasional postponed treatment may not lead to immediate disease progression, disruptions to health care would certainly be disadvantageous for short-term mortality.14 Although associations between pandemic-related lag times and cancer-related outcomes have been highlighted,15 there is still no consensus on how long lag time will lead to inferior outcomes. Reliable evidence for safe resumption of intravenous anti-cancer therapy in post-COVID-19 patients is strongly warranted. The number of SARS-CoV-2 infections in China continues to rise since the release of the lockdown policy in December 2022. We investigated the disease duration and immune responses of post-SARS-CoV-2 breast cancer patients and evaluated the safety of resuming anti-cancer therapies.
Our data show that the length of treatment delays is almost consistent with the SARS-CoV-2 nucleic acid conversion time, indicating a pandemic-related disruption in breast cancer treatment. The COVID-19 infection had a greater impact on older patients, with a significantly prolonged delayed time of treatment and increased likelihood of viral pneumonia. In our study, nearly half of the breast cancer patients over 60 years old infected with COVID-19 suffered from pneumonia (44.4%), even though all these patients eventually recovered. This is to be expected because older people were more likely to have comorbid conditions and weakened immune systems. Previous studies have demonstrated that older age and presence of comorbidities (eg, diabetes and hypertension) were the main risk factors for severe and long COVID-19.12,16,17 The results suggested more intensive surveillance for older patients admitted with COVID-19 who have breast cancer.
Immunotherapy has been demonstrated as a promising treatment for breast cancer patients.18 Multiple studies have shown a correlation between lymphocyte subsets and cytokines with severity of COVID-19.19,20 Patients with higher levels of lymphocyte, CD3+ T cells, CD4+ T cells, or CD8+ T cells were associated with shorter hospitalization time.19 In contrast, levels of IL-6 significantly correlated with longer length of stay, clinical severity, and mortality.20 In the current study, we demonstrated the decreased proportions of CD3+CD4+ T cells, B cells, as well as CD3+CD4+/CD3+CD8+ ratio, suggesting a suppressed T cell-mediated immunity post-SARS-CoV-2 infection. In contrast, the cytokines including IL-6, IL-8, IFN-γ, and so on, were broadly elevated in response to SARS-CoV-2 infection. However, most patients did not suffer serious adverse events after resumption of intravenous anti-cancer therapy, suggesting that the recovery of lymphocyte subsets and cytokines may lag behind the recovery of symptoms. The timing of resuming chemotherapy should be considered comprehensively based on laboratory indicators, clinical symptoms, and physical conditions. Although the study lacked data on pre-SARS-CoV-2 infection, we collected peripheral blood 2 months after recovery from SARS-CoV-2 infection, which should be considered closer to the baseline immune status pre-SARS-CoV-2 infection. It shows a sharp decrease in cytokines 2 months after recovery from SARS-CoV-2 infection (Figure S1). The results were consistent with the imbalanced host response to SARS-CoV-2, which was characterized by reduced innate antiviral defenses coupled with exuberant inflammatory cytokine production.21 There might be a parallel between COVID-19 and cytokine release syndrome (CRS), with uniquely elevated IL-6 and IL1RA.21 Recombinant human granulocyte colony-stimulating factor (G-CSF) is widely given to patients to counteract neutropenia, which is commonly encountered after chemotherapy in breast cancer. It was reported that in the setting of active COVID-19 infection, G-CSF led to an increased number of hospitalizations and the need for high levels of oxygen supplementation and death.22 The rapidly increasing neutrophils induced by G-CSF may cause extensive infiltration of myeloid cells into the lungs, leading to a cytokine storm. Therefore, the potential risks versus benefits should be adequately considered before G-CSF administration in neutropenic cancer patients with COVID-19.
The pandemic-related disruptions in breast cancer care were suggested to have a small long-term cumulative influence on breast cancer mortality estimated by collaborative simulation models.5 Information on the safety of resuming anti-cancer therapies is required to identify the at-risk population, as well as to avoid unnecessary delays in cancer management. It has been reported that a high percentage of COVID-19 patients still showed mild-to-substantial residual radiological lung abnormalities 3 months after discharge.23 In our study, no severe adverse events or death occurred after the resumption of intravenous anti-cancer therapy, even in those showing viral pneumonia by CT scan. However, it is essential to evaluate the risk for each patient before resuming the anti-cancer therapy. Patients with older age presented with comorbidities like hypertension, or treated with some molecular target drugs, might be at a higher risk of intensive care unit admission and/or death due to COVID-19 than people without these conditions.24,25 We propose the minimization of treatment delays and resumption of anti-cancer therapy after adequately informing patients of the risks and benefits. Novel health-care managements such as tele-consultations and day-care services should be considered to provide optimal treatment strategies.
This is the first study investigating immune responses and safety when resuming intravenous anti-cancer therapy post-SARS-CoV-2 in breast cancer, which could provide an important guide for clinicians. We will observe whether these patients suffering from COVID-19 display any difference in terms of recurrence and metastasis compared to patients not suffering from COVID-19 during follow-up.
There are several potential limitations of this study. First, this is a single-center retrospective study with limited samples. Analyses of confounding factors should be considered with a larger number of patients in the future. Second, the nucleic acid test was not conducted every day, so the nucleic acid conversion time could not represent the actual disease duration. Third, selection bias may exist given that analyses were based on patients attending medical care facilities. Fourth, this study lacked long-term dynamic monitoring of lymphocyte subsets and cytokines, especially before SARS-CoV-2 infection. Additionally, we did not assess the lymphocyte subsets and cytokines before the SARS-CoV-2 infection, so the altered lymphocyte subset proportions and cytokine levels could already be present before the influence of SARS-CoV-2 infection.
Conclusion
This study revealed a postponement on the resumption of intravenous anti-cancer therapy and imbalanced immune responses caused by SARS-CoV-2 infection in breast cancer. It is generally considered safe to resume anti-cancer therapy in patients who have recovered from COVID-19 without obvious symptoms. However, special caution should be exercised for elderly patients. It is important to note that the recovery of lymphocyte subsets and inflammatory factors may take longer than the resolution of symptoms. Therefore, resuming anti-cancer therapy should not be delayed based solely on abnormal indicators. It should be feasible to resume systematic treatment in low-risk cancer patients post-COVID-19. This might provide valuable insights into how to manage these patients during the pandemic.
Funding
This research was funded by National Natural Science Foundation of China (No. 82002783), Nanjing Outstanding Youth Fund (No. JQX21001).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang Q, Berger NA, Xu R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021;7(2):220–227. doi:10.1001/jamaoncol.2020.6178
2. Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer care in the time of COVID-19. Ann Intern Med. 2020;172(11):756–758. doi:10.7326/M20-1133
3. Li J, Wang H, Geng C, et al. Suboptimal declines and delays in early breast cancer treatment after COVID-19 quarantine restrictions in China: a national survey of 8397 patients in the first quarter of 2020. E Clinical Medicine. 2020;26:100503. doi:10.1016/j.eclinm.2020.100503
4. Papautsky EL, Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat. 2020;184(1):249–254. doi:10.1007/s10549-020-05828-7
5. Alagoz O, Lowry KP, Kurian AW, et al. Impact of the COVID-19 pandemic on breast cancer mortality in the US: estimates from collaborative simulation modeling. J Natl Cancer Inst. 2021;113(11):1484–1494. doi:10.1093/jnci/djab097
6. Lee LY, Cazier JB, Angelis V, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919–1926. doi:10.1016/S0140-6736(20)31173-9
7. Eijkelboom AH, de Munck L, Menke-van der Houven van Oordt CW, et al. Changes in breast cancer treatment during the COVID-19 pandemic: a Dutch population-based study. Breast Cancer Res Treat. 2023;197(1):161–175. doi:10.1007/s10549-022-06732-y
8. Cadili L, DeGirolamo K, McKevitt E, et al. COVID-19 and breast cancer at a regional breast centre: our flexible approach during the pandemic. Breast Cancer Res Treat. 2021;186(2):519–525. doi:10.1007/s10549-020-06008-3
9. Hawrot K, Shulman LN, Bleiweiss IJ, et al. Time to treatment initiation for breast cancer during the 2020 COVID-19 pandemic. JCO Oncol Pract. 2021;17(9):534–540. doi:10.1200/OP.20.00807
10. Vanni G, Tazzioli G, Pellicciaro M, et al. Delay in breast cancer treatments during the first COVID-19 Lockdown. A multicentric analysis of 432 patients. Anticancer Res. 2020;40(12):7119–7125. doi:10.21873/anticanres.14741
11. Lee KA, Ma W, Sikavi DR, et al. Cancer and risk of COVID-19 through a general community survey. Oncologist. 2021;26(1):e182–185. doi:10.1634/theoncologist.2020-0572
12. Tian J, Yuan X, Xiao J, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893–903. doi:10.1016/S1470-2045(20)30309-0
13. Prodhan A, Islam DZ, Khandker SS, et al. Breast cancer management in the era of covid-19; key issues, contemporary strategies, and future implications. Breast Cancer. 2023;15:51–89. doi:10.2147/BCTT.S390296
14. Di Cosimo S, Ljevar S, Trama A, et al. Direct and indirect effects of COVID-19 on short-term mortality of breast cancer patients. Breast. 2023;71:60–62. doi:10.1016/j.breast.2023.07.011
15. Tope P, Farah E, Ali R, El-Zein M, Miller WH, Franco EL. The impact of lag time to cancer diagnosis and treatment on clinical outcomes prior to the COVID-19 pandemic: a scoping review of systematic reviews and meta-analyses. Elife. 2023;2023:12.
16. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi:10.1001/jama.2020.6775
17. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi:10.1183/13993003.00547-2020
18. Hashemzadeh N, Dolatkhah M, Adibkia K, et al. Recent advances in breast cancer immunotherapy: the promising impact of nanomedicines. Life Sci. 2021;271:119110. doi:10.1016/j.lfs.2021.119110
19. Zhang P, Du W, Yang T, et al. Lymphocyte subsets as a predictor of severity and prognosis in COVID-19 patients. Int J Immunopathol Pharmacol. 2021;35:20587384211048567. doi:10.1177/20587384211048567
20. Mahmood SBZ, Majid H, Arshad A, et al. Interleukin-6 (IL-6) as a predictor of clinical outcomes in patients with COVID-19. Clin Lab. 2023;69(6). doi:10.7754/Clin.Lab.2022.220741
21. Blanco-Melo D, Nilsson-Payant BE, Liu WC, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181(5):1036–1045 e1039. doi:10.1016/j.cell.2020.04.026
22. Zhang AW, Morjaria S, Kaltsas A, et al. The effect of neutropenia and filgrastim (G-CSF) on cancer patients with coronavirus disease 2019 (COVID-19) Infection. Clin Infect Dis. 2022;74(4):567–574. doi:10.1093/cid/ciab534
23. Zhao YM, Shang YM, Song WB, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;25:100463. doi:10.1016/j.eclinm.2020.100463
24. Vuagnat P, Frelaut M, Ramtohul T, et al. COVID-19 in breast cancer patients: a cohort at the Institut Curie hospitals in the Paris area. Breast Cancer Res. 2020;22(1):55. doi:10.1186/s13058-020-01293-8
25. Infante MS, Salmanton-Garcia J, Fernandez-Cruz A, et al. B-cell malignancies treated with targeted drugs and SARS-CoV-2 infection: a European Hematology Association Survey (EPICOVIDEHA). Front Oncol. 2022;12:992137. doi:10.3389/fonc.2022.992137
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


