Back to Journals » Advances in Medical Education and Practice » Volume 14
Resilient Coping is More Important Than Previous Virtual Learning Experience: Predicting Pharmacy Student Stress During the COVID-19 Pandemic
Authors Campbell MH , Maharaj S , Khan K, Sa B , Adams OP , Majumder MAA
Received 11 January 2023
Accepted for publication 20 April 2023
Published 28 April 2023 Volume 2023:14 Pages 443—451
DOI https://doi.org/10.2147/AMEP.S402178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Michael H Campbell,1 Sandeep Maharaj,2 Katija Khan,2,3 Bidyadhar Sa,2 O Peter Adams,1 Md Anwarul Azim Majumder1
1The Faculty of Medical Sciences, The University of the West Indies, Bridgetown, Barbados; 2The Faculty of Medical Sciences, The University of the West Indies, St Augustine, Trinidad and Tobago; 3The Faculty of Social Sciences, The University of the West Indies, St Augustine, Trinidad and Tobago
Correspondence: Md Anwarul Azim Majumder, Faculty of Medical Sciences, The University of the West Indies, Cave Hill Campus, Bridgetown, Barbados, Tel +1 246 8228160, Email [email protected]
Purpose: The COVID-19 pandemic precipitated a swift transition to online learning in medical and health sciences. This study investigated the associations of previous experience with online learning, current confidence with online learning, and resilient coping skills with perceived stress reported by pharmacy students during the emergency transition to online learning.
Methods: Undergraduate pharmacy students (N=113, response rate = 41%) completed an online, self-report, cross-sectional survey during April-June 2020. Measures included Likert items measuring prior experience and current comfort levels with online learning, the Brief Resilient Coping Scale (BRCS), and the Perceived Stress Scale 10-Item Version (PSS-10). Experience, comfort with online learning, reported scores, and internal consistency for the BRCS and PSS-10 were summarized. A linear regression model examined the associations of prior experience with online education, gender, and resilient coping with perceived stress.
Results: Of the 113 respondents (78% female, mean age 22.3 years), > 50% had only occasional prior experience with online learning, coursework, and examinations, but 63% expressed confidence with online learning. Mean PSS-10 and BRCS scores were 23.8 and 13.3, respectively, and both scales demonstrated good internal consistency (α > 0.80). BRCS score was the single predictor of the PSS-10 score (r2 = 0.18, p < 0.001). Female gender was not a significant predictor (p = 0.11). A multiple regression model explained moderate variation in perceived stress (adjusted R2 = 0.19).
Conclusion: PSS-10 and BRCS scores indicated moderate levels of stress and coping skills among students during online teaching. Most students had some prior exposure to online learning, coursework, and examinations. Higher resiliency scores, but not prior online learning experience, predicted lower perceived stress.
Keywords: health professions, pharmacy education, online learning, pandemic, perceived stress scale, brief resilient coping scale, Caribbean
Introduction
Health and allied health education programmes transitioned to emergency online teaching modalities in the initial phases of the COVID-19 pandemic. Some programmes had prior experience with online platforms, while others were challenged to pivot quickly as tertiary institutions abruptly suspended in-person teaching.1 Although few studies have examined learning outcomes thus far, Stojan et al’s systematic review documented challenges and successes, especially in terms of student satisfaction.2 The trial-by-fire adoption of online learning may catalyze long-term incorporation of virtual pedagogy in health professions education. However, further studies examining the feasibility and generalizability of findings are needed.3,4
Studies concerning the mental health of medical students have proliferated during the COVID-19 pandemic. A recent review of 201 studies published between January 2020 and April 2022 found that more than half of medical students reported psychological distress, with alarmingly high rates of depression (41%), anxiety (38%), post-traumatic stress disorder (34%), and suicidal ideation (15%).5 Some studies have focused specifically on the implications of transitioning to online learning for psychological well-being, but prior findings have suggested that the transition to online learning during the pandemic has contributed to stress levels of medical and health professions students. These studies have noted an association between reported stress and the transition to online learning and/or assessment among medical students.6,7 Wang et al found that students’ approach to online learning and the online learning environment predicted perceived stress levels.8 Unreliable internet connection is also associated with stress.9 Several studies found that the female gender was associated with increased stress.6,10–12
Pharmacy training programmes also affected sweeping changes in curriculum globally at the start of the pandemic. Still, the experiences of student pharmacists have been less extensively covered than those of other health professions in published studies.13 Alghamdi et al found that Saudi pharmacy students had generally good access to technology and adequate skills to use technological tools.14 Students were accepting of online education but felt that they learned more in face-to-face interactions. Cernasev et al found that pharmacy students in a multisite US study adapted to online learning but reported significant mental health challenges (eg, isolation, stress, inadequate opportunity for rest, disrupted sleep, and frustration with online learning) and emphasized the need to foster student resilience.15 Nagy, Hall, and Charrois conducted a qualitative study of Canadian pharmacy students that highlighted similar themes of adaptation, stress, and mental health.16 A qualitative analysis of themes expressed by Australian pharmacy students during the initial stages of the pandemic similarly emphasized negative emotional states and communication barriers associated with online learning.17 A survey of Lebanese pharmacy students found that self-reported stress and anxiety persisted at levels >30% one year after the transition to online learning.18
Resilience is a complex phenomenon that generally refers to “positive adaptation, or the ability to maintain or regain mental health, despite experiencing adversity”.19 Operationally, resilient coping behavior is an “effective, problem-solving coping pattern” that reduces negative self-appraisal and impact of stress.20 The importance of resilience for the well-being of pharmacy students and practitioners is well established and reflected in the American Association of Colleges of Pharmacy Statement on Commitment to Clinician Well-being and Resilience.21 Findings from studies during the COVID-19 pandemic have provided further evidence of the importance of resilience for pharmacy students. In US studies, Fuentes et al22 found that effective use of coping skills, personal resilience, and Hispanic ethnicity predicted emotional well-being, and Hirsch et al23 found maladaptive coping was associated with higher perceived stress scores.
At the time of writing, no previously published study has addressed the experiences of Caribbean pharmacy students during the pandemic. Further, no studies have examined the influence of resilient coping and prior experience with online learning environments on perceived student stress during online learning. The current study 1) summarizes pharmacy students’ virtual learning experience prior to the pandemic and confidence with online learning at the time of the study; 2) compares gender differences across measures; and 3) examines the association of resilient coping and other predictors with student stress during the first three months after the transition to online learning.
Methods
Students enrolled in the undergraduate pharmacy program at a publicly supported Caribbean university were included in a regional cross-sectional online survey of students in medicine and health professions during the first stages of the COVID-19 pandemic, from April to June 2020. The study employed voluntary response sampling and invited all currently enrolled pharmacy students (N= 276) to participate. Survey data were collected from 113 students (response rate = 41%).
Measures
The following four measures comprised the self-report survey:
Perceived Stress Scale 10-Item Version: The PSS-10 measures the extent to which respondents appraise their life circumstances as stressful.24 More specifically, the instrument seeks to “tap how predictable, uncontrollable, and overloaded respondents find their lives”.19 The PSS-10 is a shortened version of the original 14-item scale and has established psychometric support in the Caribbean.25,26 Possible PSS scores range from 0 (low stress) to 40 (high stress).
Brief Resilient Coping Scale: The BRCS is a four-item unidimensional measure of tendency to cope with stress adaptively using flexible, active coping strategies.20 Resilience is associated with better stress outcomes across a range of psychological, behavioural, and physiological measures.27,28 Possible BRCS scores range from 4 (low resiliency) to 20 (high resiliency).
Experience with online learning: The survey instrument included 3 items in a 5-point Likert format using a frequency anchor (ranging from “never” to “very often”) to measure experience with online teaching, assignments, and exams.
Confidence with online learning: Students indicated their confidence using a single item, “I am confident with online learning and teaching” measured on a 4-point Likert scale using an agreement anchor ranging from “strongly disagree” to “strongly agree”.
Ethical Approval
The study protocol was approved by the following research ethics committees and complied with the Declaration of Helsinki: (i) the University of the West Indies-Cave Hill/Barbados Ministry of Health Research Ethics Committee/Institutional Review Board, Barbados (IRB No. 200403-B. April 27, 2020) and (ii) the Campus Research Ethics Committee, the University of the West Indies, St Augustine Campus, Trinidad and Tobago (IRB No. 200403-B. April 28, 2020). Participation in the survey was voluntary and anonymous, and participants gave informed consent before participating. Gender and year of study were included in the survey; however, no identifiable personal information was collected or stored.
Data Analysis
Descriptive statistics were calculated to describe the participants and to summarize their self-reported experience with online learning, assignments, and exams. Scores and internal consistency for standardized measures of stress and coping were reported, and gender differences were compared using independent samples t-tests. Finally, a simultaneous regression model was estimated to predict PSS-10 scores based on experience with online education, gender, and resilient coping. All analyses were conducted using SPSS v. 28.0.
Results
One hundred thirteen students (88 women and 25 men from all four years of pharmacy training participated in the survey). The mean age of participants was 22.3 (SD = 4.10). The distribution of participants by year of study is summarized with total enrollment figures for comparison in Table 1. First-year students (n = 68, 29.7%) were somewhat overrepresented in the voluntary sample. All students reported access to at least one electronic device (laptop, desktop, or smartphone). Two students had access only to a smartphone.
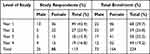 |
Table 1 Distribution of Pharmacy Students by Gender and Year of Study for Sample and Total Program Enrollment (2020) |
Experience and Confidence with Online Learning
Most students indicated that, prior to the start of the COVID-19 pandemic, they had previously used each of three elements of online instruction: teaching and learning, exams, and assignments. The distributions of experience levels varied considerably among students for all the aspects of online instruction (Figures 1–3). However, the majority of students reported “occasional” or more frequent experiences with each element of instruction. 43% of students reported engaging in online teaching and learning “often” or “very often” prior to the pandemic. Less than one-third had participated in online assignments of exams often or more frequently. Significant minorities indicated that they had “rarely” or “never” engaged in online teaching (22%, N=25), exams (30%, N=34), or assignments (32%, N=36) prior to the pandemic. Sixty-two percent of students (N=70) agreed or strongly agreed that they were confident with online teaching and learning; 37% (N=42) disagreed or strongly disagreed that they were confident. The distribution of responses is shown in Figure 4.
 |
Figure 1 Prior experience with online teaching and learning (n = 113). |
 |
Figure 2 Prior experience with online exams (n = 113). |
 |
Figure 3 Prior experience with online coursework (n = 113). |
 |
Figure 4 Confidence with online teaching and learning (n = 113). |
Perceived Stress
The PSS-10 demonstrated good internal consistency (α = 0.88). The mean PSS score was 23.2 (SD = 6.60; range: 5–40). The mean score for females was 23.8 (SD = 6.49); for males, the mean was 21.3 (SD 6.92). Gender differences approached but did not reach significance (t(108) = 1.64, p = 0.052).
Resilient Coping
The BRCS also demonstrated good internal consistency (α = 0.81). The mean BRCS score was 13.3 (SD = 11.20; range: 4–20). Mean scores were 13.2 and 13.7, respectively, for females and males. Gender differences in BRCS scores were not significant.
Modeling Perceived Stress
We conducted a multiple regression to evaluate the prediction of perceived stress from previous experience with online learning, gender, and resilient coping skills. After computing a dummy variable for gender, we estimated a simultaneous regression model for perceived stress. Regression results are summarized in Table 2. Examination of the P-P plot and scatterplot of residuals suggested that assumptions of normality were met. A Shapiro–Wilk test indicated that the distribution of standardized residuals did not differ significantly from a normal distribution (W = 0.99, p > 0.90). Multicollinearity was not a concern (for all predictors: tolerance values > 0.1 and VIF < 5). Overall, the model predicted a moderate amount of variation in perceived stress (adjusted R2 = 0.19, F(6,102) = 5.29, p < 0.001). BRCS scores were the single significant predictor of perceived stress (β = −0.83, p < 0.001).
 |
Table 2 Regression Results for Model of Perceived Stress Among Pharmacy Students |
Discussion
Considering the rapid transition to online learning at the beginning of the COVID-19 pandemic, this study described undergraduate pharmacy students’ prior experience with virtual learning and measured current perceived confidence, stress, and resilient coping skills. A model evaluating the contributions of gender, prior online learning experience, current confidence, and coping skills to perceived stress demonstrated that coping skills were the sole significant predictor of stress, accounting for just under one-fifth of the variation in self-reported scores. Although some studies have reported greater levels of perceived stress among females, gender differences were not significant in the current study.
The adverse circumstances of the COVID-19 pandemic have created academic and personal disruptions unprecedented in living memory. The resulting stressors have repositioned the importance of resilient coping from an emerging interest in academic pharmacy to a practical necessity for continued learning.29 The prominent association of resilient coping with reduced stress in student pharmacists is an instructive finding for efforts to develop interventions to bolster resilience and support the well-being of student pharmacists during the pandemic and beyond.30–32 Further, pharmacy programs can leverage the online modality to increase access to support services for students (eg, counseling, telehealth, social support networks).33 Although pharmacy programs have dedicated resources to support student well-being, research and program implementation remain somewhat fragmented.34 Support for resilience in pharmacy students is foundational for global efforts to promote resilience in pharmaceutical communities of practice.35
Pharmacists have advocated for promoting professional resilience in a framework comprising purpose, physical endurance, mental toughness, and emotional balance.36 In the context of COVID-19, pharmacy educators have framed efforts to promote wellbeing in terms of trauma-informed interventions to foster students’ sense of safety, trustworthiness and transparency, peer support, collaboration, empowerment of voice and choice, and cultural and gender diversity.30 These efforts to improve the well-being of professional pharmacists are likely to be more effective if integrated into training programs when students acquire foundations for professional behavior and practice. The American Association of Colleges of Pharmacy (AACP) has adopted an inclusive statement indicating that
AACP believes that all administrators, faculty, staff, preceptors, student pharmacists and alumni should contribute to a culture of wellness and resilience in pharmacy education; and
AACP encourages schools and colleges of pharmacy to proactively promote overall wellness and stress management techniques to students, faculty, and staff.21
Although promoting resilience is a widely shared aspirational goal, specific interventions and means of evaluating effectiveness vary widely among pharmacy programs.34 This reflects a lack of consensus on best practices to some degree, but differences also reflect the diversity of sociocultural and economic settings for pharmacy training and practice. Low- and middle-income countries (LMICs) may have particular challenges related to funding, human resources, and infrastructure that exacerbate stressors and reduce resources.37 These have the potential to contribute to the attrition of pharmacists and the degradation of health systems.38
The COVID-19 pandemic provided an unprecedented demonstration of the value of resilience, but risk factors for burnout and threats to the well-being of students and practicing pharmacists predate and will outlast the pandemic. Pharmacy educators have made significant progress in understanding the role of resilience in education and practice, and further research to identify the effectiveness of specific interventions is an important next step. Evidence-based programs are needed to promote resilience in pharmacy students and build foundations for healthy professional practice in diverse settings.
Limitations
Inferences from this study are limited by voluntary response sampling and nonresponse bias. Pandemic-related disruptions, especially during the chaotic first half of 2020, likely contributed to the low response rate, even after several follow-up email invitations on each campus. The overrepresentation of first-year students in the sample also limits generalizability. Challenges with sample size are not unique to this study; a similar study during the same time frame in the US achieved only a 26.2% response rate.39
Further, although the model is statistically significant, it explains only about one-fifth of the variation in perceived stress. More detailed knowledge of additional contributors to and contexts of stress and reliant coping during pharmacy education is needed. Despite these limitations, the findings provide an incremental contribution to understanding pharmacy student resilience during an unanticipated window of opportunity during the early phase of the COVID-19 pandemic in a Caribbean context. To our knowledge, this current study is the first effort to capture stress and coping among Caribbean pharmacy students during the pandemic.
Conclusions
Most pharmacy students had limited exposure to online learning, coursework, and exams prior to the start of the COVID-19 pandemic. Both the BRCS and PSS-10 demonstrated good internal consistency. In the three months after the introduction of online teaching due to the COVID-19 pandemic, students reported moderate levels of stress and resilient coping. Higher scores on resilient coping significantly predicted lower perceived stress, but prior experience with virtual learning and gender did not. Given the sampling limitations in the study, further research is needed to establish the replicability of our findings regarding the role of resilient coping. Research is also needed to support the use of specific interventions to foster resilience in diverse educational settings. The current study highlights the importance of resilience for the well-being of student pharmacists during the COVID-19 pandemic and in the future.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors would like to thank the students who completed the questionnaire. A previous version of this paper was presented at the 66th Annual Caribbean Public Health Agency Research Conference in Kingston, Jamaica.15–17th September 2022 (https://www.healthycaribbean.org/events/carpha-66th-annual-health-research-conference/).
Funding
This research received no external funding.
Disclosure
Dr Md Anwarul Azim Majumder is the Editor-in-Chief of Advances in Medical Education and Practice (DovePress). The other authors report no conflicts of interest in this work.
References
1. Stoehr F, Müller L, Brady A, et al. How COVID-19 kick-started online learning in medical education-the DigiMed study. PLoS One. 2021;16(9):e0257394. doi:10.1371/journal.pone.0257394
2. Stojan J, Haas M, Thammasitboon S, et al. Online learning developments in undergraduate medical education in response to the COVID-19 pandemic: a BEME systematic review: BEME Guide No. 69. Med Teach. 2022;44(2):109–129. doi:10.1080/0142159x.2021.1992373
3. Bastos RA, Carvalho D, Brandão CFS, Bergamasco EC, Sandars J, Cecilio-Fernandes D. Solutions, enablers and barriers to online learning in clinical medical education during the first year of the COVID-19 pandemic: a rapid review. Med Teach. 2022;44(2):187–195. doi:10.1080/0142159x.2021.1973979
4. Grafton-Clarke C, Uraiby H, Gordon M, et al. Pivot to online learning for adapting or continuing workplace-based clinical learning in medical education following the COVID-19 pandemic: a BEME systematic review: BEME Guide No. 70. Med Teach. 2022;44(3):227–243. doi:10.1080/0142159x.2021.1992372
5. Peng P, Hao Y, Liu Y, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2023;321:167–181. doi:10.1016/j.jad.2022.10.040
6. O’Byrne L, Gavin B, Adamis D, Lim YX, McNicholas F. Levels of stress in medical students due to COVID-19. J Med Ethics. 2021;47:383–388. doi:10.1136/medethics-2020-107155
7. Pokryszko-Dragan A, Marschollek K, Nowakowska-Kotas M, Aitken G. What can we learn from the online learning experiences of medical students in Poland during the SARS-CoV-2 pandemic? BMC Med Educ. 2021;21(1):450. doi:10.1186/s12909-021-02884-5
8. Wang J, Liu W, Zhang Y, Xie S, Yang B. Perceived stress among Chinese medical students engaging in online learning in light of COVID-19. Psychol Res Behav Manag. 2021;14:549–562. doi:10.2147/prbm.s308497
9. Nikas IP, Lamnisos D, Meletiou-Mavrotheris M, et al. Shift to emergency remote preclinical medical education amidst the Covid-19 pandemic: a single-institution study. Anat Sci Educ. 2022;15(1):27–41. doi:10.1002/ase.2159
10. Abdulghani HM, Sattar K, Ahmad T, Akram A. Association of COVID-19 pandemic with undergraduate medical students’ perceived stress and coping. Psychol Res Behav Manag. 2020;13:871–881. doi:10.2147/prbm.s276938
11. Huang L, Lei W, Xu F, Liu H, Yu L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: a comparative study. PLoS One. 2020;15(8):e0237303. doi:10.1371/journal.pone.0237303
12. Guldager JD, Jervelund S, Berg-Beckhoff G. Academic stress in Danish medical and health science students during the COVID-19 lockdown. Dan Med J. 2021;68(7):154.
13. Alzubaidi H, Jirjees FJ, Franson KL, et al. A global assessment of distance pharmacy education amid COVID-19: teaching, assessment and experiential training. Int J Pharm Pract. 2021;29(6):633–641. doi:10.1093/ijpp/riab064
14. Alghamdi S, Ali M. Pharmacy students’ perceptions and attitudes towards online education during COVID-19 lockdown in Saudi Arabia. Pharmacy (Basel). 2021;9(4). doi:10.3390/pharmacy9040169
15. Cernasev A, Desai M, Jonkman LJ, et al. Student pharmacists during the pandemic: development of a COVID-19 knowledge, attitudes, and practices (COVKAP) survey. Pharmacy (Basel). 2021;9(4). doi:10.3390/pharmacy9040159
16. Nagy DK, Hall JJ, Charrois TL. The impact of the COVID-19 pandemic on pharmacy students’ personal and professional learning. Curr Pharm Teach Learn. 2021;13(10):1312–1318. doi:10.1016/j.cptl.2021.07.014
17. Liu L, Caliph S, Simpson C, et al. Pharmacy student challenges and strategies towards initial COVID-19 curriculum changes. Healthcare (Basel). 2021;9(10). doi:10.3390/healthcare9101322
18. Hammoudi Halat D, Younes S, Safwan J, Akiki Z, Akel M, Rahal M. Pharmacy students’ mental health and resilience in COVID-19: an assessment after one year of online education. Eur J Investig Health Psychol Educ. 2022;12(8):1082–1107. doi:10.3390/ejihpe12080077
19. Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry. 2011;56(5):258–265. doi:10.1177/070674371105600504
20. Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. 2004;11(1):94–101. doi:10.1177/1073191103258144
21. American Association of Colleges of Pharmacy. Commitment to clinician well-being and resilience. American Association of Colleges of Pharmacy; 2022. Available from: https://www.aacp.org/article/commitment-clinician-well-being-and-resilience.
22. Fuentes AV, Jacobs RJ, Ip E, Owens RE, Caballero J. Coping, resilience, and emotional well-being in pharmacy students during the COVID-19 pandemic. Ment Health Clin. 2021;11(5):274–278. doi:10.9740/mhc.2021.09.274
23. Hirsch JD, Nemlekar P, Phuong P, et al. Patterns of stress, coping and health-related quality of life in doctor of pharmacy students. Am J Pharm Educ. 2020;84(3):7547. doi:10.5688/ajpe7547
24. Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage; 1988.
25. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi:10.2307/2136404
26. Campbell M, Gromer-Thomas J, Maynard D-M, Emmanuel M. Measuring stress in Caribbean university students: validation of the PSS-10 in Barbados. Caribbean J Psychol. 2019;10:65–88.
27. García-León M, Pérez-Mármol JM, Gonzalez-Pérez R, García-Ríos MDC, Peralta-Ramírez MI. Relationship between resilience and stress: perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiol Behav. 2019;202:87–93. doi:10.1016/j.physbeh.2019.02.001
28. Donohoe J, O’Rourke M, Hammond S, Stoyanov S, O’Tuathaigh C. Strategies for enhancing resilience in medical students: a group concept mapping analysis. Acad Psychiatry. 2020;44(4):427–431. doi:10.1007/s40596-020-01208-x
29. Stoffel JM, Cain J. Review of grit and resilience literature within health professions education. Am J Pharm Educ. 2018;82(2):6150. doi:10.5688/ajpe6150
30. Schlesselman LS, Cain J, DiVall M. Improving and restoring the well-being and resilience of pharmacy students during a pandemic. Am J Pharm Educ. 2020;84(6):ajpe8144. doi:10.5688/ajpe8144
31. Bird A, Tomescu O, Oyola S, Houpy J, Anderson I, Pincavage A. A curriculum to teach resilience skills to medical students during clinical training. MedEdPORTAL. 2020;16:10975. doi:10.15766/mep_2374-8265.10975
32. Cassidy S, Mawdsley A, Langran C, Hughes L, Willis SC. A large-scale multicentre study of academic resilience and wellbeing in pharmacy education. Am J Pharm Educ. 2022;8998. doi:10.5688/ajpe8998
33. Nobleza D, Hagenbaugh J, Blue S, Stepchin A, Vergare M, Pohl CA. The use of telehealth by medical and other health professional students at a college counseling center. J College Stud Psychother. 2019;33:275–289. doi:10.1080/87568225.2018.1491362
34. Arif SA, Moran K, Quiñones-Boex A, El-Ibiary SY. Student stress management and wellness programs among colleges of pharmacy. Innov Pharm. 2021;12(2):14. doi:10.24926/iip.v12i2.3478
35. Whitfield K, Arya V, Austin Z, et al. Developing a global community of practice for pharmacy workforce resilience-meet GRiT. Pharmacy (Basel). 2021;9(2). doi:10.3390/pharmacy9020110
36. Whitfield KM, Wilby KJ. Developing grit, motivation, and resilience: to give up on giving in. Pharmacy (Basel). 2021;9(2). doi:10.3390/pharmacy9020109
37. Shrestha R, Shrestha S, Sapkota B, Khanal S, Kc B. Challenges faced by hospital pharmacists in low-income countries before COVID-19 vaccine roll-out: handling approaches and implications for future pandemic roles. Turk J Pharm Sci. 2022;19(2):232–238. doi:10.4274/tjps.galenos.2021.37974
38. Alameddine M, Bou-Karroum K, Hijazi MA. A national study on the resilience of community pharmacists in Lebanon: a cross-sectional survey. J Pharma Policy Pract. 2022;15(1):8. doi:10.1186/s40545-022-00406-2
39. Attarabeen OF, Gresham-Dolby C, Broedel-Zaugg K. Pharmacy student stress with transition to online education during the COVID-19 pandemic. Curr Pharm Teach Learn. 2021;13(8):928–934. doi:10.1016/j.cptl.2021.06.011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
