Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
Relationship Between Systemic Immune-Inflammation Index and Risk of Respiratory Failure and Death in COPD: A Retrospective Cohort Study Based on the MIMIC-IV Database
Authors Zhang Y , Tan X, Hu S, Cui Z, Chen W
Received 7 November 2023
Accepted for publication 26 January 2024
Published 19 February 2024 Volume 2024:19 Pages 459—473
DOI https://doi.org/10.2147/COPD.S446364
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jill Ohar
Ye Zhang,1 Xiaoli Tan,2 Shiyu Hu,3 Zhifang Cui,4 Wenyu Chen2
1Department of General Medicine, Affiliated Hospital of Jiaxing University, Jiaxing, Zhejiang, People’s Republic of China; 2Department of Respiratory Medicine, Affiliated Hospital of Jiaxing University, Jiaxing, Zhejiang, People’s Republic of China; 3Jiaxing University Master Degree Cultivation Base, Zhejiang Chinese Medical University, Jiaxing, Zhejiang, People’s Republic of China; 4Department of Respiratory Medicine, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, People’s Republic of China
Correspondence: Wenyu Chen, Department of Respiratory Medicine, Affiliated Hospital of Jiaxing University, No. 1882, Zhonghuan South Road, Nanhu District, Jiaxing City, Zhejiang Province, 314001, People’s Republic of China, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) concurrent with respiratory failure (RF) is devastating, and may result in death and disability. Systemic immune-inflammation index (SII) is a new prognostic biomarker linked to unfavorable outcomes of acute coronary syndrome, ischemic stroke, and heart failure. Nonetheless, its role in COPD is rarely investigated. Consequently, this study intends to assess the accuracy of SII in predicting the prognosis of COPD.
Patients and Methods: The clinical information was retrospectively acquired from the Medical Information Mart for Intensive Care-IV database. The outcomes encompassed the incidence of RF and mortality. The relationship between different SII and outcomes was examined utilizing the Cox proportional-hazards model and restricted cubic splines. Kaplan-Meier analysis was employed for all-cause mortality.
Results: The present study incorporated 1653 patients. During hospitalization, 697 patients (42.2%) developed RF, and 169 patients (10.2%) died. And 637 patients (38.5%) died during long-term follow-up. Higher SII increased the risk of RF (RF: HR: 1.19, 95% CI 1.12– 1.28, P< 0.001), in-hospital mortality (HR: 1.22, 95% CI 1.07– 1.39, P=0.003), and long-term follow-up mortality (HR: 1.12, 95% CI 1.05– 1.19, P< 0.001). Kaplan-Meier analysis suggested a significantly elevated risk of all-cause death (log-rank P< 0.001) in patients with higher SII, especially during the short-term follow-up period of 21 days.
Conclusion: SII is closely linked to an elevated risk of RF and death in COPD patients. It appears to be a potential predictor of the prognosis of COPD patients, which is helpful for the risk stratification of this population. However, more prospective studies are warranted to consolidate our conclusion.
Keywords: systemic immune-inflammation index, chronic obstructive pulmonary disease, respiratory failure, mortality, MIMIC-IV database
Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent long-lasting airway inflammatory condition that features enduring respiratory symptoms and irreversible airflow restriction.1,2 Globally, COPD ranks third in terms of cause of death behind ischemic heart disease and cerebrovascular disease, owing to high morbidity and mortality rates.3,4 Respiratory failure (RF), especially hypercapnic RF (HRF), frequently occurs in most COPD patients at severe or end-stage.5,6 COPD complicated by RF (COPD+RF) increases the difficulty of treatment, resulting in poor prognosis.7 COPD+RF patients usually require unplanned hospitalization or intensive care unit (ICU). The short-term mortality reaches nearly 30%,8–10 and the mortality of critically ill patients who need mechanical ventilation is as high as 50%.11,12 This undoubtedly has a huge negative influence on patients’ health, economy, and quality of life. Therefore, early identification of the risk of RF in COPD patients is of significant importance. Exploring an easily accessible biomarker related to the incidence of RF to predict the clinical outcome can assist clinicians in determining high-risk patients early and implementing preventative strategies.
Despite the elusive pathogenesis of RF in COPD, aberrant immune activation and systemic inflammation constitute key contributors.13,14 The systemic immune-inflammation index (SII) is a comprehensive inflammatory indicator that is computed by peripheral lymphocyte, neutrophil, and platelet counts. Neutrophils, platelets, and produced cytokines are mostly tied to nonspecific immune responses.14–17 In contrast, lymphocytes are primarily linked to immune-related pathways.14–17 SII is more stable and can more accurately reflect the inflammation state of the human body than the absolute count of a single immune cell.18,19 In addition, due to low costs and easy accessibility, it is regarded as a powerful inflammatory indicator of both local immune response and systemic inflammation.20,21 In recent years, SII has been demonstrated to be indicative of poor prognosis of cardiovascular diseases,22,23 stroke,24,25 acute kidney injury26 and sepsis.27 However, no study, particularly with large sample sizes, has been done to discern how SII influences the prognosis of critically ill COPD patients.
Therefore, the current study intends to probe into the relationship between SII and the risk of RF and death in critically ill patients with COPD and to assess the prognostic value of SII in this population, providing guidance for the prevention and treatment of COPD+RF.
Materials and Methods
Data Sources
Relevant data were retrospectively acquired from the Medical Information Mart for Intensive Care-IV (MIMIC-IV version 2.2) database (https://physionet.org/content/mimiciv/2.2/). MIMIC-IV is a sizable and openly accessible database established and operated by the Massachusetts Institute of Technology (MIT). It includes the clinical data of 299,712 patients hospitalized in the Beth Israel Deaconess Medical Center (BIDMC) from 2008 to 2019. We have completed the courses required to use this database and obtained access to the database (authentication No.: 52663507). All the protected private information of patients has been de-identified. Ethical approval for this study was obtained from the Medical Research Ethics Committee of The First Hospital of Jiaxing (No. 2023-LY-633).
Study Population
Data on all patients were obtained from the MIMIC-IV database. The following patients were incorporated into our analysis: (1) Patients who were diagnosed with COPD according to the ninth and tenth revisions of the International Classification of Diseases (ICD-9 codes: 491.20, 491.21, 491.22 and 496; ICD-10 codes: J 44, J 44.0, J 44.1 and J 44.9); (2) patients who aged 18 and above. The following patients were excluded: (1) Patients who were hospitalized for less than 24 hours; (2) patients who had RF at admission; (3) patients whose platelet, neutrophil, and lymphocyte counts were missing or zero.
Data Extraction and Integration
PostgreSQL tool (version 14.6, https://www.postgresql.org/) was leveraged to extract patient data at their first admission from the MIMIC-IV database, encompassing demographic data (age, gender, race, BMI), vital signs (heart rate, blood pressure, respiratory rate, etc.), complications (hypertension, diabetes, atrial fibrillation, asthma, cancer, etc.), laboratory tests (blood routine, biochemical indicators, blood gas analysis, etc.), disease severity score [sequential organ failure assessment (SOFA), acute physiology score III (APSIII), simplified acute physiology score II (SAPSII), etc.], and treatment measures (glucocorticoid, bronchodilator, antibiotics, mechanical ventilation, etc.).
SII was computed utilizing the formula: SII = platelet count × neutrophil count/lymphocyte count.20 We extracted data on patients at their first admission. For indicators that were measured multiple times, we only used the results at the first measurement. For vital signs, laboratory tests, treatment measures, and other data, we only analyzed the data before patients developed RF.
Primary Outcome and Secondary Outcomes
The primary outcome was the incidence of RF. According to the Guidelines for Chronic Obstructive Pulmonary Disease,28 RF was defined as arterial oxygen partial pressure (PaO2) < 60 mmHg or PaO2/fractions of inspired oxygen (FiO2) ≤ 300 mmHg, with or without carbon dioxide (CO2) retention. Among them, carbon dioxide retention (PaCO2>50mmHg) means HRF.
Secondary outcomes consisted of in-hospital all-cause mortality and mortality during long-term follow-up. In-hospital mortality encompassed ICU death and general ward inpatient death. The information on the mortality of discharged patients was derived from the United States Social Security Death Index.
Missing Data
The variables that had more than 20% missing values were categorized based on the database’s reference range and converted into dummy variables for analysis. For variables with less than 20% missing values, the random-forest multiple imputation method was utilized to estimate the missing values.29
Statistical Analysis
According to the quartile of SII index, all patients were randomized into four groups. Normally distributed continuous variables were reported using mean ± standard deviation (SD), while abnormally distributed continuous variables were displayed as median and interquartile range [M (Q1, Q3)]. Categorical variables were reported as number and percentage (%). Comparisons of continuous variables were conducted utilizing the t-test or non-parametric test, and Pearson’s chi-square test or Fisher’s exact test was leveraged for categorical variable comparisons. To guarantee the comparability of baseline features across groups, covariates were adjusted utilizing Propensity score matching (PSM). The baseline traits of the original queue and the matching queue were displayed, separately.
The relationship between SII and the risk of outcomes was discerned employing the Cox proportional-hazards models, with hazard ratio (HR) with 95% confidence interval (CI) as the effect size. Three multivariate models were established based on the quartile of SII. No variables were adjusted in Model 1. Age and gender were adjusted in Model 2. On the basis of model 2, Model 3 was further adjusted for other 24 variables, encompassing asthma, acute myocardial infarction (AMI), atrial fibrillation (AF), cerebrovascular disease, chronic kidney disease (CKD), hypertension, heart failure(HF), liver disease, pneumonia, sepsis, acute exacerbations of chronic obstructive pulmonary disease (AECOPD), smoke, bronchodilator, glucocorticoid, mechanical ventilation, albumin, red cell distribution width (RDW), triglycerides, c-reactive protein, tidal volume, vital capacity, APSIII, SOFA and hemoglobin. Restricted cubic splines (RCS) model was adopted to delve into the nonlinear relationship between SII and the risk of RF and death in COPD patients. The Kaplan-Meier survival curve was leveraged to examine the relationship between different SII indexes and mortality, and the differences between groups were evaluated by Log rank test. Because of the non-normal distribution of SII, SII was converted into a logarithmic scale to minimize the skewness of the basic distribution.
Subgroup analysis was carried out to determine whether the relationship between SII and primary outcome indicators was consistent in different subgroups, and that SII was stable as a prognostic marker, such as age (≤65 years old and > 65 years old), gender, body mass index (BMI) (≤30 and > 30 kg/m2), and presence of hypertension, diabetes, coronary heart disease, cancer, dyslipidemia, heart failure, ischemic heart disease, liver disease, AECOPD, smoke, pneumonia and sepsis. Statistical analysis was executed utilizing the R software (version 4.2.3; R foundation for statistical computing, Vienna). P < 0.05 indicates a statistical difference.
Results
14,050 individuals with COPD were retrospectively extracted from the MIMIC-IV 2.2 database. Finally, 1653 COPD patients were analyzed in our study (Figure 1), encompassing 879 (53.2%) males and 774 (46.8%) females, and most of them were white people. The average age was 71.00 years (range 62.00–78.00 years). The average SII was 1302.17 (range 634.51–2821.88). RF occurred in 697 patients (42.2%), and HRF occurred in 427 patients (25.8%). Additionally, 169 patients (10.2%) died in hospital, with 39 deaths (2.3%) during hospitalization and 130 cases (7.9%) in ICU. During the follow-up, 637 patients (38.5%) died. The median follow-up time for RF, in-hospital death and follow-up death were 5.00 [1.00, 9.00], 8.00 [5.00, 15.00] and 29.00 [8.00, 187.00] days, respectively.
 |
Figure 1 Flow chart of patient screening. Abbreviations: MIMIC-IV, Medical Information Mart for Intensive Care-IV; n, Number; COPD, chronic obstructive pulmonary disease. |
Baseline Characteristics
The baseline features of SII groups are delineated in Table 1. Patients in the high SII group were mostly old, white, and males, with more unstable vital signs and higher disease scores at admission compared to the low SII group. Individuals with higher SII had a higher incidence of developing cancers, heart failure, AECOPD, pneumonia, and sepsis, but they were less likely to suffer from liver diseases and dyslipidemia. Their white blood cells, neutrophils, platelets, RDW, serum phosphorus, serum urea nitrogen, partial pressure of carbon dioxide and serum glucose levels were also higher, while the levels of red blood cells, hemoglobin, lymphocyte count, albumin, PH, PaO2, sodium ion, and chloride were lower. In addition, patients with high SII were also most likely to use glucocorticoids, antibiotics, vasopressors, oxygen, and invasive ventilation.
 |
Table 1 The Baseline Clinical Characteristics of the Study Population |
With the rise in SII index, ICU stay (1.05 days vs 1.36 days vs 1.68 days vs 2.45 days, P <0.001), hospitalization time (7.00 days vs 8.00 days vs 9.00 days vs 9.00 days, P <0.001), RF rate (28.3% vs 38.7% vs 42.6% vs 59.1% P<0.001), the incidence of HRF (16.4% vs 23.5% vs 27.1% vs 36.3%, P<0.001), ICU mortality (4.6% vs 6.3% vs 8.0% vs 12.6%, P<0.001), and in-hospital mortality (6.0% vs 7.3% vs 11.6% vs 16.0%, P<0.001) and long-term follow-up mortality (33.1% vs 33.2% vs 39.2% vs 48.7%, P<0.001) were elevated progressively. PSM analysis was performed with median SII as the cutoff value, and it was observed that the baseline features of the two groups were basically comparable after matching (Table S1 in the Supporting Information). Significant differences were found in preliminary analysis of outcome indicators (Table S2 in the Supporting Information).
Association Between SII and Outcomes
Cox proportional-hazards analysis unveiled (Table 2) that SII was significantly correlated with the incidence of RF [Model 1: HR, 1.31 (1.23–1.39), P < 0.001; Model 2: 1.30 (1.22–1.38), P < 0.001; Model 3: 1.19 (1.12–1.28), P<0.001] and the incidence of HRF [Model 1: HR, 1.29 (1.19–1.40), P < 0.001; Model 2: 1.29 (1.19–1.40), P < 0.001; Model 3: 1.16 (1.06–1.26), P<0.001]. In addition, compared with low SII (Q1), high SII (Q4) was linked to a higher incidence of RF [RF: Model 1: HR, 2.69 (2.15–3.35), P < 0.001; Model 2: 2.63 (2.11–3.29), P < 0.001; Model 3: 2.02 (1.59–2.57), P < 0.001]; HRF: Model 1: HR, 2.37 (1.78–3.15), P < 0.001; Model 2: 2.39 (1.79–3.20), P < 0.001; Model 3: 1.59 (1.17–2.15), P=0.003)].
 |
Table 2 Cox Regression Analysis for SII with Respiratory Failure and All-Cause Mortality |
Besides, SII was also significantly correlated with in-hospital mortality [Model 1: HR, 1.24 (1.09–1.41), P < 0.001; Model 2: 1.21 (1.06–1.37), P = 0.004; Model 3: 1.22 (1.07–1.39), P=0.003] and long-term follow-up mortality [Model 1: HR, 1.17 (1.09–1.25), P < 0.001; Model 2: 1.13 (1.06–1.21), P < 0.001; Model 3: 1.12 (1.05–1.19), P< 0.001].
RCS analysis suggested a nonlinear correlation between SII and RF in Model 1 and Model 2 (P<0.001) (Figure 2A and B). In the RF Model 3 and HRF Model 1–3, the nonlinear relationship was not significant (P>0.05) (Figure 2C-F). Elevated SII (logSII>7.19) was linked to an elevated risk of RF in COPD patients. In addition, we also observed similar trends in in-hospital mortality and long-term follow-up mortality (Figure S1).
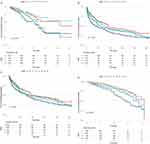
Incidence of All-Cause Mortality Among Different Groups
The Kaplan-Meier survival curve for intergroup all-cause mortality is shown in Figure 3. There were significant differences in the in-hospital mortality (Q1: 6.0% vs Q2: 7.3 vs Q3: 11.6 vs Q4: 16.0%, log-rank, P<0.001, Figure 3A) and long-term follow-up all-cause mortality (Q1: 33.1% vs Q2: 33.2 vs Q3: 39.2 vs Q4: 48.7%, log-rank, P < 0.001, Figure 3B) of each group. The association between increased mortality and higher SII disappeared after 21 days, with no statistical differences between groups (log-rank, P= 0.097, Figure 3C). Landmark analysis showed that during the 21-day short-term follow-up period, individuals with higher SII had a higher all-cause mortality rate compared to those with lower SII. (Q1: 6.0% vs Q2: 7.3 vs Q3: 11.6 vs Q4: 16.0%, log-rank, P<0.001, Figure 3D). Besides, we also found that, with the increase of SII, the all-cause mortality of patients with RF did not show significant differences between different SII groups (Figure S2).
Subgroup Analysis
Subgroup analysis was executed to delve further into the link between SII and the incidence of RF. In the adjusted Model 3, the results unveiled that increased SII was closely related to an elevated risk of RF in COPD patients in most subgroups (Figure 4). The trends of the risk of RF in most subgroups were similar. In the subgroup analysis of RF, except for the obvious interaction observed in cancer (P<0.001), pneumonia (P = 0.001), sepsis (P = 0.005), and BMI (P = 0.019), the majority of stratification factors did not considerably affect the correlation between SII and RF (Figure 4A). However, no significant interaction factors were found in the HRF subgroup (Figure 4B).
Discussion
This study is the pioneer, to our knowledge, in probing into the link between SII and the risk of RF and death in COPD patients. In this study, 1653 critically ill patients with COPD from the MIMIC-IV database were included, and the large sample size increased the reliability of the results. According to the findings, a higher SII was linked to a higher risk of RF and death as well as a longer hospital stay. Accordingly, SII may be a useful novel predictor of the prognosis of COPD patients. In addition, this correlation is still significant in PSM analysis, variable adjustment, and subgroup analysis. This enhances the validity of SII as a prognostic marker. Our findings are clinically significant in that SII may aid in early identifying high-risk COPD patients, carrying out early intervention, and promoting risk stratification management.
Nevertheless, the mechanism of SII linked to the poor prognosis of COPD is still unclear. There is a characteristic inflammatory pattern in COPD patients, that is, there is an increased number of neutrophils in the airway tract and macrophages, T lymphocytes, and B lymphocytes.16,30,31 Numerous immune cells, like lymphocytes and neutrophils, participate in the inflammatory response.14,17,32 In recent years, it has been found that platelets are involved in the inflammatory response of sepsis and other serious infections, and serve as a main contributor to the occurrence and progression of COPD.15 When infection occurs, inflammation activates the coagulation pathway and initiates platelet activation. Then the activated platelets can secrete pro-inflammatory substances and chemokines, regulate the function of white blood cells, and then participate in and induce the inflammatory process.
SII combines the predictive ability of neutrophil, lymphocyte, and platelet count, allowing it to accurately and thoroughly reflect our body’s inflammatory and immune condition. In some diseases, SII is a powerful prognostic indicator compared with the systemic inflammatory response biomarkers, encompassing neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), and monocyte-lymphocyte ratio (MLR).33,34 Although inflammatory molecules, consisting of tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and procalcitonin, perform well in the prognosis evaluation of patients,19 they are unable to accurately express the inflammatory and immune state of our body, and the high detection cost also limits their clinical application. The SII index is obtained from blood tests, which are commonplace for almost all hospitalized patients and are easily accessible in clinical practice. It is simple, fast, and cost-effective, and has broad application prospects, particularly, in underdeveloped areas.
Based on Cox proportional-hazards regression analysis, higher SII at admission amplifies the risk of RF and death, whether confounding factors are adjusted or not. Therefore, it is reasonable to conclude that SII is valuable and reliable in forecasting the prognosis of COPD patients. Through the Kaplan-Meier curve, we observed that patients with high SII had an elevated risk of mortality over time. Considerable differences were noted in the risk of death among the three groups. This significance was especially obvious in the early stage (within 21 days of admission). We suspected that the early inflammatory cytokine storm is more prominent, and a large number of inflammatory-related cytokines are increased and activated. This initial stage has a greater impact on the prognosis. SII is more valuable for forecasting short-term prognosis than for long-term prognosis.
There are also many previous studies on the predictive indicators of COPD patients.35–37 However, these studies often focus on mortality, and lack subgroup analysis on whether COPD patients have RF or RF types. Considering that once COPD patients are complicated with RF, it is often difficult to treat and results in high mortality. Therefore, in addition to mortality, RF is used as the primary outcome measure, which enriches the root cause analysis of this research. In addition, we also analyzed the mortality of patients with RF. The results showed that with the rise in SII, there was no significant difference in the risk of death among different groups in the COPD+RF population, possibly owing to the high-grade inflammation and high mortality of RF patients themselves. Therefore, in COPD patients, early identification of those with high risks of inflammation and RF is essential for the clinical treatment of COPD, thereby decreasing mortality and ameliorating prognosis.38
In the description of baseline characteristics, our study is more detailed than other similar studies.36,37 We included smoking history, BMI, the use of glucocorticoids, bronchodilators, antibiotics, mechanical ventilation, and information about other diseases that may cause inflammation, such as pneumonia and sepsis. Our findings revealed that patients with higher SII are more susceptible to cancers, heart failure, AECOPD, pneumonia, and sepsis. Although cancer, pneumonia, sepsis, and BMI showed obvious connections with RF, this effect was not observed in the subgroup analysis of HRF. HRF is the most typical type of RF in COPD. Therefore, this seems to further prove the validity of SII as a prognostic indicator of COPD, especially in forecasting the risk of HRF. In addition, patients with higher SII were less prone to liver diseases and dyslipidemia. A previous study has shown that severe liver diseases may affect the coordinated response of the liver to infection.39 Metabolic syndrome, including dyslipidemia, is closely related to systemic inflammation and cardiovascular risk.40,41 This seems to be inconsistent with our results, but no significant interaction between these two factors was found in subgroup analysis. The influence of liver diseases and blood lipids on inflammation needs to be further validated in future research.
Besides, the predictive power of SII for the prognosis of COPD+RF patients with cancer and sepsis is relatively weak. These conditions need to be considered when predicting the risk of RF in COPD patients. We hypothesized that these patients had obvious immune inflammatory reactions at the time of admission, which may affect the baseline white blood cell counts. When it comes to RF in COPD patients, pneumonia, sepsis, and cancers have to be considered. This is consistent with previous literature.42–44 Previous studies have also confirmed that the poor prognosis of these diseases is usually related to inflammation.27,42 However, we found that there were few patients in these subgroups. Therefore, these differences may be caused by small sample sizes.
Certainly, several limitations need to be considered. Firstly, since our study is single-center retrospective, the selection bias cannot be disregarded, limiting the generalizability of these results to other populations. Therefore, a large-scale multicenter prospective study is required in the future to further support our views. Secondly, due to the retroactive nature of the data collection, several significant variables might have been missed. Although we made adjustments for the confounding variables, our findings could still be affected by unidentified factors. Thirdly, Thirdly, changes throughout hospitalization were not taken into account when calculating SII; instead, just SII values at admission were used. Therefore, the ideal time period needs to be investigated. Fourthly, our research lacks information about other inflammatory markers, such as procalcitonin, IL-1, IL-6, and TNF-α, as well as blood culture and pathogenic bacteria. These may affect the baseline white blood cell counts. Ultimately, it is impossible to identify the likely mechanism underlying the link between high SII and a poor prognosis of COPD patients in this study. Consequently, additional research is warranted.
Conclusion
In conclusion, high SII may be closely correlated with a poor prognosis of critically ill COPD patients, such as a high risk of RF and all-cause mortality. Therefore, SII serves as a potential, cost-effective, and easily available biomarker for early risk assessment of this population. Nevertheless, larger prospective studies with long-term follow-up are desired to corroborate our conclusions.
Abbreviations
COPD, chronic obstructive pulmonary disease; SII, Systemic immune-inflammation index; MIMIC-IV, Medical Information Mart for Intensive Care IV; RF, Respiratory failure; HRF, hypercapnic Respiratory failure; SOFA, The sequential organ failure assessment; HF, Heart failure; SOFA, Sequential organ failure assessment; APSIII, Acute physiology score III; SAPSII, Simplified acute physiological score II; CHD, Coronary heart disease; AF, Atrial fibrillation; DM, Diabetes mellitus; CKD, Chronic kidney disease; AKI, Acute kidney injury; IQR, Interquartile range; PSM, Propensity score matching; RCS, Restricted cubic spline; BMI, Body mass index; RBC, Red blood cell; ICU, Intensive care unit; ICD-9, The ninth revision of the International Classification of Diseases; ICD-10, The tenth revision of the International Classification of Diseases; NT-proBNP, N-terminal pro brain natriuretic peptide; AMI, Acute myocardial infarction; HR, Hazard ratio; CI, Confidence interval; N, Number; Q, Quartile; RR, Respiratory rate; MBP, Mean blood pressure; SpO2, Saturation of peripheral oxygen; IHD, Ischemic heart disease; WBC, White blood cell; RDW, Red cell distribution width; Scr, Serum creatinine; BUN, Blood urea nitrogen; CRP, C-reactive protein; CRRT, Continuous renal replacement therapy; OASIS, Oxford acute severity of illness; LOS, length of stay; MIT, the Massachusetts Institute of Technology; BIDMC, the Beth Israel Deaconess Medical Center; PaO2, arterial oxygen partial pressure; FiO2, fractions of inspired oxygen; CO2, carbon dioxide.
Data Sharing Statement
Relevant data were retrospectively acquired from the Medical Information Mart for Intensive Care-IV (MIMIC-IV version 2.2) database (https://physionet.org/content/mimiciv/2.2/).
Ethics Approval and Informed Consent
This project was approved by the institutional review committee of MIT and BIDMC. All the protected private information of patients has been de-identified. Ethical approval for this study was obtained from the Medical Research Ethics Committee of The First Hospital of Jiaxing (No. 2023-LY-633).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Scientific Technology Plan Program for Healthcare in Zhejiang Province (NO. 2021KY1100), Jiaxing Science and Technology Plan Project (NO. 2022AD30055), the Key Discipline of JiaxingGenral Practice Medicine Construction Project (No.2023-fc-002), Key Construction Disciplines of Provincial and Municipal Co construction of Zhejiang [NO.2023-SSGJ-002].
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227–2242. doi:10.1016/s0140-6736(22)00470-6
2. Wang Z, Locantore N, Haldar K, et al. Inflammatory Endotype-associated Airway Microbiome in Chronic Obstructive Pulmonary Disease Clinical Stability and Exacerbations: a Multicohort Longitudinal Analysis. Am J Respir Crit Care Med. 2021;203(12):1488–1502. doi:10.1164/rccm.202009-3448OC
3. Burney PG, Patel J, Newson R, Minelli C, Naghavi M. Global and regional trends in COPD mortality, 1990-2010. Eur Respir J. 2015;45(5):1239–1247. doi:10.1183/09031936.00142414
4. Papadopoulos G, Vardavas CI, Limperi M, Linardis A, Georgoudis G, Behrakis P. Smoking cessation can improve quality of life among COPD patients: validation of the clinical COPD questionnaire into Greek. BMC Pulm Med. 2011;11:13. doi:10.1186/1471-2466-11-13
5. Scala R, Heunks L. Highlights in acute respiratory failure. Eur Respir Rev. 2018;27(147):180008. doi:10.1183/16000617.0008-2018
6. Khilnani GC, Banga A, Sharma SK. Predictors of mortality of patients with acute respiratory failure secondary to chronic obstructive pulmonary disease admitted to an intensive care unit: a one year study. BMC Pulm Med. 2004;4:12. doi:10.1186/1471-2466-4-12
7. Zhou L, Guan L, Wu W, et al. High-pressure versus low-pressure home non-invasive positive pressure ventilation with built-in software in patients with stable hypercapnic COPD: a pilot study. Sci Rep. 2017;7(1):16728. doi:10.1038/s41598-017-17142-2
8. Singanayagam A, Schembri S, Chalmers JD. Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10(2):81–89. doi:10.1513/AnnalsATS.201208-043OC
9. Bustamante-Fermosel A, De Miguel-Yanes JM, Duffort-Falcó M, Muñoz J. Mortality-related factors after hospitalization for acute exacerbation of chronic obstructive pulmonary disease: the burden of clinical features. Am J Emerg Med. 2007;25(5):515–522. doi:10.1016/j.ajem.2006.09.014
10. Steer J, Gibson J, Bourke SC. The DECAF Score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary disease. Thorax. 2012;67(11):970–976. doi:10.1136/thoraxjnl-2012-202103
11. Chen CW, Chen YY, Lu CL, et al. Severe hypoalbuminemia is a strong independent risk factor for acute respiratory failure in COPD: a nationwide cohort study. Int J Chron Obstruct Pulmon Dis. 2015;10:1147–1154. doi:10.2147/copd.S85831
12. Halpin DM, Miravitlles M, Metzdorf N, Celli B. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. doi:10.2147/copd.S139470
13. Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):71–86. doi:10.1016/j.ccm.2013.10.004
14. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
15. Chen YR, Chen V, Hollander Z, et al. C-reactive protein and N-terminal prohormone brain natriuretic peptide as biomarkers in acute exacerbations of COPD leading to hospitalizations. PLoS One. 2017;12(3):e0174063. doi:10.1371/journal.pone.0174063
16. Brusselle GG, Joos GF, Bracke KR. New insights into the immunology of chronic obstructive pulmonary disease. Lancet. 2011;378(9795):1015–1026. doi:10.1016/s0140-6736(11)60988-4
17. Yamaya M, Usami O, Nakayama S, et al. Malnutrition, Airflow Limitation and Severe Emphysema are Risks for Exacerbation of Chronic Obstructive Pulmonary Disease in Japanese Subjects: a Retrospective Single-Center Study. Int J Chron Obstruct Pulmon Dis. 2020;15:857–868. doi:10.2147/copd.S238457
18. Zhao J, Feng J, Ma Q, Li C, Qiu F. Prognostic value of inflammation biomarkers for 30-day mortality in critically ill patients with stroke. Front Neurol. 2023;14:1110347. doi:10.3389/fneur.2023.1110347
19. Şahin F, Koşar AF, Aslan AF, Yiğitbaş B, Uslu B. Serum Biomarkers in Patients with Stable and Acute Exacerbation of Chronic Obstructive Pulmonary Disease: a Comparative Study. J Med Biochem. 2019;38(4):503–511. doi:10.2478/jomb-2018-0050
20. Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. doi:10.1158/1078-0432.Ccr-14-0442
21. Wang BL, Tian L, Gao XH, et al. Dynamic change of the systemic immune inflammation index predicts the prognosis of patients with hepatocellular carcinoma after curative resection. Clin Chem Lab Med. 2016;54(12):1963–1969. doi:10.1515/cclm-2015-1191
22. Tang Y, Zeng X, Feng Y, et al. Association of Systemic Immune-Inflammation Index With Short-Term Mortality of Congestive Heart Failure: a Retrospective Cohort Study. Front Cardiovasc Med. 2021;8:753133. doi:10.3389/fcvm.2021.753133
23. Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
24. Wu S, Shi X, Zhou Q, Duan X, Zhang X, Guo H. The Association between Systemic Immune-Inflammation Index and All-Cause Mortality in Acute Ischemic Stroke Patients: analysis from the MIMIC-IV Database. Emerg Med Int. 2022;2022:4156489. doi:10.1155/2022/4156489
25. Hu L, Yu J, Deng J, Zhou H, Yang F, Lu X. Development of nomogram to predict in-hospital death for patients with intracerebral hemorrhage: a retrospective cohort study. Front Neurol. 2022;13:968623. doi:10.3389/fneur.2022.968623
26. Jia L, Li C, Bi X, et al. Prognostic Value of Systemic Immune-Inflammation Index among Critically Ill Patients with Acute Kidney Injury: a Retrospective Cohort Study. J Clin Med. 2022;11(14):3978. doi:10.3390/jcm11143978
27. Jiang D, Bian T, Shen Y, Huang Z. Association between admission systemic immune-inflammation index and mortality in critically ill patients with sepsis: a retrospective cohort study based on MIMIC-IV database. Clin Exp Med. 2023;1–10. doi:10.1007/s10238-023-01029-w
28. Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: a Review of the 2018 GOLD Report. Mayo Clin Proc. 2018;93(10):1488–1502. doi:10.1016/j.mayocp.2018.05.026
29. Blazek K, van Zwieten A, Saglimbene V, Teixeira-Pinto A. A practical guide to multiple imputation of missing data in nephrology. Kidney Int. 2021;99(1):68–74. doi:10.1016/j.kint.2020.07.035
30. Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–2653. doi:10.1056/NEJMoa032158
31. Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008;8(3):183–192. doi:10.1038/nri2254
32. Pan QX, Su ZJ, Zhang JH, Wang CR, Ke SY. A comparison of the prognostic value of preoperative inflammation-based scores and TNM stage in patients with gastric cancer. Onco Targets Ther. 2015;8:1375–1385. doi:10.2147/ott.S82437
33. Mirili C, Paydas S, Kapukaya TK, Yılmaz A. Systemic immune-inflammation index predicting survival outcome in patients with classical Hodgkin lymphoma. Biomarker Med. 2019;13(18):1565–1575. doi:10.2217/bmm-2019-0303
34. Shoji F, Takeoka H, Kozuma Y, et al. Pretreatment prognostic nutritional index as a novel biomarker in non-small cell lung cancer patients treated with immune checkpoint inhibitors. Lung Cancer. 2019;136:45–51. doi:10.1016/j.lungcan.2019.08.006
35. Zuo H, Xie X, Peng J, Wang L, Zhu R. Predictive Value of Novel Inflammation-Based Biomarkers for Pulmonary Hypertension in the Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Anal Cell Pathol. 2019;2019:5189165. doi:10.1155/2019/5189165
36. Fan L, Sun D, Yang J, et al. Association Between Serum Sodium and Long-Term Mortality in Critically Ill Patients with Comorbid Chronic Obstructive Pulmonary Disease: analysis from the MIMIC-IV Database. Int J Chron Obstruct Pulmon Dis. 2022;17:1143–1155. doi:10.2147/copd.S353741
37. Qiu Y, Wang Y, Shen N, et al. Association Between Red Blood Cell Distribution Width-Albumin Ratio and Hospital Mortality in Chronic Obstructive Pulmonary Disease Patients Admitted to the Intensive Care Unit: a Retrospective Study. Int J Chron Obstruct Pulmon Dis. 2022;17:1797–1809. doi:10.2147/copd.S371765
38. Zhou F, Xiong X, Li S, et al. Enhanced autophagic retrograde axonal transport by dynein intermediate chain upregulation improves Aβ clearance and cognitive function in APP/PS1 double transgenic mice. Aging (Albany NY). 2020;12(12):12142–12159. doi:10.18632/aging.103382
39. Bernsmeier C, van der Merwe S, Périanin A. Innate immune cells in cirrhosis. J Hepatol. 2020;73(1):186–201. doi:10.1016/j.jhep.2020.03.027
40. Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R. Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation. 2005;111(11):1448–1454. doi:10.1161/01.Cir.0000158483.13093.9d
41. Watz H, Waschki B, Kirsten A, et al. The metabolic syndrome in patients with chronic bronchitis and COPD: frequency and associated consequences for systemic inflammation and physical inactivity. Chest. 2009;136(4):1039–1046. doi:10.1378/chest.09-0393
42. Afessa B, Morales IJ, Scanlon PD, Peters SG. Prognostic factors, clinical course, and hospital outcome of patients with chronic obstructive pulmonary disease admitted to an intensive care unit for acute respiratory failure. Crit Care Med. 2002;30(7):1610–1615. doi:10.1097/00003246-200207000-00035
43. Ucgun I, Metintas M, Moral H, Alatas F, Yildirim H, Erginel S. Predictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failure. Respir Med. 2006;100(1):66–74. doi:10.1016/j.rmed.2005.04.005
44. Connors AF, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med. 1996;154(4 Pt 1):959–967. doi:10.1164/ajrccm.154.4.8887592
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.