Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Recommendations for the Implementation of the Self-Administration of Alpha-1 Antitrypsin
Authors Torres-Durán M, López-Campos JL , Calle Rubio M , Montero-Martínez C, Priegue Carrera A, Amaro Rodríguez R, Barrecheguren M, Barrio Guirado MA, Callejas-González FJ , Casas-Maldonado F , Diab-Cáceres L, García-Meseguer P, Hernández-Pérez JM , Lázaro-Asegurado L, Martínez-González C, Martínez Rivera C , Michel FJ, Montoro-Ronsano JB , Sánchez R, Ortiz-Pica M, Parra I, Quintero García JP, Ruiz-Serrano-de la Espada MDR, Tortajada-Goitia B, Miravitlles M
Received 18 May 2023
Accepted for publication 24 July 2023
Published 4 August 2023 Volume 2023:18 Pages 1691—1700
DOI https://doi.org/10.2147/COPD.S410611
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
María Torres-Durán,1 José Luis López-Campos,2,3 Myriam Calle Rubio,4 Carmen Montero-Martínez,5 Ana Priegue Carrera,6 Rosanel Amaro Rodríguez,7 Miriam Barrecheguren,8 María Ángeles Barrio Guirado,9 Francisco Javier Callejas-González,10 Francisco Casas-Maldonado,11 Layla Diab-Cáceres,12 Pilar García-Meseguer,9 José María Hernández-Pérez,13 Lourdes Lázaro-Asegurado,14 Cristina Martínez-González,15 Carlos Martínez Rivera,16 Francisco Javier Michel,17 José-Bruno Montoro-Ronsano,18 Raquel Sánchez,19 Marta Ortiz-Pica,20 Isabel Parra,21 José Pablo Quintero García,22 María del Rosario Ruiz-Serrano-de la Espada,23 Begoña Tortajada-Goitia,24 Marc Miravitlles8
1Pneumology Department, Hospital Álvaro Cunqueiro, NeumoVigo I+i Research Group, IIS Galicia Sur, Vigo, Spain; 2Instituto de Salud Carlos III, Centro de Investigación Biomédica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; 3Medical and Surgery Unit for Respiratory Diseases, Instituto de Biomedicina de Sevilla (IBiS), Hospital Universitario Virgen del Rocío/Universidad de Sevilla, Seville, Spain; 4Pneumology Department, Research Institute of Hospital Clínico San Carlos (IdISSC), Department of Medicine, Faculty of Medicine, University Complutense of Madrid, Madrid, Spain; 5Pneumology Department, Hospital Universitario de A Coruña, A Coruña, Spain; 6Nursing Unit, Hospital Álvaro Cunqueiro, Pontevedra, Spain; 7Pneumology Department, Hospital Clínic, Barcelona, Spain; 8Pneumology Department, Hospital Universitari Vall d’Hebron, Vall d’Hebron Institut de Recerca (VHIR), Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain; 9Nursung Unit, Hospital Universitari Vall d’Hebron, Barcelona, Spain; 10Pneumology Department, Complejo Hospitalario Universitario de Albacete, Albacete, Spain; 11Pneumology Department, Hospital Universitario Clínico San Cecilio, Granada, Spain; 12Pneumology Department, Hospital Universitario 12 de Octubre, Madrid, Spain; 13Pneumology Department, Hospital Universitario Nuestra Señora de La Candelaria, Santa Cruz de Tenerife, Tenerife, Spain; 14Pneumology Department, Complejo Asistencial Universitario de Burgos, Burgos, Spain; 15Instituto de Investigación Sanitaria del Principado de Asturias (FINBA-ISPA) Oviedo, Oviedo, Spain; 16Pneumology Department, Hospital Universitario Germans Trías I Pujol, Institut d’investigació Germans Trias i Pujol (IGTP), Badalona, Spain; 17Pneumology Department, Hospital Universitario Donostia, Donostia, Spain; 18Hospital Pharmacy Department, Hospital Universitari Vall d’Hebron, Vall d’Hebron Barcelona Hospital Campus, Barcelona, Spain; 19Pneumology Department, Hospital Universitario Basurto, Bilbao, Spain; 20Nursing Unit, Hospital Clínico San Carlos, Madrid, Spain; 21Pneumology Department, Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain; 22Hospital Pharmacy Department, Hospital Universitario Virgen del Rocío, Sevilla, Spain; 23Nursing Unit, Hospital Universitario Virgen del Rocío, Sevilla, Spain; 24Hospital Pharmacy Department, Hospital Costa del Sol, Málaga, Spain
Correspondence: María Torres-Durán, Tel +34986811111, Email [email protected]
Purpose: Administration of exogenous alpha-1 antitrypsin (AAT) is the only specific therapy for the management of pulmonary morbidity in patients with AAT deficiency. It requires weekly or biweekly intravenous infusions, which may impact patient independence and quality of life. Self-administration of AAT therapy is an alternative to reduce the burden for patients who require AAT therapy. We presented herein experts’ recommendations for the implementation of a program for the self-administration of AAT.
Methods: This project was conducted using a modified nominal group technique and was undertaken in two online meetings involving the participation of 25 experts: specialists in pulmonology (n=17), nurses (n=5) and hospital pharmacists (n=3).
Results: The following issues were discussed, and several recommendations were agreed upon on the following topics: a) patient profile and clinical evaluation, establishing selection criteria that should include clinical as well as social criteria; b) role of health care professionals, suggested roles for specialists in pulmonology, nurses, and hospital pharmacists; c) training by the nurse, including recommendations before initiating the training and the content of the training sessions; and d) logistic issues and follow-up, adherence, and patient support.
Conclusion: We expect this proposal to increase awareness of this therapeutic alternative and facilitate the implementation of self-administration programs, thus contributing to optimizing the patient experience with AAT therapy. Further research on the outcomes of these programs, especially from the patient perspective, will also help to improve their design and implementation.
Keywords: alpha-1 antitrypsin deficiency, disease burden, augmentation therapy, self-administration
Introduction
Administration of exogenous alpha-1 antitrypsin (AAT) is the only specific therapy for the management of pulmonary morbidity in patients with AAT deficiency.1,2 According to the Spanish registry on AAT deficiency, it is received by two-thirds of the patients with the genotype PI*ZZ,3 although large variations exist across Europe.4 Administration of exogenous AAT requires weekly or biweekly intravenous infusions, which may impact patient independence and quality of life.5 In a recent survey conducted among 16 patients with AAT deficiency who underwent a home-based administration program of AAT therapy, before starting the program, all patients reported that their augmentation therapy interfered “much” or “very much” with their lives.6 In the European Alpha-1 Research Collaboration survey conducted in 26 European countries, in nonreimbursed countries, hospital administration of augmentation therapy was considered by patients/caregivers as one of the most challenging barriers to treatment.7 Based on previous experiences with the successful self-administration of other intravenous therapies, such as in patients with hemophilia8,9 or hereditary angioedema,10–12 there is a growing interest in the self-administration of AAT therapy as an alternative to reduce the burden for patients who require AAT therapy. The initial infusions of AAT must be administered under the supervision of a health professional experienced in the treatment of AAT deficiency. However, for the subsequent infusions, an approved product by the European Medicines Agency for AAT therapy is allowed to be administered by a caregiver or by the patients themselves.13 Despite the potential advantages of self-administration and that this practice is supported by experts on the management of this clinical condition,4 self-administration of AAT therapy has been scarcely adopted by patients and rarely discussed with them by health care professionals (HCP).14 To improve this situation, several experts advocate for increasing awareness of the self-administration of AAT therapy through the development of guidelines and training programs for both HCP and patients.14,15 The objective of this project was to produce a set of recommendations for the implementation of a program for the self-administration of AAT.
Materials and Methods
This project was conducted using a modified nominal group technique, a qualitative method of consensus that is used when the evidence on a specific topic is very limited. It has been applied to different health care contexts, including practice development and education and training,16 two characteristics of the program we developed. For the scope of this consensus, self-administration was considered any administration out of the hospital that is undertaken by the patient, partner, or caregiver (ie, a nonhealthcare professional).
The project was initiated by the coordinator (MT) with the support of a sponsor and a research organization with expertise in these methods (see acknowledgments). The coordinator, a pulmonologist, selected a group of 5 experts on the management of AAT deficiency, 4 pulmonologists and a nurse who comprised the scientific committee (MCR, J-LL-C, CM-M, MM, APC). An additional group of 19 experts—the expert committee—was also selected based on their experience with the management of AAT deficiency and included pulmonologists (n=12), nurses (n=4) and hospital pharmacists (n=3).
The project was undertaken in two online meetings. The first meeting took place on June 10, 2021 with the participation of the coordinator and the scientific committee with the objective of presenting the project and the methodology to the scientific committee, establishing the timing, and defining the outline for the content of these recommendations. The second meeting was held on October 19, 2021, with all 25 participants present, including the coordinator and the scientific and expert committees. After a plenary session where the participants were told about the project and the process for that meeting, they were split into 5 groups in virtual rooms to discuss one point each of the index and the outline content (Supplementary Table 1). Each group was coordinated by a member of the scientific committee, and a member of the research organization acted as a facilitator of the discussion. The coordinator presented the initial content of their section as agreed upon in the first meeting by the scientific committee, and the facilitator asked the following: “What aspects do you consider should be modified in the proposed content that should be included in your section of the document?” The attendees spent several minutes thinking about the question and writing down their thoughts on the topics, which were recorded on a whiteboard. Afterward, the participants’ ideas were discussed and clarified in a group discussion, and where appropriate, similar views were grouped together with the agreement of all participants. Then, the facilitator asked the following: “Based on your expert opinion, which of these agreements do you think should be included in this section?” Finally, all participants met in a second plenary session where the coordinator of each group presented the agreements of the corresponding group, and the members of the other groups had the opportunity to add their views.
Results
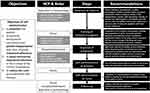
Below, we present a summary of the recommendations agreed upon by the experts, and the program is outlined in Figure 1.
Patient Profile and Clinical Evaluation
To establish the profile of patients who are adequate candidates for self-administration, the panel considers that it is important to bear in mind the objectives of self-administration: 1. to empower the patient to actively manage and control the disease; 2. to promote family/work conciliation and patient independence and, thus, improve treatment adherence; 3. to avoid nosocomial respiratory infections in the context of the COVID-19 pandemic; and 4. to reduce the costs associated with AAT therapy, especially those related to nursing activities.
The selection criteria should include clinical as well as social criteria. From the clinical perspective, patients must meet national or international criteria for receiving augmentation therapy, that in the Spanish setting are those of the REDAAT organization (Spanish Network on AAT deficiency)17 (Box 1); should show hemodynamic stability; should exhibit psychological stability to ensure adherence to the procedures and treatment; and must have the potential ability to perform canalization. From the social perspective, the patients should express their desire to improve their quality of life and/or to achieve greater independence from the hospital center; they should commit, after appropriate training, to perform the administration in an effective and safe manner, including the aseptic conditions for the administration; they should be able and willing to learn the administration technique; they should be stable from a personal point of view; and they should be compliant with their current treatments.
 |
Box 1 Criteria of the Spanish Network on AAT Deficiency (REDAAT-SEPAR) for the Administration of Alpha-1 Antitrypsin Augmentation Therapy |
The experts consider that the following situations preclude the participation of a patient in the self-administration program: not providing informed consent, presence of severe thrombocytopenia (<50,000 platelets/µL), being under treatment with anticoagulants, exhibiting New York Heart Association class III or IV heart failure, having a modified Medical Research Council Dyspnea Scale greater than 3 (except when the self-administration is provided by the partner or a caregiver), having a severe mental disorder (eg, a psychotic disorder) or having any social issue that precludes adequate self-administration or the ability to contact a health center.
Role of Health Care Professionals
We consider that HCPs who should be involved in a self-administration program for patients with AAT deficiency are pulmonologists, nurses, and hospital pharmacists. Their respective roles in the self-administration program are presented in Table 1 and can be summarized in three key points: consistent with the summary of product characteristics of the medicinal product, the pulmonologist is responsible for the decision of whether a patient is suitable for self-administration and will ensure that appropriate training is provided; the nurse is responsible for the patient/caregiver’s training; and the hospital pharmacist is responsible for dispensing the medicinal product and related issues such as monitoring treatment adherence.
 |
Table 1 Role of Health Care Professionals in a Self-Administration Program |
In addition to those roles, the participants consider that patients participating in the self-administration program should keep a diary where they can record information on every self-administered infusion (eg, date of administration, batches, dosage) and potential associated complications, including those related to the administration technique. This diary may help with the follow-up by the HCPs.
To facilitate communication among the HCPs, it is considered that the nurse could complete a checklist with the activities and/or actions related with the self-administration training performed with the patient/caregiver and share it with the hospital pharmacist and the pulmonologist. The proposed checklist is shown in Box 2.
 |
Box 2 Nurse Checklist for the Management of Patients Included in a Self-Administration Program of AAT Therapy |
Training by the Nurse
Although this section focuses on the training of the patients/caregivers, it is important to stress that all HCPs involved in the self-administration program should be trained on the basics of self-administration, including the technique itself and the problems—and how to handle them—that could arise during self-administration.
Potential risks associated with self-administration are related to the handling and administration of the medicinal product as well as to the handling of adverse reactions, particularly hypersensitivity. Therefore, patients/caregivers should be trained in all these aspects. A summary of the key points to be considered for the training of the patients/caregivers is presented in Table 2 and include recommendations before initiating the training and the content of the training sessions; the latter could be used as a checklist to ensure that the patients/caregivers have received adequate training and to inform the other HCPs. First self-administered infusions should be performed under the supervision of the nurse at the hospital; if possible, it is recommended to maintain a close follow-up during the first self-administered infusions at the patient’s home. Once the patient starts the self-administration without supervision, it is recommended that follow-up sessions be conducted every 4–6 months to ensure that once the skills have been acquired by a patient/caregiver, they are retained in the long term.
 |
Table 2 Key Points for the Training of the Patients on Self-Administration |
In addition to the training on the self-administration technique, the patient/caregiver should receive information on the potential incidents, including the most common adverse events that could arise during self-administration and how to handle them initially. It is also important that hospitals that implement a self-administration program offer support to the patients included in the program through a simple way to contact the HCP for the urgent resolution of doubts or problems with self-administration. In this regard, it is recommended that a pathway for problem solving for these patients be established.
To reinforce the patients/caregivers’ competencies for self-administration, it could be useful to provide them with actual patients’ testimonies on self-administration, including advantages and potential difficulties.
Logistic Issues
There are several logistic issues that patients/caregivers should be aware of regarding how to pick up the medicinal product, the equipment for the administration, and the disposal of the equipment after self-administration.
Initially, as stated above, medication is dispensed by the hospital pharmacy and, therefore, should be picked up there. The time intervals for picking up the medication should be agreed upon with the hospital pharmacy but should be sufficiently broad to be perceived as an advantage by the patients; however, it is recommended that the intervals not be longer than 3 months. The patients/caregivers should be informed that the medicinal product as provided (ie, before reconstitution) can be stored at room temperature (up to 25 °C).
The patients/caregivers should be familiarized with the material that is provided with the medicinal product: powder vial, solvent vial of water for injections, transfer set for reconstitution, IV infusion set, butterfly set and alcohol swabs.
The hospital pharmacist will instruct the patient/caregivers to return any unused medicinal product and how the waste material should be disposed of and returned. Thus, regular waste (eg, dressing, bags) can be managed normally and disposed of with common garbage; and sharp materials (eg, needles) and material containing biological waste should be disposed of in a sharp container marked with the biohazard symbol, which is resistant to puncture, leak-proof, and safe to handle. In any case, waste material disposal should comply with local regulations and hospital procedures. Appropriate containers will be provided by the hospital pharmacy. It would be useful to prepare some kind of visual aid for patients/caregivers (eg, a table, or infographic) which links the material provided for the self-administration with the type of waste/container that should be used.
Follow-Up, Adherence, and Patient Support
As in other therapeutic areas, treatment adherence and appropriate patient follow-up are essential to ensure the efficacy and safety of AAT therapy.
The monitoring of treatment adherence could be implemented in a complementary way. For example, at the time of dispensing the drug using the corresponding pharmacy registry, which, ideally, could have a red flag system to signal that the patients have not picked up the medication as scheduled; at that time, the pharmacist could ask for empty vials before dispensing the medications; and, as mentioned before, the patient should be encouraged to use a diary to record the medication administered with dates, batch numbers and so on.
It would be useful to prepare a patient resource booklet and/or quick guides providing basic instructions for self-administration, informing about common adverse events and the initial measures to handle them, and including practical recommendations for self-care (eg, skin care). Whenever possible, these resources should be prepared by a multidisciplinary team that includes all stakeholders involved in the self-administration, that is, HCPs and patients. The more visual they are, the more useful they will be for patients.
Patients must be able to clearly identify a HCP of reference, the nurse, who will provide the basic support for self-administration. To facilitate access to this professional, in addition to having a helpline, it is recommended that the patient schedule the infusions with a timing compatible with HCP availability. Patient advocacy groups could also have a role in patients’ support.
Discussion
The limited use of self-administration of AAT therapy despite its benefits is probably due to the lack of knowledge of this option by patients, as has been the case with other self-administration programs of parenteral medicines.18 It is likely that increasing awareness among HCPs about this alternative of administration would lead to better communication between HCPs and the patients and, in turn, would lead to greater awareness and interest among patients with AAT in self-administration. Our program aims to address that issue and to help HCPs implement a self-administration program in their settings. In a US survey among patients participating in the AlphaNet Disease Management and Prevention Program, 44 of the 555 patients who participated in the survey self-administered their AAT infusions, and 95% were very satisfied and 5% were satisfied with their treatment, but no other patient-reported outcomes were provided.14 Therefore, in our view, it is important to demonstrate the beneficial effects of the self-administration of AAT from the patients’ perspective, as it has been shown with other self-administered therapies, such as those for the management of hereditary angioedema.19,20
Another alternative strategy for the administration of AAT therapy is the administration of augmentation therapy at home by nurses. Some authors considered that using nurses for home-based administration has the advantage that they could routinely perform basic health assessments of patients with AAT deficiency.21 This strategy was evaluated in 16 patients with AAT deficiency, showing an improvement in the quality of life with no safety issues.6 We think that home-based administration by nurses could be an alternative for some patients, but it does not take into consideration the advantages of self-administration, such as self-care competence and independence.22,23
The selection of patients is considered critical for the success of a self-administration program.15 The criteria we have proposed are based on the opinions of experts. Although they are consistent with other expert recommendations,15 we should investigate using real-world data which takes in account characteristics of the patients, the disease, and the health care organization that are associated with the success of the program, with success being a complex outcome that should combine adherence to the program, patient’s satisfaction and quality of life, efficacy and lack of occurrence of relevant safety issues.
In the above mentioned survey among 44 users of self-administration of AAT therapy, most patients (84%) reported no difficulties with the procedure; the difficulties reported by 5 patients included the choice of the injection site, problems finding a vein, port blockage and intravenous stick injuries.14 In a qualitative study of potential users of self-administration of intravenous antibiotics, one of the key determinants encouraging patients to engage in self-administrations was the perception of being sufficiently knowledgeable, having adequate skills and feeling competent.18 A small survey of 22 patients undergoing AAT therapy showed that 8 patients were willing to switch from standard administration to a self-infusion program provided they were trained and educated.21 All these data indicate that training the patient is the core of the self-administration program and the area in which we should concentrate our efforts. Regarding the retention of initial training, an experience with self-administration of antibiotics suggests that these training programs could achieve excellent retention.24 However, in our view, it is recommended that follow-up training sessions be conducted to confirm that retention.
A major limitation of our work is that it did not involve the key stakeholder: the patient. We were focused on the organization of the program from the HCP point of view. However, it is essential that, in a second phase, we obtain feedback from patients with AAT deficiency on the materials we have produced and the procedure itself. Another potential limitation is that we have used the term self-administration with a meaning that goes beyond administration by the patients. However, this is consistent with the use of the term by other authors when referring to self-administration of AAT therapy.15 Finally, health care organizations differ across countries and even within the same country; therefore, our proposal should be customized to each specific setting through, for instance, the development of specific pathways for self-administration. Overall, it is important to stress that this is not a practice guideline, but a set of expert recommendations that needs to be validated. Current studies such as the AmAREtTI Study25 and future investigations such as those suggested above will help to improve these programs.
Conclusion
Overall, we expect that this proposal increases awareness about this therapeutic alternative and facilitates the implementation of self-administration programs and, thus, contributes to optimizing the patient’s experience with AAT therapy.
Abbreviations
AAT, alpha-1 antitrypsin; HCP, health care professionals; REDAAT, Spanish Network on AAT deficiency.
Data Sharing Statement
Not applicable. All the relevant information is presented with the manuscript.
Ethics Approval and Informed Consent
This project did not involve the participation of patients. Due to its nature, following the general Spanish regulations on biomedical research (ie Law 14/2007, of July 3, on Biomedical Research/La Ley 14/2007, de 3 de julio, de Investigación biomédica), this project did not require the evaluation of an Ethics Committee. The participating experts were informed about the nature of the project and agreed to participate by signing a contract.
Acknowledgments
The authors thank Sonia Pisa and Sofía Barreiro (Ampersand Consulting, Barcelona, Spain) for the coordination of the project and methodological support and Fernando Rico-Villademoros (COCIENTE S.L., Madrid, Spain) for editorial assistance. This support and assistance was funded by CSL Behring España.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was funded by CSL Behring España.
Disclosure
MT-D: has received consulting fees from CSL Behring and Grifols; payment or honoraria for lectures, presentations, speaker bureaus, manuscript writing or educational events from CSL Behring and Grifols; and support for attending meetings and/or travel from CSL Behring, Grifols and Chiesi. JLL-C: has received honoraria during the last 3 years for lecturing, scientific advice, participation in clinical studies or writing for publications from AstraZeneca, Bial, Boehringer Ingelheim, Chiesi, CSL Behring, Ferrer, Gebro, GlaxoSmithKline, Grifols, Menarini, Megalabs, Novartis and Rovi. MCR: has received speaker fees from AstraZeneca, Bial, Chiesi, CSL Behring, GlaxoSmithKline, Menarini, and Grifols; and consulting fees from GlaxoSmithKline, CSL Behring and Bial. CM-M: has received speaker fees and/or consulting fees and/or support to attend congresses from Astra-Zeneca, Boehringer-Ingelheim, Chiesi, CSL Behring, GlaxoSmithKline, Grifols and Menarini. APC: has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from CSL Behring. MB: has received speaker fees from Grifols, Menarini, CSL Behring, GSK, Boehringer Ingelheim and consulting fees from GSK, Novartis, CSL Behring and Boehringer Ingelheim. FJC-G: has received speaker honorarium from GlaxoSmithKline, Chiesi, Boehringer Ingelheim, Mundipharma, Menarini, Pfizer, Novartis, Esteve, Teva Pharmaceutical, Ferrer, Rovi, Roche, Astra Zeneca, Bial, Actelion, Alter, CSL Behring, Faes Farma, Alter, Grifols, Sanofi Genzyme and Gebro Pharma; consulting honorarium from Chiesi, Boehringer Ingelheim, Teva Pharmaceutical, Astra Zeneca, Bial, CSL Behring and Sanofi Genzyme; and travel grants from GlaxoSmithKline, Chiesi, Boehringer Ingelheim, Teva Pharmaceutical, Astra Zeneca and CSL Behring. FC-M: has received speaker fees from AstraZeneca, Bial, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Sanofi, Vertex, CSL Behring and Grifols; and consulting fees from AstraZeneca, Chiesi, GlaxoSmithKline, CSL Behring, and Grifols. JMH-P: Speaker honorarium from Grifols, CSL Behring, Astra-Zeneca, GSK, Bial laboratory, Teva laboratory and FAES Farma. Advisory honorarium from CSL Behring. Travel grants from Grifols and CSL Behring. LL-A: has received speaker honorarium from CSL Behring and Grifols SA; research grants from Grifols SA; consulting honorarium from CSL Behring; and travel grants from CSL Behring and Grifols SA. CMR: has received speaker honorarium from Astra Zeneca, CSL Behring CSL, Chiesi, Gebro, GSK, Mundipharma, TEVA and Sanofi; research grants from AstraZeneca, GSK and TEVA; and consulting and advisory honorarium from Astra Zeneca, CSL Behring, Chiesi, Mundipharma and TEVA. FJM: has received speaker fees and/or consulting fees and/or support to attend congresses from Astra-Zeneca, Boehringer-Ingelheim, Chiesi, CSL Behring, GlaxoSmithKline, Grifols, Menarini, Novartis, Sanofi Aventis and Teva. J-BM-R: has received speaker fees and/or consulting fees and/or support to attend congresses from CSL Behring and Grifols. RS: has received speaker fees and/or consulting fees and/or support to attend congresses from CSL Behring, Astra Zeneca, Chiesi, GlaxoSmithKline, Grifols, Teva, Novartis and Menarini. MO-P: has received speaker honorarium from Biogen, Novartis, Roche, Genzyme Sanofi and Takeda. JPQG: Advisory board member for CSL Behring. MM: has received speaker fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Menarini, Rovi, Bial, Kamada, Takeda, Sandoz, Zambon, CSL Behring, Specialty Therapeutics, Janssen, Grifols and Novartis; consulting fees from AstraZeneca, Atriva Therapeutics, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Bial, Gebro Pharma, CSL Behring, Inhibrx, Laboratorios Esteve, Ferrer, Menarini, Mereo Biopharma, Verona Pharma, Spin Therapeutics, ONO Pharma, pH Pharma, Palobiofarma SL, Takeda, Novartis, Sanofi and Grifols; and research grants from Grifols. RAR, MABG, LD-C, PGM, CM-G, IP, MRR-S-E and BT-G: have no conflict of interest.
References
1. Edgar RG, Patel M, Bayliss S, Crossley D, Sapey E, Turner AM. Treatment of lung disease in alpha-1 antitrypsin deficiency: a systematic review. Int J Chron Obstruct Pulmon Dis. 2017;12:1295–1308. doi:10.2147/COPD.S130440
2. Miravitlles M, Dirksen A, Ferrarotti I, et al. European Respiratory Society statement: diagnosis and treatment of pulmonary disease in α1-antitrypsin deficiency. Eur Respir J. 2017;50(5):1700610. doi:10.1183/13993003.00610-2017
3. Torres-Durán M, López-Campos JL, Rodríguez-Hermosa JL, et al. Demographic and clinical characteristics of patients with alpha-1 antitrypsin deficiency genotypes PI*ZZ and PI*SZ in the Spanish registry of EARCO. ERJ Open Res. 2022;8(3):00213–2022. doi:10.1183/23120541.00213-2022
4. Horváth I, Canotilho M, Chlumský J, et al. Diagnosis and management of α(1)-antitrypsin deficiency in Europe: an expert survey. ERJ Open Res. 2019;5(1):00171–2018. doi:10.1183/23120541.00171-2018
5. Sandhaus RA, Strange C, Zanichelli A, Skålvoll K, Koczulla AR, Stockley RA. Improving the lives of patients with alpha-1 antitrypsin deficiency. Int J Chron Obstruct Pulmon Dis. 2020;15:3313–3322. doi:10.2147/COPD.S276773
6. Annunziata A, Lanza M, Coppola A, Andreozzi P, Spinelli S, Fiorentino G. Alpha-1 antitrypsin deficiency: home therapy. Front Pharmacol. 2021;12:575402. doi:10.3389/fphar.2021.575402
7. Barrecheguren M, O’Hara K, Wilkens M, et al. Research priorities in α(1)-antitrypsin deficiency: results of a patients’ and healthcare providers’ international survey from the EARCO Clinical Research Collaboration. ERJ Open Res. 2020;6(4):00523–2020. doi:10.1183/23120541.00523-2020
8. Schrijvers LH, Beijlevelt-van der Zande M, Peters M, Schuurmans MJ, Fischer K. Learning intravenous infusion in haemophilia: experience from the Netherlands. Haemophilia. 2012;18(4):516–520. doi:10.1111/j.1365-2516.2012.02752.x
9. Khair K, Meerabeau L, Gibson F. Self-management and skills acquisition in boys with haemophilia. Health Expect. 2015;18(5):1105–1113. doi:10.1111/hex.12083
10. Longhurst HJ, Carr S, Khair K. C1-inhibitor concentrate home therapy for hereditary angioedema: a viable, effective treatment option. Clin Exp Immunol. 2007;147(1):11–17. doi:10.1111/j.1365-2249.2006.03256.x
11. Craig TJ. Recent advances in hereditary angioedema self-administration treatment: summary of an international hereditary angioedema expert meeting. Int Arch Allergy Immunol. 2013;161(suppl 1):1–2. doi:10.1159/000351228
12. Aberer W, Maurer M, Reshef A, et al. Open-label, multicenter study of self-administered icatibant for attacks of hereditary angioedema. Allergy. 2014;69(3):305–314. doi:10.1111/all.12303
13. European Medicines Agency. Respreeza. Summary of product characteristics; 2022. Available form: https://www.ema.europa.eu/en/documents/product-information/respreeza-epar-product-information_en.pdf.
14. Boyd B. Alpha-1 antitrypsin therapy: a satisfaction survey of individuals self-administering. A46 topics in alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2018;197:A1758.
15. Herth FJF, Sandhaus RA, Turner AM, Sucena M, Welte T, Greulich T. Alpha-1 antitrypsin therapy in patients with alpha-1 antitrypsin deficiency: perspectives from a registry study and practical considerations for self-administration during the COVID-19 pandemic. Int J Chron Obstruct Pulmon Dis. 2021;16:2983–2996. doi:10.2147/COPD.S325211
16. Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380. doi:10.1136/bmj.311.7001.376
17. Casas F, Blanco I, Martínez MT, et al. Indications for active case searches and intravenous alpha-1 antitrypsin treatment for patients with alpha-1 antitrypsin deficiency chronic pulmonary obstructive disease: an update. Arch Bronconeumol. 2015;51(4):185–192. doi:10.1016/j.arbres.2014.05.008
18. Tonna A, Anthony G, Tonna I, et al. Home self-administration of intravenous antibiotics as part of an outpatient parenteral antibiotic therapy service: a qualitative study of the perspectives of patients who do not self-administer. BMJ Open. 2019;9(1):e027475. doi:10.1136/bmjopen-2018-027475
19. Zanichelli A, Azin GM, Cristina F, Vacchini R, Caballero T. Safety, effectiveness, and impact on quality of life of self-administration with plasma-derived nanofiltered C1 inhibitor (Berinert®) in patients with hereditary angioedema: the SABHA study. Orphanet J Rare Dis. 2018;13(1):51. doi:10.1186/s13023-018-0797-3
20. Bygum A, Andersen KE, Mikkelsen CS. Self-administration of intravenous C1-inhibitor therapy for hereditary angioedema and associated quality of life benefits. Eur J Dermatol. 2009;19(2):147–151. doi:10.1684/ejd.2008.0603
21. Colello J, Ptasinski A, Zhan X, Kaur S, Craig T. Assessment of patient perspectives and barriers to self-infusion of augmentation therapy for alpha-1 antitrypsin deficiency during the COVID-19 pandemic. Pulm Ther. 2022;8(1):95–103. doi:10.1007/s41030-022-00182-z
22. Richardson SJ, Brooks HL, Bramley G, Coleman JJ. Evaluating the effectiveness of self-administration of medication (SAM) schemes in the hospital setting: a systematic review of the literature. PLoS One. 2014;9(12):e113912. doi:10.1371/journal.pone.0113912
23. Deeks PA, Byatt K. Are patients who self-administer their medicines in hospital more satisfied with their care? J Adv Nurs. 2000;31(2):395–400. doi:10.1046/j.1365-2648.2000.01286.x
24. Eaves K, Thornton J, Chapman AL. Patient retention of training in self-administration of intravenous antibiotic therapy in an outpatient parenteral antibiotic therapy service. J Clin Nurs. 2014;23(9–10):1318–1322. doi:10.1111/jocn.12376
25. CSL Behring. Respreeza® self-administration and learning program (AmAREtTI Study) (AmAREtTI); 2022. Available form: https://clinicaltrials.gov/ct2/show/NCT04262284.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.