Back to Journals » Clinical Interventions in Aging » Volume 17
Recognizing the Needs of High-Need High-Risk Veterans
Authors Dang S , Desir M, Lamba S, Muralidhar K , Tang F, Valencia WM
Received 18 June 2022
Accepted for publication 22 October 2022
Published 29 December 2022 Volume 2022:17 Pages 1907—1918
DOI https://doi.org/10.2147/CIA.S280437
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Stuti Dang,1– 3 Marianne Desir,1– 3 Shiv Lamba,4 Kiranmayee Muralidhar,1 Fei Tang,2 Willy Marcos Valencia5
1Miller School of Medicine, University of Miami, Miami, FL, USA; 2Geriatric Research, Education and Clinical Center, Miami Veterans Affairs Healthcare System, Miami, FL, USA; 3Department of Veterans Affairs Elizabeth Dole Center of Excellence in Veteran and Caregiver Research, Miami, FL, USA; 4Washington University, St. Louis, MO, USA; 5Division of Endocrinology, Diabetes and Metabolic Diseases, Medical University of South Carolina, Charleston, SC, USA
Correspondence: Stuti Dang, Email [email protected]
Introduction: Understanding the needs of higher-risk older adult patients can support the delivery of high quality and patient-centered healthcare. We sought to characterize the physical, functional, social and psychological needs of High-Need High-Risk (HNHR) Veterans. We hypothesized that the concept of frailty could be useful in identifying the highest-risk HNHR patients and characterizing their needs.
Methods: We conducted a cross-sectional study of Veterans in the Miami Veterans Affairs Healthcare System who were identified as High-Need High-Risk by the Department of Veterans Affairs (VA) using data analytic techniques. We analyzed data of 634 Veterans who completed questionnaires by mail, telephone or in person. We assessed the Veterans’ frailty status and needs in the physical, functional, psychological and social domains. Beyond descriptive statistics, we used Chi-square (χ2) test, one-way ANOVA and Kruskal–Wallis to analyze whether there were differences in Veterans’ needs in relation to frailty status.
Results: The HNHR Veterans who participated in the questionnaire had complex needs that spanned the physical, functional, psychological, and social domains. We observed a potential mismatch between functional needs and social support; over two-thirds of respondents endorsed having dependence in at least one ADL but only about a third of respondents reported having a caregiver. Patients with frailty had higher levels of functional dependence and were more likely than the other HNHR respondents to report recent falls, recent hospitalizations, depression, and transportation issues.
Conclusion: High-Need High-Risk Veterans have complex needs related to the physical, functional, psychological and social domains. Within the HNHR population, HNHR Veterans with frailty appear to have particularly high levels of risk and multidomain needs. Increased attention to identifying members of these groups and aligning them with biopsychosocial interventions that are targeted to their specific needs may support development of appropriate strategies and care-models to support HNHR Veterans.
Keywords: needs assessment, older adults, high need, frailty, biopsychosocial
Introduction
The United States population aged over 65 has nearly quadrupled in the current century.1 There has also been growth in the number of adults with multiple chronic health conditions and complex medical needs.2 Understanding the characteristics, experiences and needs of our highest-need patients can support the delivery to them of high quality and patient-centered healthcare.
The Veterans Health Administration’s Geriatrics and Extended Care Data Analysis Center (VHA GECDAC) uses a population health approach to identify High-Need High-Risk (HNHR) Veterans, who are community-dwelling Veterans at high risk of hospitalization and institutionalization. This national risk-stratified categorization represents Veterans who would qualify for Medicare’s demonstration of home-based primary care (ie, Independence at Home).3 The HNHR categorization is based on several factors, including service utilization and the Jen Frailty Index (JFI), which accounts for categories of illness linked to need for long-term care services.
The concept of frailty may be useful in characterizing the needs of HNHR Veterans. Frailty is a syndrome involving decreased physiological reserve that increases vulnerability to stressors.4,5 The development of frailty is often a complex and multifactorial process with etiologies and manifestations in the physical, functional and psychosocial domains.6–13 Frailty has been associated with a wide range of medical comorbidities, including heart failure, diabetes, cancer and end stage renal disease.7–10 Frailty has also been associated with cognitive impairment, functional dependence, and social isolation.4,5,11–13 Patients with frailty are at increased risk of institutionalization and mortality.13 Recognizing the presence of frailty and addressing relevant physical, functional, social and psychological factors in the lives of patients living with frailty may be helpful in improving patient outcomes.14
Our primary aim was to characterize the physical, social and psychological needs of the HNHR Veterans in the Miami Veterans Affairs Healthcare System (VAHS) in the context of frailty. Our hypothesis is that among HNHR older adults, the physical, functional, social and psychological needs progress with frailty. We seek to provide actionable data that will support ongoing efforts to develop targeted interventions that address and attend the needs of HNHR older adults.
Methods
We conducted a cross-sectional study of Veterans identified via GECDAC as HNHR. The variables used by GECDAC to determine HNHR status are available in the Department of Veterans Affairs (VA) electronic data, and include hospitalization in the prior 12 months, having a JEN Frailty Index15 score ≥6 [a measure of risk for characteristics related to frailty, including dependency in activities of daily living (ADLs) and institutionalization, based on ICD-9/10 diagnostic codes, with a score of ≥6 suggesting dependency in ≥2 ADLs], Nosos16 score (a VA risk-adjustment measure based on ICD-9/ICD-10 diagnostic codes), and Care Assessment Needs17 score (CAN score: a VA measure for hospitalization and mortality risk). Patients are excluded from the HNHR list if they have end-stage renal disease; are enrolled in Home Based Primary Care (HBPC) or medical foster home; have received hospice, palliative care, or nursing home care in the past 12 months; or live >60 minutes away from the closest VA primary care site. The exclusion criteria relate to the use of HNHR status to identify patients who may benefit from VA HBPC.
Two-thousand five hundred and forty-three Veterans receiving care in the Miami VAHS were identified by GECDAC as HNHR between October 2017 and September 2018. Of these 2,543 Veterans we randomly selected 1,300. Part of the 1,300 Veterans were sent a questionnaire by mail through the United States Postal Service in May 2018 and the remainder were sent the questionnaire by mail in November 2018. The questionnaires were conducted by mail only once, with no reminders to improve the response rate. An additional 173 HNHR Veterans being scheduled for a geriatric frailty clinic appointment completed the questionnaire: 71 in person and 102 by phone (Figure 1).
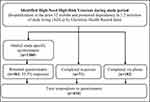 |
Figure 1 Flowchart showing completed questionnaires. |
The questionnaire was designed to provide information on physical health, functional ability, psychological health, and social characteristics. It incorporated some validated screening tools and some study specific questions to assess physical health including physical status18 and frailty;19–21 functional ability including mobility, falls, ADLs,22 instrumental activities of daily living (IADLs),23 and homebound status;24 psychological health including risk for depression,25 and self-perception of aging;26 and social characteristics including social isolation,27 social support, and transportation.28 Details of questionnaire components are given in Table 1.
 |
Table 1 Questionnaire Components |
Besides gathering data on the HNHR Veterans through the questionnaire, we also obtained other data for them from VA records, including CAN scores,17 JFI,15 Nosos scores,16 Hierarchical Condition Categories (HCC),30 and recent hospitalizations and ER visits. Additionally, we obtained the Area Deprivation Index (ADI), an established measure of socio-economic disadvantage at the census track level, from the Neighborhood Atlas.31,32
Statistical Analysis
Continuous variables are presented as mean ± standard deviation; categorical variables are presented as frequency and percent. Veterans were divided based on whether they responded to the questionnaire. The questionnaire respondents are divided by frailty status (frail, pre-frail, and robust) based on the 5-item FRAIL scale (Fatigue, Resistance, Ambulation, Illnesses, and Loss of Weight).19 Differences between groups for categorical variables were evaluated with a chi-square (χ2) test. One-way ANOVA and Kruskal–Wallis tests were used to evaluate the differences in continuous variables based on their distribution. All statistical analyses were performed with SAS 9.4 (Cary, NC). Statistical significance was considered at an alpha level of 0.05.
Ethical Considerations
The Miami VAHS institutional review board granted this study a waiver of documentation of informed consent, as it was deemed a quality improvement study (reference number 1360043-3). Participants provided their consent by filling out and returning the voluntary questionnaire.
Results
Questionnaire Respondents
Thirteen hundred HNHR Veterans were mailed the questionnaire, of which 461 (35.5%) were returned. Additionally, 102 Veterans filled the questionnaire over the phone and 71 in person in the frailty clinic, for a total of 634 respondents.
The average age of our 634 respondents was 70.5±9.2 years old, ranging from 39 to 100. The distribution of our subjects by age group were: ≤64 (n = 127, 20.0%), 65–69 (n = 163, 25.7%), 70–74 (n = 164, 25.9%), 75–79 (n = 87, 13.7%), ≥80 (n = 93, 14.7%). Only nineteen respondents were female. Of the respondents, 44.3% were White/Non-Hispanic and 35.2% were Black/Non-Hispanic, while 17.5% were Hispanic. Of the respondents, 47.9% were confident filling the medical forms by themselves, and 63.4% had more than a high school degree in education.
Table 2 gives a comparison of Veterans who responded to the mailed questionnaire (n = 461) and those who did not respond to the mailed questionnaire (n = 839). Non-respondence was associated with lower age and higher Nosos score (p < 0.001).
From the total of 634 Veterans who responded to the questionnaire, we were unable to determine frailty status, according to the FRAIL scale, for 39 (6.2%) individuals due to missing or incomplete responses. The 595 respondents with FRAIL scale data represent the main focus of our study. Table 3 provides detailed results regarding the 595 respondents with FRAIL scale data by physical, functional, psychological, and social domains.
 |
Table 2 Comparison of Veterans Who Did and Did Not Respond to the Questionnaire |
Physical Domain
Using the 5-Item FRAIL scale,19–21 we determined 266 (44.7%) Veterans were frail (score 3–5), 242 (40.7%) were prefrail (score 1–2), and 87 (14.6%) were robust (score 0). The mean JFI was 7.1±1.2. The mean CAN score was 93.4±7.3. A third (33.1%) of respondents rated their general health as bad or very bad, 41.7% of respondents rated it as average and 24.5% rated it as very good or good.
 |
Table 3 Respondents’ Characteristics by Frailty Status |
Functional Domain
The average Barthel Index score for ADLs of this sample was 84.4±19.8 (possible range 0–100, higher score indicating greater functional independence) and Lawton Score for IADLs was 6.1±2.1 (possible range 0–8, higher score indicating greater functional independence). On average, our study population was dependent in 2.3±2.7 ADLs and 1.9±2.1 IADLs. 71.8% of respondents reported dependence in at least one ADL, and 52.2% of respondents endorsed dependence in two or more ADLs.
Walking or balance issues were present among 436 (73.3%) HNHR Veterans and 381 (64.0%) reported using an assistive device: a cane (163, 27.4%), walker (147, 24.7%), or wheelchair (71, 11.9%). In the previous year, 378 (63.5%) reported one or more falls and 164 (27.6%) required medical attention for at least one fall.
Of the 375 respondents to questions on homebound status, we found that 42 (11.2%) were completely homebound and 121 (32.3%) were semi-homebound.
Psychological Domain
In the PHQ-2 depression screening, 195 (32.8%) Veterans screened positive for possible depression. The mean age of Veterans with positive depression screenings was lower than that of Veterans with negative depression screenings (67.7±9, vs 71.8±8.9, p≤0.01). Compared to those who screened negative, those who screened positive on the PHQ-2 scored lower on the Social Network Index, suggesting less participation in social relationships (1.2±1 vs 1.7±1.1, p ≤ 0.01). On a scale of 1–5, our population had an average score of 3.2±1.5 on the Attitude Toward Own Aging Scale, indicating a predominantly negative perception of aging, with frail Veterans scoring higher (3.7±1.3) compared to prefrail (3.2±1.5) or robust (2.0±1.6), p≤0.001.
Social Domain
Among all the respondents, 235 (39.5%) Veterans scored a 0 or 1 out of 4 in the Social Network Index, in which lower scores suggest greater social isolation. Merely 19 (3.2%) of the respondents had a score of 4 in the Social Network Index, which would suggest a high level of social integration. Only a third (199, 33.4%) of the Veterans reported having a caregiver, of whom 25 had paid/professional caregivers.
Veterans who were aged 70 or older were more likely to have a caregiver than younger Veterans (132, 39.3% vs 73, 25.8%, p ≤ 0.01). Those who screened positive for depression on the PHQ-2 were also more likely to report having a caregiver than those who screened negative (88, 44.4% of 198 vs 100, 30.6% of 327 Veterans, p ≤ 0.01).
Regarding transportation, 219 (36.8%) had trouble with transportation, and 130 (21.8%) reported delaying a doctor’s appointment due to transportation issues.
Health Care Utilization
In the six months prior to answering the questionnaire, 413 (69.4%) had visited the emergency room and 401 (67.4%) had been hospitalized. Among those who were hospitalized, 328 (55.1%) Veterans self-reported being admitted to a VA facility (acute hospital, skilled nursing facility or long-term nursing facility) whereas the rest (34, 5.7%) endorsed admission to community hospitals or nursing facilities.
Characteristics and Needs by Frailty Status
There were no significant differences in age, race or ethnicity between the robust, prefrail and frail HNHR Veterans who responded to the questionnaire (Table 3). Robust Veterans had a higher health literacy score (average score for confidence filling medical forms 4.5±0.9) compared to prefrail (4.2±1.2) or frail (3.7±1.4), p < 0.001.
The frail subgroup had higher JFI (7.2±1.2, p < 0.01), CAN score (94.5±6.1, p < 0.01) and Nosos score (3.6±3.0, p < 0.05) compared to the pre-frail group (JFI of 7±1.2, CAN score of 92.9±7.9, Nosos score of 3.2±3.3), and the robust group (JFI of 6.7±1.0, CAN score of 91.2±8.5, Nosos of 2.6±2.9). Patients with frailty were more likely to have been hospitalized in the past six months (p ≤ 0.05).
Among the frail population, a majority rated their health as “Bad” or “Very Bad” (140, 52.6%), while the pre-frail group primarily said it was “Average” (126, 52.1%) and most of the robust group rated it “Good” or “Very Good” (55, 63.2%) (p ≤ 0.01). Similarly, the frail population rated their physical status worse than the pre-frail and robust (4.7±2.0 in frail vs 5.6±1.8 in pre-frail and 7.3±1.5 in robust, p ≤ 0.01).
There was a higher average number of deficits in ADLs among the frail, compared to prefrail and robust (3.1±3.0 among frail patients, 2.1±2.5 among pre-frail, 0.4±1.2 among robust; p ≤ 0.01). There were also higher average numbers of IADL dependencies among patients with positive frailty screenings (2.7±2.2 among frail, 1.6±1.9 among pre-frail and 0.7±1.2 among robust; p ≤ 0.01). A higher number of frail patients reported one or more falls in the past 12 months (197, 74.1% vs 141, 58.3% in pre-frail vs 40, 46% in robust; p ≤ 0.01), and frail patients were more likely to have needed medical attention for falls in the past year (p ≤ 0.01). The frail group left their home less frequently and required more assistance doing so (p ≤ 0.01).
A higher number of frail patients screened positive for depression on the PHQ-2 (123, 46.2% vs 60, 24.8% in pre-frail and 12, 13.8% in robust, p ≤ 0.01) and had a more negative self-perception of aging (Attitude Toward Own Aging Scale score 3.7±1.3 vs 3.2±1.5 in pre-frail and 2.0±1.6 in robust, p ≤ 0.01).
A larger proportion of the frail reported having a caregiver (42.1%), compared to the pre-frail (31.8%) and robust (11.5%) (p ≤ 0.01). Over half (57.8%) of the frail reported not having a caregiver. Individuals who screened positive for frailty were also likely to be more socially isolated (SNI of 1.3±1.1) vs pre-frail (SNI = 1.7±1.1), vs robust (SNI = 1.6±1.1) (p = 0.01). Transportation troubles were reported more by the respondents with frailty (p ≤ 0.01), and they were more likely to have delayed medical appointments due to transportation issues (p ≤ 0.05).
Discussion
The study results demonstrate that HNHR Veterans have complex needs that span the physical, psychological, functional, and social domains and highlights some of the common challenges they face. Nearly three-quarters reported walking and balance issues, with over half having experienced at least one fall in the prior year. About a third of respondents had positive depression screenings, and those who screened positive for depression were more likely to be socially isolated compared to non-depressed. Social Network Index scores suggested that more than a third of respondents may be experiencing social isolation. Respondents reported functional dependence in an approximate average of two ADLs and two IADLs. Over two-thirds of respondents endorsed having dependence in at least one ADL, and over half of respondents reported dependence in two or more ADLs. Yet only about a third of respondents endorsed having a caregiver, and only about six percent of respondents reported having paid/professional caregivers. Overall, over 22 percent of HNHR Veterans reported having some or a lot of trouble with transportation and having delayed medical appointments due to transportation issues, and these increased with frailty.
These findings support the use of population-based metrics to help identify high-risk older adults. Preemptive identification using such automated electronic data may help enhance care delivery to ensure that intervention programs target those at highest risk and most likely to benefit. One such program is HBPC. The VA Geriatrics and Extended Care advise that all HNHR Veterans be enrolled in HBPC, yet Veterans Affairs Healthcare System is currently providing HBPC to less than 25% of the identified HNHR Veterans nationwide, due to limited reach and program capacity.3
Moreover, our data clearly show that the HNHR Veterans identified using population based metrics are not all the same. In fact, their needs are quite varied and seem to progress with increasing frailty. Our findings indicate that frailty screening may facilitate identification of particularly high-risk members of the population of HNHR Veterans, and high-risk patients in general, for targeting of relevant interventions such as HBPC. The 42% of HNHR Veterans who were assessed via the FRAIL scale as having frailty were more likely than the other HNHR Veterans to have had falls in the prior year and to have been hospitalized in the prior six months. The HNHR Veterans with frailty had higher average levels of dependence in ADLs and IADLs. They were more likely to screen as having depression, and they were more likely to endorse transportation concerns having caused delay of healthcare appointments. Only about forty percent of the frail HNHR Veterans reported having a caregiver, further raising concerns about these vulnerable adults’ access to needed support.
Our findings regarding HNHR patients with frailty are consistent with other studies that have supported that frailty is often a complex and multifactorial process with etiologies and manifestations in the physical, functional, psychological and social domains.6–13 Older adults with frailty, therefore, merit a biopsychosocial approach to healthcare delivery.7–9,11,12,14,33,34 Taking a biopsychosocial approach to provision of individualized supports in the four geriatric domains may reduce the burden of the specific physical, functional, psychological, and social concerns that we found HNHR patients in our healthcare system to be experiencing, while also supporting the commonly held goal of avoiding long-term institutionalization through successful “aging in place”.35 Our findings support more specifically that HNHR Veterans with frailty may benefit from increased alignment with existing VA programs that employ a biopsychosocial approach in addressing their multidomain needs, possibly in conjunction with expansion of these programs.
This study has multiple strengths. We used a novel VA set of preidentified HNHR older adults and surveyed them to gather insight into the four geriatric domains – physical, emotional, functional, and social, and further correlated the four domains to frailty status. Another strength is our multi-modal approach to gathering the data, via mail, telephone, and in person, which allows reaching a wider range of HNHR older adults and avoids the limitations of a single approach. Our respondents are representative of the HNHR Veteran population as evidenced by the few differences between the HNHR Veterans that responded to the questionnaire compared to those that did not. However, this study does have a few limitations. Our population was limited to the Miami VA, and may not be representative of all Veterans, since regional disparities in needs and resources may exist. We consider it will be beneficial to study these differences and equalize opportunities for all Veterans across the nation. A second limitation is the limited analysis of social needs, related to the methods available for data collection at this stage. Our next steps are to amplify the assessment of social needs including income, food, medication, and housing security. Third, we did not assess caregiver needs in this stage. We consider them a major component of the gaps in our understanding of HNHR patients and their contexts. We are currently implementing the longitudinal HERO Care survey which incorporates expanded social data and caregiver assessments in a large multicenter collaboration with other VA teams.36 Another limitation is that our population was overwhelmingly male. The gender demographics here reflect that of the VA, where 89.6% of all Veterans are male, and not of the general older adult population. Older female HNHR patients may have different needs than those described in this study.
Conclusion
High-Need High-Risk (HNHR) Veterans have complex needs related to the physical, functional, psychological and social domains. Within the HNHR population, HNHR Veterans with frailty appear to have particularly high levels of risk and multidomain needs. Increased attention to identifying members of these groups and aligning them with biopsychosocial interventions that are targeted to their specific needs may support achievement of Veterans’ personalized healthcare goals, which often include postponement or avoidance of extended stays in nursing homes.33,34,37 Next essential steps to improve the current state of care for vulnerable, HNHR patients, includes developing integrated evidence-based interventions38 and home- and community-based services that address provision of sufficient functional supports at home, connection with social and psychological supports, mitigation of fall risk, provision of transportation to healthcare appointments, and reduction of hospitalizations.
Impact Statement
We certify that this work is novel. No previous study had characterized needs of High Need High Risk older adult Veterans based on frailty status.
Funding
This work was supported in part by funding from the Health Services Research & Development Service of the US Department of Veterans Affairs (VA; SDR 18-313), the VA Office of Geriatrics and Extended Care (GEC) (VA GEC SP3E-GREA160), Veterans Integrated Service Network 8 (VISN8) GEC Office, and the Miami VA Geriatric Research, Education, and Clinical Center (GRECC).
Disclosure
The authors report no conflicts of interest in this work. The views expressed are those of the authors and do not represent an official position of the Department of Veterans Affairs. The data presented here were presented partly in a poster at the Gerontological Society of America Annual conference in 2020, in Philadelphia, PA, titled, Social Determinants and Frailty in High-Need, High-Risk Veterans. Innovation in Aging, Volume 4, Issue Supplement_1, 2020. PMCID: PMC7740872 doi: 10.1093/geroni/igaa057.578d.
References
1. Administration for Community Living/United States Department of Health and Human Services. 2020 profile of older Americans; 2021. Available from: https://acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans.
2. Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. doi:10.1093/epirev/mxs009
3. Edes TE, Davis D, Intrator O, Phibbs CS, Kinosian B. Focusing Independence at Home Qualifying Criteria (IAH-Q) to Identify High Need High Risk (HNHR) veterans who benefit from Home Based Primary Care (HBPC). J Am Geriatr Soc. 2019;67(S1):171.
4. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. doi:10.1093/gerona/56.3.M146
5. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727. doi:10.1093/gerona/62.7.722
6. Ni Lochlainn M, Cox NJ, Wilson T, et al. Nutrition and frailty: opportunities for prevention and treatment. Nutrients. 2021;13(7):2349. doi:10.3390/nu13072349
7. Pandey A, Kitzman D, Reeves G. Frailty is intertwined with heart failure: mechanisms, prevalence, prognosis, assessment, and management. JACC Heart Fail. 2019;7(12):1001–1011. doi:10.1016/j.jchf.2019.10.005
8. Simpson FR, Pajewski NM, Nicklas B, et al. Impact of multidomain lifestyle intervention on frailty through the lens of deficit accumulation in adults with type 2 diabetes mellitus. J Gerontol A Biol Sci Med Sci. 2020;75(10):1921–1927. doi:10.1093/gerona/glz197
9. Handforth C, Clegg A, Young C, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. 2015;26(6):1091–1101. doi:10.1093/annonc/mdu540
10. Zhao Y, Liu Q, Ji J. The prevalence of frailty in patients on hemodialysis: a systematic review and meta-analysis. Int Urol Nephrol. 2020;52(1):115–120. doi:10.1007/s11255-019-02310-2
11. Pinheiro IM, de Aguiar DS, Dos Santos DM, et al. Biopsychosocial factors associated with the frailty and pre-frailty among older adults. Geriatr Nurs. 2019;40(6):597–602. doi:10.1016/j.gerinurse.2019.06.002
12. Adja KYC, Lenzi J, Sezgin D, et al. The importance of taking a patient-centered, community-based approach to preventing and managing frailty: a public health perspective. Front Public Health. 2020;8:599170. doi:10.3389/fpubh.2020.599170
13. Vermeiren S, Vella-Azzopardi R, Beckwee D, et al. Frailty and the prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc. 2016;17(12):1163e1161–1163 e1117. doi:10.1016/j.jamda.2016.09.010
14. Travers J, Romero-Ortuno R, Bailey J, Cooney MT. Delaying and reversing frailty: a systematic review of primary care interventions. Br J Gen Pract. 2019;69(678):e61–e69. doi:10.3399/bjgp18X700241
15. Kinosian B, Wieland D, Gu X, Stallard E, Phibbs CS, Intrator O. Validation of the JEN frailty index in the National Long-Term Care Survey community population: identifying functionally impaired older adults from claims data. BMC Health Serv Res. 2018;18(1):908. doi:10.1186/s12913-018-3689-2
16. Wagner T, Gehlert E, Rosen A, Valenstein MJ. Updating the Psychiatric Case Mix System (PsyCMS) mental health and substance use grouper for ICD-10-CM. 2016.
17. Wang L, Porter B, Maynard C, et al. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368–373. doi:10.1097/MLR.0b013e31827da95a
18. Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. Am J Public Health. 1990;80(4):446–452. doi:10.2105/AJPH.80.4.446
19. Morley JE, Malmstrom TK, Miller DK, et al. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
20. Aprahamian I, Cezar NOC, Izbicki R, et al. Screening for frailty with the FRAIL scale: a comparison with the phenotype criteria. J Am Med Dir Assoc. 2017;18(7):592–596. doi:10.1016/j.jamda.2017.01.009
21. Thompson MQ, Theou O, Tucker GR, Adams RJ, Visvanathan R. FRAIL scale: predictive validity and diagnostic test accuracy. Australas J Ageing. 2020;39(4):e529–e536. doi:10.1111/ajag.12829
22. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
23. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi:10.1093/geront/9.3_Part_1.179
24. Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175(7):1180–1186. doi:10.1001/jamainternmed.2015.1849
25. Kroenke K, Spitzer RL, Williams JBW. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi:10.1097/01.MLR.0000093487.78664.3C
26. Lawton MP. The Philadelphia geriatric center morale scale: a revision. J Gerontol. 1975;30(1):85–89. doi:10.1093/geronj/30.1.85
27. Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County Residents. Am J Epidemiol. 1979;16(2):186–204. doi:10.1093/oxfordjournals.aje.a112674
28. Locatelli SM, Sharp LK, Syed ST, Bhansari S, Gerber BS. Measuring health-related transportation barriers in urban settings. J Appl Meas. 2017;18(2):178–193.
29. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594.
30. Centers for Medicare and Medicaid Services. Risk adjustment; 2022. Available from: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors.
31. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–2458. doi:10.1056/NEJMp1802313
32. University of Wisconsin School of Medicine and Public Health. 2019 area deprivation index v2.0. Downloaded from; 2019. Available from: https://www.neighborhoodatlas.medicine.wisc.edu/.
33. McDonald AP, Rizzotti R, Rivera JM, D’Arcy RCN, Park G, Song X. Toward improved homecare of frail older adults: a focus group study synthesizing patient and caregiver perspectives. Aging Med. 2021;4(1):4–11. doi:10.1002/agm2.12144
34. Kono A, Izumi K, Yoshiyuki N, Kanaya Y, Rubenstein LZ. Effects of an updated preventive home visit program based on a systematic structured assessment of care needs for ambulatory frail older adults in Japan: a randomized controlled trial. J Gerontol a Biol Sci Med Sci. 2016;71(12):1631–1637. doi:10.1093/gerona/glw068
35. National Institute on Aging/United States Department of Health and Human Services. Aging in place: growing older at home; 2017. Available from: https://www.nia.nih.gov/health/aging-place-growing-older-home.
36. Dang S, Garcia S, Munoz RA, et al. Intrator O. Measuring Unmet Needs of High-Need, High-Risk American Veterans and their Caregivers Using a Prospective Survey. In Symposium “Mission and vision of the multisite VA Elizabeth Dole Center of Excellence (EDCoE) for Veteran and Caregiver Research.” Accepted for the Gerontological Society of America (GSA) 2022 Annual Meeting, Abstract ID 1229240
37. Edes T, Kinosian B, Vuckovic NH, Nichols LO, Becker MM, Hossain M. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954–1961. doi:10.1111/jgs.13030
38. Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high-need, high-cost patients - an urgent priority. N Engl J Med. 2016;375(10):909–911. doi:10.1056/NEJMp1608511
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
