Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Real-World Treatment Patterns and Switching Following Moderate/Severe Chronic Obstructive Pulmonary Disease Exacerbation in Patients with Commercial or Medicare Insurance in the United States
Authors Bogart M, Germain G, Laliberté F, Lejeune D, Duh MS
Received 11 January 2023
Accepted for publication 3 July 2023
Published 24 July 2023 Volume 2023:18 Pages 1575—1586
DOI https://doi.org/10.2147/COPD.S398816
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Michael Bogart,1 Guillaume Germain,2 François Laliberté,2 Dominique Lejeune,2 Mei Sheng Duh3
1U.S. Value Evidence and Outcomes, R&D US, GSK, Research Triangle Park, NC, USA; 2Groupe d’analyse, Ltée, Montréal, QC, Canada; 3Analysis Group, Boston, MA, USA
Correspondence: Mei Sheng Duh, Analysis Group, 111 Huntington Ave 14th Floor, Boston, MA, 02199, USA, Tel +1 617 425 8131, Email [email protected]
Purpose: There is limited literature regarding real-world treatment patterns of patients with COPD, particularly since the introduction of once-daily single-inhaler triple therapy with fluticasone furoate/umeclidinium/vilanterol in 2017. Here, we evaluated treatment patterns of patients with COPD before and after a COPD exacerbation.
Patients and Methods: Retrospective, descriptive study using medical and pharmacy claims data and enrollment information from the Optum® Clinformatics® Data Mart database. Patients aged ≥ 40 years with ≥ 1 COPD exacerbation on or after September 18, 2017 were included. The index date was the last day of the first COPD exacerbation (ie day of visit for a moderate exacerbation or discharge date for a severe exacerbation). The baseline period was 12 months prior to index and the follow-up period (≥ 3 months) spanned from index until the earliest of health plan disenrollment, end of data availability (September 30, 2020), or death. Treatment patterns were evaluated during baseline and follow-up, with a focus on medication switching in the 90 days pre- and post-index.
Results: COPD exacerbations were identified in 307,727 patients (125,942 severe; 181,785 moderate). Mean age at index was 72.8 years; 56.3% were female. Before and after first exacerbation, 37.7% and 48.2% of patients used ≥ 1 controller medication, respectively. In the 90 days pre-index, ICS, LABA, and LAMA medications were used by 27.5% of patients. Of these users, 64.3% remained on the same medication class, 21.7% discontinued, and 14.1% switched medication in the 90 days post-index. Among switchers, 44.0% switched to triple therapy. Most common switches were ICS/LABA to ICS/LABA/LAMA (20.7%) and LAMA to ICS/LABA/LAMA (16.4%).
Conclusion: Many COPD exacerbations occur among patients not on controller medications. Although the percentage of patients receiving a controller medication increased following a first exacerbation, it remained below 50%. Of patients receiving controller medications pre-exacerbation, only a small proportion escalated to triple therapy post-exacerbation.
Keywords: COPD, medication switching, medication discontinuation, single-inhaler triple therapy, FF/UMEC/VI
Plain Language Summary
Chronic obstructive pulmonary disease (COPD) makes breathing difficult because airflow in and out of the lungs is restricted. COPD is often treated with inhalers that contain different combinations of drugs depending on how severe the patient’s COPD is. It is important that patients take controller medications to manage COPD symptoms and prevent flare-ups (exacerbations). It is also important that doctors change which medications they prescribe for patients with COPD when necessary, such as after an exacerbation. For patients who are on medication but keep having exacerbations, triple therapy can be prescribed, which reduces exacerbations and improves lung function compared with dual therapy. There is currently limited evidence to show which medication patients with COPD are taking before and after an exacerbation, so we searched a large database of medical and pharmacy insurance claims to investigate if medications were changed, continued, or stopped after an exacerbation. We found that many patients (62.3%) who had an exacerbation were not taking a controller medication at the time. After an exacerbation, more patients started taking a controller medication, but this number was still less than 50%. Additionally, 64.3% of patients kept taking the same medication, 21.7% stopped taking their medication, and 14.1% changed to a different medication. Among patients who changed medication, 44.0% started taking triple therapy. Doctors should therefore consider prescribing controller medications to patients who need them and triple therapy for those experiencing exacerbations.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive, incurable disease that can have a substantial impact on quality of life and reduce life expectancy.1–3 Options for pharmacological therapy of COPD include bronchodilators (eg long-acting β2-agonists [LABA]), antimuscarinic drugs (eg long-acting muscarinic antagonists [LAMA]), methylxanthines, and anti-inflammatory agents (eg inhaled corticosteroids [ICS]).1 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) clinical management guidelines recommend escalation to triple therapy (ICS/LABA/LAMA) for patients with COPD who experience persistent symptoms or exacerbations, despite dual therapy with LAMA/LABA or ICS/LABA.1
Historically, triple therapy required the use of two or three different inhalers (ie multiple-inhaler triple therapy [MITT]). More recently, fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI; once-daily dosing) and budesonide/glycopyrrolate/formoterol fumarate (twice-daily dosing) have been approved by the US Food and Drug Administration for maintenance treatment of COPD4,5 as single-inhaler triple therapy (SITT). Availability of combination therapy via a single inhaler may have a positive impact on treatment adherence, potentially improving clinical outcomes and saving costs.6–8 Compared with dual therapy (ICS/LABA or LAMA/LABA), triple therapy (ICS/LABA/LAMA) has been shown to improve lung function, decrease exacerbation rates (specifically in patients with prior exacerbations), and improve quality of life among patients with COPD.9–12
There is limited literature on treatment patterns in patients with COPD since the introduction of SITTs, particularly regarding medication switching following a COPD exacerbation. This study was therefore designed to evaluate real-world treatment patterns (including switch and discontinuation) of patients with COPD before and after a COPD exacerbation.
Materials and Methods
Study Design
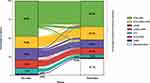
This retrospective, descriptive study was conducted using medical and pharmacy claims data and enrollment information from the Optum® Clinformatics® Data Mart (CDM) database from September 18, 2016 to September 30, 2020. The index date was defined as patients’ first COPD-related exacerbation (the date of visit for moderate exacerbations or discharge date for severe exacerbations; see the Study population section below for detailed definitions of exacerbations) on or after September 18, 2017. Baseline demographic and clinical characteristics were assessed in the 12 months prior to the index date (ie baseline period). Patients were observed from the index date for a minimum of 3 months until the earliest date of either death, health plan disenrollment, or end of data availability (ie follow-up period). Treatment patterns were evaluated during the baseline and follow-up periods, with a focus on medication switching in the 90 days pre- and post-index (Figure 1).
Data Source
The Optum® CDM database is a large, de-identified administrative claims database containing healthcare claims from approximately 17–19 million members annually in all US census regions. Both commercial and Medicare Advantage health plan data are included in the database, with information on patient demographics, dates of eligibility, date of death, and claims for inpatient and outpatient visits, pharmacy encounters, costs of services, and laboratory tests and results.
There was no direct subject contact or primary collection of data from individual study participants; data were obtained in tabular form and analyzed in aggregate form, ensuring anonymity of the participants. Consequently, informed consent, ethics committee approval, and Institutional Review Board approval were not required. This study used de-identified data that complied with the requirements of the Health Insurance Portability and Accountability Act.
Study Population
Eligible patients met the following inclusion criteria: ≥1 moderate or severe COPD exacerbation on or after September 18, 2017; ≥1 diagnosis of COPD during the baseline period or on the index date; ≥12 months of continuous health insurance coverage (with both medical and pharmacy coverage) before the index date; ≥3 months of continuous health insurance coverage after the index date; and ≥40 years of age at the index date. Patients with ≥1 COPD exacerbation during the 12-month baseline period and prior to the index exacerbation episode were excluded.
Moderate COPD exacerbations were defined as an outpatient or emergency room (ER) visit with a COPD exacerbation diagnosis code in the primary position and ≥1 dispensing/administration of a systemic corticosteroid or guideline-recommended antibiotic within 5 days following, or prior to, the visit. Severe COPD exacerbations were defined as an inpatient stay with a COPD exacerbation diagnosis code in the primary position. Exacerbations occurring within 14 days of each other were considered a single exacerbation episode and classified according to the highest severity.
Outcomes
Primary Endpoint
Patterns of COPD medication use were evaluated among the overall study population. Medication use (number and percentage of patients using COPD medications) was reported during the baseline and follow-up periods. Treatment patterns (switching, discontinuing, or remaining on the same medication) were compared between the 90 days pre- and post-first COPD exacerbation.
A switch was defined as the last medication on hand in the 90-day pre-index period (not including the index date) having a different medication class (ICS, LABA, LAMA, or any combinations) compared to the medication on hand at the first medication dispensed within the 90 days post-index (including the index date). Discontinuation was defined as a gap of >45 days between the end of the days of supply of a dispensing and the start date of the next fill, or between the end of the days of supply of the last dispensing and the end of the observation period. Patients remaining on therapy were those with the same medication class (ICS, LABA, LAMA, or any combinations) for the latest medication on hand in the 90 days pre-index (not including the index date) and the medication on hand at the first medication dispensed within the 90 days post-index (including the index date) or dispensing of the first medication beyond the 90-day window after the index date without discontinuation.
Secondary Endpoints
The secondary endpoint stratified medication use during the baseline and follow-up periods and treatment patterns pre- and post-first exacerbation by severity (moderate or severe) of the index COPD exacerbation.
Sensitivity Analyses
Sensitivity analyses were performed to evaluate treatment patterns (switching, discontinuing, or remaining on the same medication) in the 30 days pre- and post-first COPD exacerbation. In addition, an alternative definition of discontinuation was applied (a gap of >60 days between the end of the days of supply of a dispensing and the start date of the next fill, or between the end of the days of supply of the last dispensing and the end of the observation period).
Subgroup Analysis
Subgroup analyses were conducted among patients with additional COPD exacerbations during follow-up (ie patients experiencing a second and third exacerbation; all patients with a third exacerbation were also included in the group with a second exacerbation). The observation period for these patients spanned from the date of visit (moderate exacerbations) or date of discharge (severe exacerbations) of their second/third COPD exacerbation until the end of follow-up. Patients were required to have ≥3 months of continuous health insurance coverage following the discharge date of their second/third COPD exacerbation.
Results
Study Population
A total of 307,727 patients were included in the study. The mean age was 72.8 years, 56.3% of patients were female, and 88.5% had Medicare Advantage health insurance. The most common comorbidities were hypertension (82.3%), cardiac arrhythmias (39.8%), and diabetes (38.2%). A baseline asthma diagnosis was reported for 18.0% of patients (Table 1).
 |
Table 1 Patients’ Baseline Demographic and Clinical Characteristics |
The index exacerbation was defined as moderate for 181,785 (59.1%) patients and severe for 125,942 (40.9%) patients. The overall burden of comorbidities (as shown by the mean Quan-Charlson comorbidity index score) and healthcare costs (both overall and COPD-related) were higher among patients experiencing a severe versus moderate exacerbation. In total, 111,373 (36.2%) patients had a second exacerbation and 49,831 (16.2%) had a third exacerbation during the follow-up period.
Patterns of COPD Medication Use in the Overall Study Population
Prior to the first exacerbation, 37.7% of patients used ≥1 unique controller medication (Table 2). This rose to 48.2% during follow-up. The most used classes of controller medication during both the baseline and follow-up periods were ICS/LABA, and LAMA. Details of the individual drugs within each class are shown in Supplementary Table 1. SITT was used by 5.7% of patients after a COPD exacerbation compared with 1.1% at baseline and use of MITT also increased from 6.8% during baseline to 9.7% in the follow-up period. A total of 40.7% of patients used ≥1 rescue medication during the baseline period, which increased to 55.1% post-exacerbation. Short-acting β2-agonist was the most used class of rescue medication throughout the study.
 |
Table 2 Patients’ Use of COPD Medications During the Baseline and Follow-Up Periods |
A total of 84,615 (27.5%) patients were dispensed ≥1 controller medication during the 90 days before the index exacerbation. Pre-index controller medication classes dispensed closest to the index date were ICS/LABA (48.2%), LAMA (16.0%), and ICS/LAMA/LABA (15.9%; Figure 2). During the 90 days post-index, 14.1% of patients switched from their most recent pre-index controller medication to a new controller medication post-exacerbation. Details of switches by medication class are shown in Supplementary Table 2. Approximately two-thirds (64.3%) of patients remained on the same controller medication, and 21.7% discontinued their medication. Of the patients who switched to a different controller regimen, triple therapy (either MITT or SITT) was the most common controller medication switched to (44.0%), followed by ICS/LABA (21.9%), and LAMA (16.7%).
Patterns of COPD Medication Use Stratified by Exacerbation Severity
Prior to first exacerbation, fewer patients in the severe cohort used ≥1 unique controller medication than patients in the moderate cohort (27.3% and 44.8%, respectively; Table 2), which increased to 35.9% and 56.7%, respectively, during the follow-up period. ICS/LABA was the most common medication class for both the severe and moderate cohorts during both the baseline (16.2% vs 26.6%) and follow-up (21.1% vs 33.7%) periods.
In the 90 days post-index COPD exacerbation, the percentage of patients switching treatment was similar among patients experiencing either severe or moderate COPD exacerbations (16.4% vs 13.0%; Supplementary Table 2). More patients in the severe cohort switched from any medication class to triple therapy following an exacerbation compared with the moderate cohort (6.7% vs 5.9%, respectively). Treatment patterns for both stratifications were similar to those of the overall population.
Sensitivity Analyses
A total of 72,234 patients used ≥1 controller medication in the 30 days prior to the index date and, of these, 17.7% were using any type of triple therapy. Results for treatment patterns were similar to those in the main analysis, with 9.9% of patients switching medication, 63.5% remaining on the same medication, and 26.7% discontinuing treatment (Supplementary Table 3).
Using a 60-day gap definition for medication discontinuation, similar trends were observed relative to the main analysis, with a slightly lower proportion of patients switching treatments (13.7%) and slightly fewer patients discontinuing treatments (21.3%; data not shown).
Subgroup Analyses of Patients with Second and Third Exacerbations
More patients in the subgroups used ≥1 unique controller medication during follow-up than in the overall population (second exacerbation: 61.6%; third exacerbation: 69.2%; vs 48.2% in the overall population; Table 3). As in the overall population, the most common controller medication classes used during follow-up were ICS/LABA (second exacerbation: 36.3%; third exacerbation: 40.3%) and LAMA (second: 19.3%; third: 22.5%). In addition, the percentages of patients who received SITT during follow-up after a second and third exacerbation were higher than in the overall population (9.4% and 12.3%, respectively, vs 5.7%).
 |
Table 3 Subgroup Analysis: COPD Medications Used During the Follow-Up Period Among Patients Experiencing ≥1 COPD Exacerbation |
In total, 46,978/111,373 (42.2%) patients with a second exacerbation and 25,541/49,831 (51.3%) patients with a third exacerbation were dispensed a controller medication during the 90 days prior to the index exacerbation (data not shown in table or figure). The percentages of patients who switched (second: 15.7%; third: 16.4%), remained (second: 63.4%; third: 64.1%), or discontinued (second: 21.0%; third: 19.5%) treatment in the subgroups were similar to those in the main analysis (data not shown in table or figure).
Discussion
This real-world retrospective study using a large US claims database found that many COPD exacerbations occur among patients not treated with controller medications. Although the proportion of patients receiving a controller medication increased following a first exacerbation, less than half of the patients in this study were using controller medications. In addition, this study showed that although the most common medication switched to was triple therapy, very few patients in the subgroup of patients with a history of multiple exacerbations were using triple therapy, despite this being recommended by GOLD guidelines.1
A higher percentage of patients with a severe exacerbation were not receiving controller medication at baseline compared with those with a moderate exacerbation, which might suggest that some patients with COPD may be initially diagnosed at the time of hospitalization. The data also suggest that patients with COPD may be at increased risk of a severe exacerbation due to the under-use of controller therapy. This finding reiterates an ongoing observation that many patients do not receive guideline-recommended care or are diagnosed after an acute worsening of COPD. In a study using healthcare claims from 2007 to 2008, approximately one-third of patients with COPD were not using long-acting maintenance medications despite having a history of exacerbation.13 In this study, 51.8% of patients were not treated with a controller medication following a first COPD exacerbation. Among patients with a second and third exacerbation, less than 70% initiated a controller medication following their exacerbation, further highlighting that many patients are not being treated in line with GOLD recommendations.
The percentage of patients receiving triple therapy increased after an exacerbation and was higher in patients experiencing multiple exacerbations. Triple therapy was the most common medication switched to post-exacerbation. However, the proportion of patients with a history of exacerbation who escalated to triple therapy was still low, suggesting that not all patients were treated in accordance with GOLD recommendations.1 This possibility would be consistent with a previous US study of treatment patterns that showed the reasons for prescribing triple therapy for COPD in clinical practice differed from those defined by GOLD.14 Triple therapy, as recommended by current guidelines, could fill an unmet need for many patients with COPD in whom the occurrence of an exacerbation demonstrates insufficient therapy.
Detailed exploration of the reasons underlying treatment patterns was beyond the scope of this study. However, a recent real-world study from Slovakia reported that the principal motivations for switching to SITT in COPD were expected improvements in lung function, dyspnea, and number of exacerbations.15 In the UK, patients initiating MITT tend to have a history of acute exacerbations or clinically relevant/severe symptoms.16 In an earlier study from the US, approximately 50% of patients had an exacerbation in the 12 months prior to initiation of triple therapy, and treatment discontinuation, smoking history, LAMA use, and concomitant medication use were identified as significant predictors of progression to triple therapy.17 Another US study found that the majority of patients with COPD were prescribed MITT following maintenance medication use or after an exacerbation, with 9.6% of patients initiating MITT without prior history of an exacerbation or no previous COPD treatment. Patients may have initiated triple therapy without history of an exacerbation due to persistent symptoms, mild or unobserved exacerbations, or based on spirometry results.18 In this study, the proportion of patients who initiated triple therapy without history of exacerbation was lower (7.9%). It should be noted that our population had more advanced age than the studies referenced here, and the patients we included were likely to have Medicare health insurance and a high comorbidity burden, which may have affected treatment patterns and exacerbation rates.
This study has limitations which should be considered. Firstly, a dispensed medication does not indicate that the patient took the medication as prescribed on that date. Therefore, medication combination relies on overlapping days of supply. In addition, requiring the study population to have ≥3 months of continuous health insurance coverage after the index date selects for a population of patients who survive their first COPD exacerbation or do not disenroll within 3 months. The subgroups of patients with a second/third exacerbation are further selected as survivors, potentially introducing a survival bias. Specific clinical measures (eg lung function) and some patient characteristics (eg tobacco use) were not available in the claims database, as well as the reason for changing medication and the individuals involved in the decision. Medications such as over-the-counter products, drug samples, and medications received during an inpatient stay were also not captured in the database. Medical events (including COPD exacerbations) that did not require medical care resulting in an insurance claim were also not represented in the data. Results may have limited generalizability to segments of the US population with no insurance/other types of public insurance. Finally, the analysis is vulnerable to coding inaccuracies.
Conclusion
Many COPD exacerbations occur among patients who are not treated with controller medications. Although the percentage of patients receiving a controller medication increased following a first exacerbation, it remained below 50% in the overall study population. Of the patients receiving controller medications prior to an exacerbation, only a small proportion escalated to triple therapy after an exacerbation. The results of this study may help inform healthcare providers when considering the use of controller therapy among patients with evidence of exacerbation, in line with guideline recommendations.
Abbreviations
CCI, Charlson Comorbidity Index; CDM, Clinformatics® Data Mart; COPD, chronic obstructive pulmonary disease; ER, emergency room; FF, fluticasone furoate; GOLD, Global Initiative for Chronic Obstructive Lung Disease; HRU, healthcare resource utilization; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; MITT, multiple-inhaler triple therapy; PDE-4, phosphodiesterase-4; SABA, short-acting β2-agonist; SAMA, short-acting muscarinic antagonist; SITT, single-inhaler triple therapy; SD, standard deviation; UMEC, umeclidinium; VI, vilanterol.
Data Sharing Statement
The data held in the Optum® database contain proprietary elements owned by Optum® and therefore cannot be broadly disclosed or made publicly available at this time. The disclosure of these data to third-party clients assumes certain data security and privacy protocols are in place and that the third-party client has executed Optum®’s standard license agreement which includes restrictive covenants governing the use of the data.
Ethics Approval and Informed Consent
There was no direct subject contact or primary collection of data for individual study participants; data were obtained in tabular form and analyses were performed in aggregate, ensuring anonymity of the participants. Consequently, informed consent, ethics committee approval, and Institutional Review Board approval were not required. This study used de-identified data that complied with the requirements of the Health Insurance Portability and Accountability Act.
Acknowledgments
Editorial support (in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing, and referencing) was provided by Kathryn Wardle and Abigail Marmont of Aura, a division of Spirit Medical Communications Group Limited, and was funded by GSK.
These data have been previously presented in abstract/presentation form at the American Thoracic Society Meeting, San Francisco, California, May 13–18, 2022: Bogart M, Germain G, Laliberté F, Lejeune D, Duh MS. Real-world treatment patterns following chronic obstructive pulmonary disease (COPD) exacerbation in patients with commercial or Medicare insurance in the United States. Am J Respir Crit Care Med. 2022;205:A3777.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by GSK (study number 214998). The sponsor was involved in study conception and design, data interpretation, and the decision to submit the article for publication. The sponsor also had the opportunity to review the manuscript for medical and scientific accuracy and intellectual property considerations.
Disclosure
The authors declare the following real or perceived conflicts of interest during the last 3 years in relation to this manuscript: MB was a permanent employee of, and held stocks/shares in, GSK at the time of study conduct. GG, FL, DL, and MSD are employees of Analysis Group, which received funding from GSK to conduct this study, although not for manuscript development.
Current affiliation details for MB: Gilead Sciences, Foster City, CA, USA. Dr Mei Sheng Duh reports grants from GSK, during the conduct of the study; grants from AbbVie, grants from AstraZeneca, grants from Ayala Pharmaceuticals, grants from Bayer, grants from Blueprint Medicines, grants from GSK, grants from Humacyte, grants from Janssen, grants from Merck, grants from Novartis, grants from Pfizer, grants from Sanofi, and grants from Takeda, outside the submitted work. The authors report on other conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease – 2022 report; 2022. Available from: https://goldcopd.org/2022-gold-reports/.
2. Hindelang M, Kirsch F, Leidl R. Effectiveness of non-pharmacological COPD management on health-related quality of life - a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2020;20(1):79–91.
3. World Health Organization. Chronic obstructive pulmonary disease (COPD); 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)).
4. GlaxoSmithKline. Prescribing information for Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol inhalation powder); 2019. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/209482s003lbl.pdf.
5. AstraZeneca. Prescribing information for Breztri Aerosphere™ (budesonide, glycopyrrolate, and formoterol fumarate inhalation aerosol); 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/212122s000lbl.pdf.
6. Bogart M, Stanford RH, Laliberte F, Germain G, Wu JW, Duh MS. Medication adherence and persistence in chronic obstructive pulmonary disease patients receiving triple therapy in a USA commercially insured population. Int J Chron Obstruct Pulmon Dis. 2019;14:343–352.
7. Bourbeau J, Bafadhel M, Barnes NC, et al. Benefit/risk profile of single-inhaler triple therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2021;16:499–517.
8. Miravitlles M, Marin A, Huerta A, Carcedo D, Villacampa A, Puig-Junoy J. Estimation of the clinical and economic impact of an improvement in adherence based on the use of once-daily single-inhaler triple therapy in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2020;15:1643–1654.
9. Lipson DA, Barnacle H, Birk R, et al. FULFIL trial: once-daily triple therapy for patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;196(4):438–446.
10. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680.
11. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084.
12. Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48.
13. Diette GB, Dalal AA, D’Souza AO, Lunacsek OE, Nagar SP. Treatment patterns of chronic obstructive pulmonary disease in employed adults in the United States. Int J Chron Obstruct Pulmon Dis. 2015;10:415–422.
14. Schabert V, Shah S, Holmgren U, Cabrera C. Prescribing pathways to triple therapy in patients with chronic obstructive pulmonary disease in the United States. Ther Adv Respir Dis. 2021;15:17534666211001018.
15. Lassan S, Keszegh J, Lassanova M. Characteristics of COPD patients treated with single-inhaler triple therapy in real-life clinical practice. Bratisl Lek Listy. 2022;123(1):27–36.
16. Sansbury LB, Bains C, Lipson DA, Ismaila AS, Landis SH. Real-world treatment patterns of multiple-inhaler triple therapy among patients with chronic obstructive pulmonary disease in UK general practice. Int J Chron Obstruct Pulmon Dis. 2021;16:1255–1264.
17. Lane DC, Stemkowski S, Stanford RH, Tao Z. Initiation of triple therapy with multiple inhalers in chronic obstructive pulmonary disease: an analysis of treatment patterns from a U.S. retrospective database study. J Manag Care Spec Pharm. 2018;24(11):1165–1172.
18. Bogart M, Stanford RH, Reinsch T, Hull M, Buikema A, Hulbert E. Clinical characteristics and medication patterns in patients with COPD prior to initiation of triple therapy with ICS/LAMA/LABA: a retrospective study. Respir Med. 2018;142:73–80.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.