Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Readiness for Interprofessional Education Among Health Profession Students in a University in the United Arab Emirates
Authors Yasin H , Palaian S , Shankar PR , Nallamilli S
Received 28 October 2022
Accepted for publication 9 February 2023
Published 26 April 2023 Volume 2023:16 Pages 1141—1149
DOI https://doi.org/10.2147/JMDH.S395320
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Haya Yasin
Views: 145
Haya Yasin,1,2 Subish Palaian,3,4 Pathiyil Ravi Shankar,5 Sridevi Nallamilli6
1Department of Pharmaceutical Sciences, College of Pharmacy and Health Sciences, Ajman University, Ajman, United Arab Emirates; 2Discipline of Pharmaceutical Sciences, School of Pharmaceutical Sciences, University Sains Malaysia, Penang, Malaysia; 3Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University, Ajman, United Arab Emirates; 4Center of Medical and Bio-Allied Health Sciences Research, Ajman University, Ajman, United Arab Emirates; 5IMU Centre for Education, International Medical University, Kuala Lumpur, Malaysia; 6Department of Obstetrics and Gynecology, College of Medical Sciences, Bharatpur, Bagmati Province, Nepal
Correspondence: Haya Yasin, Department of Pharmaceutical Sciences, College of Pharmacy and Health Sciences, Ajman University, Ajman, United Arab Emirates, Tel +971557176919, Email [email protected] Subish Palaian, Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University, Ajman, United Arab Emirates, Tel +971551322957, Email [email protected]
Introduction: Inter-Professional Education (IPE) is an educational engagement between students from two or more professions possibly leading to better collaboration among them in the future workplace. Several organizations have advocated, developed, and updated guidelines for IPE.
Objective: This study was aimed at assessing the medical, dental, and pharmacy students’ readiness toward interprofessional education (IPE), and to identify the association between readiness and the demographic profile of students in a university in the United Arab Emirates (UAE).
Methods: A cross-sectional questionnaire-based exploratory study involving 215 medical, dental, and pharmacy students at Ajman University, UAE, using convenience sampling. The survey questionnaire (Readiness for Interprofessional Learning Scale, RIPLS) had a total of 19 statements. The first 9 items were related to “teamwork and collaboration”, items 10– 16 were related to “professional identity”, and the remaining three (items 17– 19) were related to “roles and responsibilities”. The individual statements’ median (IQR) scores were calculated and the total scores were compared with the demographic characteristics of the respondents with suitable non-parametric tests at alpha=0.05.
Results: Altogether, 215 undergraduate students (medical (n= 35)), pharmacy (n=105), and dental (n=75) responded to the survey. The median (IQR) score for the 19 individual statements was ‘ 5 (4– 5)’ for 12 of the statements. The total scores and domain-specific scores (teamwork and collaboration, professional identity, and roles and responsibilities) according to respondents’ demography showed significant differences only in the case of the educational stream with professional identity score (p=< 0.001), and the total RIPLS score (p=0.024). Further, post hoc pairwise comparison showed a significant difference between medicine-pharmacy (p< 0.001), and dentistry-medicine (p=0.009), for professional identity, and medicine-pharmacy (p=0.020) for the total RIPLS score.
Conclusion: A high readiness score among students offers the possibility of conducting IPE modules. A favorable attitude can be considered by curriculum planners while initiating IPE sessions.
Keywords: dental, interprofessional education, medical, pharmacy, teamwork, United Arab Emirates
Introduction
Healthcare is undergoing rapid changes, highlighting the need for the healthcare system to reform, unite and extend. The primary mission of members of the health care system is to provide effective and safe health services. This mission has several dimensions, including medications, procedures, patients, and other healthcare team members. Physicians, Dentists, and Pharmacists are vital members of the healthcare system, who work to deliver the best health outcome for patients. Alignment in practice between these professions is crucial to attaining the goals of the health system.
Inter-Professional Education (IPE) is expected to occur when “members of two or more professions learn with, from and about one another to improve collaboration and the quality of care”.1 Organizations such as the World Health Organization (WHO) has acknowledged the need for IPE and collaboration between healthcare professionals to improve health worldwide.2
Rapid changes in health care along with the increase in the complexity of patient illness underline the need for innovative strategies in teaching, learning, attitude, mentality, and behavior in the health professions. Several organizations including the WHO and accreditation agencies have advocated, developed, and updated guidelines for IPE. For example, in 2016, the Interprofessional Education Collaborative (IPEC) updated the accreditation standards across health subjects in the core curriculum and emphasized IPE.3,4 The Accreditation Council for Graduate Medical Education (ACGME) in the United States also supports IPE in practice, simulations, and team collaboration as a core component for postgraduate medical training.5,6
Pharmacists play an important role in IPE and interprofessional collaboration (IPC). Over the last few decades, there have been significant changes in the pharmacy profession. The profession shifted from being a compounder of pharmaceutical products to an information provider, and eventually to a comprehensive patient care provider.7 The transition in the role of the pharmacist, from traditional medication compounding and dispensing toward clinical services, increases the opportunity for IPC between physicians, pharmacists, nurses and other health professions.8,9 With a growing healthcare system team-based collaboration in learning and practice is of key importance for optimizing patient care and health outcomes.10,11 Patients with complex illnesses need different high-functioning professionals to coordinate and collaborate as a team.
Achieving IPC will have a significant impact on the pharmacy profession by clarifying professional boundaries and their function in the healthcare system.12,13 Team decision-making is of great importance, as it allows each team member to contribute their opinions, expertise, and decisions in patient care. This will create a better understanding of other health professions, negotiate conflict if any and create respect and better communication amongst professionals.14
Several studies reported, pharmacy students and other non-medical students, usually felt discomfort and were not confident to discuss or express their opinions and saw themselves as not equal to medical students. This may be due to the limited knowledge and understanding by each profession about the clinical knowledge and expertise of the other.15 This lack of knowledge, affects the recognition of each profession’s potential and contribution towards a better health care system and patient care, causing awkwardness, ineffectiveness, and conflict.16 This lack of collaboration may lead to medical errors, especially when members of the health care system are hesitant to express their opinions, or beliefs about the medical care of the patient. In one study, pharmacy students showed a higher need for professional cooperation and collaboration than medical students.17
There are several challenges with IPE implementation. The American Association of Colleges of Pharmacy (AACP) is recognizing these challenges, especially in experiential settings. Some of these challenges are scheduling conflicts between the team, lack of administrative support, and insufficient support for IPE. In the Middle East, interprofessional education and collaboration is uncommon. Unfortunately, there is previous evidence of negative stereotyping and beliefs towards non-physicians18 in Kuwait19 and the United Arab Emirates (UAE).20 Whilst IPE is yet to be integrated in the health care curriculum, it is foreseen to grow in the coming years. Several countries such as Qatar,21 UAE,20 and Egypt22 initiated research on the feasibility of IPE. IPE has been progressively encouraged in pharmacy and medical schools internationally.23 There are only a limited number of studies on IPE conducted in the UAE and its neighboring countries. One UAE IPE study constructed in alignment with the Situated Learning Theory principle, among students from medicine, pharmacy, nursing, and physiotherapy disciplines showed an increase in the readiness among students to engage in teamwork.24
Understanding the readiness of students can be valuable in knowing their willingness and is an important first step prior to incorporating IPE in the curricula. A higher level of readiness can be considered a positive factor toward IPE implementation. Further, studying student readiness among different subgroups according to demographic characteristics can provide valuable information on groups with varying levels of readiness and thus offer scope for strategies such as conducting sensitization sessions, webinars, etc for different groups.
In addition, the understanding and knowledge of the receptiveness of interdisciplinary learning and collaboration amongst healthcare students is of great importance to the UAE, a country yearning for the best teaching-learning strategies, especially in relation to the healthcare system.
Objectives
This study was aimed at assessing the readiness among medical, dental, and pharmacy students towards interprofessional education, and to study the association, if any, between the readiness and demographic profile of students at a UAE university.
Materials and Methods
Study Design
This research is a cross-sectional questionnaire-based exploratory study conducted among medical, dental, and pharmacy students at Ajman University, UAE. This university admits students to various health and non-health related disciplines. The health-related courses offered by the university are medical, dental and pharmacy. IPE is still not included in the curricula of the health profession students.
Ethical Approval
The institutional ethical committee at Ajman University approved the study on 20/11/2021 with reference number P-H-S-2022-1-1. Prior to the administration of the questionnaires, the intentions of the survey were explained to the respondents. All the guidelines stated by the ethical approving body were strictly followed.
Study Respondents
Two hundred and fifteen students from the pharmacy, medicine, and dentistry faculties of Ajman University were included using convenience sampling method. Criteria for inclusion in this study was being older than 18 years, studying for the included professions and consenting to participate.
Informed Consent
The respondents provided consent online prior to participation in the research. In addition, the preliminary section of the survey had a paragraph on informed consent and respondent’s freedom to participate or decline the survey.
Sampling Method and Technique
This research followed a population sampling method in which every students eligible and willing to respond the survey were included during 25th November 2021 to 11th February 2022.
Sample Size Calculation
The sample size calculated using Raosoft sample size calculator25 with a 5% margin of error, 95% CI, 50% response distribution, and a population size of 1150, was 289. The calculated sample size of 289 was targeted. However, the authors were able to obtain response only from 215 respondents with a response rate of 74.39%.
Data Collection Instrument
The standard Readiness for Interprofessional Learning Scale (RIPLS) Questionnaire26 was used in the study as the data collection tool. The RIPLS has three subscales with a total of 19 items: The first 9 items were related to “teamwork and collaboration”, 10–16 related to “professional identity”, and 17–19 related to “roles and responsibilities”. Respondents were asked to score between 1–5 (1= strongly disagree with the statement, 2= disagree, 3 = undecided, 4 = agree and 5 = strongly agree) based on their degree of agreement. The minimum and maximum possible scores were 19 and 95 respectively. Higher the score, the greater the readiness for IPE.
Study Tool Validation
The questionnaire has been standardized and widely used all over the world. Authors adopted it for this research due to its ease in administration and free availability. This tool has been used by previous researchers in UAE.27 In addition, authors checked the Cronbach alpha of all the completed responses (n=215) and found it to be 0.834 suggesting a good level of internal consistency.
Data Collection Method
The responses were collected during the final exams of all three professional students (pharmacy, dentistry, and medicine) after explaining the intentions of the study. The student assistants distributed the online questionnaire via Google form and it was also sent through WhatsApp and Airdrop as during the COVID-19 pandemic, questionnaires could not be distributed physically for safety reasons.
Data Analysis
The filled questionnaire data were transferred to SPSS Version 26 and the data were verified and cleaned for any irregularities. The SPSS data were then checked for the normality of distribution using one sample-KS test which showed a non-normal distribution The total scores and subscores were compared among different subgroups of respondents. And hence nonparametric tests (Mann–Whitney U-test for variables with two subgroups of respondents and Kruskal Wallis test for variables with more than two subgroups) were used at alpha =0.05.
Results
A total of 215 students responded to the survey. Table 1 shows the respondents’ demographic characteristics.
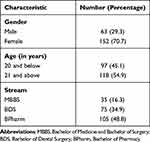 |
Table 1 Demographic Characteristics of Respondents (n =215) |
Comparison of Respondents’ Total Scores with Demographic Characteristics
The details of comparison of total scores and domain-specific scores (teamwork and collaboration, professional identity, and roles and responsibilities) with respondents’ demography are listed in Table 2. Significant differences were seen only in the case of the educational stream with professional identity score (p<0.001) and the total score (p=0.024). A further post hoc analysis using the Bonferroni-Dunn test showed a p-value of 0.001 between medicine-pharmacy students, and 0.009 for dentistry-medicine, for professional identity, suggesting the respondents’ professional identity has a strong influence on the readiness to practice IPE. The total score was significantly different between MBBS and BPharm students (p=0.020).
 |
Table 2 Median Subscale and Total Scores According to Demographic Characteristics of Respondents |
Student Responses to Individual Statements in RIPLS
Overall, the respondents were in favor of and willing for IPE sessions. The median score was 5 (maximum score) for 12 of the 19 statements. The IQR scores for those statements with median score 5 were 4–5. A low median score of 2 was seen for two of the statements “I am not sure what my professional role will be” and “Clinical problem solving can only be learnt effectively with students from my own school”.
Discussion
Currently, healthcare is moving towards patient-centeredness.28 Patient-centeredness offers multiple benefits such as self-care by patients, better physical and mental health, improved treatment, lower healthcare cost, patient dignity,29 and enhanced reputation of health workers among patients.30 Patient-centered healthcare can be implemented only with teamwork and collaboration among healthcare workers. Teamwork and interprofessional collaboration among healthcare workers can reduce errors and provide optimal treatment with adequate resource utilization and minimized cost.31 Studies in the Gulf Cooperation Council (GCC) countries document lack of interprofessional collaboration among health workers.32–34 Considering that healthcare is becoming more technical and patients with complicated illnesses are increasing, there is a need to promote a culture of collaboration among health workers to solve complex patient issues. This can be successfully incorporated while they are students. During the current era of information sharing and exposure, it is expected that healthcare students will be knowledgeable about the importance of IPE. Overall, the study finding showed students to be in favor of IPE and demonstrated a high readiness to practice interprofessional collaboration, like other studies reported elsewhere.35–38
Considering that healthcare organizations are currently focusing on equity, diversity, and inclusion39 it is important to explore the role of the gender gap on interprofessional collaboration. In a study, the authors argued that poor teamwork and collaboration was a major contributing factor to surgical complications and assessed how gender affects interprofessional practice in the operating room. The authors found gender to play a major role in shaping interactions within and between professional groups in the operating room.40 In the present study, overall females had a higher score (not statistically significant) than males. A comparison of the present study with a similar study conducted in Saudi Arabia among multiple undergraduate health programs showed a higher total score and teamwork and collaboration scores among females.41 Similar observations were noted in a Swiss study as well.42 Thus, females can be considered to be more willing for teamwork and collaboration.
In the present study, students aged above 20 years had a slightly lower total score. A similar observation was noticed in a study from Nepal.43 There is a possibility that with increasing age and year of study students are more exposed to the hierarchical system in healthcare affecting their readiness to learn and practice IPE. In a Saudi Arabian study, junior students had a better score compared to senior ones (70.1vs 67.6).41 Similar observations were noted in a Swiss study as well,42 wherein pre-clinical medical students showed more positive attitudes toward IPE. At this point, it is worth mentioning that, often the medical doctor is considered the leader of the healthcare team and s/he may not appreciate the importance of IPE. However, in the present study, on the contrary, MBBS students scored high on professional identity and total score. This finding is a positive one. Another study from Saudi Arabia also had similar findings wherein medical students showed a positive perception and were ready to adopt IPE activities in medical schools.44 Thus, it is obvious that over time after the students enter the healthcare system they are influenced by the hierarchical system and hence IPE at an early stage of their career may overcome this issue.
An in-depth analysis of individual statements showed a better preparedness among responding students. A high score was obtained for the statement “learning with other students will make a more effective member of a healthcare and social care team”. It is important that each student understand the strengths and weakness of their own and of other professions on topics related to patient care. For example, a medical doctor requires pharmacists for drug-related information, a nurse for supportive care, a laboratory technologist for patient laboratory data, etc. It is important for each student to appreciate the strengths and limitations of their professions. This understanding can facilitate and improve willingness to collaborate in the future for better patient care. In the UAE there have been sessions on IPE conducted in medical schools during case presentations.45
There was also a high score for the statement “patient would ultimately benefit if professionals work together”. As reported in the literature, teamwork and collaboration offers many advantages in improving patient care. At this point in time, it is worth stressing the fact that students are ready for IPE though such a practice is still largely lacking. Thus, the problem may be in delivering IPE and not at the student level. Delivering IPE sessions is linked to multiple challenges. However, a recent study from UAE reported that students are willing for IPE and reported positive outcomes in terms of students’ willingness to engage in inter-disciplinary learning and collaboration.27
As reported in this research, students perceived team working skills to be vital for all healthcare students. These skills can be developed through IPE as reported by Shrader et al46 wherein the authors found that community-based IPE could help health professional students develop their skills in collaborative practice. Other authors found that communication gaps due to lack of confidence, contrasting ways of thinking affecting communication in decision-making, and the hierarchical leadership culture in the health services were the main barriers to teamwork and collaboration among midwifery and nursing students. Mutual trust and respect are crucial in healthcare.47 In the present study, students agreed that “for small group learning to work, there should be trust among students”. Students also agreed that “shared learning will help them understand their own professional limitations” which is an important aspect of patient care. In today’s healthcare scenario, it is impossible for a single professional to manage a highly complicated patient. Thus, it is important for each professional to know their limitations and their strengths so that they can take help from other professionals in the healthcare team when needed. In an UAE study, there was no interprofessional collaboration among community pharmacists and physicians.48
Students also agreed that shared learning and practice would help them clarify the nature of patients’ problems which is a welcome finding. Further, they also agreed that shared learning will help them think positively about other health professions (Statement 8). In today’s healthcare settings often, professionals experience conflict which can threaten quality healthcare.43 IPE sessions on conflict management can be helpful to offer future professionals the means to avoid and deal with conflicts.
In order to successfully implement IPE sessions, they should be student-friendly, assessed, part of the curriculum, and scheduled at a time convenient to students and faculty members. There are multiple ways to offer IPE sessions. In the UAE, one institution conducts IPE case discussions wherein students from medical, dental, pharmacy, nursing, and other allied health professionals collectively present a single patient case and discuss their areas of expertise.45,49 This could be an easier approach to initiate IPE in UAE institutions.
Limitations
A low sample size can be considered a limitation of this research. As participation was voluntary it is possible more students with a positive attitude toward IPE may have participated. In addition, evaluating the differences toward interprofessional education of freshmen or junior students and higher-level or senior students could have been useful.
Recommendations
Based on the research findings the authors would like to recommend the initiation of IPE sessions for health profession students at the university. To begin with, IPE can be started with simple case presentations, and preferably should be offered at an early stage in the curriculum. Over a period of time IPE should be made mandatory and a part of every health professional curriculum. More in-depth research is needed to identify the barriers associated with the implementation of IPE sessions. Measures should be taken to further strengthen students’ positive perception toward and readiness for IPE. Students who have a low readiness should be identified and sensitization sessions conducted for them prior to enrolling them in IPE programs.
Conclusion
The current study reported a high IPE readiness among healthcare students suggesting their willingness toward IPE. This can be a positive aspect to be considered by curriculum planners while initiating IPE sessions. Effective measures to introduce IPE can offer students the ability to learn from and appreciate other professionals which eventually can pave the way for a culture of teamwork and collaboration during their future career.
Abbreviations
MBBS, Bachelor of Medicine, Bachelor of Surgery; BDS, Bachelor of Dentistry; BPharm, Bachelor of Pharmacy; IPE, Interprofessional education; UAE, United Arab Emirates; IPEC, Interprofessional Education Collaborative; ACGME, The Accreditation Council for Graduate Medical Education; IPC, Interprofessional Collaborative; AACP, The American Association of Colleges of Pharmacy; GCC, Gulf Cooperation Council; IQR, Interquartile range; RIPLS, Readiness for Interprofessional Learning Scale.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author (Subish Palaian) on reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was granted by the Research Ethics Committee of Ajman University on 20/11/2021 with reference number P-H-S-2022-1-1.
Acknowledgments
Authors would like to acknowledge the BPharm students Toleen Mohammad Nasereddin Hidari and Miar Sabri Moustafa Mohamed Elghamri for their help in collecting the study response. Authors would also like to thank Ajman University for partially paying the processing fee.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Barr H, Low H. Principles of Interprofessional Education. London: CAIPE; 2011.
2. WHO (World Health Organization). Framework for Action on Interprofessional Education and Collaborative Practice. World Health Organization; 2010.
3. Liaison Committee on Medical Education. Functions and Structure of a Medical School. Standards for accreditation of medical education programs lading to the MD degree. Available from: https://lcme.org/publications/.
4. Accreditation Council for Pharmacy Education. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Available from: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf.
5. Martinez-Strengel A, Balasuriya L, Black A, et al. Perspectives of internal medicine residency program directors on the accreditation council for graduate medical education (ACGME) diversity standards. J Gen Intern Med. 2021;36(9):2539–2546. doi:10.1007/s11606-021-06825-2
6. Nevin CR, Westfall AO, Martin Rodriguez J, et al. Gamification as a tool for enhancing graduate medical education. Postgrad Med J. 2014;90(1070):685–693. doi:10.1136/postgradmedj-2013-132486
7. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543. doi:10.1093/ajhp/47.3.533
8. Bazaldua O, Ables AZ, Dickerson LM, et al. Suggested guidelines for pharmacotherapy curricula in family medicine residency training: recommendations from the society of teachers of family medicine group on pharmacotherapy. Fam Med. 2005;37(2):15.
9. Wolfe ME, Moeller KE, Woods B. Medical students’ perceptions on the role of pharmacists. J Pharm Pract. 2018;31(6):623–628. doi:10.1177/0897190017734764
10. Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes (Review) SUMMARY OF FINDINGS FOR THE MAIN COMPARISON. Cochrane Libr. 2017;2017(6):125.
11. Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;2017(6). doi:10.1002/14651858.CD000072.pub3
12. Shrader S, Hummel H, Byrd L, Wiley K. An introprofessional geriatric medication activity within a senior mentor program. Am J Pharm Educ. 2013;77(1):15. doi:10.5688/ajpe77115
13. Van Winkle LJ, Bjork BC, Chandar N, et al. Interprofessional workshop to improve mutual understanding between pharmacy and medical students. Am J Pharm Educ. 2012;76(8):150. doi:10.5688/ajpe768150
14. Kanter MH, Nguyen M, Klau MH, Spiegel NH, Ambrosini VL. What does professionalism mean to the physician? Perm J. 2013;17(3):87–90. doi:10.7812/TPP/12-120
15. Gillespie U, Mörlin C, Hammarlund-Udenaes M, Hedström M. Perceived value of ward-based pharmacists from the perspective of physicians and nurses. Int J Clin Pharm. 2012;34(1):127–135. doi:10.1007/s11096-011-9603-1
16. Brown J, Lewis L, Ellis K, Stewart M, Freeman TR, Kasperski MJ. Conflict on interprofessional primary health care teams can it be resolved? J Interprof Care. 2011;25(1):4–10. doi:10.3109/13561820.2010.497750
17. Lehrer MD, Murray S, Benzar R, et al. Peer-led problem-based learning in interprofessional education of health professions students. Med Educ Online. 2015;20(1):28851. doi:10.3402/meo.v20.28851
18. Champion V, Austin J, Tzeng OC. Cross-cultural comparison of images of nurses and physicians. Int Nurs Rev. 1987;34(2):43–48.
19. Meleis AI. A model for establishment of educational programmes in developing countries: the nursing paradoxes in Kuwait. J Adv Nurs. 1980;5(3):285–300. doi:10.1111/j.1365-2648.1980.tb03353.x
20. El-Zubeir M, Rizk DEE, Al-Khalil RK. Are senior UAE medical and nursing students ready for interprofessional learning? Validating the RIPL scale in a Middle Eastern context. J Interprof Care. 2006;20(6):619–632. doi:10.1080/13561820600895952
21. Johnson B, Pyburn R, Bolan C, et al. Qatar Interprofessional Health Council: IPE for Qatar. Avicenna. 2011;2011(1). doi:10.5339/avi.2011.2
22. Hosny S, Kamel MH, El-Wazir Y, Gilbert J. Integrating interprofessional education in community-based learning activities: case study. Med Teach. 2013;35(SUPPL. 1):S68–S73. doi:10.3109/0142159X.2013.765550
23. Van Winkle LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2011;75(9):178. doi:10.5688/ajpe759178
24. Zaher S, Otaki F, Zary N, Amina Al Marzouqi RR. Effect of introducing interprofessional education concept on students of various healthcare discipline in the United Arab Emirates. medRxiv. 2021. doi:10.1101/2021.04.02.21254859
25. Raosoft I. Sample size calculator by Raosoft, Inc. 2020.
26. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ. 1999;33(2):95–100. doi:10.1046/j.1365-2923.1999.00298.x
27. Zaher S, Otaki F, Zary N, Al Marzouqi ARR, Radhakrishnan R. Effect of introducing interprofessional education concepts on students of various healthcare disciplines: a pre-post study in the United Arab Emirates. BMC Med Educ. 2022;22(1):517. doi:10.1186/s12909-022-03571-9
28. Abdulrahman Mohammed Al M, Zakiuddin A, Abdullah MA. Paradigm shift in healthcare through technology and patient-centeredness. Int Arch Public Health Commun Med. 2018;2(1). doi:10.23937/iaphcm-2017/1710015
29. Ulin K, Malm D, Nygårdh A. What is known about the benefits of patient-centered care in patients with heart failure. Curr Heart Fail Rep. 2015;12(6):350–359. doi:10.1007/s11897-015-0272-6
30. Schmid S, Schlosser S, Gülow K, Pavel V, Müller M, Kratzer A. Interprofessional collaboration between ICU physicians, staff nurses, and hospital pharmacists optimizes antimicrobial treatment and improves quality of care and economic outcome. Antibiotics. 2022;11(3):381. doi:10.3390/antibiotics11030381
31. Huber C. Interprofessional collaboration in health care. Praxis. 2022;111(1). doi:10.1024/1661-8157/a003808
32. El-Awaisi A, Wilby KJ, Wilbur K, El Hajj MS, Awaisu A, Paravattil B. A Middle Eastern journey of integrating Interprofessional Education into the healthcare curriculum: a SWOC analysis. BMC Med Educ. 2017;17(1). doi:10.1186/s12909-016-0852-5
33. El-Awaisi A, Saffouh El Hajj M, Joseph S, Diack L. Interprofessional education in the Arabic-speaking Middle East: perspectives of pharmacy academics. J Interprof Care. 2016;30(6):769–776. doi:10.1080/13561820.2016.1218830
34. AlSayegh A, Enayah S, Khoja W, Enayah R, Sendi N. Assessment of the current knowledge and willingness to conduct medical research work of future healthcare providers: a cross-sectional study in Jeddah, Saudi Arabia. J Fam Med Prim Care. 2020;9(3). doi:10.4103/jfmpc.jfmpc_1047_19
35. Ogawara H, Hayashi T, Asakawa Y, et al. Interprofessional education initiatives at gunma university: simulated interprofessional training for students of various health science professions. In: Advanced Initiatives in Interprofessional Education in Japan. Japan Interprofessional Working and Education Network; 2010. doi:10.1007/978-4-431-98076-6_10
36. Ahmad MI, Chan SWC, Wong LL, Tan ML, Liaw SY. Are first-year healthcare undergraduates at an Asian university ready for interprofessional education? J Interprof Care. 2013;27(4):341–343. doi:10.3109/13561820.2013.769094
37. Carlisle C, Taing MW. Interprofessional education between dentistry and pharmacy students: delivery, barriers and facilitating implementation. Aust Dent J. 2021;66(4):351–357. doi:10.1111/adj.12856
38. Winship JM, Falls K, Gregory M, et al. A case study in rapid adaptation of interprofessional education and remote visits during COVID-19. J Interprof Care. 2020;34(5):702–705. doi:10.1080/13561820.2020.1807921
39. Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359. doi:10.1136/bmj.j4366
40. Etherington C, Kitto S, Burns JK, et al. How gender shapes interprofessional teamwork in the operating room: a qualitative secondary analysis. BMC Health Serv Res. 2021;21(1). doi:10.1186/s12913-021-07403-2
41. Alruwaili A, Mumenah N, Alharthy N, Othman F. Students’ readiness for and perception of Interprofessional learning: a cross-sectional study. BMC Med Educ. 2020;20(1). doi:10.1186/s12909-020-02325-9
42. Berger-Estilita J, Chiang H, Stricker D, Fuchs A, Greif R, McAleer S. Attitudes of medical students towards interprofessional education: a mixed methods study. PLoS One. 2020;15:e0240835. doi:10.1371/journal.pone.0240835
43. Ramsay MAE. Conflict in the health care workplace. Baylor Univ Med Cent Proc. 2001;14(2). doi:10.1080/08998280.2001.11927749
44. Alzamil H, Meo SA. Medical students’ readiness and perceptions about interprofessional education: a cross sectional study. Pak J Med Sci. 2020;36(4). doi:10.12669/pjms.36.4.2214
45. GMU. Inter-Professional educ act. Available from: https://gmu.ac.ae/com_news/inter-professional-education-activity/.
46. Shrader S, Kern D, Zoller J, Blue A. Interprofessional teamwork skills as predictors of clinical outcomes in a simulated healthcare setting. J Allied Health. 2013;42(1):547.
47. ACADEMY HEALTH. Building trust and mutual respect to improve health care. Available from: https://academyhealth.org/about/programs/building-trust-and-mutual-respect-improve-health-care.
48. Palaian S, Buabeid M, Ashames A. Patient safety culture in handling prescriptions and interprofessional collaboration practices amongst community pharmacists: an investigative simulated patient study from the United Arab Emirates. Risk Manag Healthc Policy. 2020;13:3201–3209. doi:10.2147/RMHP.S282571
49. GMU. GMU PHARMD-MBBS interprofessional education in medication management. Available from: https://gmu.ac.ae/cop_news/gmu-pharmd-mbbs-interprofessional-education-in-medication-management/.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
