Back to Journals » Journal of Pain Research » Volume 16
Race, Ethnicity, and Sustained Opioid Use After Major Abdominal Surgery for Cancer
Authors Owusu-Agyemang P , Feng L , Cata JP
Received 19 July 2023
Accepted for publication 30 October 2023
Published 7 November 2023 Volume 2023:16 Pages 3759—3774
DOI https://doi.org/10.2147/JPR.S427411
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ellen M Soffin
Pascal Owusu-Agyemang,1,2 Lei Feng,3 Juan P Cata1,2
1Department of Anesthesiology and Perioperative Medicine, University of Texas MD Anderson Cancer Center, Houston, TX, USA; 2Anesthesiology and Surgical Oncology Research Group, Houston, TX, USA; 3Department of Biostatistics, University of Texas MD Anderson Cancer Center, Houston, TX, USA
Correspondence: Pascal Owusu-Agyemang, Department of Anesthesiology and Perioperative Medicine, the University of Texas MD Anderson Cancer Center, 1515 Holcombe Boulevard, Unit 0401, Houston, TX, 77030, USA, Tel + 1 832 465 8964, Email [email protected]
Purpose: Sustained opioid use is a well-known complication after surgery. Our objective was to determine whether there is any association between a patient’s race or ethnicity and the sustained use of opioids in the year following surgery. Opioid use over the initial 3, 6, and 12 postoperative months was categorized as “sustained early”, persistent, and chronic, respectively.
Patients and Methods: Single-institution retrospective study of adults (≥ 18 years) who had undergone open abdominal surgery for cancer. Multivariable logistic regression was used to evaluate the association between race/ethnicity and opioid use.
Results: Of the 3523 patients included in the study, 2543 (72.2%) were non-Hispanic (NH) White, 476 (13.5%) were Hispanic or Latino, 262 (7.4%) were NH-Black, 186 (5.3%) were Asian, and 56 (1.6%) belonged to other racial or ethnic groups. The overall rates of sustained early, persistent, and chronic opioid use were 15.9%, 7.1%, and 2.6%, respectively. In the multivariable analysis, patient race/ethnicity was associated with sustained early postoperative opioid use (p-value=0.037), with Hispanics/Latinos having significantly higher odds than NH-Whites (OR = 1.382 [95% CI: 1.057– 1.808]; p = 0.018). However, neither persistent nor chronic opioid use was associated with race/ethnicity (p = 0.697 and p = 0.443, respectively).
Conclusion: In this retrospective study of adults who had undergone open abdominal surgery, patient race/ethnicity was not consistently associated with the development of sustained opioid use over the first 12 postoperative months.
Keywords: race, ethnicity, persistent, chronic, opioids, cancer
Introduction
Pain continues to be one of the most common and debilitating symptoms of cancer.1 Recent estimates suggest 30% to 50% of cancer patients experience pain, with 30.6% experiencing pain of a moderate-to-severe nature.2,3 Furthermore, an estimated 33% to 40% of cancer survivors are known to experience chronic pain.4
Despite the availability of analgesic options, opioids have remained a cornerstone for the treatment of moderate-to-severe pain in cancer patients.5 However, opioid-related adverse effects have been shown to negatively impact the quality of life of cancer patients and survivors.6 Particularly concerning is the development of persistent or chronic opioid use, which may not only prolong the disabling adverse effects of opioids but also increase the risk of death related to overdose.7–9 In a retrospective study of 19,219 adults who had undergone curative-intent cancer surgery, patients who developed new persistent opioid use had more than twice the risk of opioid overdose compared to non-opioid users.10
Some studies, albeit in patients undergoing non-oncological surgery, have shown an association between patient race or ethnicity and persistent opioid use. Examples include a retrospective study of 1656 patients who had undergone upper extremity surgery, where White race was associated with lesser odds of persistent opioid use,11 and other studies where Black race was associated with higher odds of persistent opioid use after hysterectomy,12 cardiothoracic surgery,13 and spine surgery.14 In addition, race-dependent polymorphisms of the CYP2D6 and mu-opioid receptor genes have been associated with variable potency of some commonly prescribed opioids in NH-Blacks and decreased pain sensitivity among NH-Whites, respectively.15,16 To date, the interaction between patient race or ethnicity and persistent or chronic opioid use in the surgical oncology patient population is unclear. An assessment of this risk may be considered important since it may help inform prevention strategies and reduce the risk of complications related to persistent opioid use.
In addition, other factors including adjuvant chemotherapy, type of surgery, and alcohol abuse have been shown to be associated with long-term opioid use.17–19 In other studies, the use of epidural analgesia during major abdominal surgery has been shown to reduce short-term incisional pain.20–23 However, its effect on the occurrence of persistent or chronic opioid use after cancer-related surgery is less clear.21
To that end, we conducted a single-institution retrospective study of adults who had undergone open-abdominal surgical procedures, with the primary objective of comparing the rates of early sustained, persistent, and chronic opioid use between patients of different races or ethnicities. Our hypothesis was that the rates of opioid use would be similar across racial/ethnic groups. For our secondary objectives, we sought to evaluate the impacts of adjuvant chemotherapy, type of surgery, alcohol abuse, smoking history, and epidural analgesia on the occurrence of sustained opioid use.
Materials and Methods
This study was approved by the Institutional Review Board (IRB) of the University of Texas MD Anderson Cancer Center on September 27, 2021 (IRB # 2021–0738). Due to the retrospective nature of this study, written informed consent was not required. The data accessed complied with relevant data protection and privacy regulations. Extracted study variables were stored on the Research Electronic Data Capture web platform hosted by the University of Texas MD Anderson Cancer Center. Our findings are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.24
Patient Selection Process
We used a dataset from our previous publication on race, ethnicity, and the use of regional anesthesia in patients who had undergone surgical procedures between March 1, 2016, and August 1, 2021.25 Unlike our previous publication where patients who had used opioids prior to surgery we included, the patient selection process in this current study (Figure 1) was designed to include only those patients who had undergone open abdominal surgical procedures and had not reported any opioid use within three months of the index surgical procedure. Previously established exclusion criteria including patients of American Society of Anesthesiologists Physical Status (ASA PS) 4 and above, those undergoing emergency, laparoscopic, robotic, minimally invasive, and outpatient procedures were maintained. In addition, patients with missing data on their race and ethnicity were excluded from the current study. To avoid over-representation of individual patients, only data related to their index admission for open abdominal surgery was included.
 |
Figure 1 STROBE Flow diagram of the patient selection process. |
Anesthetic Management
At our institution, the anesthetic management of patients undergoing open abdominal surgery is not standardized. However, a typical regimen consists of the preoperative administration of celecoxib, tramadol, acetaminophen, and midazolam, followed by volatile-based general anesthesia with a regional block.
The decision to use regional anesthesia is largely influenced by the extensiveness of the surgical procedure to be performed. These types of regional anesthesia include thoracic epidural analgesia or bilateral subcostal transversus abdominis plane with quadratus lumborum blocks. For less extensive procedures, local anesthetic infiltration of the incision is performed by the surgeon. Fentanyl, hydromorphone, and intravenous acetaminophen are commonly administered during surgery, and the use of opioid-free anesthesia is rare.
The institutional post-anesthesia care unit (PACU) order-set, which is completed by the attending anesthesiologist, has options for the treatment of mild, moderate, and severe pain. Acetaminophen and methocarbamol are included in the options for managing mild pain, while varying dosages of fentanyl, morphine, and hydromorphone are used for the management of mild, moderate, or severe pain.
Exposure Variables
The primary exposure variable was a patient’s self-reported race or ethnicity. Accordingly, patients were divided into the following groups: Asian, Not-Hispanic or Latino (NH) Black, Hispanic or Latino, NH-White, and NH-Other. The group of NH-Other included patients who self-identified as follows: American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and those who self-identified as “Other race”.
The secondary exposure variables were the receipt of adjuvant chemotherapy up to 12 months following the date of surgery, the type of surgical procedure, alcohol abuse prior to the date of surgery, smoking history, and the use of epidural analgesia during surgery.
Outcome Measures
The primary outcome measures were sustained early postoperative opioid use, persistent opioid use, and chronic opioid use. Sustained early postoperative use of opioid was defined as self-reported opioid use during outpatient visits at 1 and 3 months after surgery. Based on previously used definitions, persistent opioid use was defined as self-reported opioid use during outpatient visits at 1, 3, and 6 months after surgery.26–29 Accordingly, chronic opioid use was defined as self-reported opioid use during outpatient visits at 1, 3, 6, and 12 months after surgery. Based on conversions used in the Centers for Disease Control Guideline for Prescribing Opioids for Pain, perioperative opioid administration was converted into morphine equivalent daily dose units (MEDD).30
Study Covariates
Baseline and perioperative variables extracted from subsections of the institutional data warehouse are summarized in Table 1. The following demographic and potentially confounding categorical variables were included in the analysis: Race/ethnicity, gender, American Society of Anesthesiologists Physical Status (ASA), history of anxiety/depression, alcohol abuse, smoking status, and cancer stage.
 |
Table 1 Baseline and Postoperative Characteristics of 3523 Adults Who Had Open Abdominal Surgery |
Additionally, the types of surgery, regional anesthesia, epidural analgesia, and the use of a truncal block were included in the analysis.
Continuous variables of body mass index (BMI), anesthesia duration, and total intraoperative opioid dose were also included. Immediate postoperative variables included total dose of opioids administered in the PACU. The occurrence of the following in the year following surgery was also assessed: additional surgery, adjuvant chemotherapy, and outpatient opioid use.
Statistical Methods
Patients’ demographics, treatment, and clinical outcomes were summarized through descriptive statistics. Wilcoxon rank sum test or Kruskal–Wallis test was used to compare location parameters of continuous distributions between or among patient groups. Chi-square test was used to evaluate the association between two categorical variables. A multivariable logistic regression model was fitted to estimate the effects of important covariates on opioid use after surgery. Statistical software SAS 9.4 (SAS, Cary, NC) was used for all the analyses.
Results
Of the 3523 patients included in the study, 2543 (72.2%) were non-Hispanic (NH) White, 476 (13.5%) were Hispanic or Latino, 262 (7.4%) were NH-Black, 186 (5.3%) were Asian, and 56 (1.6%) belonged to other racial or ethnic groups. The majority were male (55.3%), and the median age (interquartile range [IQR]) was 60 years (IQR, 50–69). The overall rates of sustained early, persistent, and chronic opioid use over the initial 3, 6, and 12 months were 15.9%, 7.1%, and 2.6%, respectively. Other baseline characteristics of the study population are shown in Table 1.
Among the baseline characteristics, age (p < 0.001), BMI (p < 0.001), anxiety/depression (p = 0.002), and smoking (p = 0.012) were significantly different across racial/ethnic groups. The types of surgeries undergone and the use of epidural analgesia also differed significantly across racial/ethnic groups (p = 0.021 and p = 0.006, respectively). With regard to epidural analgesia, the lowest rate of use (18.7%) was observed in the NH-Black patient population, and the highest rate (39.3%) was in patients of NH-Other race/ethnicity.
However, in the immediate postoperative period, a significantly higher proportion of PACU pain scores ≥ 7 was observed among patients of NH-Other race (p = 0.012). PACU opioid consumption varied significantly across racial/ethnic groups (p = 0.024), with the highest median dose observed in the group of NH-Black patients (p = 0.024).
After being discharged from the hospital, a larger proportion of NH-Black patients required additional surgery within 12 months of the original surgery date (p = 0.032).
Sustained Early Postoperative Opioid Use
Race/Ethnicity and Sustained Early Postoperative Opioid Use
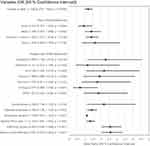
In the univariable analysis (Table 2), the rates of sustained early opioid use varied across racial/ethnic groups (p = 0.013), with the highest rate observed among patients of NH-Other race. With the adjustment of gender, surgery type, alcohol abuse, regional anesthesia with epidural, anesthesia duration, highest PACU pain score, any repeat surgery within the three previous months, and any adjuvant chemotherapy within the 3 months, the multivariable analysis (Figure 2) demonstrates a statistically significant association between the race/ethnicity variable and sustained early opioid use (p = 0.037).
 |
Table 2 Univariable Analysis of Factors Associated with Sustained Opioid Use After Open Abdominal Surgery for Cancer |
Within this association, Hispanic/Latino patients had 38% higher odds of sustained early opioid use than NH-White patients (odds ratio [OR] = 1.382; 95% confidence interval [CI] = 1.057 −1.808; p = 0.018).
Adjuvant Chemotherapy and Sustained Early Postoperative Opioid Use
In the univariable analysis (Table 2), the rates of sustained early postoperative use were higher in patients who had received adjuvant chemotherapy within the three-month period (32.3% versus 13.7%, p < 0.001). In the multivariable analysis (Figure 2), the receipt of adjuvant chemotherapy within the first three postoperative months was associated with a more than two-fold increase in the risk of developing sustained early postoperative opioid use (OR = 2.591; 95% CI = 2.010–3.340; p < 0.001).
Effect of Surgery Type on Sustained Early Postoperative Opioid Use
The rates of sustained early opioid use varied significantly across surgery types (p < 0.001), with the highest rate (21.1%) observed in patients who had undergone colorectal surgery. In the multivariable analysis (Figure 2), patients who had undergone colorectal (OR = 2.284; 95% CI = 1.155–4.517; p = 0.018) and gastrointestinal (OR = 2.183; 95% CI = 1.090–4.372; p = 0.028) surgeries had significantly higher odds of sustained early opioid use than those who had undergone peritoneal surface malignancy procedures.
Effect of Alcohol Abuse on Sustained Early Postoperative Opioid Use
Significantly higher rates of history of alcohol abuse (30.2% versus 15.6%, p = 0.004) were observed in the group of patients who subsequently developed sustained early postoperative opioid use. In the adjusted analysis (Figure 2), a documented history of alcohol abuse at the time of surgery was associated with a two-fold increase in the odds of developing sustained early opioid use (OR = 2.169; 95% CI = 1.139–4.130; p = 0.019).
Regional Anesthesia and Sustained Early Postoperative Opioid Use
The group of patients who received regional anesthesia had higher rates of sustained early postoperative opioid use than those who did not (17.6% versus 13.8%, p = 0.002). Among the types of regional anesthesia used, patients who received epidural analgesia had higher rates of sustained early postoperative opioid use than those who did not (21.7% versus 14.0%, p < 0.001).
After adjusting for gender, surgery type, alcohol abuse, regional anesthesia with epidural, anesthesia duration, highest PACU pain score, repeat surgery within the three previous months, and adjuvant chemotherapy within the 3 months, the multivariable analysis (Figure 2) demonstrates a 39.9% increase in the odds of developing sustained early opioid use in patients who received epidural analgesia during surgery (OR = 1.399; 95% CI = 1.129–1.734; p = 0.002).
Effect of Additional Factors
In the univariable analysis (Table 2), a significantly higher rate of anxiety/depression (18.5% versus 15.3%, p = 0.046) was observed in the group of patients with sustained early postoperative opioid use. In addition, the rate of sustained early opioid use varied by cancer stage (p = 0.024). Anesthesia duration (median [IQR]: 6.7 hr [4.8–9.4] versus 6.1 hr [4.3–8.2]; p < 0.001) and intraoperative opioid administration (median [IQR]: 30 MEDD [20–50], versus median 30 MEDD [20–46]; p = 0.001) were also comparatively longer in the group of patients with sustained early postoperative opioid use.
Of the postoperative characteristics, sustained early opioid use was associated with higher average PACU pain scores (median [IQR] 2.7 [1.2–4.1] versus median, 2.5 [1.3–3.7]; p = 0.029) and additional surgery within the three-month period (32.4% versus 13.3%, p < 0.001).
In the multivariable analysis (Figure 2), other factors that were independently associated with the development of sustained early opioid use included anesthesia duration (OR = 1.101; 95% CI = 1.066–1.137; p < 0.001), a peak PACU pain score > 7 (OR = 1.318; 95% CI = 1.087–1.597; p = 0.005), and repeat surgery within the 3-month period (OR = 2.563; 95% CI = 2.026–3.244; p < 0.001).
Persistent Opioid Use
Race/Ethnicity and Persistent Opioid Use
As shown in Table 2, the rates of persistent opioid use did not differ significantly across racial/ethnic groups (p = 0.071). With the adjustment of age, BMI, gender, anxiety/depression, alcohol abuse, regional anesthesia with epidural, anesthesia duration, PACU opioid dose, highest PACU pain score, repeat surgery within six months, and adjuvant chemotherapy within 6 months (Figure 3), the association between race/ethnicity and persistent opioid use was not significant (p = 0.696).
Adjuvant Chemotherapy and the Development of Persistent Opioid Use
Six months after surgery, a higher rate of persistent opioid use was observed in patients who had received adjuvant chemotherapy within the six-month period (20.9% versus 4.7%, p < 0.001). In the multivariable analysis (Figure 3), the receipt of adjuvant chemotherapy was associated with a more than five-fold increase in the odds of developing persistent opioid use (OR = 5.276; 95% CI = 3.663–7.600; p < 0.001).
Effect of Regional Anesthesia on the Development of Persistent Opioid Use
The group of patients who received regional analgesia had higher rates of persistent opioid use than those who did not (8.2% versus 5.7%, p = 0.004). Furthermore, the group of patients who received epidural analgesia had higher rates of persistent opioid use than those who did not (11.1% versus 5.7%, p < 0.001).
With the adjustment of age, BMI, gender, anxiety/depression, alcohol abuse, regional anesthesia with epidural, anesthesia duration, total PACU opioid dose, highest PACU pain, any repeat surgery within the six months, and adjuvant chemotherapy within the 6 months (Figure 3), the use of epidural analgesia was associated with a 58.1% increase in the odds of developing persistent opioid use (OR = 1.581; 95% CI = 1.035–2.416; p = 0.034).
Effects of Other Potentially Confounding Factors
In the unadjusted analysis (Table 2), the rates of persistent opioid use were higher in females (8.1% versus 6.3% in males, p = 0.039), patients with anxiety/depression (9.3% versus 6.6%, p = 0.015), alcohol abuse (17.0% versus 6.9%, p = 0.005), and in those with higher BMI (median [IQR], 29 [25–34] versus median 32 [24–32]; p = 0.027).
In addition, the incidence of persistent opioid use varied significantly across surgery types (p < 0.001) and cancer stage (p = 0.004) with higher rates observed among patients who underwent colorectal surgery, and in those with stage 3 cancer. Furthermore, higher rates of persistent opioid use were observed among patients with longer anesthesia duration (median [IQR] 7 hr [5–9] versus 6 hr [4–8]; p = 0.007), and in those who received more opioids intraoperatively (median [IQR] 34 MEDD [20–46] versus 30 MEDD [20–46]; p = 0.016).
In the immediate postoperative period, the group of patients with persistent opioid use had higher average PACU pain scores (median [IQR] 2.7 [1.4–4.2] versus median, 2.5 [IQR, 1.3–3.7]; p = 0.033).
Six months after surgery, higher rates of persistent opioid use were observed in patients who required additional surgery within the six-month period (14.8% versus 5.1%, p < 0.001).
In the adjusted model (Figure 3), increasing age (OR = 1.074; 95% CI = 1.004–1.148; p = 0.037), female gender (OR = 1.743; 95% CI = 1.229–2.471; p = 0.002), anesthesia duration (OR = 1.086; 95% CI =1.021–1.154; p = 0.008), and additional surgery within the 6-month period (OR = 2.293; 95% CI = 1.588–3.310; p < 0.001) were each associated with increased odds of developing persistent opioid use.
Chronic Opioid Use
Race/Ethnicity and Chronic Opioid Use
In the univariable analysis (Table 2), the rates of chronic opioid use were similar across racial/ethnic groups (p = 0.131). Figure 4 shows results of the multivariable logistic regression model that was fitted to estimate the effects of important covariates on chronic opioid use. The race/ethnicity variable was forced into the model since it was of interest. With the adjustment of BMI, gender, regional anesthesia with epidural, anesthesia duration, repeat surgery within the 12-month period, adjuvant chemotherapy within the 12-month period, the association between race/ethnicity and chronic opioid use was not significant (p = 0.443).
Effect of Adjuvant Chemotherapy on the Occurrence of Chronic Opioid Use
Patients who required adjuvant chemotherapy had higher rates of persistent opioid use than those who did not (8.6% versus 1.3%, p < 0.001). In the adjusted model (Figure 4), adjuvant chemotherapy within the 12-month period was associated with more than a six-fold increase in the odds of developing chronic opioid use (OR = 6.207; 95% CI = 3.985–9.666; p < 0.001).
Epidural Analgesia and Chronic Opioid Use
The group of patients who received epidural analgesia had higher rates of chronic opioid use than those who did not (4.1% versus 2.1%, p = 0.002). In the adjusted model (Figure 4), the receipt of epidural analgesia was associated with a 64.2% increase in the odds of developing chronic opioid use (OR = 1.642; 95% CI = 1.047–2.576; p = 0.031).
Effects of Other Potentially Confounding Factors
In the univariable analysis, the rate of chronic opioid was higher in females (3.2% versus 2.1% in males, p = 0.047) and varied significantly across surgery types (p = 0.022). Among surgery types, the highest rate was observed in patients who had undergone colorectal surgery (4.1%). In addition, rates of chronic opioid use were higher in patients who required additional surgery within the 12-month period (5.8% versus 1.4%, p < 0.001).
In the multivariable analysis (Figure 4), female gender (OR = 1.581; 95% CI = 1.031–2.424; p = 0.037) and additional surgery within the twelve-month period (OR = 2.944; 95% CI = 1.901–4.560; p < 0.001) were each associated with chronic opioid use.
Discussion
In this retrospective study of adults who had undergone open abdominal surgery for cancer, Hispanic/Latino patients had significantly higher odds of sustained early postoperative opioid use than NH-White patients. However, this association was not present 6 or 12 months after surgery.
Race/Ethnicity and Sustained Early Opioid Use
An explanation for the association between race/ethnicity and sustained early postoperative opioid use is not easily discernible from our data. Unfortunately, a lack of comparable studies further limits our ability to derive potential explanations. However, albeit in a study describing persistent opioid use, ours is not the first study to report a higher risk of continuous opioid use in Hispanic patients who had undergone open abdominal surgery. In a multicenter study of 1646 patients who had undergone colorectal surgery at affiliated medical centers in Massachusetts, compared to White patients, Hispanic patients had more than twice the risk of receiving a new opioid prescription between 90 and 180 days after discharge.31 A potential explanation for this significant finding was not provided by the authors. However, as suggested by previous research, it is possible that factors such as opioid prescribing patterns of primary care clinicians may have influenced our findings.27,32,33
In addition, some experimental studies suggest Hispanics/Latinos and NH-Blacks may have a lower threshold and lower tolerance for pain than NH-Whites.34–36 The underlying mechanisms for this may include a combination of cultural factors and polymorphisms of the CYP2D6 enzyme and mu-opioid receptor genes.15,16,33,36 The extent to which these findings translate into an increased risk of sustained opioid use is less clear, especially since opioid use may be influenced by factors such as the aforementioned prescribing patterns, socio-cultural factors, and the type of health insurance.27,32,37,38
Other large-scale studies involving primarily non-surgical cancer patients have reported differing associations between race/ethnicity and persistent opioid use. For example, in a large retrospective study of 106,732 veteran cancer survivors, White race was independently associated with increased odds of having filled 120 days’ or greater supply or 10 or more opioid prescriptions from 1 to 2 years after the start of curative treatment.39 However, using the same definition of persistent opioid use, another large observational study of 33,872 older (>65 years) cancer patients who were undergoing definitive treatment did not find an association between race/ethnicity and persistent opioid use.40 These differences in findings may suggest that associations between race/ethnicity and persistent or chronic opioid use may, at best, be useful in informing local or regional practice patterns and must be used with caution when applied more broadly.
With regard to our study, the inconsistent nature of our results and the literature showing that Hispanic Americans are less likely to consult a physician for acute or chronic pain makes it plausible that our association between race/ethnicity and sustained early postoperative opioid use may have been a spurious finding.41,42
Importance of Adjuvant Chemotherapy
Similar to the findings of previous studies, adjuvant chemotherapy was consistently associated with the development of sustained opioid use in our study population. In another retrospective study of 68,463 patients who underwent curative-intent cancer surgery, patients who received adjuvant chemotherapy had a significantly higher risk of new persistent opioid use across all procedures.17 This observation raises the question as to whether the timing of adjuvant therapies should be considered in the definitions of persistent opioid use after cancer surgery. The most common definition of persistent opioid use relies on the observation that acute post-surgical pain usually resolves within 3 months.43 However, the duration of recovery from acute surgical pain varies for different procedures and may be difficult to define in patients who receive adjuvant chemotherapy, which may result in neuropathic injury in addition to the mechanical injury associated with surgery.
It has been shown that chemotherapy-induced peripheral neuropathy occurs in approximately 20% of patients who receive standard doses of chemotherapy and in almost 100% of patients treated with high doses.44 This may perhaps explain why the need for adjuvant chemotherapy was consistently associated with sustained opioid use in our study population.
Effect of Surgery Type on the Occurrence of Sustained Early Opioid Use
As would be expected, undergoing additional surgery was associated with an increased risk for early sustained, persistent, and chronic opioid use. Notably, among the surgical procedures included in our study, patients who had undergone colorectal and gastrointestinal procedures had significantly higher odds of sustained early postoperative opioid use compared to those who had surgery for peritoneal surface malignancy. A similar observation was made by Bicket and colleagues, where compared to patients who had undergone urologic procedures, patients who had undergone colorectal surgery had significantly higher odds of persistent opioid use.18 It is possible that the requirement for ostomies and their reversal may have influenced this finding.
Epidural Analgesia and Sustained Opioid Use
Compared to systemic opioids, the use of epidural analgesia has been associated with superior acute pain control after a various surgical procedures.45 However, contrary to what might have been expected, the use of epidural analgesia in our patient population was consistently associated with an increased risk for developing sustained opioid use. The currently available literature does not provide clear evidence that perioperative epidural analgesia reduces the risk for chronic post-surgical pain.45 Several studies have suggested no clear advantage of epidural analgesia over intravenous opioid analgesia in the prevention of chronic post-surgical pain after major abdominal and thoracic surgery procedures,21–23 while others have reported it to be inferior.20
With regard to our study, we speculate that our findings may be confounded by the fact that epidural analgesia is more frequently used for very extensive procedures such as pelvic exenterations, abdominoperineal resections, and cytoreductive surgery.
Alcohol Abuse, Acute Pain, Age, Gender, and Anesthesia Duration
Confirming previous literature, alcohol abuse,17 acute pain of severe intensity,46 increasing age,12 and female gender were associated with the development of early sustained, persistent, or chronic opioid use.13 Furthermore, longer anesthesia duration was associated with sustained early and persistent opioid use. We speculate that similar to the findings of a large retrospective study of opioid naïve patients who had undergone surgery, larger opioid prescription size after more extensive procedures may have placed this group of patients at higher risk for persistent opioid use.47
Study Limitations
This study is not without its limitations. Firstly, the inherent biases and inaccuracies associated with the retrospective nature of our study may have prevented us from accurately identifying our study endpoints. In addition, the inclusion of multiple surgical procedures may have prevented us from identifying the interaction of race/ethnicity with persistent opioid use after individual surgical procedures. Furthermore, the heterogeneity and low sample size of certain sub-groups may have resulted in significant underpowering.
Conclusions
In this retrospective study of 3523 patients who had undergone open abdominal surgery for cancer, the association between race/ethnicity and opioid use over the first 12 postsurgical months was inconsistent. Further studies are needed to clearly define whether there is any association between a patient’s race or ethnicity and their risk of developing persistent or chronic opioid use.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ng JY, Sharma AE. Guidelines for Cancer-Related Pain: a Systematic Review of Complementary and Alternative Medicine Recommendations. Pain Pract. 2021;21(4):454–467. doi:10.1111/papr.12964
2. Snijders RAH, Brom L, Theunissen M, et al. Update on Prevalence of Pain in Patients with Cancer 2022: a Systematic Literature Review and Meta-Analysis. Cancers. 2023;15(3). doi:10.3390/cancers15030591
3. Dalal S, Bruera E. Pain Management for Patients With Advanced Cancer in the Opioid Epidemic Era. Am Soc Clin Oncol Educ Book. 2019;39(39):24–35. doi:10.1200/EDBK_100020
4. Bennett MI, Kaasa S, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic cancer-related pain. Pain. 2019;160(1):38–44. doi:10.1097/j.pain.0000000000001363
5. Jackson LK, Imam SN, Braun UK. Opioids in Cancer Pain: right or Privilege? J Oncol Pract. 2017;13(9):e809–e814. doi:10.1200/JOP.2016.019216
6. Wiffen PJ, Wee B, Derry S, et al. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7(7):Cd012592. doi:10.1002/14651858.CD012592.pub2
7. Paice JA, Von Roenn JH. Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol. 2014;32(16):1721–1726. doi:10.1200/JCO.2013.52.5196
8. Lillemoe HA, Newhook TE, Vreeland TJ, et al. Educating Surgical Oncology Providers on Perioperative Opioid Use: results of a Departmental Survey on Perceptions of Opioid Needs and Prescribing Habits. Ann Surg Oncol. 2019;26(7):2011–2018. doi:10.1245/s10434-019-07321-y
9. Newhook TE, Vreeland TJ, Dewhurst WL, et al. Opioid-prescribing Practices After Oncologic Surgery: opportunities for Improvement and a Call to Action. Ann Surg. 2020;271(2):e9–e10. doi:10.1097/SLA.0000000000003595
10. Lin N, Dabas E, Quan ML, et al. Outcomes and Healthcare Utilization Among New Persistent Opioid Users and Non-opioid Users After Curative-intent Surgery for Cancer. Ann Surg. 2023;277(4):e752–e758. doi:10.1097/SLA.0000000000005109
11. Giladi AM, Shipp MM, Sanghavi KK, et al. Patient-Reported Data Augment Health Record Data for Prediction Models of Persistent Opioid Use after Elective Upper Extremity Surgery. Plast Reconstr Surg. 2023;152(2):358e–366e. doi:10.1097/PRS.0000000000010297
12. Swenson CW, Kamdar NS, Seiler K, et al. Definition development and prevalence of new persistent opioid use following hysterectomy. Am J Obstet Gynecol. 2018;219(5):486.e1–486.e7. doi:10.1016/j.ajog.2018.06.010
13. Brescia AA, Waljee JF, Hu HM, et al. Impact of Prescribing on New Persistent Opioid Use After Cardiothoracic Surgery. Ann Thorac Surg. 2019;108(4):1107–1113. doi:10.1016/j.athoracsur.2019.06.019
14. Davison MA, Lilly DT, Desai SA, et al. Racial Differences in Perioperative Opioid Utilization in Lumbar Decompression and Fusion Surgery for Symptomatic Lumbar Stenosis or Spondylolisthesis. Global Spine J. 2020;10(2):160–168. doi:10.1177/2192568219850092
15. Smith HS. Opioid metabolism. Mayo Clin Proc. 2009;84(7):613–624. doi:10.1016/S0025-6196(11)60750-7
16. Hastie BA, Riley JL 3rd, Kaplan L, et al. Ethnicity interacts with the OPRM1 gene in experimental pain sensitivity. Pain. 2012;153(8):1610–1619. doi:10.1016/j.pain.2012.03.022
17. Lee JS, Hu HM, Edelman AL, et al. New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. J Clin Oncol. 2017;JCO2017741363.
18. Bicket MC, Murimi IB, Mansour O, et al. Association of new opioid continuation with surgical specialty and type in the United States. Am J Surg. 2019;218(5):818–827. doi:10.1016/j.amjsurg.2019.04.010
19. Dev R, Parsons HA, Palla S, et al. Undocumented alcoholism and its correlation with tobacco and illegal drug use in advanced cancer patients. Cancer. 2011;117(19):4551–4556. doi:10.1002/cncr.26082
20. Lavand’homme P, De Kock M, Waterloos H. Intraoperative epidural analgesia combined with ketamine provides effective preventive analgesia in patients undergoing major digestive surgery. Anesthesiology. 2005;103(4):813–820. doi:10.1097/00000542-200510000-00020
21. Fassoulaki A, Chassiakos D, Melemeni A. Intermittent epidural vs continuous wound infusion of ropivacaine for acute and chronic pain control after hysterectomy or myomectomy: a randomized controlled trial. Pain Med. 2014;15(9):1603–1608. doi:10.1111/pme.12523
22. Jensen MK, Andersen C. Can chronic poststernotomy pain after cardiac valve replacement be reduced using thoracic epidural analgesia? Acta Anaesthesiol Scand. 2004;48(7):871–874. doi:10.1111/j.0001-5172.2004.00437.x
23. Ho SC, Royse CF, Royse AG, et al. Persistent pain after cardiac surgery: an audit of high thoracic epidural and primary opioid analgesia therapies. Anesth Analg. 2002;95(4):820–823. doi:10.1213/00000539-200210000-00006
24. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–804. doi:10.1097/EDE.0b013e3181577654
25. Owusu-Agyemang P, Feng L, Porche VH, et al. Race, ethnicity, and the use of regional anesthesia in cancer patients undergoing open abdominal surgery: a single-center retrospective cohort study. Front Med. 2022;9:950444. doi:10.3389/fmed.2022.950444
26. Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017;152(6):e170504. doi:10.1001/jamasurg.2017.0504
27. Delaney LD, Waljee JF. New persistent opioid use: definitions and opportunities. Reg Anesth Pain Med. 2021;46(2):97–98. doi:10.1136/rapm-2020-102121
28. Johnson A, Milne B, Jamali N, et al. Chronic opioid use after joint replacement surgery in seniors is associated with increased healthcare utilization and costs: a historical cohort study. Can J Anaesth. 2022;69(8):963–973. doi:10.1007/s12630-022-02240-1
29. Sun EC, Darnall BD, Baker LC, et al. Incidence of and Risk Factors for Chronic Opioid Use Among Opioid-Naive Patients in the Postoperative Period. JAMA Intern Med. 2016;176(9):1286–1293. doi:10.1001/jamainternmed.2016.3298
30. Dowell D, Ragan KR, Jones CM, et al. CDC Clinical Practice Guideline for Prescribing Opioids for Pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. doi:10.15585/mmwr.rr7103a1
31. Cavallaro PM, Fields AC, Bleday R, et al. A multi-center analysis of cumulative inpatient opioid use in colorectal surgery patients. Am J Surg. 2020;220(5):1160–1166. doi:10.1016/j.amjsurg.2020.06.038
32. Delaney LD, Gunaseelan V, Rieck H, et al. High-Risk Prescribing Increases Rates of New Persistent Opioid Use in Total Hip Arthroplasty Patients. J Arthroplasty. 2020;35(9):2472–2479.e2. doi:10.1016/j.arth.2020.04.019
33. Campbell CM, Edwards RR. Ethnic differences in pain and pain management. Pain Manag. 2012;2(3):219–230. doi:10.2217/pmt.12.7
34. Rahim-Williams FB, Riley JL 3rd, Herrera D, et al. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. Pain. 2007;129(1–2):177–184. doi:10.1016/j.pain.2006.12.016
35. Lawlis GF, Achterberg J, Kenner L, et al. Ethnic and sex differences in response to clinical and induced pain in chronic spinal pain patients. Spine. 1984;9(7):751–754. doi:10.1097/00007632-198410000-00017
36. Rahim-Williams B, Riley JL, Williams AK, et al. A quantitative review of ethnic group differences in experimental pain response: do biology, psychology, and culture matter? Pain Med. 2012;13(4):522–540. doi:10.1111/j.1526-4637.2012.01336.x
37. Jiang X, Orton M, Feng R, et al. Chronic Opioid Usage in Surgical Patients in a Large Academic Center. Ann Surg. 2017;265(4):722–727. doi:10.1097/SLA.0000000000001780
38. Breuler CJ, Shabet C, Delaney LD, et al. Prescribed Opioid Dosages, Payer Type, and Self-Reported Outcomes After Surgical Procedures in Michigan, 2018-2020. JAMA Netw Open. 2023;6(7):e2322581. doi:10.1001/jamanetworkopen.2023.22581
39. Vitzthum LK, Riviere P, Sheridan P, et al. Predicting Persistent Opioid Use, Abuse, and Toxicity Among Cancer Survivors. J Natl Cancer Inst. 2020;112(7):720–727. doi:10.1093/jnci/djz200
40. Vitzthum LK, Nalawade V, Riviere P, et al. Racial, Ethnic, and Socioeconomic Discrepancies in Opioid Prescriptions Among Older Patients With Cancer. JCO Oncol Pract. 2021;17(6):e703–e713. doi:10.1200/OP.20.00773
41. Ell K, Haywood LJ, deGuzman M, et al. Differential perceptions, behaviors, and motivations among African Americans, Latinos, and whites suspected of heart attacks in two hospital populations. J Assoc Acad Minor Phys. 1995;6(2):60–69.
42. Portenoy RK, Ugarte C, Fuller I, et al. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004;5(6):317–328. doi:10.1016/j.jpain.2004.05.005
43. Schug SA, Lavand’homme P, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain. 2019;160(1):45–52. doi:10.1097/j.pain.0000000000001413
44. Park HJ. Chemotherapy induced peripheral neuropathic pain. Korean J Anesthesiol. 2014;67(1):4–7. doi:10.4097/kjae.2014.67.1.4
45. Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesth Analg. 2007;104(3):689–702. doi:10.1213/01.ane.0000255040.71600.41
46. Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11(12):1859–1871. doi:10.1111/j.1526-4637.2010.00983.x
47. Howard R, Brown CS, Lai YL, et al. Postoperative Opioid Prescribing and New Persistent Opioid Use: the Risk of Excessive Prescribing. Ann Surg. 2022.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.