Back to Journals » Psychology Research and Behavior Management » Volume 16
Psychological Status, Influencing Factors and Intervention Countermeasures of Hospital Pharmacists in Extreme Working Environments in the Post-Pandemic Era--An Embedded Mixed Study
Authors Yang X , Wen L, Zheng J, Nie H, Liu S, Chen C, Si F, Zhang X, Kang J, Du S, Yin Z
Received 26 July 2023
Accepted for publication 30 November 2023
Published 19 December 2023 Volume 2023:16 Pages 5089—5100
DOI https://doi.org/10.2147/PRBM.S431825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Xi Yang,1 Linlin Wen,1 Jinqian Zheng,1 Huijuan Nie,1 Shengli Liu,1 Chengqun Chen,1 Fangying Si,1 Xiaojian Zhang,1,2 Jian Kang,1,2 Shuzhang Du,1 Zhao Yin1
1Department of Pharmacy, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 2Henan Drug Clinical Comprehensive Evaluation Center, Zhengzhou, People’s Republic of China
Correspondence: Zhao Yin; Shuzhang Du, Email [email protected]; [email protected]
Objective: The study explores the psychological state and related influences of hospital pharmacists enclosed in extreme work environments in the post-epidemic era, and also explores potential measures to alleviate negative emotions.
Methods: An embedded mixed research methodology was used. In the qualitative research phase, semi-structured interviews were carried out with 30 pharmacists consistently confined to their work environments. The data were managed and analyzed using NVivo12 software. In the quantitative research phase, 146 pharmacists with experience in extreme work environments were selected, and the data were collected through questionnaires (GAD-7 and CD-RISC-25) and self-administered questions generated during the qualitative phase. The Shapiro–Wilk test was utilized to assess data normality. Spearman correlation was conducted to evaluate correlations among self-designed questions, resilience, and anxiety.
Results: The results from interviews with 30 pharmacists revealed four factors influencing the psychological state of pharmacists in the post-epidemic era: personal factors, interpersonal relationships, environmental factors, and policy and public opinion. Mitigation measures for negative emotions encompass material security, life adjustment, epidemic prevention policy, public opinion information, and organizational management. The results of a quantitative study of 146 pharmacists showed that only 1% had severe anxiety, but the psychological resilience scores were generally low, and 62% had poor psychological resilience, with scores below 73. Simultaneously, it was observed that, except religious beliefs, factors influencing psychological status in extreme work environments were significantly negatively correlated with personal anxiety levels and significantly positively correlated with psychological resilience.
Conclusion: Our study holds significance in unraveling the psychological aspects of pharmacists as healthcare workers. It also offers insights into how healthcare organizations respond to the negative emotions experienced by healthcare workers in emergencies or extreme environments.
Keywords: mixed study, hospital pharmacists, post-pandemic era, psychological state
Introduction
COVID-19 has been around for three years globally, and its impact on us has been widespread and persistent.1 In a survey of 204 countries, it was found that in the early stages of the COVID-19 epidemic, an increase in the prevalence of severe anxiety and depression correlated with an increase in the prevalence of the virus and a decrease in population mobility.2 Over time, governments responded to the new crown outbreak with a range of measures, including restrictions on the movement of people, closure of offline educational institutions, appropriate public distances, restrictions on dine-in restaurants, and the construction of COVID-19-specific wards and hospitals.3–6 For quite some time, the epidemic was significantly contained globally, however, new problems ensued. In the post-epidemic era, mass quarantine seems to have hurt people’s working lives as much as the epidemic itself, with closed environments leading to economic downturns and reduced incomes.7,8 Meanwhile, segregation reduces interpersonal communication to some extent, which affects people’s mental health in various ways.1,8,9
In the early stages of COVID-19 (primarily referring to a time from the outbreak to the end of 20206,10–12), the mental health of medical staff garnered widespread attention, with approximately one-third of medical staff experiencing anxiety, depression, and stress.11 However, in the post-epidemic era (primarily referring to the latter half of 2021 and beyond8,13–15), there is a general lack of attention to the mental health levels and the factors influencing them among healthcare workers, especially pharmacists. As an integral part of the healthcare system, pharmacists played a crucial role in responding to COVID-19. They were involved in tasks such as drafting guidelines for pharmacists and pharmacies on professional services, establishing an emergency medication list, monitoring and resolving medication shortages, providing telemedicine services, delivering education on infection prevention and disease management, and participating in clinical trials and medication evaluations.16,17 The occurrence of psychological problems can directly impact daily work, negatively affecting the attention, cognitive functioning, and clinical decision-making of healthcare professionals. This can increase the incidence of medical errors and accidents, posing risks to patients.18 Therefore, attention to the mental health of pharmacists is particularly important in the post-epidemic era.
After initially bringing the outbreak under control, China entered a phase of normalized prevention and control, with localized outbreaks still occurring from time to time. The impact of various government measures on the daily lives and mental health of the population cannot be ignored. In the second half of 2022, China’s megacities with populations of more than 10 million people, such as Zhengzhou, Wuhan, and Xi’an, were severely affected by the epidemic. In Zhengzhou, the government implemented rigorous closure and control measures to effectively address the spread of the epidemic. Additionally, numerous communities adopted a management approach, wherein residents were instructed not to leave their homes.19 Simultaneously, in response to the epidemic control policy, hospital pharmacists experienced tens of consecutive days working on-site,20 during which they did not leave and were completely confined to the work environment. This situation presented an unprecedented challenge for all pharmacists in their careers. Scholars have not yet delved into the psychological state and influencing factors, including potential interventions, of this group in the post-epidemic era and under extreme working environments. Our study explores the process of changes in the psychological state of pharmacists since the outbreak of the epidemic in 2019 to the present day through a mixed research methodology. The influencing factors and potential intervention countermeasures for the psychological state of pharmacists in the extreme work environment in the post-epidemic era were also examined. Additionally, the correlation between the influencing factors and the level of psychological well-being was explored through a quantitative study. This research aims to offer valuable insights into how healthcare organizations can effectively cope with negative emotions among their staff in emergency or extreme environments.
Methods
A mixed research methodology with an embedded design was used to explore the influences and potential interventions on the psychological state of hospital pharmacists in extreme work environments and to validate the correlation between the influences and the level of psychological well-being. First, focus group interviews with pharmacists in extreme work environments were conducted to explore the process of changes in pharmacists’ psychological states since the 2019 outbreak to the present day. Factors affecting psychological states and possible interventions were collected through the interviews. Second, several self-defined questions were formulated based on the insights gained from the interviews. Third, pharmacists with experience working in closed environments were selected from multiple hospitals. The quantitative approach was employed to investigate the correlations between factors influencing psychological states and the levels of psychological resilience and anxiety among the selected pharmacists. The steps of the study are shown in Figure 1.
 |
Figure 1 Research methodology. |
Ethics Approval
The present study received approval from the Ethics Committee at The First Affiliated Hospital of Zhengzhou University (Approval No. 2022-KY-0735). Written informed consent forms, including permission for the publication of anonymized responses, were signed by all participants. Our study adheres to the principles outlined in the Declaration of Helsinki.
Participants
Inclusion criteria: ① Voluntary participation in this study.② Worked in the hospital pharmacy department for at least 1 year.③ Have a continuous work experience of more than 3 days of closed work in the hospital.
Instruments
Anxiety
Anxiety was measured using the 7‐item Generalized Anxiety Disorder Scale (GAD‐7), a well-validated tool that sums 7 questions to screen and diagnose generalized anxiety disorder21 with 4-point responses ranging from 0 (not at all) to 3 (nearly every day) in clinical practice and research, that are summed to yield a total score ranging from 0 to 21.22 The total score of anxiety was interpreted as normal (0–4), mild (5–9), moderate (10–14), and severe (15–21) anxiety. Respondents with a GAD-7 total score ≥10 were classified as screening positive for anxiety.22
Resilience
The Chinese version of the Connor-Davidson Resilience Scale (CD-RISC-25) was used to evaluate individual resilience, designed by Connor KM and Davidson JR23 and translated by Yu et al.24 This valid and reliable scale comprises 25 items rated on a five-point Likert scale from 0 (not true at all) to 4 (true all the time). The total score of the scale ranges from 0 to 100, with a higher score indicating higher resilience. The lowest quartile scores ranged from 0 to 73; the second lowest quartile scores ranged from 74 to 82, followed by the third quartile scores from 83 to 90, and the fourth quartile scores from 91 to 100.23,25
Data Collection
Qualitative Data
For the qualitative survey, purposeful sampling was used to obtain participants that represented the spectrum of respondent characteristics. All interviews were conducted face-to-face. Following informed consent, focus group discussions were conducted by one researcher and recorded by another. An interview topic guide (see Supplementary Figure 1) was piloted in an interview. Data saturation was reached after interviewing 7 focus group discussions. All interviews completed by November 21, 2022. Data saturation was defined as “no new themes or codes emerging from interviews”.
Quantitative Data
The online survey was implemented using the online platform Questionnaire Star (Changsha Ranxing Information Technology Co., Ltd), a widely used free online questionnaire platform in China. Our online questionnaire included six main sections: a letter of invitation to participate in the study, a consent form, a demographic form, 11 self-designed questions (corresponding to the multi-dimensional influencing factors extracted in the qualitative study), the Chinese version of the CD-RISC-25 and the GAD-7. The self-designed questions were developed specifically for use in this study and were based on findings from the qualitative study. The online questionnaire survey was distributed by researchers via questionnaire star QR code or link to their social media platforms, and the participants voluntarily filled in the questionnaire after reading the informed consent form. The online questionnaire was completed from December 2022 to February 2023.
Analysis
For qualitative study, interview data were analyzed using a thematic analysis approach, which is a method for identifying, analyzing, and reporting patterns within data that is widely used in qualitative research. The key steps of thematic analysis include familiarization with the data, generating initial codes, searching and reviewing themes, naming themes, and producing the final report.26 Within 24 hours after the interview, the interview data were transcribed verbatim by one researcher and checked by two other researchers. After confirming that the transcriptions were correct, two researchers independently completed the extraction of the codes and wrote the first draft of the themes and subthemes. Subsequently, the research group discussed the first draft of the themes and subthemes and proposed comments and suggestions for theme structure and language expression. Under the guidance of a senior research expert, the research team compared and analyzed all differences and established the final themes and subthemes. The final themes and subthemes were developed with the agreement of the research group and appropriate representative quotes were selected to present the themes or subthemes. In the process described above, NVivo12 software was used to manage and analyze the data. The Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (see Supplementary Table 1) was followed for the qualitative reporting.27
For the quantitative study, the online survey responses were exported from Questionnaire Star into an Excel file (Excel version 2016; Microsoft Corp., Redmond, WA, USA). Data was then cleaned, coded, and analyzed using IBM SPSS® (Armonk, NY, USA) statistics software version 26. For demographic data, the measurement data were expressed as Mean ± Standard, and the count data were expressed as percentages. A total score for the CD-RISC-25 and the GAD-7 was calculated for each participant by summing the individual item scores respectively. The Shapiro–Wilk test was used to assess data normality. Then, Spearman correlation was conducted to assess correlations between self-designed questions, resilience, and anxiety. All statistical tests were two-tailed, and p-values < 0.05, and p-values < 0.01 were considered statistically significant.
Results
Demographic Characteristics
The first phase of the qualitative study had 30 participants with an average age of 35 years, 66.67% female, and an average work experience of 10.48 years. The second phase of the quantitative study had 146 participants with a mean age of 36 years, 61.64% female, and a mean work experience of 12.34 years. The demographics are shown in Table 1.
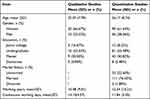 |
Table 1 Demographic Characteristics of Pharmacists Involved in Qualitative and Quantitative Studies |
Qualitative Results
The results of the qualitative study were divided into three parts: pharmacists’ psychological state and current status since the 2019 outbreak, factors influencing pharmacists’ psychological state in extreme work environments, and countermeasures against negative psychological states in extreme work environments.
Part I: Psychological states of pharmacists since the 2019 outbreak
Since the outbreak of the epidemic in 2019, most respondents reported that their psychological state had experienced initial panic, gradual adaptation in the middle, and helplessness and fear about mass quarantine in the later stages (the themes, subthemes, and representative quotations are shown in Table 2).
 |
Table 2 Psychological States of Pharmacists Since the 2019 Outbreak |
Part II: Factors influencing the psychological state of pharmacists in extreme work environments
The results of our interviews show that in extreme work environments, pharmacists’ psychological state is influenced by four main sources: personal factors, interpersonal relationships, environmental factors, and policy and public opinion (the themes, subthemes, and representative quotations are shown in Table 3).
 |
Table 3 Factors Influencing the Psychological State of Pharmacists in Extreme Working Environment |
Theme 1: Personal factors
Interviewees indicated that their personality, hobbies, personal experiences, and religious beliefs would have an impact on their psychological state in extreme work environments. A cheerful and optimistic personality, clear personal hobbies, rich personal experiences, and altruism could help pharmacists better adapt to extreme work environments.
Theme 2: Interpersonal relationships
The influence of interpersonal relationships refers to the psychological impact of the respondent’s state of being with those around him or her. This includes the influence of the respondent’s coworkers, family members, and pets. It was found that the support and understanding of family members, having someone to share the corresponding work in the family, friendly exchanges between coworkers, and mutual understanding and tolerance in extreme work environments all had a positive impact on the psychological state of extreme work environments. On the other hand, the lack of care for young children at home, the fear of family illness, the sense of guilt towards family members, the lack of care and feeding of pets at home for those who live alone, and the friction and disputes among coworkers due to trivial matters in life during the period of closed work hurt the psychological state.
Theme 3: Environmental factors
Environmental factors refer to the influence of family environment, work environment, and community environment. Respondents indicated that a harmonious family environment, adequate supplies at work, leadership care, and understanding of medical workers by community members all positively influence psychological status. Inadequate infrastructure in the work environment, lack of workflow and contingency plans to cope with extreme work environments, lack of protection mechanisms for employees, and external disapproval and inability to ensure nucleic acid collection negatively influenced psychological status.
Theme 4: Policy and Public Opinion
In this outbreak, the lack of information transparency, the lack of reports related to the outbreak leading to more rumors, the lack of uniformity in epidemic prevention policies in neighboring communities, the rapid change of policies, and the emphasis on closure, all of these hurt the psychological state of pharmacists.
Part III: Coping measures for the negative mental state in the extreme working environment
In the interviews, the interviewees also gave some countermeasures against the negative psychological state, including five aspects: material security, life adjustment, epidemic prevention policy, public opinion information, and organizational management (see Table 4).
 |
Table 4 Coping Measures for Negative Mental State in Extreme Working Environment |
Quantitative Results
In the quantitative part of the study, we distilled the influencing factors obtained in the first part of the qualitative study into 11 questions (see Supplementary Figure 2), assigning a score of 1–5 to the answer to each question, respectively. We also used the Generalized Anxiety Disorder Scale (GAD-7) (7 items) and the Psychological Resilience Inventory (Connor-Davidson, CD-RISC) (25 items) by a web-based questionnaire to investigate the mental health status of hospital pharmacists. Based on the results of previous qualitative studies, the correlation between potential influencing factors and the level of mental health was explored.
We found that after experiencing an extreme work environment, 52% of the 146 hospital pharmacists who participated in the quantitative study had no anxiety, 41% had mild anxiety, and 6% and 1% had moderate or severe anxiety respectively. 62% of the pharmacists had poor psychological resilience, with scores of 73 or less; 17% had scores of 74–82; 9% had scores of 83–90; and 12% of pharmacists showed high psychological resilience, with scores between 91–100 (see Supplementary Figure 3a and Supplementary Figure 3b). Also, we found that, except for religious beliefs, the factors influencing psychological state in extreme work environments were significantly negatively correlated with personal anxiety levels and significantly positively correlated with psychological resilience (see Table 5).
 |
Table 5 Correlation of Influencing Factors with Anxiety and Psychological Resilience |
Among the 11 questions related to influencing factors, we observed that respondents who were in good physical condition and naturally optimistic were more likely to exhibit higher levels of psychological resilience and were less prone to anxiety. Of the respondents, 75.34% agreed with the notion that they were in good physical condition and could effectively handle the physiological impacts of the epidemic. Additionally, 58.90% reported feeling naturally optimistic. Moreover, when subjected to extreme working conditions, the support and understanding of family and friends, harmonious relationships with colleagues, and a comfortable family atmosphere and working environment were found to positively influence one’s psychological well-being. Lastly, concerning the general epidemic prevention environment, we discovered significant correlations between the scientific nature of epidemic prevention policies and the positivity of public opinion information with individuals’ psychological states. In the online questionnaires we collected, only 39.73% of the respondents believed that current epidemic prevention measures were sufficiently scientific, and just 30.14% felt that public opinion during the epidemic was filled with positive energy (see Supplementary Table 2).
This section explored the mental health of pharmacists in extreme working environments. Based on the influencing factors from the qualitative study, the correlation between the factors influencing pharmacists’ psychological state and their level of mental health in extreme working environments was further explored (see Figure 2).
 |
Figure 2 The connections between anxiety, resilience and negative or positive factors. |
Discussion
This study was conducted during the latter phase of the COVID-19 outbreak. Despite the epidemic persisting for nearly three years, its ongoing impact on individuals remains evident. Although most countries worldwide have been open to the control of the epidemic, the Chinese government still insisted on orderly control in the late stage of the epidemic. In October 2022, Zhengzhou, China, experienced severe repercussions from the epidemic. Due to policy restrictions, medical workers have to remain confined to their workplaces for dozens of days. Following the conclusion of the closure and control measures, we conducted this study to investigate the influencing factors and propose improvement measures for the psychological well-being of hospital pharmacists working in extreme conditions during the post-epidemic era. This research holds significant public health implications.
Our findings show that in the early stage of the outbreak, people’s panic and anxiety mainly came from the unknown of the virus and the worry about their health status. In the middle stage of the outbreak, with the introduction of a series of anti-epidemic and anti-disease policies by the governments of various countries, the spread of the virus was effectively controlled, and the public’s mindset gradually stabilized. As a result, they were full of confidence in overcoming the virus. In the late stage of the outbreak, people were no longer anxious about the outbreak itself, but more anxious and helpless because of the lack of supplies, stagnation of work, and economic recession brought about by the large-scale quarantine. Our findings were consistent with previous studies. In the meta-analysis by Wu et al, the risk of anxiety and depression for those who had experienced a blockade or quarantine was 1.38 and 1.74 times higher than that of those who had not experienced a blockade or quarantine.9 During the COVID-19 pandemic, the risk of anxiety and depression was higher in the quarantined population than in the general population. Cheng’s findings also suggest that the prevalence of anxiety or depression was higher in the quarantined population during the SARS epidemic.1
In the special context of the post-epidemic era, we explored the factors influencing the psychological state of pharmacists in extreme work environments. It was found that the personal factors of pharmacists were one of the influencing factors of psychological state in extreme working environments, including their personalities, preferences, living habits, physical conditions, and religious beliefs. Several interviewees indicated that good physical condition and an optimistic personality could effectively circumvent negative emotions, and Atiah H. Almalki et al found that their chronic diseases were one of the factors of anxiety susceptibility among pharmacists,28 which was similar to the results of our study one. In addition, people with specific hobbies were more likely to have positive emotions in extreme work environments, and immersing oneself in something one enjoys gave one relaxation and a release from negative emotions. It is worth noting that the environment is also capable of acting on personal attributes and influencing them in some way,29,30 and this dynamic relationship between personal attributes and the environment also plays an important role in pharmacists’ mental health. The findings of the present study revealed that the environment and people surrounding hospital pharmacists were another important influence on psychological state. Including the influence of coworkers, family members, pets, etc., and the influence of the work environment, family environment, and community environment, radiating to a wider scope. The respondents of this study also indicated that the government’s relevant policies on epidemic prevention and control and the orientation of public opinion would affect the psychological state. For most married women, closed to their work environment and unable to go out, the greatest concern is whether the younger children at home can adapt to the absence of their mothers, thus giving rise to a sense of guilt towards the family. For people who live alone, enclosed in their workplace, and unable to go outside, the availability of water and food for their pets at home is a concern. In a study by Hashem A. Kilani et al, it was noted that the government restricts travel and enforces daily isolation at home, which had become a concern for many people around the world and greatly affected their mental health.31 At the same time, the interviewees indicated that the lack of accurate official reports on the development of the epidemic during the period of closed work and the uncertainty about the length of the closed work period also had a greater negative impact on the psychological state.
In response to the influences obtained in the first phase of the qualitative study, we explored the correlation between these influences and pharmacists’ psychological resilience and anxiety levels subsequently. We selected 146 pharmacists with closed work experience and used the CD-RISK-25 scale and the GAD-7 scale to look at their psychological resilience levels and anxiety levels, and found that 52% of the participants had no anxiety, 41% had mild anxiety, and only 7% had moderately severe anxiety. However, regarding the generally low scores on the psychological resilience test, with 62% of the participants having poor psychological resilience, this is because anxiety levels are influenced by factors other than psychological resilience levels.32,33 Meanwhile, before this closure, the outbreak had lasted for nearly three years, and the public’s attitude towards the outbreak had gradually transitioned from initial panic and anxiety to a state of adaptation, acceptance, or numbness, and thus the level of anxiety had been alleviated to a certain extent compared with that at the beginning of the outbreak. However, during the three years of the outbreak, most people experienced repeated government closures and controls, which have somewhat depleted the inner strength of individuals to overcome adversity, and to some extent reduced the public’s psychological resilience.34,35 We further validated the correlations of the factors influencing the psychological state obtained in the first stage with psychological resilience and anxiety level, and the results confirmed that, except religiosity, the other factors were significantly positively and significantly negatively correlated with psychological resilience and anxiety state, respectively, which may be attributed to the relatively low proportion of pharmacists with religiosity among the interviewees.
We also paid attention to the interventions to cope with the negative psychological state under extreme working environment, including adequate material security, regular work and rest, development of personal hobbies, optimization of epidemic prevention policy, and development of workflow, etc. It is suggested that in our daily work, we need to construct corresponding workflow and emergency plan to cope with the public health emergencies, including the reserve and security of the material base, to maximize the security under extreme. Meanwhile, we need to build appropriate work processes and emergency programs to cope with public health emergencies, including material reserves and protection, to maximize the protection of pharmacists in extreme work environments, to better adapt to and complete their work properly, and to avoid errors. The study also concluded that good communication between coworkers and family members could greatly alleviate negative emotions. This is similar to the findings of Zhi Ye et al’s investigation of the psychological state of Chinese university students during the epidemic, which concluded that communities, schools, and families need to pay more attention to the physical and mental health of individuals.36 Family members are the closest and best resource for help during isolation and should support each other with close, open, and timely communication.
Conclusion
Our study focused on the psychological state of pharmacists in the extreme working environment in the post-epidemic era, which provided a reference for how to ensure the good psychological state of healthcare workers during sudden emergencies in the future.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cheng SK, Wong CW, Tsang J, et al. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol Med. 2004;34(7):1187–1195. doi:10.1017/S0033291704002272
2. Santomauro DF, Mantilla Herrera AM, Shadid J. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312)):1700–1712. doi:10.1016/S0140-6736(21)02143-7
3. Wu Q, Li D, Yan M, et al. Mental health status of medical staff in Xinjiang province of China based on the normalisation of COVID-19 epidemic prevention and control. Int J Disaster Risk Reduct. 2022;74:102928. doi:10.1016/j.ijdrr.2022.102928
4. Zhang M, Xiao J, Deng A, et al. Transmission dynamics of an outbreak of the COVID-19 delta variant B.1.617.2 — Guangdong province, China, May–June 2021. China CDC Weekly. 2021;3(27):584–586. doi:10.46234/ccdcw2021.148
5. Taccone FS, Van Goethem N, De Pauw R, et al. The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium. Lancet Reg Health Eur. 2021;2:100019. doi:10.1016/j.lanepe.2020.100019
6. Zach S, Fernandez-Rio J, Zeev A, et al. Physical activity, resilience, emotions, moods, and weight control, during the COVID-19 global crisis. Isr J Health Policy Res. 2021;10(1):52. doi:10.1186/s13584-021-00473-x
7. Wang Q, Huang R. The impact of COVID-19 pandemic on sustainable development goals - A survey. Environ Res. 2021;202:111637. doi:10.1016/j.envres.2021.111637
8. Qi L, Yu Q, Liang Z, et al. Psychological responses and dietary changes of residents during the local outbreak of COVID-19 in the post-epidemic era: a cross-sectional study. Medicine. 2023;102(5):e32792. doi:10.1097/MD.0000000000032792
9. Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–98. doi:10.1016/j.jad.2020.11.117
10. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (covid-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1789.
11. Dong F, Liu HL, Yang M, et al. Immediate psychosocial impact on healthcare workers during covid-19 pandemic in china: a systematic review and meta-analysis. Front Psychol. 2021;12:645460. doi:10.3389/fpsyg.2021.645460
12. Romm KF, Patterson B, Wysota CN, et al. Predictors of negative psychosocial and health behavior impact of COVID-19 among young adults. Health Educ Res. 2022;36(4):385–397. doi:10.1093/her/cyab026
13. Li S, Guo B, Yang Q, et al. Factors associated with depression in residents in the post-epidemic era. QJM. 2022;115(9):605–609. doi:10.1093/qjmed/hcac181
14. Tang S, Chen H, Wang L, et al. The relationship between physical exercise and negative emotions in college students in the post-epidemic era: the mediating role of emotion regulation self-efficacy. Int J Environ Res Public Health. 2022;19(19):12166. doi:10.3390/ijerph191912166
15. Hui-Ren Z, Li-Li M, Qin L, et al. Evaluation of the correlation between sleep quality and work engagement among nurses in Shanghai during the post-epidemic era. Nurs Open. 2023;10(7):4838–4848. doi:10.1002/nop2.1735
16. Liu S, Luo P, Tang M, et al. Providing pharmacy services during the coronavirus pandemic. Int J Clin Pharm. 2020;42(2):299–304. doi:10.1007/s11096-020-01017-0
17. Bukhari N, Rasheed H, Nayyer B, et al. Pharmacists at the frontline beating the COVID-19 pandemic. J Pharm Policy Pract. 2020;13(1):8. doi:10.1186/s40545-020-00210-w
18. LeBlanc VR. The effects of acute stress on performance: implications for health professions education. Acad Med. 2009;84(10 Suppl):S25–S33. doi:10.1097/ACM.0b013e3181b37b8f
19. Fountoulakis KN, Karakatsoulis GN, Abraham S, et al. The effect of different degrees of lockdown and self-identified gender on anxiety, depression and suicidality during the COVID-19 pandemic: data from the international COMET-G study. Psychiatry Res. 2022;315:114702. doi:10.1016/j.psychres.2022.114702
20. Buomprisco G, Cedrone F, Vitali M, et al. Pharmacists’ mental health during the SARS-CoV-2 pandemic in Italy. Eur Rev Med Pharmacol Sci. 2022;26(11):4140–4147. doi:10.26355/eurrev_202206_28987
21. Gong Y, Zhou H, Zhang Y, et al. Validation of the 7-item generalized anxiety disorder scale (GAD-7) as a screening tool for anxiety among pregnant Chinese women. J Affect Disord. 2021;282:98–103. doi:10.1016/j.jad.2020.12.129
22. Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
23. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi:10.1002/da.10113
24. Yu XN, Zhang JX. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Pers. 2007;35(1):19–30. doi:10.2224/sbp.2007.35.1.19
25. Hamadeh KS, Garvey L, Willetts G, et al. Undergraduate nursing students’ resilience, challenges, and supports during Corona virus pandemic. Int J Ment Health Nurs. 2021;30(Suppl 1):1407–1416. doi:10.1111/inm.12896
26. Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE guide No. 131. Med Teach. 2020;42(8):846–854. doi:10.1080/0142159X.2020.1755030
27. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042
28. Almalki AH, Alzahrani MS, Alshehri FS, et al. The psychological impact of covid-19 on healthcare workers in Saudi Arabia: a year later into the pandemic. Front Psychiatry. 2021;12:797545. doi:10.3389/fpsyt.2021.797545
29. Akbari M, Seydavi M, Babaeifard M, et al. Psychometric properties and psychological correlates of the COVID-19 anxiety syndrome scale: a comprehensive systematic review and meta-analysis. Clin Psychol Psychot. 2023;30(5):931–949. doi:10.1002/cpp.2861
30. Hlubocky FJ, Back AL, Shanafelt TD, et al. Occupational and personal consequences of the covid-19 pandemic on us oncologist burnout and well-being: a study from the asco clinician well-being task Force. JCO Oncol Pract. 2021;17(7):e427–e438. doi:10.1200/OP.21.00147
31. KilaniI HA, Bataineh MF, Al-Nawayseh A, et al. Correction: healthy lifestyle behaviors are major predictors of mental wellbeing during COVID-19 pandemic confinement: a study on adult Arabs in higher educational institutions. PLoS One. 2022;17(8):e273276. doi:10.1371/journal.pone.0273276
32. Labrague LJ, De Los SJ. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–1661. doi:10.1111/jonm.13121
33. Nikčević AV, Marino C, Kolubinski DC, et al. Modelling the contribution of the big five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J Affect Disord. 2021;279:578–584. doi:10.1016/j.jad.2020.10.053
34. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of coronavirus disease 2019 (covid-19) beyond paranoia and panic. Ann Acad Med Singap. 2020;49(3):155–160. doi:10.47102/annals-acadmedsg.202043
35. Eales L, Ferguson GM, Gillespie S, et al. Family resilience and psychological distress in the COVID-19 pandemic: a mixed methods study. Dev Psychol. 2021;57(10):1563–1581. doi:10.1037/dev0001221
36. Ye Z, Yang X, Zeng C, et al. Resilience, social support, and coping as mediators between covid-19-related stressful experiences and acute stress disorder among college students in China. Appl Psychol Health Well Being. 2020;12(4):1074–1094. doi:10.1111/aphw.12211
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
