Back to Journals » Journal of Inflammation Research » Volume 16
Prognostic Value of Pentraxin-3 Change After Primary Percutaneous Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction
Authors Li SY, Liu L, Wang DK, Ding XS , Li WP, Li HW
Received 17 October 2022
Accepted for publication 10 March 2023
Published 22 March 2023 Volume 2023:16 Pages 1255—1266
DOI https://doi.org/10.2147/JIR.S393703
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Sheng-Yu Li,1 Lei Liu,1 Ding-Kun Wang,1 Xiao-Song Ding,1 Wei-Ping Li,1,2 Hong-Wei Li1,2
1Department of Cardiology, Cardiovascular Center, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Beijing Key Laboratory of Metabolic Disorder Related Cardiovascular Disease, Beijing, People’s Republic of China
Correspondence: Wei-Ping Li; Hong-Wei Li, Department of Cardiology, Cardiovascular Center, Beijing Friendship Hospital, Capital Medical University, No. 95 Yongan Road, Xicheng District, Beijing, 100050, People’s Republic of China, Tel +86-13810267817 ; +86-13801396679, Email [email protected]; [email protected]
Purpose: So far, ST-segment elevation myocardial infarction (STEMI) is still the main cause of morbidity and mortality of cardiovascular diseases worldwide. Recent studies showed that pentraxin-3 (PTX3) was related to the early diagnosis and prognosis of coronary heart disease. This study aimed to investigate the dynamical change of PTX3 after primary percutaneous coronary intervention (pPCI) in STEMI patients and its prognostic value.
Patients and methods: In this prospective cohort study, a total of 350 patients were enrolled. The plasma level of PTX3 was measured at admission, 24-hour and 5-day after pPCI. The primary endpoint was the incidence of major adverse cardiac cerebral events (MACCEs) during 1-year follow-up.
Results: Compared with the admission, PTX3 levels were significantly increased at 24 hours, and decreased at 5 days after pPCI in the whole cohort. PTX3 levels at these three time points were not significantly different between the patients with and without MACCEs. Notably, the change in PTX3 from admission to post-pPCI 24-hour (ΔPTX3) was higher in patients with MACCEs (112.83 vs 17.94 ng/dl, P = 0.001). The ROC curves showed that the cut-off value was 29.22 ng/dl and the area under curves was 0.622 (95% CI: 0.554– 0.690, p = 0.001). Multivariable cox regression models revealed that the high ΔPTX3 group was an independent predictor of MACCEs (adjusted HR = 2.010, 95% CI = 1.280– 3.186, p = 0.003). The higher ΔPTX3 group had significantly higher incidences of revascularization (HR = 2.094, 95% CI: 1.056– 4.150, p = 0.034) and composite MACCEs (HR = 2.219, 95% CI: 1.425– 3.454, p < 0.001). However, the change of PTX3 level from admission to post-pPCI 5-day had no independently predictive value.
Conclusion: The higher increase of PTX3 level 24-hour after pPCI appeared to have a potential value in independently predicting the incidence of 1-year MACCEs in STEMI patients, especially for coronary revascularization.
Keywords: pentraxin-3, primary percutaneous coronary intervention, ST-segment elevation myocardial infarction, prognosis
Introduction
Inflammatory process plays a key role in the creation and development of atherosclerosis.1 Pentraxin-3 (PTX3) is a member of the pentraxin superfamily, and was first identified in 1992.2 PTX3 is rapidly produced and released by several cell types, in particular by mononuclear phagocytes, dendritic cells, fibroblasts and endothelial cells in response to primary inflammatory signals.3 It was shown to have a special role in the pathophysiology of atherosclerosis and myocardial infarction.4 As ST segment elevation myocardial infarction (STEMI) is one of the main reasons for morbidity and mortality worldwide,5 more attention should be paid to the biomarkers of the prognosis in this population. In previous studies, after systemic administration of microbial products and inflammatory cytokines or ligation of the left coronary artery to model acute myocardial infarction in rodents, the expression of PTX3 in the myocardium increased significantly.6 Elevated initial PTX3 levels are not only more sensitive than other commonly used clinical biomarkers, including N-terminal prohormone brain natriuretic peptide (NT-proBNP), troponin T (TnT), creatine kinase (CK), in predicting the 3-month prognosis of patients with STEMI,7 but also associated with higher mortality even in long-term observational studies.8 However, the predictive value of early dynamic changes of PTX3 levels for long-term MACCEs in STEMI patients undergoing primary percutaneous coronary intervention (pPCI) remains unclear. Therefore, we investigated the change in PTX3 levels from admission to post-pPCI in STEMI patients, and further assessed the relationship between the change and the incidence of major adverse cardiac cerebral events (MACCEs) during 1-year follow-up period.
Methods
Patients
Study subjects were identified from the Cardiovascular Center of Beijing Friendship Hospital Database (CBD) Bank. This study has been cleared by our Institution Ethics Review Board for human studies and that patients have signed an informed consent. The patient flowchart is presented in Figure 1. A total of 481 patients were diagnosed with STEMI from February 2017 to April 2020. Of these patients, 396 underwent successful pPCI within 6 hours of chest pain onset. All patients met the diagnostic criteria of European Society of Cardiology (ESC) for STEMI: 1) there were symptoms and signs of continuous myocardial ischemia (such as continuous chest pain) 6 hours before admission, 2) ECG examination showed that ST-segment elevation in at least two contiguous leads. Of the 396 patients, 46 were excluded according to the exclusion criteria, which were 1) severe renal dysfunction; 2) severe liver disease; 3) acute infectious disease or rheumatic disease; 4) current neoplastic disease; 5) estimated life expectancy less than 1 year, 6) lacking clinical or follow-up data. Finally, 350 patients were included in this study and divided into 2 groups (patients with MACCEs, n = 90 and patients without MACCEs, n = 260). All patients were followed up 1 year. The study protocol was conducted in accordance with the principles outlined in the Declaration of Helsinki. Every patient signed the informed written consent before enrolled in the study.
Data Collection
The data collection protocol was approved by the Institutional Review Board of Beijing Friendship Hospital affiliated to Capital Medical University. Patients’ demographics, medical history, laboratory test results, echocardiographic, and angiographic evaluation results were collected and verified using an electronic medical recording system. The outcomes of MACCEs were collected and recorded during clinical follow-up visits. MACCEs included cardiac death, non-fatal MI, non-fatal stroke, revascularization, and cardiac rehospitalization. Cardiac death was defined as fatal myocardial infarction, sudden death, and other cardiovascular death. Any coronary revascularization was defined as a revascularization of the target vessel or non-target vessels. Cardiac rehospitalization refers to rehospitalization for chest tightness, chest pain, angina pectoris or heart failure.
Cardiac troponin I (cTnI), creatine kinase (CK) and creatine kinase isoenzyme-MB (CKMB) levels were measured with a sandwich electrochemiluminescence immunoassay in the Department of Laboratory Medicine. The serum levels of N-terminal pro-B-type natriuretic peptide (NT-proBNP) were measured with a solid-phase chromatographic immunoassay. The high-sensitivity C-reactive protein (hsCRP) level was measured with the particle-enhanced immunonephelometric assay. One tube of venous blood was collected from all patients at admission, 24 hours after pPCI and 5 days after pPCI. The blood was centrifuged at 4°C and 1000 rpm for 15 minutes. Plasma was separated and stored at –80°C to analyze the concentration of PTX3. PTX3 was assayed with a commercial Human PTX3 ELISA kit (Human PTX3/TSG-14 immunoassay Quantikine® ELISA, Catalog Number DPTX30B, USA R&D Systems, Inc.) by dedicated laboratory personnel and blinded to the characteristics of the patients. A streptavidin-coated plate was incubated with a biotinylated monoclonal antibody specific for human PTX3. Plates were washed, standards and samples were pipetted into the wells. Any PTX3 present was bound by the immobilized biotinylated antibody. After washing away any unbound substances, an enzyme-linked monoclonal antibody specific for human PTX3 was added to the wells. Following a wash to remove any unbound antibody-enzyme reagents, a substrate solution was added to the wells and color developed in proportion to the amount of PTX3 bound. The color development was stopped and the intensity of the color was measured. The PTX3 level (ng/dl) was determined using a standard curve. The minimum detectable dose (MDD) of PTX3 ranged from 0.4 to 2.6 ng/dl and the mean MDD was 1.4 ng/mL. The intra-assay coefficient of variation (CV) was 1.87% and the inter-assay CV was 5.93% according to the protocol. Reagents of the same lot numbers were used for all determinations to minimize the measurement variability.
Statistical Analysis
Continuous variables were presented as mean±standard deviation (SD) or median (IQR). Comparisons between the 2 groups or PTX3 concentration at the same time point were analyzed by Student’s t-test or ManWhitney U-test. Categorical variables were expressed as number and percentage and compared using the Pearson chi-square test or Fisher’s exact test. Besides, this study calculated the change in PTX3 concentration between postoperative and preoperative. ΔPTX3 represented the change from admission to post-pPCI 24-hour. Spearman correlation was used to measure correlation between ΔPTX3 and other indexes. The receiver operating characteristic (ROC) curve was drawn to evaluate the cut-off value of ΔPTX3 in predicting MACCEs. A multivariable Cox regression analysis was performed in order to determine whether ΔPTX3 was an independent predictor for MACCEs, and to identify other predictors of MACCEs. Some of baseline variables that were significantly correlated with outcomes by univariate analysis and clinically relevant were entered into the multivariate model. The formal test of proportional hazard assumption using Schoenfeld residuals. The cumulative incidence of MACCEs was estimated by Kaplan–Meier survival curves, and the groups were compared using the Log rank test. All analyses were two-tailed and p value <0.05 was considered statistically significant. Data were analyzed using IBM SPSS statistics 21.
Results
Baseline Characteristics of Patients
As shown in Table 1, MACCEs occurred in 25.7% of the included patients during 1-year follow-up. Most of the patients were male (75.4%) but there was no significant difference between the patients with and without MACCEs. Patients with MACCEs were significantly older, showed higher percentage of previous AMI and PCI/CABG (all p < 0.05). Compared with patients without MACCEs, the patients with MACCEs had lower TC, lower HDL-c and LDL-c, and significantly higher peak level of NT-proBNP (all p < 0.05). Echo evaluation showed that the LVESVI in the patients with MACCEs were higher while LVEF were lower (all p < 0.05). Angiographically, the percentages of multi-vessel/left main (LM) coronary artery lesions were similar between 2 groups but syntax score was significantly higher in the patients with MACCEs (p < 0.05). Besides, the GRACE risk score and the TIMI risk score were also significantly higher in this group (p < 0.05). As for medication before admission, the patients with MACCEs took more statins.
 |
Table 1 Baseline Characteristics of Patients with and without MACCEs |
Dynamical Change of PTX3 Concentration
Figure 2 shows PTX3 concentration increased at 24-hour after pPCI and then significantly decreased at 5-day after pPCI whether in all patients or in the patients with or without MACCEs. There was no difference in PTX3 concentration at the same time point between the 2 groups. However, the change in PTX3 from admission to post-pPCI 24-hour (ΔPTX3) was higher in the patients with MACCEs (112.83 ng/dl vs 17.94 ng/dl, p = 0.001), while the change in PTX3 from admission to post-pPCI 5-day was similar. Spearman correlation analysis displayed that ΔPTX3 was associated with peak NT-proBNP (r = 0.1374, p = 0.0104), LVEF (r=−0.1294, p = 0.0156), Syntax score (r = 0.2006, p = 0.0002), GRACE score (r = 0.1398, p = 0.0088) and TIMI score (r = 0.1274, p = 0.0171), respectively (Figure 3).
ΔPTX3 as a Marker to Predict MACCEs
The ROC curve of ΔPTX3 as a marker to predict MACCEs in all patients is illustrated in Figure 4. The AUC of ΔPTX3 for predicting the occurrence of MACCEs was 0.622 (95% CI = 0.554–0.690, p = 0.001). The cut-off value was 29.22 ng/dl, and the sensitivity and specificity were 67.8% and 45.2%, respectively.
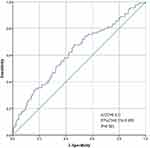 |
Figure 4 The receiver operating characteristic (ROC) curve of the ΔPTX3 as a marker to predict MACCEs. Abbreviations: PTX3, pentraxin-3; ΔPTX3, the change in PTX3 from admission to post-pPCI 24-hour. |
Cox Regression Analysis for 1-Year MACCEs
Based on the cut-off value of ΔPTX3, all the patients were divided into low ΔPTX3 group (ΔPTX3 <29.22 ng/dl) and high ΔPTX3 group (ΔPTX3 ≥29.22 ng/dl). Univariate and multivariate analyses to determine the predictors for MACCEs are presented in Table 2. Univariate analysis revealed that the high ΔPTX3 group, age, previous PCI/CABG, HDL-c, LDL-c, peak NT-proBNP, LVEF, and statin were risk factors of MACCEs (all p < 0.05). Because gender is also one of the important clinical risk factors, we included male gender in multivariate analysis. Schoenfeld residuals test is shown in Supplementary Figure 1 and Supplementary Table 1. All continuous variables in the cox model confirmed with the proportional hazard assumption. After adjusting for male gender and other potential confounding factors, multivariate analysis found that the ΔPTX3 ≥29.22 ng/dl (adjusted HR = 2.010, 95% CI = 1.280–3.186, p = 0.003), previous PCI/CABG, LVEF was the independent predictor of 1-year MACCEs.
 |
Table 2 Univariate and Multivariate Cox Regression Analysis of MACCEs in All Patients |
Prognostic Performances of ΔPTX3 for Different Clinical Events
Table 3 and Figure 5 demonstrate the incidences of MACCEs in the two groups. During 1-year follow-up, MACCEs occurred in 29 (17.2%) patients in low ΔPTX3 group and 61 (33.7%) patients in high ΔPTX3 group (HR = 2.219, 95% CI = 1.425–3.454, p < 0.001). No-fatal MI occurred in 3(1.7%) patients in low ΔPTX3 group and 4 (2.4%) patients in high ΔPTX3 group (HR = 0.699, 95% CI = 0.157–3.125, p = 0.637). No-fatal stroke occurred in 1(0.6%) patients in low ΔPTX3 group and 1(0.6%) patients in high ΔPTX3 group (HR = 0.931, 95% CI = 0.058–14.883, p = 0.960). Revascularization occurred in 26 (14.4%) patients in low ΔPTX3 group and 12 (7.1%) patients in high ΔPTX3 group (HR = 2.094, 95% CI = 1.056–4.150, p = 0.028). Cardiac rehospitalization occurred in 30 (16.6%) patients in low ΔPTX3 group and 22 (13.0%) patients in high ΔPTX3 group (HR = 1.312, 95% CI = 0.757–2.2740, p = 0.332). Cardiac death occurred in 4(2.2%) patients in low ΔPTX3 group and 2(1.2%) patients in high ΔPTX3 group (HR = 1.872, 95% CI = 0.343–10.222, p = 0.469).
 |
Table 3 Clinical Events in Low ΔPTX3 Group and High ΔPTX3 Group During 1-Year Follow-Up |
Discussion
To the best of our knowledge, this is the first study to explore the association between dynamical change of PTX3 concentration and cardiovascular outcomes in STEMI patients undergoing pPCI. We presented two important findings in this study. 1) We measured the plasma concentrations of PTX3 at three time points after pPCI and found that the pattern of PTX3 changes was similar to that of myocardial enzymes. The concentration of PTX3 increased significantly 24 hours after pPCI and decreased 5 days after pPCI. 2) The change in PTX3 from admission to post-pPCI 24-hour has a strong predictive value for MACCE incidence during 1-year follow-up in patients with STEMI. Patients with MACCEs had significantly greater increase of plasma PTX3 levels than patients without MACCEs.
It is well known that STEMI is still the main cause of morbidity and mortality of cardiovascular diseases worldwide.5 Even for patients undergoing pPCI, the in-hospital mortality of STEMI patients remains still high after opening the infarcted vessels within a short time after the onset of symptoms. At the same time, they also have a high risk of major cardiovascular adverse events (MACEs) and cardiovascular mortality after the acute phase.5,9 Gladys et al10 followed up 142 patients with STEMI who were treated with delayed or immediate coronary intervention and found that the 1-year MACEs (consisting of death, recurrent infarction, and target lesion revascularization) rate was 10.1%. Another study by Stephen et al11 included 3534 patients with STEMI. The rate of the 15-month primary end point (including death from cardiovascular causes, nonfatal MI, or nonfatal stroke) they reported was 22.4%. Thus, it can be seen that the 1-year adverse events rate of 25.7% reported by us was relatively higher in the current era of primary PCI. It may be because our cohort was non-random, and we included more categories of adverse events. Therefore, paying attention to the prognosis of this population has become an important task, and it is necessary to find more appropriate biomarkers to predict clinical outcomes. Previous studies had shown that PTX3 was related to the early diagnosis and prognosis of coronary heart disease, including stable angina pectoris and acute coronary syndrome (ACS).12–15 In our study, the change in PTX3 concentrations in acute myocardial infarction (AMI) is similar to the previous study, because it is released from dead or necrotic cells.16 Fornai et al indicated that the plasma PTX3 level increased significantly about 7 hours after the onset of AMI and decreased to the baseline level 3 days later.17 Marie et al18 found that plasma PTX3 at 24h after STEMI onset is a strong predictor of 30-day and 1-year mortality. PTX3 as a single biomarker is comparable with currently used scoring systems (TIMI or GRACE) or brain natriuretic peptide (BNP).
Mjelva et al19 followed up 817 patients suspected of ACS for up to 7 years and compared the predictive effects of HsCRP, PTX3 and BNP on long-term MACEs. The results showed that plasma PTX3 level >5.88 ng/mL could independently predict all-cause mortality like plasma D-dimer and BNP levels. Kontny et al20 analyzed the correlation between PTX3 and other biomarkers and clinical prognosis in 5154 patients with ACS included in PLATO trial. After adjusting leukocyte, HsCRP, interleukin-6 and cystatin C, the plasma PTX3 level at admission can independently predict the occurrence of cardiovascular death and fatal myocardial infarction. Moreover, the level of PTX3 detected at 1 month can still predict the composite cardiovascular endpoint (cardiovascular death, myocardial infarction or stroke). Khamitova et al21 conducted a 1-year follow-up of 180 patients with myocardial infarction. The results showed that the risk assessment model established by PTX3 combined with NT-proBNP and soluble ST2 level could predict the risk of 1-year composite endpoint events (myocardial infarction, acute cerebrovascular disease, hospitalization for cardiovascular disease and cardiovascular death). Altay et al22 followed up 140 patients with acute myocardial infarction for 5 years. They found that the level of PTX3 in the coronary restenosis group was significantly higher than that in the non restenosis group. Cox risk model analysis after adjusting for multiple risk factors showed that PTX3, NT-proBNP and GRACE scores could independently predict long-term cardiovascular mortality (odds ratios were 2.175, 1.632 and 1.132, respectively), but cTnI had no predictive effect. Dharma et al23 observed 335 patients with STEMI undergoing PCI and found that patients with PTX3 at the highest quartile level (≥0.4ng/mL) had a higher proportion of baseline leukocyte count, cTnT value and preoperative TIMI blood flow of grade 0, were more likely to be complicated with acute heart failure, showed heavier thrombus load during operation and lower TIMI blood flow grade after operation. Multiple Cox regression analysis showed that the 30 day mortality of patients with PTX3≥0.4ng/mL increased by nearly 12%. Ljuca et al24 measured the plasma levels of PTX3, HsCRP and cTnI in patients undergoing bare metal stent implantation for STEMI immediately after admission and 24 hours after PCI, and followed up for 1 year. The results showed that the plasma levels of PTX3, HsCRP and cTnI increased significantly after PCI. The level of PTX3 24 hours after operation in patients with MACEs was higher than that in patients without MACEs during 1 year. The risk of MACEs was significantly increased in patients with PTX3>5.042 ng/mL. Multivariate Cox regression analysis showed that PTX3 had a higher value in predicting 2-year MACE than cTnI, while HsCRP had no independent predictive value. However, the predictive value of PTX in NSTE-ACS (non ST-elevation acute coronary syndrome) patients is unclear. Eggers et al25 reported the study of PTX3 and NSTE-ACS patients, they found that PTX3 levels were higher in patients who died within 1 year but was not an independent predictor of 1-year mortality.
In our study, the patients with MACCEs were older, had higher percent of previous revascularization, lower LVEF and higher syntax score, GRACE and TIMI risk score. Besides, the lower LDL-c was related to higher percent of statins treatment before admission. However, different from the above studies, there was no significant difference in PTX3 levels at all different time (immediately after admission, 24 hours after pPCI and 5 days after pPCI) between patients with and without MACCEs in our study. This may be because the selected population is different, or the number of participants is diverse. Therefore, we further discussed the predictive value of the PTX3 concentration change for 1-year MACCEs.
The results showed that there was a significant difference in ΔPTX3 (the change in PTX3 from admission to post-pPCI 24-hour) between the patients with and without MACCEs. As mentioned above, PTX3 is released from dead or necrotic cells17 and participates in the primary inflammatory signal response.3 The trend of PTX3 concentration change after myocardial infarction is similar to that of myocardial enzymes. Current studies show that PTX3 plays an important role in the development of atherosclerosis by regulating complement system, inflammatory response, oxidative stress, vascular remodeling, thrombosis etcetera.26–28 This probably explained ΔPTX3 was related to peak NT-proBNP, LVEF, syntax score, GRACE and TIMI risk score.
ROC curve was applied in order to find the cut-off value of ΔPTX3 to predict MACCEs, and then we got 29.22 ng/dl. Multivariate cox regression analysis found that ΔPTX3≥29.22 ng/dl was an independent predictor of MACCEs after adjusting for age, gender and other confounding factors. This result proved that ΔPTX3 was an independent predictor of MACCEs. Compared with the ΔPTX3<29.22 ng/dl group, the ΔPTX3≥29.22 ng/dl group had significantly higher incidences of revascularization and composite MACCEs during 1-year follow-up.
Our study had several limitations. First, our rate of events was relatively higher than some previous reports. Although the possible causes were discussed above, it may also have some impact on the results. After all, this was a single center study with relatively small sample, and the generalization of the findings should be cautious. Second, this study was followed up for only one year, which may limit the power of the study, and a longer follow-up time is needed to strengthen the long-term predictive value of PTX3.
Conclusions
The increase of plasma PTX3 level from admission to 24-hour after pPCI has a strong value in independently predicting 1-year MACCEs, especially coronary revascularization, in STEMI patients undergoing pPCI. This result suggests that we should pay more attention to the dynamical change of PTX3 rather than a single time point in the future management of STEMI patients. Mitigating PTX3 elevation as a therapeutic target may reduce post-pPCI MACCEs and improve clinical outcomes.
Data Sharing Statement
All data are available upon request to the corresponding author Wei-ping Li and Hong-wei Li.
Acknowledgments
We gratefully acknowledge the contributions of all staffs who work on the Cardiovascular Center of Beijing Friendship Hospital Data Bank (CBD BANK).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Key R&D Program of China (2021ZD0111004), Natural Science Foundation of\ China (No. 82070357), Beijing Municipal Administration of Hospital Incubating Program (No. PX2018002), and Beijing Key Clinical Subject Program.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ross R. Atherosclerosis – an inflammatory disease. N Engl J Med. 1993;340:115–126.
2. Emsley J, White HE, O’Hara BP, et al. Structure of pentameric human serum amyloid P component. Nature. 1994;367(6461):338–345. doi:10.1038/367338a0
3. Garlanda C, Bottazzi B, Bastone A, Mantovani A. Pentraxins at the crossroads between innate immunity, inflammation, matrix deposition, and female fertility. Annu Rev Immunol. 2005;23:337–366. doi:10.1146/annurev.immunol.23.021704.115756
4. Ristagno G, Fumagalli F, Bottazzi B, et al. Pentraxin 3 in cardiovascular disease. Front Immunol. 2019;10:823. doi:10.3389/fimmu.2019.00823
5. Ibanez B, Lames S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi:10.1093/eurheartj/ehx393
6. Introna M, Vidal Alles V, Castellano M, et al. Cloning of mouse PTX3, a new member of the pentraxin gene family expressed at extrahepatic sites. Blood. 1996;87:1862–1872. doi:10.1182/blood.V87.5.1862.1862
7. Latini R, Maggioni AP, Peri G, et al. Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2004;110(16):2349. doi:10.1161/01.CIR.0000145167.30987.2E
8. Akgul O, Baycan OF, Nakano A, et al. Long-term prognostic value of elevated pentraxin 3 in patients undergoing primary angioplasty for ST-elevation myocardial infarction. Coron Artery Dis. 2015;26:592–597. doi:10.1097/MCA.0000000000000280
9. Ponikowski P, Voors AA, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi:10.1002/ejhf.592
10. Janssens GN, van der Hoeven NW, Lemkes JS, et al. 1-year outcomes of delayed versus immediate intervention in patients with transient ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2019;12(22):2272–2282. doi:10.1016/j.jcin.2019.07.018
11. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–2015. doi:10.1056/NEJMoa0706482
12. Kume N, Mitsuoka H, Hayashida K, Tanaka M. Pentraxin 3 as a biomarker for acute coronary syndrome: comparison with biomarkers for cardiac damage. J Cardiol. 2011;58(1):38–45. doi:10.1016/j.jjcc.2011.03.006
13. Kimura S, Sugiyama T, Hishikari K, et al. Relationship of systemic pentraxin-3 values with coronary plaque components on optical coherence tomography and post-percutaneous coronary intervention outcomes in patients with stable angina pectoris. Atherosclerosis. 2020;292:127–135. doi:10.1016/j.atherosclerosis.2019.11.022
14. Demir MT, Baydin A, Amanvermez R, Erenler AK, Güzel M, Yücel O. Comparison of pentraxin-3 and ischemia-modified albumin with troponin in early diagnosis of acute coronary syndrome. Bratisl Lek Listy. 2018;119(8):509–512. doi:10.4149/BLL_2018_093
15. George M, Shanmugam E, Srivatsan V, et al. Value of pentraxin-3 and galectin-3 in acute coronary syndrome: a short-term prospective cohort study. Ther Adv Cardiovasc Dis. 2015;9(5):275–284. doi:10.1177/1753944715578405
16. Peri G, Introna M, Corradi D, et al. PTX3, A prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation. 2000;102(6):636. doi:10.1161/01.CIR.102.6.636
17. Fornai F, Carrizzo A, Forte M, et al. The inflammatory protein Pentraxin 3 in cardiovascular disease. Immun Ageing. 2016;13(1):25. doi:10.1186/s12979-016-0080-1
18. Marie T, Jiri J, Josef T, et al. Prognostic value of pentraxin-3 level in patients with STEMI and its relationship with heart failure and markers of oxidative stress. Dis Markers. 2015;2015:1–11.
19. Mjelva ØR, Pönitz V, Brügger-Andersen T, et al. Long-term prognostic utility of pentraxin 3 and D-dimer as compared to high-sensitivity C-reactive protein and B-type natriuretic peptide in suspected acute coronary syndrome. Eur J Prev Cardiol. 2016;23(11):1130–1140. doi:10.1177/2047487315619733
20. Kontny F, Andersen T, Ueland T, et al. Pentraxin-3 vs C-reactive protein and other prognostic biomarkers in acute coronary syndrome: a substudy of the Platelet Inhibition and Patients Outcomes (PLATO) trial. Eur Heart J. 2019;9(4):313–322.
21. Khamitova AF, Lakman IA, Akhmetvaleev RR, et al. Multifactor predictive model in patients with myocardial infarction based on modern biomarkers. Kardiologiia. 2020;60(3):14–20. doi:10.18087/cardio.2020.3.2593
22. Altay S, Çakmak HA, Kemaloğlu ÖZT, et al. Long-term prognostic significance of pentraxin-3 in patients with acute myocardial infarction: 5-year prospective cohort study. Anatol J Cardiol. 2017;17(3):202–209. doi:10.14744/AnatolJCardiol.2016.7307
23. Dharma S, Sari NY, Santoso A, et al. Association of plasma pentraxin 3 concentration with angiographic and clinical outcomes in patients with acute ST-segment elevation myocardial infarction treated by primary angioplasty. Catheter Cardiovasc Interv. 2020;96(6):1233–1239. doi:10.1002/ccd.28626
24. Ljuca F, Hadžiefendić B, Jahić E, et al. Pentraxin 3 might be better prognostic serum marker than IL-6, IL-10, and high-sensitivity C-reactive protein for major adverse cardiovascular events in patients with ST-elevation myocardial infarction after bare-metal stent implantation. Saudi Med J. 2019;40(12):1202–1208. doi:10.15537/smj.2019.12.24737
25. Eggers KM, Armstrong PW, Califf RM, et al. Clinical and prognostic implications of circulating pentraxin 3 levels in non ST-elevation acute coronary syndrome. Clin Biochem. 2013;46(16–17):1655–1659. doi:10.1016/j.clinbiochem.2013.08.014
26. Luo X-Y, Zhu X-Q, Li Y, et al. MicroRNA-150 restores endothelial cell function and attenuates vascular remodeling by targeting PTX3 through the NF-κB signaling pathway in mice with acute coronary syndrome. Cell Biol Int. 2018;42(9):1170–1181. doi:10.1002/cbin.10985
27. Balhara J, Shan L, Zhang J, et al. Pentraxin 3 deletion aggravates allergic inflammation through a T17-dominant phenotype and enhanced CD4 T-cell survival. J Allergy Clin Immunol. 2017;139(3):950–963.e9. doi:10.1016/j.jaci.2016.04.063
28. Zlibut A, Bocsan IC, Agoston-Coldea L. Pentraxin-3 and endothelial dysfunction. Adv Clin Chem. 2019;91:163–179.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




