Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Process Evaluation of Health System Responsiveness Level and Associated Factors Among Mothers Gave Birth at Obstetric Ward in a Tertiary Hospital, Southwest of Ethiopia: Mixed Study Methods
Authors Girma G, Tamire A , Edessa GJ , Dechasa M , Tefasa OK , Negash A , Dereje J , Masrie A , Shawel S , Mandefro M , Abraham G
Received 12 June 2023
Accepted for publication 7 August 2023
Published 14 August 2023 Volume 2023:16 Pages 2291—2308
DOI https://doi.org/10.2147/JMDH.S397735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Gezu Girma,1 Aklilu Tamire,2 Gebeyehu Jeldu Edessa,3 Mesay Dechasa,4 Obsan Kassa Tefasa,2 Abraham Negash,5 Jerman Dereje,6 Awoke Masrie,2 Samrawit Shawel,2 Miheret Mandefro,2 Gelila Abraham3
1Department of Health Research, International Center for AIDS Care and Treatment Program (ICAP), Finfine, Ethiopia; 2School of Public Health, College of Health and Medical Science, Haramaya University, Harar, Harari, Ethiopia; 3Department of Health Policy and Management, Public Health Faculty, Institute of Health Jimma University, Jimma, Oromia, Ethiopia; 4Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Science, Haramaya University, Harar, Ethiopia; 5School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 6Department of Psychiatry, School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Aklilu Tamire, School of Public Health, College of Health and Medical Science, Haramaya University, P.O. Box 235, Harar, Harari, 3200, Ethiopia, Tel +251921211752, Email [email protected]
Background: The term responsiveness emerged during the World Health Organization (WHO) report in 2000 as new and essential goals of the health systems to meet the needs of people to their expectations from different services being given in healthcare systems. Obstetric violence and childbirth mistreatment are global problems, but the worst obstetric violence usually occurs in underdeveloped countries. Thus, the main objective of this study was to evaluate the responsiveness of obstetric service at Jimma University Medical Center.
Methods: A single-case study design with quantitative and qualitative data collection was employed. Availability with 17 indicators and health system responsiveness with 24 indicators were used. Consecutive sampling technique was used to select the clients and qualitative data were collected from key informants. SPSS version 25 was used for the analysis of quantitative data, whereas thematic analysis was conducted for qualitative data. A multiple linear regression model was fitted after all assumptions were checked and fit to ensure the relation of the dependent variable with independent variables.
Results: The overall evaluation was 75.6% and judged good. The resource availability and health system responsiveness were 85.5% and 69.7%, which were judged very good and fair, respectively. A stethoscope and thermometer were not available, while 40% glucose, dexamethasone, and intravenous fluid were the most frequently stocked-out supplies. Dignity (72.1%), confidentiality (71.4%), and prompt attention (70%) were the top three good scores for the health system’s responsiveness. Health system responsiveness significantly associated with the following: Not attending formal education, attending college and above, place of delivery (health center), mode of delivery (cesarean section), and being merchant.
Conclusion & Recommendation: The health system responsiveness of delivery service in study setting was good. All stakeholders should work for improving the health system’s responsiveness in delivery service.
Keywords: obstetric, health system responsiveness, Jimma University Medical Center, Ethiopia
Background
The term responsiveness emerged during the World Health Report in 2000 as comparatively new and one of the essential goals of the health systems in meeting the needs of people to their legitimate expectations from different dimensions of services given in healthcare systems.1 Health system responsiveness is a non-monetary and non-clinical aspect which is incorporated into service quality of healthcare that imitates respect humanity and interaction of clients and care providers in the healthcare process.2
Responsive care is not an option or luxury; rather, it is a universal right for childbearing women to get care with humanity and in a very compassionate manner. Mothers have a right to get help when pain felt, not be hurt, to be forced, detain, humiliate, verbally abuse, or discriminate.3 In hospitals all across the world, many women get disrespectful and brutal treatment while giving birth. In addition to violating women’s rights, such mistreatment also puts their rights to life, health, bodily integrity, and equality at risk.4
Obstetric violence and childbirth mistreatment are global problems, but the worst form occurs in under-developed countries including sub-Saharan Africa, specifically, Ethiopia.5 There are some studies assessing the existence of mechanisms for the health system responsiveness in developing nations. The lack of a “whole-systems” approach reflects both the real workings of healthcare institutions and the apparent lack of system-thinking response in the health sector.6 Thus, all-dimension process evaluation of health system responsiveness in the hospitals of low-income countries is crucial to improving the health system’s responsiveness and potentially fulfilling clients’ legitimate expectations.7
There are different health professionals working with great dedication in Ethiopia. Nevertheless, a substantial number of healthcare workers understands all clients as patients, and healthcare workers lack respect for clients and families, resulting in major complaints. A cruel treatment and disregard for women when a child is being born has been practiced repeatedly in the healthcare organization.8,9
A survey conducted in 28 health facilities in Ethiopia in 2017, during labor and delivery, there was mistreatment of women including verbal abuse (8%), physical abuse (9%), violation of privacy (17%), and abandonment or being left alone (19%). Disrespecting and mistreating women is among health facilities delivery services provision limits the Ethiopian women’s use of maternity care services.10 Women’s disrespect and abuse are progressively recognized as an infringement of rights and a deterrent to the use of life-saving institutional-based labor and delivery services. These might contribute to women’s judgments of low care quality and worry about abuse, which are repeatedly practiced in healthcare.11,12
The study reported in 2019 revealed the overall the magnitude of disrespecting and abusing throughout delivery service at Jimma Medical Center (JMC) was 91.7%.13 There were gaps found in that health providers did not respect women’s rights to information, informed consent, preference, a periodic update on the progress of labor, self-introduction before any procedure, and encouraging mothers to ask questions. In Harar Hospital, Eastern Ethiopia, about 62% of women participating in the study did not get respectful maternal care.14,15 The major causes of high maternal death in underdeveloped countries was found to be birth attended by healthcare workers with enough birth attending skills.16 The main factor that could support to decrease maternal and neonatal death was access to maternal healthcare services quality.17
Although a study was performed in the current study settings,13 this study did not focus on all dimensions of responsiveness, and it was conducted before the start of Health System Transformation Plan II (HSTP-II). To the researchers’ knowledge, there has been no study conducted regarding the availability of resources in JMC and responsiveness. Therefore, it is intended to identify the healthcare service responsiveness of the obstetrics ward in Jimma Medical Center in terms of resource availability and responsiveness. Evaluation of delivery service responsiveness has predominant significance in providing information for service provision and improvement. Even though the current maternal mortality of Ethiopia is 412 per 100,000 live births, the national goal for 2024–2025 was set to reduce maternal mortality from 401 to 279.18 This study will provide evidence-based decision-making for both stakeholders and service providers to enhance the non-clinical aspect of the healthcare system to play its role in reducing maternal mortality. The results obtained could be the inputs for hospital managers in improving the healthcare services quality by identifying gaps in client–provider interaction, resource allocation, and trainings. The study is also useful for healthcare professionals to learn about identified gaps during service delivery to improve the client–provider relationship and satisfaction. In addition, this study serves as a basis for further researchers. Figure 1 summarizes the factors affecting HSR.
 |
Figure 1 Newly developed Conceptual Framework for delivery service Responsiveness. |
Methods
Study Design and Area
A single-case study design with mixed data collection method was used to assess the whole delivery services at JMC, Ethiopia. JMC is a teaching hospital founded at Jimma University, a public tertiary hospitals in the Ethiopia which was constructed in 1938. It is found at 352 kilometers southwest of capital city, Addis Ababa.19
It is the huge referral and tertiary hospital in the south-west region of the country with a total of 15 million catchment population. Since 1984, the hospital has served as a clinical teaching center for undergraduate health professionals of different categories and for clinical postgraduate specialty teaching in different clinical specialties. Currently, there are over 120 beds providing services to obstetrics and gynecology wards. For this evaluation, the evaluability assessment was conducted from January 15–24, 2021, and evaluation data were collected from May 1–May 30, 2021.
Evaluation Approach and Focus
A formative evaluation approach was used, which is important to identify and improve the service. The focus of this evaluation was a process that helps to determine whether the service is delivered as intended to the target populations regarding health system responsiveness, which is a non-clinical aspect of the health system, and provides explanations for observed levels of performance.
Variables and Measurement
Resources availabilities in the obstetric ward were assessed by eleven indicators of whether basic equipment, materials, essential drugs, and all necessary supplies were available to provide the services or not in JMC. On the other hand, health system responsiveness was determined and measured by 24 indicators under 8 sub-dimensions of health system responsiveness, including dignity, autonomy, confidentiality, communication, promotion attention, social support, choice, and amenities. This health system response was assessed by four Likert scales: 1 = never, 2 = sometimes, 3 = usually, and 4 = always. Resource availability was assessed by using an inventory checklist developed based on the Ethiopian Hospital Reform Implementation Guideline (EHRIG) minimum requirement. On the other hand, the health system responsiveness assessment tool was adopted from the WHO health system responsiveness survey. Furthermore, a key informant interview guide was developed under two sections (resource availabilities and health system responsiveness), which comprise general questions on the state of service delivery and perceptions of service barriers.
Sample Size Determination
Single population proportion formula was used in calculating sample size, by considering the overall proportion of maternal care responsiveness 0.53,20 margin of error 5%, confidence interval (CI) of 95% assumed (Z1-α/2 = 1.96) and contingency of 10% was added for non-response. The sample size for clients’ interviews was calculated as follows: 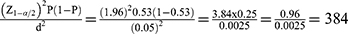 and having 10% of non-response rate and final calculated sample size was 422 for exit interview.
and having 10% of non-response rate and final calculated sample size was 422 for exit interview.
Sampling techniques: Consecutive sampling techniques were used to get the number of clients required, while a key informant were selected purposively.
Dependent Variables
Health System Responsiveness
Independent Variables
Socio demographic variables: Age, Marital status, Education status, Religion, Ethnicity, Residency, Occupational status, Number of family members, Average family monthly income, place of delivery, Mode of current delivery, History of stillbirth, Family size, and Income. Obstetric characters: Number of pregnancies, Parity, Previous place of delivery, Antinatal care (ANC) follow-up history, Stillbirth history, and Abortion history.
Study Populations and Sampling Technique
Mothers came to the Obstetrics Ward in Jimma Medical Center during the evaluation period, and health service providers in labor, delivery, and maternity units, Key stakeholders (JMC management, nursing school, obstetrics and gynecology department, Jimma zonal, and city health office) were the study population. A consecutive sampling method was used in selecting mothers for exit interviews, while they were being discharged from the obstetric ward at Jimma University Medical Center. Purposive sampling was employed for the selection of key informants.
Data Quality Management
The tool was prepared in English and then converted into the native languages (Afan Oromo and Amharic) by both language experts, then returned to English to ensure uniformity. Data were collected from these native-language mothers’ responses to questionnaires in Afan, Oromo, and Amharic. For supervisors and data collectors, adequate training was provided regarding the collection methodologies, objectives, data collection tools, and ethical concerns. A pretest was conducted using 5% (21 clients) of the total participants in Black Lion Hospital. The entire data collection process was closely monitored and reviewed frequently by supervisors. Quantitative data entry was done using EpiData version 4.6.02, and then it was exported to SPSS version 25. Daily collected data were closely followed for consistency and completeness by the data collector together with the supervisor to correct incomplete data timely and were cleaned during and after data entry. On the other hand, appointments were made with key informants for key informants’ interviews. Information about the situation was taken in detail (both note-taking and audio recording were done through probing). The audio records were transcribed and provided back to the key informants (member check).
Data Analysis
Resource availability was analyzed and presented by using descriptive statistics. Health system responsiveness data were analyzed by using descriptive statistics, and factors determining good HSR were determined by multiple linear regression. The relationship between clients’ responsiveness and independent variables was assessed by simple linear regression. The variables with P = <0.25 were selected for simple linear regression analysis that helps to identify candidate variables for the multivariable linear regression. A multiple linear regression model was fitted to identify independent predictors associated with responsiveness of delivery service with a p-value less than 0.05 at 95% CI was considered as cutoff point and standardized β was used in interpreting after assumption for linearity, normality, independency, homogeneity of residual variance, multicollinearity, autocorrelation and outlier checked and found to be fit. The generated data were presented by texts and frequency tables. The overall level of responsiveness (as a dependent variable) was determined by the mean percentage of maximum scale score (PMSS) which was determined by the below formula (55).
For qualitative data, audio records were transcribed. Next it was translated back into English followed by coding and categorizing. Thematic analysis was done manually, and each code was divided into two themes to reason out the causes of why and how the services were as in their current status. The findings were described and triangulated with the quantitative findings.
Result
Resources Availability
Human Resources Availability
Of a total of 201 manpower, 122 were healthcare professionals, and the rest were non-healthcare workers. Of these, fifty-seven were midwives and seven midwives and residents. However, there was only one obstetrician in the obstetric ward (Supplementary Table 1).
The majority of key informants reported that there was a shortage of human resources at the obstetric ward. It was reported that the number of nurses, midwives and obstetrician were not adequate as compared to clients came for delivery service.
The staff left the hospital for searching a better life or family problems at a different time. There is an improvement in the workforce as compared to before. However, the department still needs more staff to minimize the workload and deliver quality care to mothers. [Early 35 years old male]
The staffs leave the hospital due to a lack of motivation: a chance for education, incentive in the form of payment, lack of training after serving even up to seven years and lack of duty payment timely. We have staff shortages to give more quality service as recommended. Even if we communicated human resources unit frequently, they didn’t recruit yet. [32 years old male midwife]
There is a high staff turnover rate for different reasons. Even though the number of human resources didn’t meet the standard/requirement, we are trying to work more with the available staff. However, the hospital has the plan to employ extra health professionals in future. (34 years old male ex-Nurse Director)
Infrastructures Availability for Delivery Services
There were 12 rooms and 62 beds in the available in the rooms. On the other hand, electric power was available continuously with power back up (Supplementary Table 2)
There were gaps we noticed from some attendants of mothers in way of using available infrastructures even though maintenance of building and furniture was done repeatedly. There is frequent damage to chairs, shower room accessories and beds mothers hinder mothers from taking showers at times they want. [33 years old male]
Availability of Materials Resources in Obstetric Ward
Even though the maternity unit has medical equipment that was utilized for delivery services, there were no thermometer or stethoscope for staff to follow the clients just they use the medical interns’ or residents’ owned instruments, and there were three blood pressure apparatus in the maternity ward and one in the labour ward. The supplies interruption of equipment, drugs other from two to ten days within one month noticed, were sterile gloves, intervenes (IV) cannula, syringe with needle, urinary catheter, IV fluids, 40% glucose, ceftriaxone and dexamethasone. There was no stethoscope or thermometer for staff to follow clients in their assigned beds (Supplementary Table 3).
The majority of key informants reported that there was a shortage of medical equipment and supplies required to deliver all healthcare services needed in the obstetric ward.
There is a shortage of intravenous fluids and drugs. We usually use fluids, drugs, and stitches collected from discharged mothers for those who cannot afford them. Mothers who come for delivery services can get 100% free medication and services. However, if they are stocked out, mothers are usually forced to buy from the private drug store. I don’t know the maximum number of supplies needed per mother. [48 years old female obstetrician]
Equipment and supplies like thermometers, stethoscopes, intravenous fluids and drugs were stocked out. In this ward, sometimes services were interrupted due to equipment and other supplies poor in quality, old in age and serving for a long period of, time and high caseload. [36 years old male town health bureau]
As known, this hospital is the complex one and it has many caseloads. Sometimes we faced medication & supplies stock. When we faced such events, we decided to support mothers who cannot afford for services by collecting 50 to 100 Ethiopian birrs monthly. [35 years old male town’s midwives department head]
Sometimes stock out noticed and difficult for us to manage due to some of stock out happened from misuse of supplies and inappropriate handling of equipment. The department has no guidelines to minimize wastage. [38 years old male midwives in labour unit]
The number of healthcare workers, availability of tables in the procedure room, coaches, delivery sets, caesarean sections, and laparotomies set in the obstetric ward was judged excellent. However, there was no CEmONC guideline in study settings during the study period (Table 1).
 |
Table 1 Judgment Matrix Analysis of Resource Availability in Obstetrics Ward of Jimma Medical Center, Jimma, Ethiopia |
Health System Responsiveness
Study Participants’ Socio-Demographic Characteristic Description
All participants answered the questioners which made 100% response rate. Most of participants’ age was in the range of 26–30 year with average age of 26.97 (SD ± 4.77). The majority of participants, 178 (42.2%, live in the rural area, while 140 (33.2%) of them attended primary school. Furthermore, 183 (43.4%), 290 (68.7%) and (168 (39.8%) of the participants were housewives, had two to four children, got 1651–3200 average monthly income, respectively (Table 2).
 |
Table 2 Socio-Demographic and Family Income Characteristics of Participants in the Evaluation of Responsiveness in Obstetrics Ward of JMC, Jimma, Ethiopia |
Reproductive Health History of Respondents
The majority current mode of deliveries of study participants was SVD 166 (39.3%). Episiotomy and instrumentally assisted delivery were 111 (26.3%), 15 (3.6%), respectively (Figure 2).
Health System Responsiveness of Delivery Service in JUMC
On average, 304.2 (72.1%) clients responded good and 94.2 (27.9%) of them responded poor with dignity subdimension. On the other hand, 144 (34.2%) and 277.6 (65.8%) clients were categorized under poor and good, respectively, in basic amenities (Table 3).
 |
Table 3 Health System Responsiveness Scores in Obstetrics Ward JMC, Jimma (N = 422) |
Majority of key informants approved that there were some gaps in keeping all rights of childbearing mothers or in addressing legitimate expectation of mothers while giving delivery services.
Sometimes, gaps were observed due to care provider behavior and work over load in giving service with respect. Nevertheless, the majority of staffs tried to give service with keeping all mothers rights. [40 years old male maternal and child health directorate]
The information provided to mothers is sometimes incorrect and given in susceptible manner in order to assist mothers to make the best choice on service. [25 years old husbands].
Most of the time, all privacy is maintained. However, there may be a lapse in keeping the clients’ card private because the card kept on the mother’s side, which has a chance of being seen by anyone who enters the room. [36 years old male at medical record unit]
Sometimes, there is a communication gap before, during and after giving services. Most of the time, staffs try to give service or do procedures without communicating the mother well and left the room. [35 years old mothers]
Majority of key informant said that that mothers should get prompt attention all the time and most of health care providers dedicated for such service. Nevertheless, there is a delay of service
More or less, it is good. All staffs are actively giving services for mothers on basic service and based on mothers need. However, due to shortage in supplies, services are being delayed. [28 years old husband]
Most of the mother had social supports and sometimes trafficking of attendants disturb the service unit as majority of key informant agreed.
Majority of mothers have more attendants who wants to get in as they want. But, due to fear of COVID-19, psychological impact for being alone resulted in crowded rooms that affects the service quality. Sometimes entering to the rooms was not allowed. [25 years old male attendants]
Majority of key respondents have not got chance for asking to choose the healthcare providers they want.
Mostly, mothers came from different areas. They do not know which health professionals to choose. However, who come in private wing can communicate with the senior clinicians they want before reaching this hospital by telephone. If not, the probability of getting the service by the health care providers they want is rare. [46 years old male nursing directorate]
Majority of key informant agreed that even though there was some constraint in making the physical environment/amenities more comfortable, it is improved than before.
Due to high number of mothers and attendants from different areas served here, there was supply shortage and there was even inappropriate use and handling observed from attendants of mothers. [28 years old female supporter]
Proportion of mothers who respond to the healthcare giver is kind and respectful was 85% and judged as very good. On the other hand, the proportion of women getting consultation where others cannot see, waste short time in waiting area, and get daily visitors were 75%, 74% and 72%, respectively, which were judged good, while the rest indicators were judged fair (Table 4).
 |
Table 4 Judgment Matrix Analysis of Responsiveness in Delivery Service of Jimma Medical Center, Jimma (N = 422) |
Seventeen variables had relationship with the dependent variables as checked by simple linear regression analysis. Variables with p-value of less than 0.25 were candidate for multiple linear regression. Accordingly, six variables were significantly associated with HSR (dependent variable). These variables are not attending formal education, educational level of college and above, previous place of delivery being health center, current mode of delivery being cesarean section, and occupation of clients being merchant. Occupation of clients being merchant leads to ten times decrement in HSR as compared to being housewives (β = −10, P = 0.000, 95% confidence interval (−13.758, −6.242)). On the other hand, educational level of clients being college and above leads to decrement of HSR 8.6 times as compared to attended elementary school (β = −8.6, P-value=0.001 and 95.5 confidence interval = (−13, 54,-3.74)) (Table 5).
 |
Table 5 Determinant Factors of HSR at Obstetric Ward of JMC |
Overall Judgment Matrix
Resource availability and HSR were judged as very good and fair, respectively. The overall process evaluation of health system responsiveness at obstetric ward of JMC was found to be 75.6 which was judged good (Table 6).
 |
Table 6 Overall Judgment Matrix Analysis of Evaluation of Responsiveness of Delivery Service in Jimma Medical Center |
Discussion
The study was mainly aimed to evaluate the resource availability and the process of health system responsiveness in the obstetric ward. This study evaluated the availability of resources and the health system responsiveness level under the sub-dimensions of dignity, autonomy, confidentiality, communication, prompt attention, social support, choice, and basic amenities from the perspective of mothers and key stakeholders and factors affecting the health scheme’s responsiveness in JUMC. The overall evaluation of services at the Obstetrics Ward of JUMC shows that 75.6% were judged good. This finding was greater than the study from other parts of Ethiopia.20,21 The inconsistency may be due to the fact that the current study was an evaluation and not research, and it included information on related with resources availability needed to provide the services. The final HSR measurement was made from selected indicators that were a mixture of both resources and HSR. Improving HSR can address people’s legitimate expectations, which is the heart of the stewardship function of health systems. Improving the HSR is fundamental as it relates to basic human rights. On the other hand, some of the HSR elements require only small investments, and the results of interventions to improve them may show quick results.1
The overall evaluation of resource availability was greater than eighty percent. We discovered that seven out of ten midwives and nurses on the obstetric ward were available. According to Ethiopia’s comprehensive specialized hospital suggestion, a total of 64 nurses and midwives are required in the obstetric ward.22 Our results are higher than the national guideline recommendation, which may be due to the high available number of professions trained in nursing and midwives who graduate in this country. Assigning nurses and midwives in an obstetric ward becomes expanded to execute important services in sub-Saharan Africa and strengthen related health systems. Enough nurses and midwives can reduce high workloads and fatigue, which may affect a global target to reduce maternal mortality.23
On the other hand, this study revealed that three obstetricians, 21 residents, 22 medical interns, and six anesthetists were found in the obstetric ward of JUMC. The number of obstetricians found in JUMC is higher than that suggested by Comprehensive Specialized Hospital Requirements (CSHR). This evaluation also found that the number of anesthetists found in the obstetric ward of JUMC was higher than that of anesthetists suggested by CSHR (Comprehensive Specialized Hospital Requirements).22 In the context of Ethiopia, comprehensive specialized hospitals are teaching university hospitals which have enough senior obstetricians, surgeons, internists and pediatricians, residents (who are doing their specialties) and medical and intermedical students. This is because, in Ethiopia, the number of CSHR hospitals is very limited, with maximum of one CSHR per region. This may be the reason why the number of obstetrician, anesthetics and other specialties was higher than the numbers suggested by CSHR. In general, even though the number of human resources available in the obstetric ward of JUMC is over what suggested by CSHR, still, there is an imbalance between caseload and staff availability.
From the indicator judgment, the overall HSR evaluation was found to be fair. In this study, nearly three-fourths of clients are rated as good in the dignity sub-dimension, while the lowest number of clients was rated as good in the basic amenities’ category. Other study done in Ethiopia indicated the highest percentage of clients were categorized as good in dignity and the lowest as poor in choice dimension.24 Different factors in the study setting and health facility type may affect the different results observed. Keeping patients’ dignity helps in treating them and giving them attention with good understanding when they feel vulnerable.25 Nearly seventy percent of clients in this evaluation reported that they received good autonomous treatment. Similarly, nearly three-quarters of clients reported that confidentiality, communication, prompt attention, social support, and choice were good, while they received services. However, only 65.8% reported that the basic amenities were poor.
These results were inconsistent with a study conducted in another area of Ethiopia on HIV/AIDS patients that revealed that prompt attention was the poorest one, while more than eight in ten clients reported that they got prompt attention while receiving the services (HIV/AIDS Study). Another study conducted in Tanzanian primary healthcare facilities found that the highest HSR performance was that of respecting information confidentiality, whereas the lowest HSR domain was accessibility of care.26 Good HSR is important to improve patients’ grief through compassion, sharing patients suffering, and having patients feeling. Additionally, a basic human right is to be respected during client and care provider interaction includes respecting patients’ autonomy, dignity, choices, attention, communication and choice of healthcare worker. They were an authentic showing of love and compassion to support a person-centered approach for their patients. However, the absence of HRS positive dimension could be leads to being carelessness and negligent.27 Furthermore, our result was similar to a study done in Ghana, which indicated that domains like privacy, confidentiality, dignity, and autonomy have good performance, while conducive physical environments and amenities have the lowest standard score.27 The similarity may be indicated by similarity in the target population, the study setting, or the related socioeconomic background of the target population. Another comparative study conducted in Sri Lanka shows that semi-government hospitals have good HSR than government hospitals. In the majority of sub-Saharan Africa, the public hospitals of the countries cater to all socioeconomic strata of the population and predominantly utilized by low socioeconomic groups, while the private hospitals serve both high and middle socioeconomic groups. In the majority of sub-Saharan Africa, our study setting, Ethiopia, HSR and healthcare service quality are more satisfactory to the patients and clients in private than in public hospitals.28 Similar study from Lao People’s Democratic Republic shows similar finding.29
Improved HSR has a significant input to all healthcare services that intended to increase the standard of all medical treatments. Making a framework, harmonizing policies and practices based on global experiences and local opinions, can help improve the responsiveness of the healthcare system. Additionally, improved resource allocation, staff training, patient and medical staff knowledge and attitudes, as well as process re-engineering, can all help to increase responsiveness.30
HSR is crucial to providing high-quality medical care and ought to be the foundation of the healthcare system. HSR is essential for creating a sustainable, just, and healthy future for everyone. An increasing amount of research has shown that effective HSR is linked to better health outcomes, more patient satisfaction, greater treatment adherence, fewer malpractice claims, and lower healthcare costs.31 Compassionate and respectful care (CRC), which is directly related to HSR, among clients requires a genuine act of kindness and humanity to support their patients’ person-centered practice. The absence of CRC by healthcare providers leads to negligence, ignorance, and malpractice. The CRC provides a significant benefit if life circumstances that are believed to cause burnout and tiredness are required to advance it. During healthcare services provision, the client requests consolation and treatment as a human being.32 Not attending formal education directly affects the HSR. However, study from other part of Ethiopia20 shows educational level has no effect on health system responsiveness level. Illiterate or functionally illiterate people are not critical thinkers, do not analyze problems, do not understand the complex healthcare system, and may be satisfied with a simple process or procedure.33 Our finding revealed that instrumentally assisted delivery negatively affected the HSR level, which was inconsistent with study from southern Thailand.29 Study from other part of Ethiopia34 shows that instrumentally assisted delivery affects HSR positively, and the inconsistency may be due to deference to sociocultural differences among study participants. In the current study, cesarean section was negatively associated with HSR, while a similar study done in another area of Ethiopia indicated HSR was affected positively by cesarean section.19
Strength and Weakness
This evaluation was done by a single-case study design with mixed methods of data collection process. The data from both quantitative and qualitative sources were triangulated to support each other. However, quantitative and qualitative data were collected concurrently instead of sequentially, as there was a probability of missing important points that had not been covered by the quantitative data collection method. In this evaluation, we did not use direct observation of healthcare provider and client interactions, in which more clear and informative information can be obtained.
Implications for Policy Service Delivery
Health system responsiveness directly affects health care seeking behavior and healthcare service utilization. As process quality involves the sub-dimension of health system responsiveness, healthcare workers’ performance in the area of health system responsiveness can impede or boost health care seeking behavior. Furthermore, health system responsiveness determines healthcare service quality and interpersonal component quality. On the other hand, poor health system responsiveness dissatisfies the clients, which further affects healthcare service utilization and can be linked to maternal mortality.2
Improved HSR has a significant input to all programs that intended to increase the standard of healthcare delivery system. In low- and middle-income countries, there are evidential gaps requiring further development of HSR, especially in brittle and unstable states. Furthermore, the implications of poor HSR responsiveness relate to health quality, equity, minority populations, and exposed community.35
Conclusion
The overall process of evaluation of the HSR at the obstetric ward of JMC was found to be 75.6% and judged good. The resource availability evaluation was at 84.5%, which was judged very good. On the other hand, the evaluation of health system responsiveness was 69.7%, which was judged fair. Educational level (not attending formal education and attending college and above), previous giving birth at health center, cesarean delivery, instrumental delivery, and being a merchant significantly affect the HSR. Efforts should be made to provide stocked out supplies to increase HSR, as this has a direct influence on the quality of healthcare services.
Abbreviations
ANC, antinatal care; CEmONaC, comprehensive emergency obstetric and newborn care; CRC, compassionate and respectful care; CSHR, Comprehensive Specialized Hospital Requirements; EHRIG, Ethiopian Hospital Reform Implementation Guideline; HSR, health system responsiveness; JUMC, Jimma University MedicalCenter; PMSS, percentage mean of maximum scale score; SPSS, Statistical Package for the Social Sciences; SVD, spontaneous vaginal delivery; WHO, World Health Organization.
Data Sharing Statement
Supporting data for this evaluation were available from the corresponding author and will be provided with reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Review Board (IRB) of Jimma University Institute of Health with reference number of IHRPGY/57/21 which was in lined with Helsinki declaration. The supportive letter to JUMC was written and taken from Jimma University, Faculty of Public Health, Department of Health Policy and Management. Jimma University Medical Center chief clinical director refer the supportive letter to all concerned bodies in support of data collection process. Informed oral consents were taken which was approved by IRB of Jimma University. In order to preserve participant rights, data collectors read an informed consent attached to each questionnaire, all study participants were requested to engage in the study based on their interest by clarifying about the purpose of this evaluation. Furthermore, each data collectors explained to each participant that their response will be published without identifying their name and other personal identities. Their respect, anonymity and confidentiality were given, and their importance of involvement and the freedom to withdraw at any point of the interview were discussed well.
Acknowledgment
We thank Jimma University Institute of Health for sponsoring the evaluation and Jimma University, Department of Health Policy and Management, for its technical facilitation to conduct the evaluation. Also, we thank JUMC administrative bodies and all staffs who were working in obstetric unit for their cooperation and technical support during the whole evaluation period.
Author Contributions
All authors made a significant contribution to this work, whether that is in the conception, study design, execution, acquisition of data, data analysis and interpretation, or in all these areas. They also played a significant role in drafting or writing, substantially, revising or critically reviewing the article, agreeing on the journal to which the article was submitted, reviewing and agreeing on all versions of the article before submission, during revision. The final version accepted for publication, and any significant changes introduced at the proofing stage agree to take responsibility and be accountable for the contents of the article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Darby C, Valentine N, De Silva A, Murray CJ. World Health Organization (WHO): Strategy on Measuring Responsiveness. World Health Organization; 2003.
2. De Silva A, Valentine N. A Framework for Measuring Responsiveness. Geneva: World Health Organization; 2000.
3. Alliance WR. Respectful Maternity Care: The Universal Rights of Childbearing Women. White Ribbon Alliance; 2011:1–6.
4. Vogel JP, Bohren MA, Tunçalp Ӧ, Oladapo OT, Gülmezoglu A. Promoting respect and preventing mistreatment during childbirth. BJOG. 2016;123(5):671. doi:10.1111/1471-0528.13750
5. Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384(9948):e42–e4. doi:10.1016/S0140-6736(14)60859-X
6. Thi Thu Ha B, Mirzoev T, Morgan R. Patient complaints in healthcare services in Vietnam’s health system. SAGE Open Med. 2015;3:2050312115610127. doi:10.1177/2050312115610127
7. Yakob B, Ncama B. Measuring health system responsiveness at facility level in Ethiopia: performance, correlates and implications. BMC Health Serv Res. 2017;17:17. doi:10.1186/s12913-016-1946-9
8. Ababa A. Competency Based National Comprehensive PMTCT/MNCH Training Participant’s Manual. Federal Ministry of Health (FMoH); 2017.
9. Mengesha MB, Desta AG, Maeruf H, Hidru HD. Disrespect and abuse during childbirth in Ethiopia: a systematic review. Biomed Res Int. 2020;2020. doi:10.1155/2020/8186070
10. Sheferaw ED, Bazant E, Gibson H, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health. 2017;14(1):1–12. doi:10.1186/s12978-017-0323-4
11. Tekle Bobo F, Kebebe Kasaye H, Etana B, Woldie M, Feyissa TR. Disrespect and abuse during childbirth in Western Ethiopia: should women continue to tolerate? PLoS One. 2019;14(6):e0217126. doi:10.1371/journal.pone.0217126
12. Asefa A, Morgan A, Gebremedhin S, et al. Mitigating the mistreatment of childbearing women: evaluation of respectful maternity care intervention in Ethiopian hospitals. BMJ open. 2020;10(9):e038871. doi:10.1136/bmjopen-2020-038871
13. Siraj A, Teka W, Hebo H. Prevalence of disrespect and abuse during facility based child birth and associated factors, Jimma University Medical Center, Southwest Ethiopia. BMC Pregnancy Childbirth. 2019;19:1–9. doi:10.1186/s12884-019-2332-5
14. Bante A, Teji K, Seyoum B, Mersha A. Respectful maternity care and associated factors among women who delivered at Harar hospitals, eastern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20:1–9. doi:10.1186/s12884-020-2757-x
15. Ogaji DS, Egu CB, Nwakor-osaji M, Smart AC, Anyiam EF, Diorgu FC. Responsiveness of primary health care services in Nigeria: the patients’ perspective. Patient Exp J. 2020;7(3):146–154. doi:10.35680/2372-0247.1458
16. Mezmur M, Navaneetham K, Letamo G, Bariagaber H. Socioeconomic inequalities in the uptake of maternal healthcare services in Ethiopia. BMC Health Serv Res. 2017;17(1):1–11. doi:10.1186/s12913-017-2298-9
17. Sumankuuro J, Crockett J, Wang S. Perceived barriers to maternal and newborn health services delivery: a qualitative study of health workers and community members in low and middle-income settings. BMJ Open. 2018;8(11):e021223. doi:10.1136/bmjopen-2017-021223
18. FMOH. Health Sector Transformation Plan II (HSTP II) 2020/21–2024/25. FMOH; 2021.
19. Wassihun B, Zeleke SJ. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth. 2018;18:1–9. doi:10.1186/s12884-018-1909-8
20. Abdo RA, Halil HM, Kebede BA, et al. Health system responsiveness in maternity care at Hadiya Zone public hospitals in Southern Ethiopia: users’ perspectives. PLoS One. 2021;16(10):e0258092.
21. Asefa G, Atnafu A, Dellie E, et al. Health system responsiveness for HIV/AIDS treatment and care services in Shewarobit, North Shewa Zone, Ethiopia. Patient Prefer Adherence;2021. 581–588. doi:10.2147/PPA.S300825
22. EFMHACA. Ethiopia Specialized Hospital. Ethiopia: Ethiopian Standard Agency; 2012.
23. World Health Organization. The Extension of the 2025 Maternal, Infant, and Young Child Nutrition Targets to 2030. UNICEF; 2018.
24. Negash WD, Tsehay CT, Yazachew L, Asmamaw DB, Desta DZ, Atnafu AJ. Health system responsiveness and associated factors among outpatients in primary health care facilities in Ethiopia. BMC Health Serv Res. 2022;22(1):249. doi:10.1186/s12913-022-07651-w
25. Simões Â, Sapeta PJ. The concept of dignity in nursing care: a theoretical analysis of the ethics of care. Rev Bioet. 2019;27:244–252. doi:10.1590/1983-80422019272306
26. Baker T, Lugazia E, Eriksen J, Mwafongo V, Irestedt L, Konrad DJ. Emergency and critical care services in Tanzania: a survey of ten hospitals. BMC Health Serv Res. 2013;13:1–9. doi:10.1186/1472-6963-13-140
27. Emmanuel K, Srofenyoh EHO, Roger A. Mother’s perception of responsiveness of labour and delivery services in first referral facilities in Ghana. Int J Health Sci Res. 2017;2:3.
28. Taner T, Antony JJ. Comparing public and private hospital care service quality in Turkey. Leadersh Health Serv. 2006;19(2):1–10. doi:10.1108/13660750610664991
29. Douangvichit D, Liabsuetrakul TJ. Obstetric care and health system responsiveness for hospital-based delivery in Lao People’s Democratic Republic. J Med Assoc Thail. 2012;95(9):1126.
30. Ebrahimipour H, Najjar AV, Jahani AK, et al. Health system responsiveness: a case study of general hospitals in Iran. Int J Health Policy Manag. 2013;1(1):85. doi:10.15171/ijhpm.2013.13
31. Jemal K, Samuel A, Geta A, et al. Evaluation of compassionate and respectful care implementation status in model healthcare facilities: a cross-sectional study. Arch Public Health. 2022;80(1):84. doi:10.1186/s13690-022-00845-y
32. Jemal K, Hailu D, Mekonnen M, Tesfa B, Bekele K, Kinati TJJo PH. The importance of compassion and respectful care for the health workforce: a mixed-methods study. J Public Health. 2021;2021:1–12.
33. Andrus MR, Roth HP, Therapy D. Health literacy: a review. Pharmacotherapy. 2002;22(3):282–302. doi:10.1592/phco.22.5.282.33191
34. Gashaye KT, Tsegaye AT, Shiferaw G, Worku AG, Abebe SM. Client satisfaction with existing labor and delivery care and associated factors among mothers who gave birth in university of Gondar teaching hospital; Northwest Ethiopia: institution based cross-sectional study. PLoS One. 2019;14(2):e0210693. doi:10.1371/journal.pone.0210693
35. Khan G, Kagwanja N, Whyle E, et al. Health system responsiveness: a systematic evidence mapping review of the global literature. Int J Equity Health. 2021;20(1):1–24. doi:10.1186/s12939-021-01447-w
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


