Back to Journals » Pathology and Laboratory Medicine International » Volume 14
Primary Intraosseous Meningioma: Bifrontal Skull Mass
Authors Dires Fenta B , Israel Korga T , Dinka Bikila T , Kassahun Tadele A , Lijalem Yigezu B, Gosa Negash M
Received 31 August 2022
Accepted for publication 2 December 2022
Published 7 December 2022 Volume 2022:14 Pages 25—31
DOI https://doi.org/10.2147/PLMI.S388172
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Paul Zhang
Bizunesh Dires Fenta,1 Tesfalem Israel Korga,2 Tuji Dinka Bikila,1 Abraham Kassahun Tadele,1 Berhanu Lijalem Yigezu,2 Mikiyas Gosa Negash3
1Department of Pathology, Hawassa University Comprehensive Specialized Hospital, Hawassa, Sidama, Ethiopia; 2Department of Pathology, Wolaita Sodo University Comprehensive Specialized Hospital, Wolaita Sodo, SNNP, Ethiopia; 3Department of Public Health, Universite’ Libre de Bruxelles, Brussels, Belgium
Correspondence: Tesfalem Israel Korga, Tel +251912052945, Email [email protected]
Abstract: Primary intraosseous meningioma is a rare tumor arising commonly from the calvarial bone. Here, we report a case of primary intraosseous meningioma which presented as a Bifrontal skull mass in a 30-year-old woman who presented with a progressive forehead enlargement and headache of 3 years duration. Brain CT shows hyperostosis of the frontal bone and microscopy shows intertrabecular syncytial proliferation of oval to spindle cells at the area forming whorl. Even though it is rare, PIM is the most common subtype of extradural meningioma.
Keywords: bifrontal, PIM, calvarium, meningioma
Introduction
Meningioma is classified into three: primary neuraxial meningioma the commonest type arising within neuraxis, primary extra neuraxial meningioma arising outside of neuraxis, and secondary meningioma which metastasized from elsewhere.17 A primary intraosseous meningioma is a form of primary extradural meningioma that arises from the bone. It represents the most common form of primary extradural meningioma though it constitutes around 2% of meningiomas overall. Tumors originating from the calvaria usually present with swelling, nonspecific pain, and loss of vision depending on the site of their origin.2–4 Due to the diverse radiologic features, distinguishing them from their mimickers usually requires additional histopathologic workup.3–5 The lack of a clear and standardized definition made primary intraosseous meningioma a topic of confusion. According to Arana et al, it is best defined as a meningioma with the largest component contained within the Calvarium with no or only minimal dural involvement.6 Till the year of 2015, only 100 primary intraosseous meningioma cases were reported.7
Case Report
A 30-year-old female patient presented with a global throbbing headache and progressive forehead swelling of 4 years duration. She has a heavy sensation upon opening her both eyes. She has no history of head trauma and neurologic symptoms. On physical examinations, she has a 15x15cm hard, non-tender, hard Bifrontal mass with grossly intact cranial nerves (Figure 1).
 |
Figure 1 15x15cm hard bifrontal skull mass. |
CT scan shows hyperostosis of the frontal bone with a well-defined outline measuring 2.2 cm at its maximum thickness. The diploic space is obliterated and replaced by a less dense matrix (ground glass matrix). Both the inner and outer tables of the frontal bone are involved, and the lesion extended to almost all frontal bone being thick at the center and decreasing bilaterally in a symmetric fashion. Overlying forehead soft tissue thickness is also increased paralleling the bone lesion (Figures 2–5).
 |
Figure 2 CT scan (the bone window) shows hyperostosis of the frontal bone with a well-defined outline measuring 2.2 cm at its maximum thickness. |
 |
Figure 3 CT scan of the head showing the thickening of the overlying forehead soft tissue and increased paralleling bone lesions. |
 |
Figure 4 Left lateral view of the CT scan of the head with 3D reconstruction showing the bifrontal mass. |
 |
Figure 5 Superior view of the CT scan of the head with 3D reconstruction showing the bifrontal mass. |
Complete excision of the tumor with a clear surgical margin and cranioplasty was done. The specimen was sent for histopathologic evaluation.
Grossly, 13 x 12cm slightly irregular Bifrontal calvarial bone with 1.5–3 cm thickness and two separate irregular skin tissues larger measuring 13 x 8cm, smaller measuring 10×2 cm were submitted (Figure 6A and B).
Histopathologic evaluation of fixed and decalcified tissue showed thickened lamellar and woven bone cuffing whorl and syncytium of oval to spindle meningothelial cells confined to the dura and bony components with no soft tissue invasion or extension (Figures 7 and 8).
 |
Figure 7 (A and B) Microscopic picture on 10/HPF showing thickened lamellar and woven bone cuffing whorl and syncytium of oval to spindle meningothelial cells. |
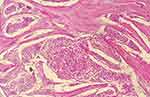 |
Figure 8 Microscopic picture on 40/HPF showing whorls and syncytium of oval to spindle meningothelial cells. |
Immunohistochemistry also shows nuclear pattern positivity for progesterone (Figure 9A and B).
 |
Figure 9 (A and B) Immunostaining for progesterone shows a nuclear pattern of staining. |
Discussion
Meningioma is the most common benign primary intracranial tumor comprising a fifth of all tumors of the same category.1 They are slowly growing Dura-based tumors and typically they originate from arachnoid cap cells with a high chance of cure.19 Sometimes it can also arise from the scalp, orbit, paranasal sinus, neck, and skin.8 Ectopic or extra-dural primary meningioma accounts for about 2% of all meningiomas.9 Calvaria is involved in 68% of primary extradural meningioma with frontotemporal and orbital regions being the most involved.10,11 It has bimodal peak incidence with one peak in the second decade and a second peak during the fifth through seventh decades of life with slight female preponderance. The tumors are nearly uniformly solitary, although a small number of case reports have presented patients with two separate lesions.
Primary intraosseous meningioma may exhibit osteoblastic, osteolytic, or mixed patterns of growth with the osteoblastic pattern being the most common accounting for around 58% of all cases.11–13 Based on the location of proliferation, primary extradural tumors are classified as: purely extra calvarial (Type I), purely calvarial tumors (Type II), and calvarial tumors with extra calvarial extension (Type III). Type II and III are further sub-classified as C or B subtypes based on their anatomical location.10,14
Histopathologically, there are 15 WHO-recognized morphologic variants though more emphasis is given to the tumor grade regardless of the subtype. There are 3 grades according to the WHO with WHO grade 1 being under the benign category and comprising 2/3rd of the subtypes, and WHO grade 2 and grade 3 are characterized by recurrence and potential for metastasis, respectively.18
Like conventional meningioma, PIOM can have any of the histologic subtypes and is positive for EMA, PR, SSTR2a, and vimentin. In one study, progesterone is found to be positive in 87% of low-grade meningiomas as in our case.9,22
Management options include complete excision with a wide free margin with subsequent cranioplasty or decompression of tumor near vital structures that is difficult to resect, and adjuvant chemotherapy or radiation can also be given in incomplete resection. In our case, complete excision with a wide free margin with subsequent cranioplasty was done. The patient is stable, and no problem was reported in the last 4 months.
Prognosis is generally good for completely excised lesions with free margin whereas, atypical primary intraosseous meningioma carries around 21% risk of recurrence.
Osteoma, osteoblastoma, fibrous dysplasia, and Paget disease of the bone can radiographically mimic PIOM with osteoblastic growth pattern, whereas, plasma cell tumors, Langerhans cell histiocytosis, lymphomas, and metastatic skull tumors can mimic osteolytic counterparts.15,16 Detailed clinical evaluation, imaging, and histopathologic evaluation are the mainstay method to distinguish one from the other. Moreover, new instrumental exams and tools should be investigated to possibly improve the detection and management of PIOMs.20,21
Conclusion
Primary intraosseous meningioma is a rare tumor, and it should be taken into consideration in a patient with calvarial mass. Imaging and histopathology are the main means of definitive diagnosis.
Data Sharing Statement
The data used to support the findings of this study will be available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Informed consent was obtained from the patient for the publication of this case report and accompanying images. The study is also approved by the institutional board review of Hawassa University College of medicine and health science.
Acknowledgments
The authors would like to acknowledge all the managing teams who are directly or indirectly involved in the management of this patient and the accomplishment of this case report.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This paperwork did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
All authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
1. Omofoye OA, Huynh T, Jhun R, Ashfaque H, Cronk K. Primary intraosseous meningioma of the calvarium: a systematic review. Clin Neurol Neurosurg. 2020;199:106283. doi:10.1016/j.clineuro.2020.106283
2. Butscheidt S, Ernst M, Rolvien T, et al. Primary intraosseous meningioma: clinical, histological, and differential diagnostic aspects. J Neurosurg. 2019:1–10. PMID: 31226688. doi:10.3171/2019.3.JNS182968
3. Adler C-P, Kozlowski K. Primary Bone Tumours and Tumourous Conditions in Children: Pathological and Radiological Diagnosis. Berlin: Springer; 1993:129–139.
4. Gibson SE, Paryson RA. Primary skull lesions in the pediatrics populations: a 25 years’ experience. Arch Pathol Lab Med. 2007;131:761–766. doi:10.5858/2007-131-761-PSLITP
5. McGuire TP, Palme CE, Perez-Ordonez B, Gilbert RW, Sandor GK. primary intraosseous meningioma of calvaria; analysis of the literature and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endoc. 2007;104:e34–41. doi:10.1016/j.tripleo.2007.03.023
6. Zagzag D. Russell, and rubinstein’s pathology of tumors of the nervous system. J Neuropathol Exp Neurol. 2007;66:22.
7. Yun JH, Lee SK. primary osteolytic intraosseous atypical meningioma with soft tissue and dural invasion: report of a case and review of literatures. J Korean Neurosurg Soc. 2014;56:509–512. doi:10.3340/jkns.2014.56.6.509
8. Craig WM, Gogela LJ. Intraorbital meningiomas; a clinicopathologic study. Am J Ophthalmol. 1949;32:1663–1680. doi:10.1016/S0002-9394(49)90807-7
9. Marwah N, Gupta S, Marwah S, Singh S, Kalra R, Arora B. Primary intraosseous meningioma. Indian J Pathol Microbiol. 2008;51(1):51–52. PMID: 18417855. doi:10.4103/0377-4929.40396
10. Lang FF, Macdonald OK, Fuller GN, DeMonte F. Primary extradural meningiomas: a report on nine cases and review of the literature from the era of computerized tomography scanning. J Neurosurg. 2000;93(6):940–950. PMID: 11117866. doi:10.3171/jns.2000.93.6.0940
11. Ahmed N, Ferini G, Haque M, et al. Primary intraosseous osteolytic meningioma with aggressive clinical behaviour: clinico-pathologic correlation and proposed new clinical classification. Life. 2022;12(4):548. doi:10.3390/life12040548
12. Agrawal V, Ludwig N, Agrawal A, Bulsara KR. Intraosseous intracranial meningioma. AJNR Am J Neuroradiol. 2007;28(2):314–315. PMID: 17297003; PMCID: PMC7977404.
13. Crawford TS, Kleinschmidt-DeMasters BK, Lillehei KO. Primary intraosseous meningioma. Case report. J Neurosurg. 1995;83(5):912–915. PMID: 7472564. doi:10.3171/jns.1995.83.5.0912
14. Halpin SF, Britton J, Wilkins P, Uttley D. Intradiploic meningiomas. A radiological study of two cases confirmed histologically. Neuroradiology. 1991;33(3):247–250. PMID: 1881543. doi:10.1007/BF00588227
15. Ghobashy A, Tobler W. Intraosseous calvarial meningioma of the skull presenting as a solitary osteolytic skull lesion: case report and review of the literature. Acta Neurochir. 1994;129(1–2):105–108. PMID: 7998488. doi:10.1007/BF01400883
16. Hećimović I, Dmitrović B, Rubin O, Rukovanjski M, Vranković D. Skull osteolysis after mild head trauma: case report. Surg Neurol. 1999;51(1):43–46. PMID: 9952122. doi:10.1016/s0090-3019(98)00010-x
17. Daffner RH, Yakulis R, Maroon JC. Intraosseous meningioma. Skeletal Radiol. 1998;27(2):108–111. PMID: 9526778. doi:10.1007/s002560050347
18. Louis DN, Perry A, Wesseling P, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021;23(8):1231–1251. PMID: 34185076; PMCID: PMC8328013. doi:10.1093/neuonc/noab106
19. Ahmed N, Ferini G, Hossain MA, et al. Evaluation of surgical cleavage plane by preoperative magnetic resonance imaging findings in adult intracranial meningiomas. Life. 2022;12(4):473. PMID: 35454964; PMCID: PMC9025407. doi:10.3390/life12040473
20. Palmisciano P, Watanabe G, Conching A, et al. The role of [68Ga]Ga-DOTA-SSTR PET radiotracers in brain tumors: a systematic review of the literature and ongoing clinical trials. Cancers. 2022;14(12):2925. PMID: 35740591; PMCID: PMC9221214. doi:10.3390/cancers14122925
21. Brunasso L, Ferini G, Bonosi L, et al. A spotlight on the role of radiomics and machine-learning applications in the management of intracranial meningiomas: a new perspective in neuro-oncology: a review. Life. 2022;12(4):586. PMID: 35455077; PMCID: PMC9026541. doi:10.3390/life12040586
22. Baxter DS, Orrego A, Rosenfeld JV, Mathiesen T. An audit of immunohistochemical marker patterns in meningioma. J Clin Neurosci. 2014;21(3):421–426. PMID: 24231566. doi:10.1016/j.jocn.2013.06.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

