Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Prevalence and Risk Factors of Diabetes in Patients with Active Pulmonary Tuberculosis: A Cross-Sectional Study in Two Financially Affluent China Cities
Authors Li J, Zhao Y , Jiang Y , Zhang Y, Zhang P , Shen L, Chen Z
Received 18 November 2023
Accepted for publication 23 February 2024
Published 2 March 2024 Volume 2024:17 Pages 1105—1114
DOI https://doi.org/10.2147/DMSO.S450507
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Jing Li,1,* Yanhong Zhao,2,* Youli Jiang,3 Ying Zhang,4 Peize Zhang,1 Lingjun Shen,2 Zijiao Chen1
1Department of Pulmonary Medicine and Tuberculosis, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong, People’s Republic of China; 2Department of Tuberculosis, the Third People’s Hospital of Kunming, Kunming, Yunnan, People’s Republic of China; 3Department of Neurology, People’s Hospital of Longhua, Shenzhen, 518109, People’s Republic of China; 4Department of Endocrinology, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zijiao Chen; Lingjun Shen, Email [email protected]; [email protected]
Background: Tuberculosis (TB) and diabetes mellitus (DM) present a dual burden to public health. The screening of DM in TB patients may aid in the early detection and management of diabetes, ultimately improving treatment outcomes for those with the comorbidity of TB-DM. We aim to examine the prevalence and identify risk factors of diabetes in individuals with active pulmonary tuberculosis (PTB) in financially affluent China cities.
Methods: A cross-sectional survey was conducted in adult patients with highly suspected TB in two cities of China, spanning from May 9, 2023, to June 30, 2023. We compare the clinical characteristics, nutrition status, fasting blood glucose (FBG) level, living style, and knowledge of TB and DM at admission between patients with and without DM. Univariate and multivariate logistic regression analyses were employed to identify risk factors associated with TB-DM comorbidities.
Results: Of the 322 patients diagnosed with pulmonary tuberculosis (PTB), 54 individuals (16.8%) had comorbid diabetes mellitus (DM). This included 43 males (13.4%) and 11 females (3.4%). The average age was 55.44 ± 12.36 in DM patients and 46.09 ± 16.87 in non-DM patients. A multivariate logistic regression analysis revealed that male (adjusted odds ratio [aOR]=3.29, 95% confidence interval [CI]: 1.05– 10.30), age older than 47 years (aOR = 1.04, 95% CI: 1.01– 1.07), having a family history of diabetes (aOR = 5.09, 95% CI: 1.28– 20.32), and an elevated random blood glucose level (aOR = 1.6, 95% CI: 1.38– 1.86) were risk factors for DM in patients with PTB. Furthermore, it was found that diabetes awareness (aOR = 0.07, 95% CI: 0.03– 0.21) and zero, light to moderate alcohol consumption were associated with a lower risk of diabetes.
Conclusion: Diabetes is prevalent in patients with active PTB. Screening and raising awareness of DM are recommended, particularly in men after middle age with a family history of diabetes and elevated random blood glucose. Early diagnosis of diabetes and effective diabetes prevention may reduce the dual burden of TB–DM comorbidity.
Keywords: tuberculosis, diabetes, risk factors, diabetes awareness, waist-to-hip ratio, alcohol consumption
Introduction
Tuberculosis (TB) and diabetes mellitus (DM) pose a dual burden to public health worldwide. There were an estimated 10·6 million people living with TB and 537 million adults (20–79 years) with DM in 2021.1,2 The World Health Organization (WHO) advocates for collaborative efforts towards TB and DM as crucial components of the End TB strategy.3 China is a country suffering from rapidly emerging type 2 diabetes. It is estimated that approximately one in every eleven adults is currently suffering from diabetes mellitus.4 Additionally, China is also one of the high TB burden countries. A systematic review reported a near 15% prevalence of DM in TB patients, and a significantly higher prevalence of comorbidity of DM and pulmonary TB in countries with a high TB burden.5,6 As a major risk factor of TB, DM affects TB at multiple levels in disease control and treatment efficacy. Many studies demonstrated the unfavorable outcomes of TB in patients with diabetes.7,8 Screening DM in TB patients may aid in early detection and management of diabetes, preventing delayed diagnosis and diabetes-related complications and improve TB treatment outcomes accordingly.9
Our study aims to understand the prevalence of diabetes in patients with active pulmonary tuberculosis (PTB), as well as to identify risk factors of diabetes in PTB patients in financially affluent Chinese cities. We expect the findings of this study to benefit the design of diabetes screening programs for the early detection and management of diabetes in patients with PTB in cities.
Methods
Study Design and Sample Size Estimation
Shenzhen is a special administrative region and enjoys a prime geographic location with high GDP in the past 20 years. It is a big city with estimated 13 million residents in 2022.10 Kunming is the capital of the Yunnan province with fast financial development. Estimated residents was 4.7 million in 2022.11 These two cities are characterized by a relatively financially affluence. All patients who are doubted with TB are sent to the designated hospital for further confirmation and care. We conducted a cross-sectional facility-based study targeting adult in-patients suspected of having tuberculosis (TB) at the Third People’s Hospital of Kunming and the Third People’s Hospital of Shenzhen, both of them are designated hospital for TB.
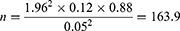
The prevalence of diabetes among tuberculosis patients is estimated to be 12%. Assuming we want to estimate the true prevalence of diabetes with a 95% confidence level and a 5% margin of error, we use the following formula to calculate the sample size:
where n is the sample size, Z is the quantile of the standard normal distribution corresponding to the confidence level, p is the expected prevalence, q is 1− p, and d is the allowable margin of error. Substituting the known parameters into the formula, we can get the result below:
That is to say, we need to survey at least 164 tuberculosis patients to estimate the true prevalence of diabetes with a 95% confidence level and a 5% margin of error. As about 20% of patients came to the designated TB hospital finally ruled out TB, the sample size will be up to 196 cases patients.
Participants and Screening of DM
The study was conducted from May 1, 2023, to June 30, 2023. We thus included a total of 410 hospitalized patients (169 from Shenzhen, 241 from Kunming respectively). All participants were screened for DM. For every patient, fingerstick blood was attained for random blood glucose test at the day of admission. Fasting blood glucose (FBG) level and Hb1Ac were tested the next day morning after admission. A confirmed diagnosis of diabetes was defined as Hb1Ac level >6.5% for both preexisting and newly diagnosed cases.12 When unequivocal hyperglycemia or borderline elevated Hb1Ac was observed, another blood sample obtained at 2 hours after meal was collected for glycemic monitoring for confirmed diagnosis. To identify the potential factors influencing TB-DM, all participants underwent a nutrition evaluation and diabetes mellitus (DM) screening. The participants were asked to complete a questionnaire on their lifestyle and knowledge of TB and DM at admission. Both non-TB and extrapulmonary TB cases were excluded from the study. Ultimately, a total of 322 patients with active pulmonary TB were included in the analysis. Among them, 54 (16.8%) patients were confirmed to have comorbid PTB-DM, while 268 (83.2%) patients had PTB alone. (Figure 1).
 |
Figure 1 Flowchart of the study. |
Key Definitions
Our study collected information on various demographic characteristics, including sex, age, education level, marital status, lifestyle, social insurance coverage, etc. Additionally, we gathered information on medical history, family history of diabetes, diabetes screening tests, and nutrition status. Alcohol consumption was categorized based on the WHO’s definition, with a standard drink being defined as 10 grams alcohol in China.13 Individuals consuming less than a standard drink in the past month were classified as non-alcohol users, 1–3 drinks as mild-alcohol users, 4–6 drinks as moderate-alcohol users, and >6 drinks in a month as heavy-alcohol users. According to the guideline for nutrition screening launched in 2023,14 the nutritional impairment status of an individual is defined as follows: 1) Absent: BMI greater than 18.5, no significant change in body weight in the past three months, no significant change in food intake in the past week. 2) Mild: Body weight loss greater than 5% in the past three months, food intake reduced by 25%–50% in the past week. 3) Moderate: Body weight loss greater than 5% in the past two months, food intake reduced by 51%–75% in the past week. 4) Severe: Body weight loss greater than 5% in the past month and greater than 15% in the past three months, BMI less than 18.5 with poor general clinical condition, food intake reduced by 76%–100% in the past week. Following WHO’s recommendations, Waist-to-Hip Ratio (WHR) ≥ 0.85 for females and ≥0.90 for males were used to define abdominal obesity.15 In addition, our questionnaire covered questions on individuals’ disease awareness.
Statistical Analysis
We conducted an extensive statistical analysis in SPSS version 25 to explore diabetes risk factors among tuberculosis patients while assessing their nutritional status. Beginning with a detailed descriptive analysis of patient characteristics and clinical data, we reported numerical variables as means with standard deviations (SDs) and medians with interquartile ranges (IQRs). Categorical variables were expressed in frequencies and percentages. We employed the chi-square (χ²) test to uncover distinctions in categorical variables. To investigate potential diabetes risk factors, we performed meticulous univariate logistic regression analyses, retaining variables with χ²-test outcomes of P < 0.05 for further scrutiny. Building on these findings, we subjected significant results from the univariate analysis to a binary stepwise logistic regression, systematically assessing variable roles within the risk factors. All presented outcomes were derived from two-tailed tests, adhering to established scientific research standards. Significance levels were conservatively set at p < 0.05, aligning seamlessly with accepted norms of scientific discourse.
Results
Basic Characteristics Between the Two Groups
Baseline demographic and clinical characteristics of the 322 patients included in the study were presented in Table 1. The DM group had a median age of 55.44 ± 12.36 years and was consisted of 43 (79.6%) males. In the non-DM group, the median age was 46.09 ± 16.87 years and 160 (59.7%) of them were male. A significant gender and age difference between the two groups was observed (P < 0.001). It was also noted that patients in the DM group had a higher alcohol consumption and lower education level (P < 0.05). No significant differences were observed between the two groups in marital status, cough, fever, and BCG vaccination coverage (P > 0.05).
 |
Table 1 Sociodemographic Characteristics of PTB Patients with and without Diabetes |
Nutrition Status and Disease Awareness Between the Two Groups
In the DM group, the mean body weight was 58.32 ± 10.27 kg. The mean waist circumference was 80.26 ± 13.69 cm, with 50% (27/54) participants attaining a normal WHR. In the non-DM group, the mean body weight was 54.55 ± 10.63 kg. The mean waist circumference was 76.66 ± 9.91 cm and the proportion of normal WHR was 69.4% (186/268). In comparison, body weight, waist circumference, and waist-hip ratio (P < 0.05) showed a statistically significant difference between the two groups. The mean random blood glucose (RBG) was 12.28 mmol/L in DM group and was 6.53 in non-DM group. The fasting blood glucose (FBG) was 8.12 mmol/L in DM group and was 5.10 in non-DM group. In addition to the RBG and FBG, family history of diabetes and DM awareness were different between the two groups (P < 0.05). Of note, the nutritional impairment score and BMI on admission showed no difference between the two groups (P = 0.184). (Table 2)
 |
Table 2 Nutrition Status and Disease Awareness of PTB Patients with Diabetes and Without Diabetes |
Risk Factors of Diabetes in Patients with Active PTB
Multivariable logistic regression analysis results are shown in Table 3. The OR value shows that male has a 3.29 times higher risk of developing DM than female. Patients with a family history of diabetes also have a higher risk than those without (aOR = 5.09, 95% CI: 1.28–20.32). And for every year of age increase, the risk of diabetes increases by 1.04 times. For every unit increase in random blood glucose, the risk of diabetes increases by 1.6 times. Diabetes awareness is a protective factor for lowering the occurrence of diabetes (aOR = 0.07, 95%:0.03–0.21). Compared to patients with heavy alcohol consumption, zero and light to moderate alcohol consumption are protective factors for DM (Figure 2).
 |
Table 3 Multivariable Analysis of the Predictors of DM |
 |
Figure 2 Adjusted odds ratios of risk factors of DM in patients with PTB. |
Discussion
Our study found that about 15% of PTB patients also had DM, with a majority being middle-aged males. Excessive alcohol use, a family history of diabetes, elevated random blood glucose, and lack of awareness of diabetes were the risk factors for these co-morbid patients.
As a risk factor of TB, the prevalence of DM in TB patients has been widely researched. A systematic review from South Asia showed a 21% pooled prevalence of diabetes in TB patients.8 A cross-sectional study from Yemen showed that DM was prevalent in 18% of the TB patients.16 Other studies indicated that up to about one-third of TB patients in India and Brunei Darussalam also had diabetes.17,18 The percentage differences among them might be due to the socio-economic characteristics of the studied population in each study. Notably, there has been a drastic rise in the prevalence of DM worldwide, particularly in South Asia, over the past three decades.19 We believe that the increasing trend of TB-DM will persist until the risk factors of DM are addressed.
In our study, we found that most TB-DM patients were men aged 47 years old or older, consistent with the results from the studies in Brunei and Yemen, which also reported a higher prevalence of TB-DM in males than in females.16,17 Additionally, findings of numerous studies in Denmark, Pakistan, and India showed a higher prevalence of TB-DM among those aged ≥45 years old.20–22 We attributed the higher prevalence of DM in older people to a decreased immunity and age-related frailty, making this population more vulnerable to developing TB.
Of note, we found that about one-third of TB-DM patients were newly diagnosed with DM. They had no history of diabetes and lacked awareness of the disease. It is reported that about 8.1% people in China has undiagnosed diabetes.23 Most of these patients are unaware of DM. As the family history of diabetes is a risk factor for TB-DM patients,16 education on tuberculosis and diabetes is pivotal in raising awareness in the public, particularly those with a family history of the diseases, in prevention, early diagnosis, and treatment. Enhancing the awareness of DM and living a healthy lifestyle help people from suffering of type 2 DM, so as to reduce the complications of diabetes and the incidence of tuberculosis.
As consumptive disease, TB often leads to malnutrition which in turn aggravates TB itself. Diabetes is a metabolic disease often leads to unbalanced nutrition. In our study, we found that the nutritional impairment score, BMI and Upper arm circumference were similar in patients with and without DM on admission. All these commonly used indicators for reflecting nutritional status were no difference. But we noticed that elevated WHR is more commonly seen in patients with DM-TB, though the correlation between WHR and DM was weak and there was no independent correlation in multiple linear regression analysis. Waist-to-hip ratio (WHR) adjusted for body mass index (BMI) had been used as an index of abdominal obesity and been demonstrated to be associated with the development of DM and coronary heart diseases.24 Abdominal adiposity was more commonly seen in patients with diabetes in our study. Further assessment of the mechanism between abdominal adiposity and the onset of DM is needed. Additionally, we found that no or light-to-moderate alcohol consumption decreased the risk of DM, while alcohol abuses increased it. This finding is similar to the Meta-analysis which reported a threshold in women and non-Asian populations, alcohol intake of <63 g/day, below which are associated with reductions in the risk of type 2 diabetes, but risks increasing above this threshold.25 As men consume more alcohol than women in populations and the benefit of moderate alcohol consumption only be demonstrated in women but not overall,26,27 and alcohol abuse was proved to be a risk factor for incidence and re-infection of TB,28 we thus believe that the effect of alcohol consumption in the development of DM should be further validated in large populations.
There were several limitations in our study. Firstly, the data in the study were limited and collected from only two hospitals specializing in TB. Therefore, the results may only reflect the current situation in large cities in China and may be limited by the geographical area. Secondly, we did not assess lifestyle, dietary habits, physical exercise, and environmental factors, which could introduce selection bias and potentially overlook additional factors contributing to the development of DM-TB. Thirdly, due to a small number of patients with extra-pulmonary TB, we were unable to address the risk factors of DM in these patients.
In conclusion, we found that about one-fifth of PTB patients have diabetes. The risk factors are male, age ≥ 47 years, excessive alcohol use, family history of DM, and an elevated random glucose level. Awareness of DM and zero-to-light alcohol consumption may lower the risk of developing DM. Raising disease awareness, effective prevention, and early diagnosis of diabetes aids in the reduction of the dual burden of TB–DM comorbidity, particularly in men after middle age.
Data Sharing Statement
All original data used in the study has been de-identified and are available from the corresponding author on request.
Declarations
This study is approval by the Ethical Committee of the third people’s hospital of Shenzhen and the Ethical Committee of the third people’s hospital of Kunming. All participants in this study provided written consent to participate. Both hospitals assure that no personal information of any patients was involved in using these statistics. Furthermore, the study adheres to the Declaration of Helsinki guidelines regarding confidentiality and ethical standards.
Acknowledgments
The authors thank all participants for their participation in this study. The authors are grateful for the continued academic support from The National Clinical Research Center for Infectious Disease in China and Clinical Research Center for Infectious Diseases (tuberculosis) of Guangdong Province.
Funding
This work was supported by the Shenzhen Science and Technology Plan Project (No. JCYJ20210324132012035), Technology Project of Guangdong Province (No.2020B1111170014) and Technology Project of Health commission of Kunming Municipality (No. 2023-03-02-019, No. 2023-03-08-012). All these fund are from government for tuberculosis treatment and control.
Disclosure
The authors declare no conflicts of interest in this study.
References
1. DF diabetes atlas reports [homepage on the Internet]. International Diabetes Federation, 2024. Available from: https://diabetesatlas.org/.
2. WHO. Global tuberculosis report 2022; 2022. Available from: https://www.who.int/publications/i/item/9789240061729.
3. World Health Organization. Framework for Collaborative Action on Tuberculosis and Comorbidities. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization;2022.
4. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. doi:10.1038/nrendo.2017.151
5. Noubiap JJ, Nansseu JR, Nyaga UF, et al. Global prevalence of diabetes in active tuberculosis: a systematic review and meta-analysis of data from 2·3 million patients with tuberculosis. Lancet Glob Health. 2019;7(4):e448–e460. doi:10.1016/S2214-109X(18)30487-X
6. Wu Q, Liu Y, Ma YB, Liu K, Chen SH. Incidence and prevalence of pulmonary tuberculosis among patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Ann Med. 2022;54(1):1657–1666. doi:10.1080/07853890.2022.2085318
7. Huangfu P, Ugarte-Gil C, Golub J, Pearson F, Critchley J. The effects of diabetes on tuberculosis treatment outcomes: an updated systematic review and meta-analysis. Int J Tuberc Lung Dis. 2019;23(7):783–796. doi:10.5588/ijtld.18.0433
8. Gautam S, Shrestha N, Mahato S, Nguyen TPA, Mishra SR, Berg-Beckhoff G. Diabetes among tuberculosis patients and its impact on tuberculosis treatment in South Asia: a systematic review and meta-analysis. Sci Rep. 2021;11(1):2113. doi:10.1038/s41598-021-81057-2
9. Nyirenda JLZ, Bockey A, Wagner D, Lange B. Effect of Tuberculosis (TB) and Diabetes mellitus (DM) integrated healthcare on bidirectional screening and treatment outcomes among TB patients and people living with DM in developing countries: a systematic review. Pathog Glob Health. 2023;117(1):36–51. doi:10.1080/20477724.2022.2046967
10. Shenzhen, China population [homepage on the Internet]. Population stat. Available from: https://populationstat.com/china/shenzhen.
11. Kunming, China population [homepage on the Internet]. Population stat. Available from: https://populationstat.com/china/shenzhen.
12. American Diabetes Association. Summary of Revisions: standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S4–S6. doi:10.2337/dc19-Srev01
13. World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm. Geneva: World Health Organization; 2000.
14. Kondrup J, Allison SP, Elia M, et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–421. doi:10.1016/S0261-5614(03)00098-0
15. World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. Geneva: World Health Organization; 2011.
16. Alturki S, Al Amad M, Mahyoub E, Al Hanash N, Alhammadi A. Prevalence of Diabetes Mellitus among Patients with Tuberculosis and Its Associated Factors in Sana’a, Yemen, 2021. Epidemiologia. 2023;4(2):202–211. doi:10.3390/epidemiologia4020021
17. Omar N, Wong J, Thu K, Alikhan MF, Chaw L. Prevalence and associated factors of diabetes mellitus among tuberculosis patients in Brunei Darussalam: a 6-year retrospective cohort study. Int J Infect Dis. 2021;105:267–273. doi:10.1016/j.ijid.2021.02.064
18. Viswanathan V, Kumpatla S, Aravindalochanan V, et al. Prevalence of diabetes and pre-diabetes and associated risk factors among tuberculosis patients in India. PLoS One. 2012;7(7):e41367. doi:10.1371/journal.pone.0041367
19. Nanditha A, Ma RC, Ramachandran A, et al. Diabetes in Asia and the Pacific: implications for the Global Epidemic. Diabetes Care. 2016;39(3):472–485. doi:10.2337/dc15-1536
20. Huber FG, Kristensen KL, Holden IK, et al. The prevalence of diabetes among tuberculosis patients in Denmark. BMC Infect Dis. 2022;22(1):64. doi:10.1186/s12879-022-07048-4
21. Aftab H, Ambreen A, Jamil M, et al. High prevalence of diabetes and anthropometric heterogeneity among tuberculosis patients in Pakistan. Trop Med Int Health. 2017;22(4):465–473. doi:10.1111/tmi.12842
22. Agarwal AK, Gupta G, Marskole P, Agarwal A. A Study of the Patients Suffering from Tuberculosis and Tuberculosis-diabetes Comorbidity in Revised National Tuberculosis Control Program Centers of Northern Madhya Pradesh, India. Indian J Endocrinol Metab. 2017;21(4):570–576. doi:10.4103/ijem.IJEM_89_17
23. Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi:10.1001/jama.2013.168118
24. Emdin CA, Khera AV, Natarajan P, et al. Genetic Association of Waist-to-Hip Ratio With Cardiometabolic Traits, Type 2 Diabetes, and Coronary Heart Disease. JAMA. 2017;317(6):626–634. doi:10.1001/jama.2016.21042
25. Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: a Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care. 2015;38(9):1804–1812. doi:10.2337/dc15-0710
26. Polsky S, Akturk HK. Alcohol Consumption, Diabetes Risk, and Cardiovascular Disease Within Diabetes. Curr Diab Rep. 2017;17(12):136. doi:10.1007/s11892-017-0950-8
27. Schrieks IC, Heil AL, Hendriks HF, Mukamal KJ, Beulens JW. The effect of alcohol consumption on insulin sensitivity and glycemic status: a systematic review and meta-analysis of intervention studies. Diabetes Care. 2015;38(4):723–732. doi:10.2337/dc14-1556
28. Rehm J, Samokhvalov AV, Neuman MG, et al. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health. 2009;9(1):450. doi:10.1186/1471-2458-9-450
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.