Back to Journals » International Journal of General Medicine » Volume 14
Prevalence and Related Risk Factors Associated with Coronary Heart Disease (CHD) Among Middle-Aged and Elderly Patients with Vision Impairment (VI)
Authors Qin S, Huang L, Zhou J, Wang H , Li Q, Wu H , Wu J
Received 29 July 2021
Accepted for publication 15 September 2021
Published 27 September 2021 Volume 2021:14 Pages 6125—6133
DOI https://doi.org/10.2147/IJGM.S330726
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Shengmei Qin,1,* Lan Huang,1,* Jie Zhou,1 Hao Wang,1 Qi Li,1 Hengjing Wu,2 Jing Wu1
1School of Nursing, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 2Clinical Center for Intelligent Rehabilitation Research, Shanghai YangZhi Rehabilitation Hospital (Shanghai Sunshine Rehabilitation Center), School of Medicine, Tongji University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jing Wu; Hengjing Wu Tel +8613817556859
Email [email protected]; [email protected]
Purpose: To investigate the prevalence and related risk factors associated with coronary heart disease (CHD) among middle-aged and elderly patients with vision impairment (VI).
Patients and Methods: The study was conducted with 1355 visually impaired adults over 45 years old, recruited from a Rehabilitation Hospital in China. Visual impairment is diagnosed by a doctor according to guidelines. Data were analyzed using multiple correspondence and logistic regression analysis. This research represents an important step towards the development of empirically based practical suggestions for decision-makers and health professionals that support visually impaired middle-aged and elderly people to participate in physical exercise and weight management when needed.
Results: Of the 1335 middle-aged and elderly adults (mean age ± SD, 63.56 ± 7.74 years; 45.6% male) with VI, a total of 154 (11.5%) developed CHD. In all people with VI, age (OR 1.47; 95% CI 1.16– 2.02), hypertension (OR 2.14; 95% CI 1.46– 3.14), diabetes (OR 3.79; 95% CI 2.29– 6.27), blindness (OR 1.68; 95% CI 1.16– 2.43), moderate activity (OR 0.86; 95% CI 0.69– 0.98), and HR < 60 beats/min (OR 1.43; 95% CI 1.08– 2.48) are significantly related to CHD. Statistical analysis based on age grouping indicated that fasting plasma glucose, hypertension, diabetes, blindness, heart rate (< 60 beats/min), and moderate activity were shown to have a strong association with development of CHD in age group < 65 years (p < 0.05).
Conclusion: Compared with historical data, poorer vision degree, resting heart rate below 60 beats a minute and low physical activity level are emerging as new and increasing threats to CHD in middle-aged and elderly VI population. Interventions to enhance physical functioning and risk screening may be effective in the prevention of CHD in VI population.
Keywords: coronary heart disease, vision disability, prevalence, risk factors, physical activity
Introduction
Based on data from the second sample survey of persons with disabilities in China, an estimated 12.23 million people reported visual disabilities.1 This number is likely to increase as the population ages. Moderate to severe impairment of visual function can lead to a visual disability (VD) and difficulty in performing daily activities.2 The strong associations between increased prevalence of disability with chronic diseases have been well established. The onset and general pattern of disability among the chronically ill is often distinct from their healthy peers.3 However, data and statistics about diseases risks for disabled people is limited, especially in developing countries such as China.
Health disparities between people with and without vision impairment (VI) has been proved in several studies.4–6 Visual acuity is a reflection of functional status and ocular health, and it has been proven that VI onset is caused by physiological changes associated with aging and underlying chronic diseases.7 Studies have demonstrated that persons with VI had poorer overall survival and increased risk of mortality.8,9 People living with VI may be more vulnerable to various chronic diseases and may be overlooked, due to activity limitations or participation restriction in the absence of supportive personal and environmental factors.
As one of the leading cause of death worldwide, coronary heart disease (CHD) presents a significant burden to China.10 Hypertension, diabetes, hypercholesterolemia, overweight and physical inactivity have been well-established as important and modifiable risk factors for cardiovascular disease.11–13 The majority of studies are specifically focused on either healthy populations or a general population. In recent years, the risk assessment and management of CHD among disabilities has attracted more attention. David W et al demonstrated that persons with VI had significantly greater risks for cardiovascular disease than their health peers.14 A population-based cross-sectional study in British showed that subjects with visual impairment reported worse health and were associated with symptoms of CHD.15 Hence, more details are needed to explore the CHD burden and risk factors in visually impaired people. The aim of the current cross-sectional study was to identify the prevalence and related risk factors of CHD among VI, and to further analyzed the effects of different age groups on this relationship, so as to provide reference for proposing intervention strategies and reducing CHD in VI population.
Patients and Methods
Study Population
We performed a cross-sectional study among a total of 1335 adults with medically diagnosed VI in one or both eyes, using data collected from January 1, 2018 to December 31, 2018 at Shanghai Yangzhi Rehabilitation Hospital in China. Each disabled person received medical examination including physical examination, imageological examination and blood routine examination. This study was approved by the Ethics Committee of Shanghai Yangzhi Rehabilitation Hospital (YZ 2019–051), which was conducted in accordance with the guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from participants, after having had the procedure and risks explained to them in their native language, and all the participants were mature adults.
Patients who met the following criteria were included in the study: medically diagnosed VI in one or both eyes (including low vision and blindness) by hereditary eye diseases and trauma, such as retinitis pigmentosa, glaucoma, cataracts, eye injuries and burns; can walk independently with or without mobility aids; aged 18 and older; can speak Chinese. Exclusion criteria included: patients with diabetic retinopathy and age-related macular degeneration; patients with severe additional impairments, such as hearing, physical and mental disabilities; those with severe congestive heart failure, cerebrovascular disease, severe chronic obstructive pulmonary disease, renal failure and cancer.
Measurements
The sociodemographic characteristics of participants were collected via a questionnaire. Anthropometric parameters including body mass index (BMI), diastolic blood pressure (DBP) and systolic blood pressure (SBP) were collected by the medical examination using standard protocol. All blood samples were obtained in the morning following an overnight fasting of at least 12h. Total cholesterol (TC), total triglyceride (TG), fasting plasma glucose (FBG), uric acid (UA), serum urea (SU), hemoglobin (Hb), red blood count (RBC), white blood count (WBC), platelet count (PLT) were collected by the medical examination. BP was recorded twice on the right arm after 5 minutes resting. Two readings were obtained 30 seconds apart. Blood routine examination was taken in the morning after an overnight fasting of at least 12h. Body mass index (BMI) was calculated based on height and weight. Serum biochemical indexes, such as FBG, TC, TG, albumin (Alb), globulin (Glo), UA, creatinine (Cr), SU, Hb, RBC, WBC, PLT were measured enzymatically (Roche Corporation, Basel, Switzerland).
Information on physical activity was obtained from patient interviews. Adults with disabilities unable to meet the Physical Activity Guidelines should regularly engage in physical activity according to their abilities and avoid inactivity.16 Based on standard, activity outcomes were derived: sedentary behavior (mainly in bed or wheelchair, self-care needs help) is defined as any waking behavior with an energy expenditure ≤1.5 metabolic equivalent, gentle activity intensity aerobic physical activity (rates of perceived exertion <12, 40–60% of the maximum heart rate), moderate to high intensity aerobic physical activity (rates of perceived exertion ≥12, 60–75% of the maximum heart rate).17
Definitions
Diagnostic Criteria of Disease
Prevalence of hypertension, diabetes mellitus (DM), Hyperlipidemia (HPL), CHD was checked by clinical doctors. Hypertension was defined systolic blood pressure (SBP) is ≥140 mmHg and/or diastolic blood pressure (DBP) is ≥90 mmHg following the repeated examination in the office or clinic.18 Diabetes was defined as fasting blood sugar levels ≥ 7.0 mmol or previous medical diagnosis of diabetes.19 Dyslipidemia was defined as total cholesterol (TC)≥ 5.2 mmol or total triglycerides (TG)≥1.7 mmol/L, or high-density lipoprotein cholesterol (HDL-C)≤1.0 mmol, or low density lipoprotein cholesterol (LDL-C)≥3.4 mmol.20 CHD was defined as documented evidence of prior MI, prior coronary revascularization procedure or more than 50% epicardial coronary stenosis by coronary angiography.21
Vision Impairment
According to China’s survey of disabled persons in 2006, VI is defined as the impairment of binocular vision or narrowing of the field of vision due to various reasons that cannot be corrected, thus affecting the subject’s daily life and social participation. VI is classified as low vision and blindness. Low vision can be further divided into two categories: severe visual impairment (SVI) (3/60 ≤ BCVA < 6/60) and moderate visual impairment (MVI) (6/60 ≤ BCVA < 6/18). Blindness can also be further divided into two categories: profound visual impairment (PVI) (12/600 ≤ BCVA < 3/60) and near total blindness (NTB) (BCVA < 12/600). The grade of VI is determined based on the measurements from both eyes; if there are discrepancies between each eye, the vision measurements from the better eye is chosen. If only one eye was classified as low vision or blind but the other eye had a vision of 0.3 or better, the subject was not classified as having a VI. Best corrected visual acuity (BCVA) is the highest visual acuity that can be achieved with proper lens correction, or measured with a pinhole mirror. Subjects with a visual field radius of less than 10 degrees, regardless of their vision are classified as being blind. The classification of VI is shown in Table 1.
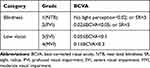 |
Table 1 Grade of Visual Disability |
Statistical Analysis
Continuous variables with normal distribution were expressed as the mean ± SD and comparisons between CHD group and non-CHD group were performed by independent Student’s t-tests. In case of skewed distribution, continuous variables were presented as median (inter-quartile range) and the comparison between groups were conducted using Mann–Whitney U-test. These newly formed categorical variables were picked into a multiple correspondence analysis (MCA) model (on the basis of optimal scaling) to investigate the interrelationships among the factors considered through a visualized two-dimensional graph. This kind of analysis is mainly descriptive and resumes information on association among factors considered through a graphical representation. x2-test for trend (linear-by-linear test) was used as a substantial supplementation to examine the possible direct viewing association appeared in the MCA plot. (The explanation of MCA plot followed the protocol that association between two points of the same quadrant in the coordinate was perceived by the distance between them, namely the larger the distance, the less associated the two points are suggested to be.22) Finally, Multiple logistic regression analysis model was performed to evaluate whether the latent independent risk factors were associated with CHD. Variables that demonstrated significant statistical differences between groups (non-CHD versus CHD) were selected and entered into multivariate logistic regression models for the assessment of independent risk factors of CHD. Two-sided P value less than 0.05 was considered statistically significant. To explore the associated risk elements of CHD between younger and elderly populations, we divided the populations into two groups based on age (<65 and ≥65 years) and conducted subgroup analysis. All statistical analyses were conducted using SPSS 25.0 statistical software (Chicago, IL, Illinois, USA).
Results
The demographic and clinical features of all subjects with non-CHD or CHD are summarized in Tables 2–3. As shown in Table 2, a prevalence rate of 11.5% (154/1335) was given, with the rate for middle-aged 8.6% (68/791) and elderly adults 15.8% (86/544). The prevalence of CHD was proven to increase significantly with age.
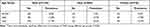 |
Table 2 The Prevalence of Coronary Heart Disease (CHD) Stratified by Age and Gender |
 |
Table 3 Baseline Characteristics of the Two Groups of Subjects |
Among the total of 1335 patients with VI, the average age was 63.56±7.74 years; 45.6% of the participants were men; average BMI was 24.14±3.22 kg/m2, Subjects with CHD had a higher rate of hypertension (64.9%), DM (31.2%), comparing to 42.1%, 11.5% in subjects with non-CHD. Table 3 depicted that age, degree of disability and physical activity, BMI, SBP in subjects with CHD was significantly higher than that in those without Non-CHD (P < 0.05). All of the remaining variables except for FPG, TC, TG, and SU were also significantly higher in subjects with CHD. Table S1 shows baseline characteristics grouped by CHD and levels of VI in the supplementary.
Further analysis of MCA graphical displays in Figures 1 and 2 after categorizing continuous data. Since MCA is not a hypothesis test but a method of statistical description, a necessary statistical verification was offered and the outcomes are presented in Table 4. Further analysis of multivariate logistic regression models was performed to clarify the relationships between the statistically significant variables and CHD (Table 4). In all people with VI, age (OR 1.47; 95% CI 1.16–2.02), hypertension (OR 2.14; 95% CI 1.46–3.14), diabetes (OR 3.79; 95% CI 2.29–6.27), moderate activity (OR 0.86; 95% CI 0.69–0.98), and HR <60 (OR 1.43; 95% CI 1.08–2.48) are significantly related to CHD. In age group <65 years, there were statistically significant differences between FPG (OR 1.363; 95% CI 1.041–1.995), hypertension (OR 2.046; 95% CI 1.540–4.134), diabetes (OR 7.651; 95% CI 3.341–17.520), HR (<60), level of VI and physical activity. In age group ≥65 years, BMI (OR 1.07; 95% CI 1.01–1.15), hypertension (OR 2.14; 95% CI 1.26–3.64), diabetes (OR 2.35; 95% CI 1.21–4.60) gentle activity (OR 0.88; 95% CI 0.79–0.96) and moderate activity (OR 0.72; 95% CI 0.65–0.92) were significantly higher in subjects with CHD.
 |
Table 4 Risk of Developing Coronary Heart Disease (CHD) According to Age Categories |
Discussion
In the current study, we found that the risk of CHD in middle-aged and elderly patients with visual impairment is 11.5%, which increase with age. The related risk factors of CHD included hypertension, diabetes, degree of visual impairment and physical exercise level. In addition, there were statistically significant differences between FPG and HR (<60) in age group <65 years, and the BMI of subjects with CHD was significantly higher in age group ≥65 years. The results of this study add to the current literature on visual impairment from the prevalence of CHD and related risk factors in middle-aged and elderly patients with VI.
We founded that the history of hypertension and diabetes were independent related risk factors for CHD either in the middle-aged group or the elderly group with impaired vision, which is consistent with previous studies.23–25 In addition, our study further strengthened the notion that BMI was the important predictor of CHD In age group <65 years. The association between BMI and coronary risk is mostly mediated through its adverse effects on other major cardiovascular risk factors, mainly diabetes, blood pressure and lipids26—which explains that in the elderly group, obese people with VI have a higher risk of CHD compared with normal weight. These findings indicate that effective control of body weight is crucial for the early prevention of CHD in patients with VI.
In this study, we demonstrated that poorer vision degree (especially blindness) was associated with a higher risk of CHD. Existing studies have confirmed that visually impaired patients have a high incidence of cardiovascular disease.15 However, there is no concrete evidence that the risk of cardiovascular disease is measured in terms of the degree of VD. The results of this study emphasize the importance of early recognition of CHD in patients with VI, and provide a new basis for the prevention of CHD in patients with VD. The relevant literature shows that people with VD have limited physical activity and have obvious psychological problems.27 In addition, reports from Alberto R. Ramos et al link severe visual disabilities to lower sleep quality.28 All of the above factors may be a potential cause of CHD in people with moderate to severe visual disabilities. Low physical activity (especially Sedentariness) was significantly associated with CHD. This finding is consistent with the Kim et al,29 and further demonstrates the importance of strategies and interventions to improve the activities of people with VD compared to the general population. Certainly, our current results can only confirm that the degree of physical activity and VI is related to the risk of CHD, the interactions of CHD and physical activity is warranted further study.
Notably, we found that HR (<60) was associated with CHD in the <65 years old group. It is well accepted that atherosclerotic plaques are viscoelastic, heart rate and heart rate variability (HRV) reduction and CHD.25 A high resting heart rate is associated with an increase in cardiovascular mortality in the general population.30,31 Scientific evidence has shown that a high resting heart rate is a risk factor for the pathogenesis of atherosclerosis, while reductions in resting heart rate decreased vascular oxidative stress and prevented atherosclerosis in animal models.32 However, there are studies that suggest otherwise. The SIGNIFY study used ivabradine to reduce the heart rate of CHD patients without clinical heart failure. The results showed that lowering heart rate could not prevent cardiovascular death or myocardial infarction in patients with CHD.33 Our findings suggest that HR <60 may increase the risk of CHD in people with VI, which may be related to the early stages of CHD and the absence of heart failure in the study population.34 There are limited data on whether the heart rate of visually impaired people affects CHD. Future research should pay more attention to the difference in heart rate monitoring between visually impaired people and normal people as well as the underlying physiological mechanisms. In addition, for the finding that HR <60 may be related to CHD, since this study is only a cross-sectional survey, and considering the influence of confounding factors, the extrapolation of the results needs to be carefully considered.
Our study has several potential limitations. First, our study uses a cross-sectional design, and thus it is impossible to infer causal and temporal relationships of risk factors with CHD. Second, our research is based on a sample of visually impaired patients from a hospital in Shanghai, China’s largest city, so our findings may not be representative of the general population. Finally, due to limited data availability, we cannot consider the influence of several risk factors such as dietary habits, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), psychological factors and genetic factors. Further research is needed to study the influence of these factors on CHD in VI patients.
Conclusion
This study provides important new information regarding the demographics and disability-specific characteristics associated with CHD in the VI population. In addition to the traditional cardiovascular risks (including age, hypertension and diabetes), poorer vision degree, resting heart rate below 60 beats a minute and lack of physical activity were demonstrated to be independently robust predictors of CHD among VI patients aged >45 years, whereas BMI was shown to associated with CHD only in the elderly subgroup (>65 years). This study can remind ophthalmologists and other clinicians about the risk of CHD when their patients are moderately to severely VI. Further longitudinal studies are warrant to confirm the causality and understand the potential pathways underlying associations between VI and CHD and poor physical functioning including frailty. Overall, improvements in CHD prevention and management among people with VI may require a targeted approach that incorporates both demographical and clinical characteristics.
Acknowledgments
The authors express their sincere gratitude to the Shanghai Yangzhi Rehabilitation Hospital in China. We would also like to warmly thank all staff involved in this survey for their important contributions.
Funding
This study was supported by National Natural Science Foundation of China [grant numbers 71904127].
Disclosure
The findings and conclusions in this paper are those of the authors and there are no conflicts of interest. This manuscript, including data and tables, has not been published elsewhere in whole or part, and is not under review for publication elsewhere.
References
1. Disability LGotSCNSSo, China NBoSotPsRo. Communiqué on major statistics of the second china national sample survey on disability. China J Rehabil Theor Pract. 2006;12(12):1013.
2. Hsueh CM, Wey JH, Yeh JS, Wu CH, Liou TH, Chang KH. Incidence and risk of major heart diseases in middle-aged adults with moderate to severe vision impairment: a Population-Based Cohort Study. Br J Ophthalmol. 2019;103(8):1054–1059. doi:10.1136/bjophthalmol-2018-312471
3. Fong JH. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. 2019;19(1):323. doi:10.1186/s12877-019-1348-z
4. Park SJ, Ahn S, Woo SJ, Park KH. Extent of exacerbation of chronic health conditions by visual impairment in terms of health-related quality of life. JAMA Ophthalmol. 2015;133(11):1267–1275. doi:10.1001/jamaophthalmol.2015.3055
5. VanNasdale DA, Jones-Jordan LA. Multi-state assessment of vision impairment and associated morbidity. Invest Ophthalmol Vis Sci. 2017;58(8):2202.
6. Crews JE, Chou CF, Sekar S, Saaddine JB. The prevalence of chronic conditions and poor health among people with and without vision impairment, aged ≥65 years, 2010–2014. Am J Ophthalmol. 2017;182:18–30. doi:10.1016/j.ajo.2017.06.038
7. Park SJ, Ahn S, Park KH. Burden of visual impairment and chronic diseases. JAMA Ophthalmol. 2016;134(7):778–784. doi:10.1001/jamaophthalmol.2016.1158
8. Siantar RG, Cheng CY, Gemmy Cheung CM, et al. Impact of visual impairment and eye diseases on mortality: the Singapore Malay Eye Study (SiMES). Sci Rep. 2015;5(1):16304. doi:10.1038/srep16304
9. McGuire S. Centers for disease control and prevention. state indicator report on physical activity, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. Adv Nutr. 2014;5(6):762–763. doi:10.3945/an.114.007211
10. Liu S, Li Y, Zeng X, et al. Burden of cardiovascular diseases in China, 1990–2016: findings from the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019;4(4):342–352. doi:10.1001/jamacardio.2019.0295
11. Khamis RY, Ammari T, Mikhail GW. Gender differences in coronary heart disease. Heart. 2016;102(14):1142–1149. doi:10.1136/heartjnl-2014-306463
12. Steinberger J, Daniels SR, Hagberg N, et al. Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American heart association. Circulation. 2016;134(12):e236–55. doi:10.1161/cir.0000000000000441
13. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
14. Hollar DW
15. Liljas AE, Wannamethee SG, Whincup PH, et al. Socio-demographic characteristics, lifestyle factors and burden of morbidity associated with self-reported hearing and vision impairments in older British community-dwelling men: a Cross-Sectional Study. J Public Health (Oxf). 2016;38(2):e21–8. doi:10.1093/pubmed/fdv095
16. Physical Activity Guidelines Advisory Committee.Physical Activity Guidelines Advisory Committee Report,2008. Washington,DC: US Department of Health and Human Services;2008
17. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. doi:10.1249/00005768-198205000-00012
18. Unger T, Borghi C, Charchar F, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi:10.1161/hypertensionaha.120.15026
19. World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. 2006.
20. Jun-Ren ZH, Run-Lin GA, Shui-Ping ZH, Guo-Ping LU, Dong ZH, Jian-Jun LI. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15(1):1–29. doi:10.11909/j.issn.1671-5411.2018.01.011
21. Wilcox T, Newman JD, Maldonado TS, Rockman C, Berger JS. Peripheral vascular disease risk in diabetic individuals without coronary heart disease. Atherosclerosis. 2018;275:419–425. doi:10.1016/j.atherosclerosis.2018.04.026
22. Rennie TW, Roberts W. Data mining of tuberculosis patient data using multiple correspondence analysis. Epidemiol Infect. 2009;137(12):1699–1704. doi:10.1017/s0950268809002787
23. Li YH, Chen JW, Lin TH, et al. A performance guide for major risk factors control in patients with atherosclerotic cardiovascular disease in Taiwan. J Formos Med Assoc. 2020;119(3):674–684. doi:10.1016/j.jfma.2019.04.007
24. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-Control Study. Lancet. 2004;364(9438):937–952. doi:10.1016/s0140-6736(04)17018-9
25. Kołtuniuk A, Rosińczuk J. The prevalence of risk factors for cardiovascular diseases among Polish surgical patients over 65 years. Clin Interv Aging. 2016;11:631–639. doi:10.2147/cia.S105201
26. Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383(9921):970–983. doi:10.1016/s0140-6736(13)61836-x
27. Fenwick EK, Cheng GH, Man REK, et al. Inter-relationship between visual symptoms, activity limitation and psychological functioning in patients with diabetic retinopathy. Br J Ophthalmol. 2018;102(7):948–953. doi:10.1136/bjophthalmol-2017-310915
28. Ramos AR, Wallace DM, Williams NJ, et al. Association between visual impairment and sleep duration: analysis of the 2009 National Health Interview Survey (NHIS). BMC Ophthalmol. 2014;14(1):115. doi:10.1186/1471-2415-14-115
29. Kim KN, Park SJ, Kim W, et al. Modification of the association between visual impairment and mortality by physical activity: a Cohort Study among the Korean national health examinees. Int J Environ Res Public Health. 2019;16(22):4386. doi:10.3390/ijerph16224386
30. Phoenix C, Griffin M, Smith B. Physical activity among older people with sight loss: a Qualitative Research Study to inform policy and practice. Public Health. 2015;129(2):124–130. doi:10.1016/j.puhe.2014.10.001
31. Capella-McDonnall M. The Need for Health Promotion for Adults Who Are Visually Impaired. J Vis Impair Blind. 2007;101(3):133–145. doi:10.1177/0145482X0710100302
32. Smith L, Timmis MA, Pardhan S, Latham K, Johnstone J, Hamer M. Physical inactivity in relation to self-rated eyesight: cross-sectional analysis from the English Longitudinal Study of Ageing. BMJ Open Ophthalmol. 2017;1(1):e000046. doi:10.1136/bmjophth-2016-000046
33. Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R. Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med. 2014;371(12):1091–1099. doi:10.1056/NEJMoa1406430
34. Ferrari R, Fox K. Heart rate reduction in coronary artery disease and heart failure. Nat Rev Cardiol. 2016;13(8):493–501. doi:10.1038/nrcardio.2016.84
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


