Back to Journals » Cancer Management and Research » Volume 12
Pretreatment Systemic Inflammation Response Index in Patients with Breast Cancer Treated with Neoadjuvant Chemotherapy as a Useful Prognostic Indicator
Authors Chen L , Kong X, Wang Z, Wang X, Fang Y, Wang J
Received 21 October 2019
Accepted for publication 14 February 2020
Published 3 March 2020 Volume 2020:12 Pages 1543—1567
DOI https://doi.org/10.2147/CMAR.S235519
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
Li Chen, Xiangyi Kong, Zhongzhao Wang, Xiangyu Wang, Yi Fang, Jing Wang
Department of Breast Surgical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, People’s Republic of China
Correspondence: Jing Wang; Yi Fang
Department of Breast Surgical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, People’s Republic of China
Email [email protected]; [email protected]
Background and Objective: Systemic inflammation response index (SIRI=N×M/L), based on neutrophil (N), monocyte (M), and lymphocyte (L) counts, is used to predict the survival of patients with malignant tumors and can fully evaluate the balance between host immune and inflammatory condition. The present study is aimed to evaluate the potential prognostic significance of SIRI in patients with breast cancer undergoing neoadjuvant chemotherapy.
Subjects and Methods: A total of 262 breast cancer patients treated with neoadjuvant chemotherapy were enrolled in this retrospective study. The optimal cutoff value of SIRI by receiver operating characteristic curve stratified patients into low SIRI (< 0.85× 109/L) group and high SIRI (≥ 0.85× 109/L) group. The associations between breast cancer and clinicopathological variables by SIRI were determined by chi-square test or Fisher’s exact test. Kaplan–Meier plots and log-rank test were used to evaluate the clinical outcomes of disease-free survival (DFS) and overall survival (OS). Univariate and multivariate Cox proportional hazards regression models were used to analyze the prognostic value of SIRI. The toxicity of neoadjuvant chemotherapy was evaluated by the National Cancer Institute Common Toxicity Criteria (NCICTC).
Results: The results were shown that SIRI had prognostic significance by optimal cutoff value of 0.85× 109/L on DFS and OS in univariate and multivariate Cox regression survival analyses. Compared with patients who had high SIRI, patients with low SIRI had longer DFS and OS (41.27 vs 30.45 months, HR: 1.694, 95% CI: 1.128– 2.543, P=0.011; 52.86 vs 45.75 months, HR: 1.288, 95% CI: 0.781– 3.124, P=0.002, respectively). The patients with low SIRI had better 3-, 5-, and 10-year rates of DFS and OS than those with high SIRI. The common toxicities after neoadjuvant chemotherapy were hematologic and gastrointestinal reaction, and the SIRI had no significance on toxicities of all enrolled patients, excepted diarrhea. In patients without neural invasion, those with low SIRI had better prognosis and lower recurrence rates than those with high SIRI.
Conclusion: Pretreatment SIRI with the advantage of repeatable, convenient, and non-invasive is a useful prognostic indicator for breast cancer patients who received neoadjuvant chemotherapy and is a promising biomarker for breast cancer on treatment strategy decisions.
Keywords: systemic inflammation response index, SIRI, breast cancer, neoadjuvant chemotherapy, survival, prognosis
Introduction
Breast cancer is the most frequent neoplasm and is leading major cause of cancer-related morbidity and mortality worldwide among women.1 In China, breast cancer has the highest incidence for females, and the incidence of breast cancer is increasing year after year.2 The postmenopausal women with breast cancer in China will reach 100/100,000 in the future, and the incidence of breast cancer is increasing rapidly in coastal developed cities of China.3 Although many patients with breast cancer are successfully treated by the early diagnoses and improved treatment strategies, approximately 20–25% patients are diagnosed with locally advanced breast cancer.4 Lots of studies have indicated that surgery combined with adjuvant chemoradiotherapy can effectively improve the survival rate of patients with breast cancer.5–7
Neoadjuvant chemotherapy (NACT) is the gold standard of care for locally advanced cancer and has been widely used to the treatment for locally advanced breast cancer.8 According to the NACT for breast cancer, the breast-conserving surgery rate is increasing, and the tumor stage is decreasing.9 Many NACT regimens have been applied to the treatment for breast cancer; however, there are no internationally generally accepted NACT regimens for patients with advanced breast carcinoma.10 Therefore, it is necessary to look for accurate and sensitive tumor indicators of breast cancer to improve the survival outcome and provide the better prognosis factor for breast cancer.
Some histologic and immunologic biomarkers have been used to evaluate the prognosis of breast cancer. However, these biomarkers largely depend on the primary tumor sample, and are often expensive, time-consuming and arduous, and are usually limited their use in clinical practice.11 The molecular subtypes, which include ER, PR, Ki-67, and HER2 expression condition, are very important for the prognosis of breast cancer. Hence, it is very important to search easily accessible and reliable markers for the prognosis of patients with breast cancer.
Cancer-related inflammation is a fundamental component of the tumor microenvironment and can influence the mechanism in the pathogenesis of patients with carcinoma. The inflammatory cells in peripheral venous blood might influence tumor carcinogenesis, progression, and metastasis.12 A great deal of studies have indicated that the inflammatory markers, such as white blood cell (W), neutrophil (N), monocyte (M), platelet (P), lymphocyte (L), as well as neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR), and systemic immune-inflammation index (SII), are present and detectable in the systemic circulation, and have been widely proposed as prognostic factors for many malignancies.13–16
A novel and integrated indicator that named Systemic Inflammation Response Index (SIRI), which is based on neutrophil (N), monocyte (M), and lymphocyte (L) counts, is reported to be associated with clinical outcomes and predict the survival of patients with gastric cancer.17 This integrated indicator may comprehensively reflect the balance of host immune and inflammatory status compared with NLR, LMR, and PLR. Nevertheless, the SIRI has been studied rarely in breast cancer patients with treated NACT. Therefore, our study aims to evaluate the prognostic significance of SIRI in patients with breast cancer receiving NACT.
Materials and Methods
Study Population
We enrolled 262 patients with breast cancer undergoing NACT to this study in Cancer Hospital Chinese Academy of Medical Sciences from January 1999 to 2014 December. This research was a retrospective study. The detailed treatment information, clinical and demographic data for all enrolled patients were extracted from the medical record. This study was approved by the ethics committee of Cancer Hospital Chinese Academy of Medical Sciences. It complied with the standards of the Declaration of Helsinki and its later amendments. Written informed consent was obtained from all patients before the study.
The inclusion criteria for the patients were as follows: 1) all patients with breast cancer were confirmed by core needle biopsy before NACT treatment; 2) all patients received surgery treatment; 3) Karnofsky Performance Scores (KPS) ≥80 and Performance Status (Zubrod-ECOG-WHO, ZPS) ranged from 0 to 2 scores; 4) all patients had complete clinical records and follow-up information; 5) Patients could survive for more than 3 months; 6) the blood samples were obtained within 1 week before NACT treatment.
The exclusion criteria for the patients were as follows: 1) patients had received chemotherapy, radiotherapy, endocrine therapy, and targeted therapy before NACT treatment; 2) patients with malignant disease or distant metastases; 3) patients with serious complications, or any form of acute and chronic inflammatory disease; 4) patients who had blood product transfusion within 1 month before NACT treatment.
Chemotherapy Protocols
We used anthracyclines-based and/or taxanes-based NACT regimens, and one cycle of these regimens was repeated every 3 weeks. Anthracyclines (Zhejiang Hisun Pharmaceutical Co., Ltd, Taizhou, China); Cyclophosphamide (Baxter Oncology GmbH, Halle, Germany); 5-Fluorouracil (Tianjin Jinyao Pharmaceutical Co., Ltd, China); Taxol (Jiangsu Hengrui Medicine Co., Ltd, Lianyungang, China); Platinum compounds (Bristol-Myers Squibb biopharmaceutical company, S.r.l., Italy).
AC regimen (A: 90 mg/m2, C: 600 mg/m2). ACF regimen (A: 90 mg/m2, C: 600 mg/m2, F: 500 mg/m2). CT regimen (C: 600 mg/m2, T: 175 mg/m2). ACT regimen (A: 90 mg/m2, C: 600 mg/m2, T: 175 mg/m2). AT regimen (A: 90 mg/m2, T: 175 mg/m2). TP regimen (T: 175 mg/m2, P: AUC 4–6).
Classification Standard and Response Evaluation
We used the eighth edition of American Joint Committee on Cancer (AJCC) and Union for International Cancer Control (UICC) TNM stage classification to evaluate the tumor pathology stage of all enrolled patients.18,19 Breast cancer molecular subtypes were classified as Luminal A, Luminal B HER2-positive, Luminal B HER2-negative, HER2-enriched, and triple negative.20 The Miller and Payne grade (MPG) was used to determine the histological response.21 Response rates were defined according to the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines.22 The hematoxylin and eosin (HE) stain was used to diagnose lymph vessel invasion and neural invasion of tumor. The National Cancer Institute Common Toxicity Criteria (NCICTC) was used to evaluate the toxicity of NACT.
Peripheral Venous Blood Parameters
Peripheral venous blood samples were obtained within 1 week before NACT. The samples were collected by a sterile EDTA tube and obtained with empty stomach. Hematologic parameters were analyzed by XE-2100 hematology analyzer (Sysmex, Kobe, Japan).
Follow-Up
All patients were followed up by inpatients and outpatients every 3 months for the first to second year after surgery, every 6 months for the third to fifth year after surgery, then annually every year and until death.23 Follow-up assessments included laboratory tests (routine blood test, blood biochemical), breast ultrasonography, mammography and some other examinations as it fits. Disease-free survival (DFS) was defined as the time from the date of surgery to the date of local recurrence or distant metastases, death from any cause or last follow-up. Overall survival (OS) was defined as the time from the date of surgery to the date of death from any cause or last follow-up.
Statistical Analysis
The optimal cutoff value was accessed by the receiver operating characteristic curve (ROC) analyses, and the area under the curve was determined by the predictive value. The ratio closest to the point with maximum sensitivity and specificity was defined as the optimal cutoff value. The clinicopathologic categorical variables were presented as frequencies and percentages (%), and the associations between breast cancer and clinicopathological variables were evaluated using the chi-square test or Fisher’s exact test. The association between breast cancer and survival was analyzed by the Kaplan–Meier plots and log-rank test. The independent prognostic factors were accessed by the univariate and multivariate Cox proportional hazards regression model, and the hazard ratios (HRs) and 95% confidence interval (CI) were obtained by the Cox proportional hazards regression model. All statistical analyses were performed using the SPSS software (version 17.0; SPSS Inc., Chicago, IL, USA) and GraphPad prism software (version 5.0; GraphPad Inc., La Jolla, CA, USA). Alpha was set at 0.05, and a two-tailed P<0.05 was considered statistically significant.
Results
Demographic and Clinicopathologic Characteristics of All Breast Cancer Patients
We enrolled 262 cases with breast cancer in this retrospective study. The optimal cutoff value of SIRI by ROC analysis was 0.85×109/L, and the optimal cutoff value was used for all analyses. The patients with breast cancer were categorized into two groups by SIRI: low SIRI group (<0.85×109/L) and high SIRI group (≥0.85×109/L). The clinicopathological characteristics of patients with breast cancer were shown in Table 1. All enrolled patients were females. The age was ranged from 27 to 73 years, and the median age was 48 years. In low SIRI group, there were 155 patients (59.2%), and in high SIRI group, there were 107 patients (40.8%). The median body mass index (BMI) of all patients was ranged from 18.03 to 39.06, and the median BMI was 24.50. In this study, a low SIRI was significantly associated with menopause (χ2=3.895, P=0.048), US-LNM (χ2=4.975, P=0.026), total lymph nodes (χ2=4.065, P=0.044).
 |  |  |
Table 1 Demographic and Clinicopathologic Characteristics of All Breast Cancer Patients |
Relationships Between SIRI and Hematologic Parameters
In this study, the maximum (sensitivity + specificity) point of the ROC curve was regarded as the optimal cutoff value of SIRI. The cutoff value of ALT, AST, LDH, IgA, IgG, IgM, ALB, CRP, CA125, CA153, CEA, D-D, FDP, W, R, Hb, N, M, P, L, NLR, MLR, PLR by median value were 23 U/L, 23 U/L, 190 U/L, 2.30 g/L, 11.67 g/L, 1.27 g/L, 44.00 g/L, 1.10 mg/dl, 27.73 U/mL, 21.86 U/mL, 3.52 ng/mL, 0.83 mg/L FEU, 2.01 ug/mL, 6.00×109/L, 4.34×109/L, 128.00×109/L, 3.83×109/L, 1.67×109/L, 0.34×109/L, 244.00×109/L, 2.50, 0.22, 160.00, respectively. The hematologic parameters of patients with breast cancer are shown in Table 2. A low SIRI was significantly related to W (P<0.001), Hb (P=0.010), N (P<0.001), L (P=0.030), M (P<0.001), NLR (P<0.001), MLR (P<0.001), PLR (P=0.003) (Table 2).
 |
Table 2 Relationships Between SIRI and Hematologic Parameters |
Association of SIRI and NACT or Postoperative Chemotherapy
All enrolled patients received anthracyclines-based and taxanes-based NACT regimens. All cases were treated with NACT, and 27 patients received the AC/ACF regimen, 29 patients received the CT/ACT regimen, 121 patients received the AT regimen, 75 patients received TP regimen, and 10 patients received other regimens, such as FP, T, F, TF, EV regimen. However, 116 patients were received postoperative chemotherapy, and 18 patients were treated with AC/ACF regimen, 17 patients were treated with CT/ACT regimen, 27 patients were treated with AT regimen, 21 patients were treated with TP regimen, and 33 patients were treated with other regimens, such as C, CTF, CTP, A, AF, AMF, AP, F, FP, T, TF, V, VP regimen. The clinical objective response rate (CR+PR) was 61.4%, and the clinical benefit rate (CR+PR+SD) was 97.3%, and non-clinical response rate (SD+PD) was 38.6%. The pathological response was accessed by MPG system, and the grade 1 rate was 5.0%, the grade 2 rate was 29.8%, the grade 3 rate was 39.3%, the grade 4 rate was 10.3%, and the grade 5 rate was 15.6%. Moreover, the pathological response of pCR rate was 20.6%. The NACT or postoperative chemotherapy of patients with breast cancer is shown in Table 3. A low SIRI was significantly related to NACT (P=0.004).
 |
Table 3 Association of SIRI and Neoadjuvant Chemotherapy or Postoperative Chemotherapy |
Correlation Between SIRI and Breast Cancer Molecular Subtypes
All enrolled cases were diagnosed and confirmed by core needle biopsy prior to NACT. Before NACT, 8 cases were Luminal A subtype, 27 cases were Luminal B HER2-positive subtype, 98 cases were Luminal B HER2-negative subtype, 62 cases were HER2-enriched subtype, and 67 cases were triple-negative subtype, respectively. After NACT and surgery, 9 patients were Luminal A subtype, 25 patients were Luminal B HER2-positive subtype, 94 patients were Luminal B HER2-negative subtype, 66 patients were HER2-enriched subtype, and 68 patients were triple-negative subtype, respectively. There was no significant association between tumor molecular subtypes and SIRI (Table 4).
 |
Table 4 Correlation Between SIRI and Breast Cancer Molecular Subtypes |
Correlation Between SIRI and Side Effects of Chemotherapy
In this study, the common toxicities after NACT were hematologic and gastrointestinal reaction. And we used the NCICTC to evaluate and analyze the side effects of NACT. There were no chemotherapy-related deaths in our study. Moreover, we used the SIRI to access the side effects of NACT, and the result indicated that the SIRI before NACT had no significance on toxicities of all enrolled patients, excepted diarrhea (χ2=4.199, P=0.040) (Table 5).
 |
Table 5 Main Toxicities According to NCICTC Scale of the Patients with Breast Cancer Undergoing Neoadjuvant Chemotherapy |
Univariate and Multivariate Cox Regression Survival Analyses
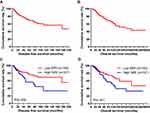
We used the univariate and multivariate Cox proportional-hazards models to determine the independent prognostic factors. According to univariate and multivariate analysis, the clinical T stage, Miller and Payne grade, pathological T stage, pathological TNM stage, core needle biopsy (molecular subtype, ER status, Ki-67 status), postoperative pathology IHC (Ki-67 status), neural invasion, PLR, SIRI, postoperative chemotherapy, postoperative radiotherapy for DFS and OS were the significant prognostic factors (Table 6). The median DFS and OS of all enrolled patients were 36.85 months (range from 4.00 to 197.97 months) and 49.95 months (range from 5.93 to 250.97 months), respectively (Figure 1A and B).
 |  |  |  |  |  |  |
Table 6 Univariate and Multivariate Cox Regression Survival Analyses of the SIRI for the Prediction of DFS and OS in Breast Cancer Patients |
The result was indicated that SIRI was the significant prognostic factor. And patients with low SIRI had significantly lower risks of disease progression compared with patients with high SIRI. Moreover, low SIRI was associated with prolonged DFS and OS by univariate analysis (P=0.018, hazard ratio [HR]: 1.817, 95% confidence interval [CI]: 0.389–8.485 and P=0.007, HR: 1.321, 95% CI: 1.049–4.109, respectively). And low SIRI was also associated with prolonged DFS and OS (P=0.011, HR: 1.694, 95% CI: 1.128–2.543 and P=0.002, HR: 1.288, 95% CI: 0.781–3.124, respectively; Table 6).
In low SIRI group, the mean DFS and OS for all enrolled patients were 41.27 months (range from 4.00 to 197.97 months) and 52.86 months (range from 5.93 to 250.97 months), respectively. In high SIRI group, the mean DFS and OS for all enrolled patients were 30.45 months (range from 4.93 to 194.90 months) and 45.75 months (range from 8.13 to 238.27 months), respectively. We also found that the mean DFS and OS time for patients with low SIRI were longer than for those with high SIRI by using log-rank methods (χ2=4.766, P=0.029 and χ2=4.181, P=0.041, respectively; Figure 1C and D).
Survival and Evaluation of the Prognostic Significance of SIRI
Among the 262 patients with breast cancer, the DFS rates at 3-, 5-, and 10-year were 31.7% (83/262), 17.2% (45/262), 4.6% (12/262); the OS rates at 3-, 5-, and 10-year were 42.7% (112/262), 28.2% (74/262), 7.6% (20/262), respectively. In low SIRI group, the DFS rates at 3-, 5-, and 10-year were 36.1% (56/155), 20.6% (32/155), 5.8% (9/155); and the OS rates at 3-, 5-, and 10-year in low SIRI were 46.5% (72/155), 31.0% (48/155), 8.4% (13/155), respectively. In high SIRI group, the DFS rates at 3-, 5-, and 10-year were 25.2% (27/107), 12.1% (13/107), 2.8% (3/107), respectively. The results were indicated that patients in low SIRI group had better 3-, 5-, and 10-year rates of DFS and OS than those in high SIRI group. However, there were no significant differences between low SIRI group and high SIRI group among 3-, 5-, and 10-year rates (Table 7, Figure 2A–D).
 |
Table 7 3-, 5-, and 10-Year DFS and OS Rates of Breast Cancer Patients |
Association of Molecular Subtypes by Core Needle Biopsy and SIRI in Patients with Breast Cancer
By univariate and multivariate analysis, the molecular subtypes by core needle biopsy was the significant prognostic factor in Table 6. In order to further evaluate the prognostic value of SIRI, the SIRI was accessed by the molecular subtypes. The SIRI with different molecular subtypes was analyzed by the log-rank test. And the patients with low SIRI had longer DFS and OS than those with high SIRI. Moreover, the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in HER2-positive subtype (χ2=5.349, P=0.021 and χ2=3.277, P=0.070, respectively). However, there were no significant differences between low SIRI group and high SIRI group by other molecular subtypes.
Correlation Between Miller and Payne Grade (MPG) and SIRI in Patients with Breast Cancer
According to univariate and multivariate analyses, the MPG was the significant prognostic factor (Table 6). In order to further evaluate the prognostic efficiency of SIRI, we analyzed the SIRI by MPG. The SIRI with different MPG Grade was analyzed by the log-rank test. The mean DFS and OS time for patients with low SIRI were longer than in those with high SIRI. However, there were no significant differences between low SIRI group and high SIRI group by MPG.
Association of Pathological TNM Stage and SIRI in Patients with Breast Cancer
According to univariate and multivariate analyses, pathological TNM stage was the significant prognostic factor. Hence, in order to further to study the prognostic efficiency of SIRI, the SIRI was analyzed by pathological TNM stage. The SIRI with different pathological TNM stage was analyzed by the log-rank test. The mean DFS and OS time for patients with low SIRI were longer than in those with high SIRI. However, there were no significant differences between low SIRI group and high SIRI group by pathological TNM stage.
Correlation Between Ki-67 Status and SIRI in Patients with Breast Cancer
The results indicated that Ki-67 status in both core needle biopsy and postoperative pathology IHC was the significant prognostic factor. In core needle biopsy, the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in Ki-67 negative (χ2=3.195, P=0.074 and χ2=1.393, P=0.238, respectively). Moreover, the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in Ki-67 positive (χ2=1.730, P=0.189 and χ2=5.028, P=0.025, respectively). In postoperative pathology IHC, the mean DFS and OS time for patients with low SIRI by the Log-rank test were longer than in those with high SIRI in Ki-67 negative (χ2=5.451, P=0.020 and χ2=3.360, P=0.067, respectively). And the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in Ki-67 positive (χ2=0.564, P=0.453 and χ2=2.088, P=0.149, respectively).
Association of Neural Invasion and SIRI in Patients with Breast Cancer
The neural invasion was the significant prognostic factor by univariate and multivariate analyses in Table 6. Consequently, in order to further determine the prognostic efficiency of SIRI, the SIRI was analyzed by neural invasion. The results proved that the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in patients without lymph vessel invasion (χ2=8.290, P=0.004 and χ2=7.209, P=0.007, respectively). And the results show that the mean DFS and OS time for patients with low SIRI by the log-rank test were longer than in those with high SIRI in patients with neural invasion (χ2=0.051, P=0.822 and χ2=0.016, P=0.901, respectively).
Discussion
Breast cancer is the most common women cancer and is the major leading cause of cancer-related death all over the world.24 Comprehensive therapies, including operation, chemotherapy, radiotherapy, endocrine therapy, and targeted therapy, have improved survival time and quality of life for these breast cancer patients.25 The neoadjuvant treatment can turn inoperable tumors into operable tumors or reduce tumor stage for more frequent conservative breast surgery. Moreover, NACT has become the standard treatment for locally advanced breast cancer, and the quality of life and clinical outcomes for these patients have largely improved.26 Therefore, it is of importance to search accurate indicator for choosing the optimal treatment regimen and improving clinical outcomes.
Various studies have shown that tumors are associated to systemic inflammation.27–29 However, the mechanisms between tumors and inflammation reaction are yet ambiguous and poorly understood. Some studies have suggested that systemic inflammatory cells, such as neutrophils, monocytes, platelets, and lymphocytes, are linked to prognosis of many malignancies. Neutrophils restrain inflammatory factors, which include matrix metalloproteinase-9 (MMP-9), nuclear factor-κB (NF-kB) and vascular endothelial growth factor (VEGF), to influence the proliferation, development, progression, and metastasis.30–32 Monocytes have been proved that it can promote tumor angiogenesis, inflammatory response and metastases, and releases some cytokines and chemokines, such as oncostatin-M and VEGF, to inhibit the immune system.33,34 Platelets are an indicator of tumor activity and angiogenesis, and are associated with tumor growth, invasion, and metastasis by releasing VEGF-integrin cooperative signaling.35,36 Moreover, lymphocytes are an important component of anticancer immunity and immune surveillance and are associated to prevent the tumor growth and progression.37,38
Some studies have shown that inflammatory markers and immune-based prognostic indexes were used to evaluate the prognosis of breast cancer, such as NLR, d-NLR, MLR/LMR, and PLR.39–41 However, these inflammatory markers were associated with poor prognosis in breast cancer patients, and the potential mechanisms were not yet clear. The SIRI based on three inflammatory cells, such as neutrophil, monocyte, and lymphocyte, and can fully evaluate the balance between host immune and inflammatory condition. Nevertheless, the prognostic value of the preoperative SIRI in breast cancer patients received NACT is still unclear. In the present study, the SIRI was the significant prognostic factor by univariate and multivariate analyses.
In our study, the clinicopathologic and demographic characteristics of all enrolled patients were analyzed. The optimal cutoff value of the SIRI was 0.85×109/L by ROC analysis. The results shown that low SIRI was significantly associated with menopause, US-LNM and total lymph nodes. And the low SIRI was in connection with W, Hb, N, L, M, NLR, MLR, and PLR. Moreover, the low SIRI was also significantly associated with NACT. Meanwhile, the common toxicities after NACT were hematologic and gastrointestinal reaction, and the SIRI had no significance on toxicities of all enrolled patients, excepted diarrhea.
On the basis of univariate and multivariate Cox regression analyses, the clinical T stage, Miller and Payne grade, pathological T stage, pathological TNM stage, core needle biopsy (molecular subtype, ER status, Ki-67 status), postoperative pathology IHC (Ki-67 status), neural invasion, PLR, SIRI, postoperative chemotherapy, postoperative radiotherapy were the independent factors. We also found that patients with low SIRI had better prognosis and survived longer than those with high SIRI. Meanwhile, patients with low SIRI had higher 3-, 5-, and 10-year rates. Moreover, our results indicated that Ki-67 status was the significant prognostic factor, and patients with low SIRI had better prognosis and survived longer than those with high SIRI. The results also indicated that patients with low SIRI had better prognosis than those with high SIRI in patients with neural invasion.
Several limitations are presented in this study. Firstly, this is a retrospective single-center study. And multicenter study and more patients should be enrolled. Secondly, the cases are not more by subgroup analysis, and influence the outcomes. Thirdly, the SIRI value of different studies may be different by different cutoff points or endpoints. Therefore, more and better designed randomized controlled trials should be studied to support our findings, and further to study the SIRI and try to combine with other biomarkers to access the clinical outcome.
Conclusion
SIRI is the significant prognostic factor for breast cancer patients and can effectively predict the survival and prognosis for breast cancer. Taking into consideration the high incidence of breast cancer and the unbalanced distribution of medical conditions in China, the repeatable, convenient and non-invasive biomarkers should be used in the prevention and treatment of breast cancer. A comprehensive understanding of hematological parameters is of great importance for finding new targets for subjective treatment and doctors to implement effective treatment in clinical practice.
Data Sharing Statement
The material supporting the conclusion of this article has been included within the article.
Funding
The work is partly supported by research grants from the National Nature Science Foundation of China (no. 81872160) and Beijing Nature Science Foundation of China (no. 7191009).
Disclosure
The authors declare that they have no competing interests.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.v69.1
2. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi:10.3322/caac.21338
3. Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res. 2017;29(1):1–10. doi:10.21147/j.issn.1000-9604.2017.01.01
4. Livingston-Rosanoff D, Hanlon B, Marka N, et al. Time to initiation of neo-adjuvant chemotherapy for breast cancer treatment does not influence patient survival: A study of US breast cancer patients. Breast J. 2019. doi:10.1111/tbj.13625
5. Brackstone M, Palma D, Tuck AB, et al. Concurrent neoadjuvant chemotherapy and radiation therapy in locally advanced breast cancer. Int J Radiat Oncol Biol Phys. 2017;99(4):769–776. doi:10.1016/j.ijrobp.2017.06.005
6. Davoine E, Dion L, Nyangoh Timoh K, et al. Predictive factors associated with involved margins in breast cancer treated with neoadjuvant chemotherapy followed by breast-conserving therapy. J Gynecol Obstet Hum Reprod. 2019;48(7):467–472. doi:10.1016/j.jogoh.2019.06.005
7. He Z, Song A, Zhang Z, et al. Comparative efficacy of non-pharmacological adjuvant therapies for quality of life in the patients with breast cancer receiving chemo- or radio-therapy: A protocol for systematic review and Bayesian network meta-analysis. Medicine (Baltimore). 2018;97(35):e12096. doi:10.1097/MD.0000000000012096
8. Li X, Dai D, Chen B, Tang H, Wei W. Oncological outcome of complete response after neoadjuvant chemotherapy for breast conserving surgery: a systematic review and meta-analysis. World J Surg Oncol. 2017;15:210. doi:10.1186/s12957-017-1273-6
9. Echeverria GV, Ge Z, Seth S, et al. Resistance to neoadjuvant chemotherapy in triple-negative breast cancer mediated by a reversible drug-tolerant state. Sci Transl Med. 2019;11(488):eaav0936. doi:10.1126/scitranslmed.aav0936
10. Wu D, Chen T, Jiang H, et al. Comparative efficacy and tolerability of neoadjuvant immunotherapy regimens for patients with HER2-positive breast cancer: a network meta-analysis. J Oncol. 2019;2019:3406972. doi:10.1155/2019/3406972
11. Zheng T, Wang A, Hu D, Wang Y. Molecular mechanisms of breast cancer metastasis by gene expression profile analysis. Mol Med Rep. 2017;16(4):4671–4677. doi:10.3892/mmr.2017.7157
12. Apple AC, Schroeder MP, Ryals AJ, et al. Hippocampal functional connectivity is related to self-reported cognitive concerns in breast cancer patients undergoing adjuvant therapy. Neuroimage Clin. 2018;20:110–118. doi:10.1016/j.nicl.2018.07.010
13. Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19(1):2. doi:10.1186/s13058-016-0794-1
14. Hu RJ, Ma JY, Hu G. Lymphocyte-to-monocyte ratio in pancreatic cancer: prognostic significance and meta-analysis. Clin Chim Acta. 2018;481:142–146. doi:10.1016/j.cca.2018.03.008
15. Guo W, Lu X, Liu Q, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for breast cancer patients: an updated meta-analysis of 17079 individuals. Cancer Med. 2019;8(9):4135–4148. doi:10.1002/cam4.2281
16. Liu J, Shi Z, Bai Y, Liu L, Cheng K. Prognostic significance of systemic immune-inflammation index in triple-negative breast cancer. Cancer Manag Res. 2019;11:4471–4480. doi:10.2147/CMAR.S197623
17. Sen L, Lan X, Gao H, et al. Systemic Inflammation Response Index (SIRI), cancer stem cells and survival of localised gastric adenocarcinoma after curative resection. J Cancer Res Clin Oncol. 2017;143:2455–2468. doi:10.1007/s00432-017-2506-3
18. Abdel-Rahman O. Validation of the 8th AJCC prognostic staging system for breast cancer in a population-based setting. Breast Cancer Res Treat. 2018;168(1):269–275. doi:10.1007/s10549-017-4577-x
19. Fouad TM, Barrera AMG, Reuben JM, et al. Inflammatory breast cancer: a proposed conceptual shift in the UICC-AJCC TNM staging system. Lancet Oncol. 2017;18(4):e228–e232. doi:10.1016/S1470-2045(17)30192-4
20. Guo R, Li L, Su Y, et al. Current practice and barriers of mesh-assisted implant-based breast reconstruction in China: A nationwide cross-sectional survey of 110 hospitals. Eur J Surg Oncol. 2019;46:
21. Del Prete S, Caraglia M, Luce A, et al. Clinical and pathological factors predictive of response to neoadjuvant chemotherapy in breast cancer: A single center experience. Oncol Lett. 2019;18(4):3873–3879. doi:10.3892/ol.2019.10729
22. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. doi:10.1016/j.ejca.2008.10.026
23. Hodorowicz-Zaniewska D, Herman K. Principles of follow-up assessments in patients with breast cancer after radical treatment. Pol Przegl Chir. 2017;89(3):36–39. doi:10.5604/0032373X
24. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Canc J Clin. 2018;68:7e30. doi:10.3322/caac.21442
25. Greenlee H, DuPont-Reyes MJ, Balneaves LG, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin. 2017;67(3):194–232.
26. Patel DA, Jing X, Luo J, et al. Campian. Neutrophil-to-lymphocyte ratio as a predictor of survival in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2019;174:443–452. doi:10.1007/s10549-018-05106-7
27. Zhao LY, Yang DD, Ma XK, et al. The prognostic value of aspartate aminotransferase to lymphocyte ratio and systemic immune-inflammation index for overall survival of hepatocellular carcinoma patients treated with palliative treatments. J Cancer. 2019;10(10):2299–2311. doi:10.7150/jca.30663
28. Zhou T, Zhao Y, Zhao S, et al. Comparison of the prognostic value of systemic inflammation response markers in small cell lung cancer patients. J Cancer. 2019;10(7):1685–1692. doi:10.7150/jca.29319
29. Romero-Cordoba S, Meneghini E, Sant M, et al. Decoding immune heterogeneity of triple negative breast cancer and its association with systemic inflammation. Cancers (Basel). 2019;11(7):E911. doi:10.3390/cancers11070911
30. Walz W, Cayabyab FS. Neutrophil infiltration and matrix metalloproteinase-9 in lacunar infarction. Neurochem Res. 2017;42(9):2560–2565. doi:10.1007/s11064-017-2265-1
31. Fusella F, Seclì L, Busso E, et al. The IKK/NF-κB signaling pathway requires Morgana to drive breast cancer metastasis. Nat Commun. 2017;8(1):1636. doi:10.1038/s41467-017-01829-1
32. Tan KW, Chong SZ, Wong FH, et al. Neutrophils contribute to inflammatory lymphangiogenesis by increasing VEGF-A bioavailability and secreting VEGF-D. Blood. 2013;122(22):3666–3677. doi:10.1182/blood-2012-11-466532
33. Laviron M, Combadière C, Boissonnas A. Tracking monocytes and macrophages in tumors with live imaging. Front Immunol. 2019;10:1201. doi:10.3389/fimmu.2019.01201
34. Huang C, Li Z, Li N, et al. 35 expression correlates with microvessel density in pancreatic ductal adenocarcinoma, recruits monocytes, and promotes growth and angiogenesis of xenograft tumors in mice. Gastroenterology. 2018;154(3):675–688. doi:10.1053/j.gastro.2017.09.039
35. Jiang L, Luan Y, Miao X, et al. Platelet releasate promotes breast cancer growth and angiogenesis via VEGF-integrin cooperative signalling. Br J Cancer. 2017;117(5):695–703. doi:10.1038/bjc.2017.214
36. Menter DG, Kopetz S, Hawk E, et al. Platelet “first responders” in wound response, cancer, and metastasis. Cancer Metastasis Rev. 2017;36(2):199–213. doi:10.1007/s10555-017-9682-0
37. Mohme M, Riethdorf S, Pantel K. Circulating and disseminated tumour cells-mechanisms of immune surveillance and escape. Nat Rev Clin Oncol. 2017;14(3):155–167. doi:10.1038/nrclinonc.2016.144
38. Shankaran V, Ikeda H, Bruce AT, et al. IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001;410(6832):1107–1111. doi:10.1038/35074122
39. Chen J, Pan Y, He B, et al. Meta-analysis of prognostic value of inflammation parameter in breast cancer. J Cancer Res Ther. 2018;14(Supplement):S85–S89. doi:10.4103/0973-1482.160917
40. Marín Hernández C, Piñero Madrona A, Gil Vázquez PJ, et al. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin Transl Oncol. 2018;20(4):476–483. doi:10.1007/s12094-017-1732-0
41. Rafee S, McHugh D, Greally M, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as predictive biomarkers of pathologic complete response (pCR) in neoadjuvant breast cancer: an Irish Clinical Oncology Group study (ICORG 16–20). Ann Oncol. 2016;27(suppl 6):1538P. doi:10.1093/annonc/mdw392.20
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.