Back to Journals » Journal of Inflammation Research » Volume 16
Predictive Value of PRISMA-7, qSOFA, ESI, and CFS for 28-Day Mortality in Elderly Patients in the Emergency Department
Authors Hao L, Zhou Y, Zou J, Hao L, Deng P
Received 1 May 2023
Accepted for publication 8 July 2023
Published 13 July 2023 Volume 2023:16 Pages 2947—2954
DOI https://doi.org/10.2147/JIR.S419538
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Liqun Hao,1 Yue Zhou,1 Jiatong Zou,1 Lirong Hao,2 Peng Deng1
1Department of Emergency Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China; 2Department of Emergency Medicine, West China Hospital Shangjin Branch, Sichuan University, Chengdu, Sichuan, People’s Republic of China
Correspondence: Peng Deng, Email [email protected]
Background: To explore the predictive value of the Programme on Research for Integrating Services for the Maintenance of Autonomy 7 (PRISMA-7), quick Sequential Organ Failure Assessment (qSOFA) score, Emergency Severity Index (ESI), and Clinical Frailty Scale (CFS) on the 28-day mortality risk in emergency elderly patients.
Methods: A multicenter prospective observational study was conducted to select elderly patients (≥ 65 years old) admitted to the emergency department of three Grade-A hospitals in different regions of China from January 2020 to March 2022. Primary data were collected at the time of admission. All patients were followed up for 28 days. The primary outcome was 28-day mortality. The predictive value of four scoring systems for 28-day mortality in elderly emergency patients was assessed by receiver operating characteristic (ROC) and logistic regression analysis.
Results: A total of 687 elderly emergency patients were enrolled, of whom 66 (9.61%) died within 28 days. Age, ICU admission rate, PRISMA-7, qSOFA, and CFS were significantly higher in the death group than in the survival group (P < 0.05), and ESI was lower than in the survival group (P < 0.001). The AUC for CFS was the largest of the four scoring systems at 0.80. According to the Youden index, the optimal cutoff values for PRISMA-7, qSOFA, ESI, and CFS were > 3.5, > 0.5, < 2.5, and > 4.5, respectively. Logistic regression revealed that qSOFA and CFS were the primary risk factors for increased 28-day mortality in elderly emergency patients (P < 0.001). The combined predictor L (L=X1+0.50X2, X1 and X2 are qSOFA and CFS values, respectively) had an AUC of 0.86 and a cutoff value > 2.75.
Conclusion: PRISMA-7, qSOFA, ESI, CFS, and the combined qSOFA+CFS predictor were all effective predictors of 28-day mortality risk in elderly emergency patients, with the combined qSOFA+CFS predictor having the best predictive power.
Keywords: PRISMA-7, qSOFA, CFS, elderly patient, prognosis
Introduction
The emergency department plays a vital role in general hospitals at all levels to ensure that patients with critical illness receive efficient and professional emergency treatment at first time.1–3 However, emergency resources are relatively scarce in China’s large population base. In addition, to the ordinary waiting outside for a long time, the professionalism of the doctors, treatment system, and treatment effect are uneven.4 At the same time, the emergency department is also one of the departments with a relatively high incidence of medical disputes, especially among the elderly and dead patients.5,6 Therefore, it is essential to find an effective assessment method or scoring system for the early detection of high-risk elderly emergency patients.
In recent years, the primary assessment scales for the prognosis of elderly patients include the Programme on Research for Integrating Services for the Maintenance of Autonomy 7 (PRISMA-7), the quick sequential organ failure assessment (qSOFA) score, the Emergency Severity Index (ESI), and the Clinical Frailty Scale (CFS).7–9 However, the value of scoring systems in predicting the risk of death in elderly patients in the emergency department has rarely been reported, and their predictive performance is unclear. To clarify the predictive value of the above-mentioned scoring systems for mortality risk in elderly patients in the emergency department, we implemented the present clinical study.
Therefore, this study prospectively included elderly patients attending the emergency departments of three hospitals, collecting baseline information at admission, and performing 28-day post-discharge follow-ups. The study aimed to investigate the value of PRISMA-7, qSOFA, ESI, CFS, and their combinations in the prediction of 28-day mortality risk in elderly emergency patients and to provide a reference for subsequent standardized mortality risk assessment and prediction strategies for elderly emergency patients.
Materials and Methods
Study Design
This study was a prospective multicenter observational study. Elderly patients admitted to the emergency department of West China Hospital of Sichuan University, Nanfu Hospital of Chengdu, and Henan Provincial People’s Hospital from January 2020 to March 2022 were enrolled. All the enrolled patients and their family members were informed and agreed to sign the written consent form for this study. At the same time, the study met the relevant ethical requirements of the Declaration of Helsinki. The Ethics Committee of West China Hospital, Sichuan University, approved the study, and all participants signed an informed consent form (No. 2022–0493). The study was registered with the Chinese Clinical Trials Registry before implementation (ChiCTR2100046545).
Inclusion and Exclusion Criteria for Clinical Trials
Inclusion criteria: (1) Age ≥65 years old; (2) Complete follow-up data for 28 days. Exclusion criteria: (1) Patients or their family members voluntarily gave up treatment during the intervention; (2) Unable to complete the assessment on admission; (3) After pre-hospital cardiopulmonary resuscitation or donor; (4) Loss of follow-up during the 28-day follow-up period.
Sample Size Calculation
The Contingency Table (Chi-Square Tests) in PASS 15.0 software was used to calculate the sample size. Considering an acceptable error rate of 5%, a design and cluster effects of 1.0, and test efficacy of 80%. In this study, the test level α = 0.05, and the test efficacy 1-β = 0.90. We estimated a sample size of 575 participants with a confidence interval of 95% (CI). Considering that some participants did not respond and added 10% of the estimated sample size, the final sample size was 633.
Program Implementation
All enrolled patients were required to sign an informed consent form before being included in the clinical trial. Elderly patients were admitted to the inpatient unit for further treatment after being evaluated by an emergency physician. After admission to the hospital, the primary data of patients were rapidly collected, and the PRISMA-7 (Supplementary Table 1), qSOFA (Supplementary Table 1), ESI (Supplementary Table 2), and CFS (Supplementary Table 3) assessments were completed. All enrolled patients were followed up for 28 days through the hospital HIS system (during hospitalization) or by telephone (after discharge). Finally, we pooled data from the elderly patients at the 3 hospitals for analysis to assess the predictive value of the 4 scoring systems for 28-day mortality in elderly patients.
Outcomes
The primary outcome was the 28-day mortality rate for elderly patients in emergency care. Secondary outcomes included receipt of critical care orders, admission to the intensive care unit, and length of stay.
Statistical Analysis
EXCEL sheets were used to collect data, and GraphPad Prism software (Version 9.4, GraphPad Inc., USA) was used for statistical analysis and mapping. Continuous variables were tested for normality using D ‘Agostino & Pearson and Shapiro–Wilk tests, and those with normal distribution were expressed as mean ± standard deviation. Independent sample t-test was used to compare two groups, and one-way analysis of variance (ANOVA) /Tukey’s test was used to compare multiple groups. Pearson’s test was used for correlation analysis. Skewness distribution in the median (interquartile range), according to the comparison between the two groups, the Mann–Whitney U-test, multiple sets of comparison between the Kruskal Wallis H/the Mann–Whitney U-test, USES Spearman correlation analysis test. Categorical variables were expressed as the number of cases and percentage (%), and the chi-square (χ) test was used to compare groups. In 28 days, whether death is the dependent variable, the establishment of the score of the receiver-operating characteristic (ROC) Curve, calculate the Area Under the Curve (Area Under the Curve, AUC), following the principle of maximum Youden index to determine the critical value (the best cutoff value) and calculate its sensitivity and specific degrees. Binary Logistic regression analysis was used to construct the combined predictor L of multiple scores and draw the ROC curve and subsequent calculation. All statistical tests adopt bilateral inspection. P < 0.05 for the difference was statistically significant.
Results
General Characteristics of the Study Population
Participants included 687 elderly patients in the emergency department (Figure 1). According to whether the death was 28 days, the patients were divided into the death group (n = 66), and survival groups (n = 621), and total mortality was 9.61%. Details of patients’ general conditions and comparison between groups are shown in Table 1. There were no significant differences in gender and length of hospital stay between the two groups. However, the age, proportion of medical orders with critical illness, ICU admission rate, PRISMA-7 score, qSOFA score, and ESI grade of patients in the death group were significantly higher than those in the survival group (P < 0.05).
 |
Table 1 Comparison of the Clinical Characteristics of the Patients |
 |
Figure 1 Flow chart of the research program. |
Predictive Value of Four Scores for 28-Day Mortality Risk in Elderly Patients in the Emergency Department
Taking death at 28 days as the dependent variable (Y=1 in the death group and Y=0 in the survival group), the ROC curve, AUC, critical value, Youden coefficient, sensitivity, and specificity of the four scores for predicting the 28-day mortality risk of elderly patients in the emergency department are shown in Figure 2 and Table 2. The AUC from high to low was CFS (0.80), PRISMA-7 (0.79), qSOFA (0.76), and ESI (0.62), and CFS had the best comprehensive predictive ability. According to the Youden index, the cut-off values of PRISMA-7, qSOFA, ESI, and CFS were > 3.5, >0.5, <2.5, and >4.5, respectively. The sensitivity of ESI was the highest (93.94%), and CFS was the worst (68.18%). The specificity of CFS was the highest (79.23%), and ESI was the worst (22.54%).
 |
Table 2 Predictive Value of the Four Scores for 28-Day Mortality in Elderly Patients in the Emergency Department |
 |
Figure 2 ROC curves of four scores for predicting 28-day mortality risk in elderly patients in the emergency department. (A) PRISMA-7. (B) qSOFA. (C) ESI. (D) CFS. |
Logistic Regression Analysis of Four Scoring Systems and 28-Day Mortality Risk of Elderly Patients in Emergency Department
The Logistic regression analysis was carried out with the 28-day death as the dependent variable (Y=1 in the death group and Y=0 in the survival group) and the four scores as the independent variables. The results are shown in Table 3. qSOFA and CFS were the emergency treatment of elderly patients with 28 days of death risk factors significantly (P < 0.001). Further Spearman correlation analysis showed a significant positive correlation between qSOFA and CFS (R = 0.29, P < 0.001).
 |
Table 3 Logistic Regression Analysis of Four Scoring Systems and 28-Day Mortality Risk in Elderly Patients in the Emergency Department |
Predictive Value of qSOFA Combined with CFS for 28-Day Mortality Risk in Elderly Patients in the Emergency Department
According to the results of Table 3, the binary Logistic regression equation was established: Logit (P) = −5.18 + 1.12×1 + 0.56X2, where X1 and X2 are qSOFA and CFS values, respectively. The equation was transformed into equality, and the partial regression coefficient of X1 was set to 1 to obtain the expression of joint predictor L: L = X1 + 0.50×2. The ROC curve of the joint predictor L for predicting the risk of death in elderly patients in the emergency department, using 28-day mortality as the dependent variable (Y=1 in the death group and Y=0 in the survival group) (Figure 3). The AUC was 0.86 (95% CI: 0.81–0.90), the critical value was >2.75, the Yuden coefficient was 0.54, the sensitivity was 77.27% (95% CI: 65.83–85.71%), and the specificity was 76.65% (95% CI: 73.17–79.81%).
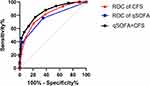 |
Figure 3 ROC curve of qSOFA combined with CFS for predicting 28-day mortality in elderly emergency department patients. |
Discussion
Emergency patients often have life-threatening conditions, especially elderly patients. Effective death risk prediction for elderly emergency patients has important clinical significance in guiding follow-up treatment, improving treatment effect, reducing mortality, and reducing medical disputes. In the past, the modified early warning Score (MEWS) was used to evaluate the five fundamental life indicators (heart rate, systolic blood pressure, respiratory rate, consciousness, and body temperature) of patients in the emergency department, which helped emergency doctors to grasp the situation of patients quickly. However, the misjudgment was more prominent due to the poor specificity of the score and the unclear grading of MEWS.6 This study explored the value of PRISMA-7, qSOFA, ESI, and CFS and their combination in predicting 28-day mortality risk in elderly patients in the emergency department. It confirmed that the sensitivity and specificity of different assessment systems were significantly different. CFS had the best overall predictive power and specificity, while ESI had the highest sensitivity. At the same time, the comprehensive predictive ability of qSOFA combined with CFS was further improved (AUC 0.86), and the sensitivity and specificity were 77.27% and 76.65%, respectively.
The PRISMA-7 is designed to identify frail older adults and is currently used by the Royal College of General Practitioners and the British Geriatrics Society to assess the frailty of the elderly.10 Beauchet et al found that the high-risk level of PRISMA-7 score was closely related to the prolonged length of hospital stay in elderly patients in the emergency department but had low value for the risk of short-term adverse events and prognosis of patients.8 PRISMA-7 is rarely used in China. This study found that PRISMA-7 > 3.5 had a good predictive value for 28-day mortality risk in elderly patients in the emergency department, with a sensitivity and specificity of more than 70%. The qSOFA scoring system was first proposed by the Infection-related Problems working group of the European Association of Intensive Care Medicine in 1994, aiming to describe and monitor the dysfunction and failure process of the respiratory system, cardiovascular system, central nervous system, kidney, liver, coagulation system and so on through simple and objective data.11,12 Seymour et al reported that qSOFA had a particular application value in predicting the risk of death in patients with EICU infection during hospitalization. The AUC was 0.607.13 This study found that the AUC of qSOFA in predicting 28-day mortality risk in elderly patients in the emergency department was 0.76, which was better than that reported in the literature. In this study, we collected data from elderly patients in the emergency department and performed PRISMA-7 and qSOFA assessments. This data truly reflects the status of elderly patients at admission. Therefore, PRISMA-7 and qSOFA are more valuable for predicting 28-day mortality.
ESI system is a 5-level pre-examination process/sensitivity system established by Eitel and Wuerz and another emergency medical staff in 1998 in the United States, which is widely used in European and American countries.14,15 This study found that ESI < 2.5 had a sensitivity of 93.94% but a specificity of 22.54% for predicting 28-day mortality risk in elderly patients in the emergency department. Given its high sensitivity, ESI can help emergency medical staff identify critically ill patients in time and prioritize treatment, especially for inexperienced emergency triage medical staff. However, ESI is not enough applied and promoted in China, and there is no similar research report. It is worth further studying the application value of ESI in emergency patients with larger samples and diseases. CFS is a scale proposed by Rockwood et al in 2005. According to the functional status of patients, CFS can be divided into 9 levels: very healthy, healthy, maintaining healthy, vulnerable, mild frailty, moderate frailty, severe frailty, very severe frailty, and end stage.16 Kaeppeli et al explored the effectiveness of CFS in predicting the 30-day risk of death, ICU admission, and hospitalization in the emergency department. They found that CFS outperformed ESI in predicting the 30-day risk of death in the emergency department.17 In this study, CFS’s comprehensive predictive power (AUC 0.80 vs 0.62) and specificity (79.23% vs 22.54%) were better than ESI’s. However, the sensitivity was significantly lower than ESI’s (68.18% vs 93.94%).
For emergency patients, both sensitivity and specificity are essential. In order to determine whether the combination of the four scores could improve the predictive ability, this study first screened out the increased qSOFA and CFS as significant independent risk factors for increased 28-day mortality risk in elderly emergency patients by regression analysis. It further evaluated the predictive value of the combination of the two scores. The results showed that the AUC of the combination of qSOFA and CFS increased to 0.86, suggesting that the combination of qSOFA and CFS had a more substantial predictive power than the single application. At the same time, the sensitivity of the combination of qSOFA and CFS was 77.27%, which was higher than that of the two alone (qSOFA: 75.76%; CFS: 68.18%). The specificity was 76.65%, slightly lower than that of CFS alone (79.23%) but significantly higher than that of qSOFA alone (64.73%). In conclusion, the combination of qSOFA and CFS has an excellent predictive value for 28-day mortality risk in elderly patients in the emergency department.
There are also some limitations to this study. Emergency department patients are often complicated with many comorbidities, and the coordinated action of multiple etiologies often causes changes in vital signs and clinical symptoms upon admission. This study only evaluated elderly patients in the emergency department during pre-examination and triage. Based on this, it calculated their 28-day mortality risk and did not classify them according to their primary diagnosis. Of course, it is prevalent for the primary diagnosis of emergency patients to be unclear or revised at the time of admission and after that, which poses a significant challenge for subsequent classification research.
Conclusion
In conclusion, PRISMA-7>3.5, qSOFA>0.5, ESI<2.5, CFS>4.5, and the combined qSOFA+CFS predictor L>2.75 (L=X1+0.50X2, X1 and X2 are qSOFA and CFS, respectively) all had predictive value for the risk of 28-day mortality in elderly emergency patients. ESI has the highest sensitivity, CFS has the highest specificity, and qSOFA combined with CFS has the best comprehensive predictive ability. Therefore, PRISMA-7, qSOFA, ESI, CFS, and qSOFA+CFS combined predictors are all effective predictors for 28-day mortality risk in elderly patients in the emergency department and have proper clinical application and promotion value.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of West China Hospital, Sichuan University and all participants signed an informed consent form (No. 2022-0493).
Acknowledgments
We are sincerely grateful to all the researchers and patients who participated in this study.
Funding
This work was supported by a grant from the Peking Union Medical Foundation - Rui E (Rui Yi) Special Fund for Emergency Medicine Research (No. 22222012003).
Disclosure
The authors have declared no conflicts of interest with respect to the authorship or publication of this article.
References
1. Blackburn J, Ousey K, Goodwin E. Information and communication in the emergency department. Int Emerg Nurs. 2019;42:30–35. doi:10.1016/j.ienj.2018.07.002
2. Morris ZS, Boyle A, Beniuk K, Robinson S. Emergency department crowding: towards an agenda for evidence-based intervention. Emerg Med J. 2012;29(6):460–466. doi:10.1136/emj.2010.107078
3. Moskop JC, Geiderman JM, Marshall KD, et al. Another look at the persistent moral problem of emergency department crowding. Ann Emerg Med. 2019;74(3):357–364. doi:10.1016/j.annemergmed.2018.11.029
4. Niu Y, Gao Y, Yang J, et al. Short-term effect of apparent temperature on daily emergency visits for mental and behavioral disorders in Beijing, China: a time-series study. Sci Total Environ. 2020;733:139040. doi:10.1016/j.scitotenv.2020.139040
5. Wu Y, Jiang F, Ma J, et al. Experience of medical disputes, medical disturbances, verbal and physical violence, and burnout among physicians in China. Front Psychol. 2021;11:556517. doi:10.3389/fpsyg.2020.556517
6. Orr Z, Jackson L, Alpert EA, et al. Neutrality, conflict, and structural determinants of health in a Jerusalem emergency department. Int J Equity Health. 2022;21(1):89. doi:10.1186/s12939-022-01681-w
7. Miranda LA, Luvizutto GJ, Stephan BCM, et al. Evaluating the performance of the PRISMA-7 frailty criteria for predicting disability and death after acute ischemic stroke. J Stroke Cerebrovasc Dis. 2022;31(12):106837. doi:10.1016/j.jstrokecerebrovasdis.2022.106837
8. Guo Q, Li HY, Song WD, et al. qSOFA predicted pneumonia mortality better than minor criteria and worse than CURB-65 with robust elements and higher convergence. Am J Emerg Med. 2022;52:1–7. doi:10.1016/j.ajem.2021.11.029
9. Luoto J, Pihlsgård M, Pistolesi M, et al. Emphysema severity index (ESI) associated with respiratory death in a large Swedish general population. Respir Med. 2022;200:106899. doi:10.1016/j.rmed.2022.106899
10. Beauchet O, Fung S, Launay CP, et al. Screening for older inpatients at risk for long length of stay: which clinical tool to use? BMC Geriatr. 2019;19(1):156. doi:10.1186/s12877-019-1165-4
11. Beauchet O, Galery K, Vilcocq C, et al. PRISMA-7 and risk for short-term adverse events in older patients visiting the emergency department: results of a large observational and prospective cohort study. J Nutr Health Aging. 2021;25(1):94–99. doi:10.1007/s12603-020-1463-8
12. Ling H, Chen M, Dai J, Zhong H, Chen R, Shi F. Evaluation of qSOFA combined with inflammatory mediators for diagnosing sepsis and predicting mortality among emergency department. Clin Chim Acta. 2023;17:117352. doi:10.1016/j.cca.2023.117352
13. Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):762–774. doi:10.1001/jama.2016.0287
14. Wuerz RC, Travers D, Gilboy N, et al. Implementation and refinement of the emergency severity index. Acad Emerg Med. 2001;8(2):170–176. doi:10.1111/j.1553-2712.2001.tb01283.x
15. Jordi K, Grossmann F, Gaddis GM, et al. Nurses’ accuracy and self-perceived ability using the emergency severity index triage tool: a cross-sectional study in four Swiss hospitals. Scand J Trauma Resusc Emerg Med. 2015;23:62. doi:10.1186/s13049-015-0142-y
16. Darvall JN, Bellomo R, Bailey M, et al. Impact of frailty on persistent critical illness: a population-based cohort study. Intensive Care Med. 2022;48(3):343–351. doi:10.1007/s00134-022-06617-0
17. Kaeppeli T, Rueegg M, Dreher-Hummel T, et al. Validation of the clinical frailty scale for prediction of thirty-day mortality in the emergency department. Ann Emerg Med. 2020;76(3):291–300. doi:10.1016/j.annemergmed.2020.03.028
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
