Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
Predictive Role of White Blood Cell Differential Count for the Development of Acute Exacerbation in Korean Chronic Obstructive Pulmonary Disease
Authors Yoon EC, Koo SM , Park HY, Kim HC , Kim WJ , Kim KU, Jung KS, Yoo KH , Yoon HK, Yoon HY
Received 18 August 2023
Accepted for publication 15 December 2023
Published 4 January 2024 Volume 2024:19 Pages 17—31
DOI https://doi.org/10.2147/COPD.S435921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Eun Chong Yoon,1 So-My Koo,1 Hye Yun Park,2 Ho Cheol Kim,3 Woo Jin Kim,4 Ki Uk Kim,5 Ki-Suck Jung,6 Kwang Ha Yoo,7 Hyoung Kyu Yoon,8 Hee-Young Yoon1
1Division of Allergy and Respiratory Diseases, Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Seoul, Republic of Korea; 2Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea; 3Department of Internal Medicine, Gyeongsang National University Changwon Hospital, Gyeongsang National University School of Medicine, Changwon, Republic of Korea; 4Department of Internal Medicine and Environmental Health Center, Kangwon National University, Chuncheon, Republic of Korea; 5Department of Internal Medicine, Pusan National University Hospital, Busan, Republic of Korea; 6Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Republic of Korea; 7Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Republic of Korea; 8Department of Internal Medicine, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
Correspondence: Hee-Young Yoon, Soonchunhyang University Seoul Hospital, 59, Daesagwan-ro, Yongsan-gu, Seoul, 04401, Republic of Korea, Tel +82-10-8728-6950, Fax +82-2-709-9554, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) is a respiratory disease characterized by chronic inflammation. Acute exacerbation of COPD (AECOPD) manifests as acute worsening of respiratory symptoms and is associated with high morbidity and mortality. The aim of the present study was to evaluate the predictive value of white blood count (WBC) and its derived inflammatory biomarkers for AECOPD.
Methods: From the Korean COPD Subgroup Study cohort, a prospective and multicenter observational study, 826 patients who had baseline complete blood count (CBC) and 3-year AECOPD data were included. Follow-up CBC data at 1 (n = 385), 2 (n = 294), and 3 (n = 231) years were collected for available patients. The primary outcome was the occurrence of AECOPD at 3 years. The risk of AECOPD was evaluated using a binary logistic analysis.
Results: The cumulative incidences of 12-, 24-, and 36-month AECOPD were 47.6%, 60.5%, and 67.6%, respectively. Patients with AECOPD at 3 years had higher baseline WBC counts, neutrophil counts, neutrophil/lymphocyte ratio (NLR), and neutrophil/monocyte ratio than those without AECOPD. Higher WBC count, neutrophil count, and NLR were associated with the 3-year occurrence of AECOPD in the univariate analysis, but only the higher neutrophil count was a significant risk factor (odds ratio [OR] = 1.468; 95% confidence interval [CI]: 1.024– 2.104) in the covariates-adjusted analysis. In the analysis of changes in inflammatory parameters, a decrease in the platelet count (OR = 0.502; 95% CI: 0.280– 0.902) and NLR (OR = 0.535; 95% CI: 0.294– 0.974) at 2 years and an increase in the eosinophil count (OR = 2.130; 95% CI: 1.027– 4.416) at 3 years were significantly associated with AECOPD in the adjusted analysis.
Conclusion: Our data suggest that a high baseline WBC count, particularly neutrophil count, was associated with a higher incidence of long-term AECOPD.
Keywords: blood cell count, blood platelets, eosinophils, lymphocytes, neutrophils, pulmonary disease, chronic obstructive
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent, often progressive airflow obstruction and tissue destruction.1 It is a leading cause of death and disability worldwide, estimated to affect nearly 400 million people globally.2 Long-term exposure to tobacco smoke is the most significant risk factor of COPD, and air pollution, genetic factors, and respiratory infections can also contribute to the development of COPD.2,3 Acute exacerbation of COPD (AECOPD) manifests as sudden worsening of COPD symptoms, including dyspnea, coughing, and sputum production. Various factors, including respiratory infections, air pollution, and exposure to allergens, can trigger AECOPD.4,5 The prognosis of AECOPD depends on the severity of the exacerbation and the patient’s comorbidities. AECOPD can be severe and associated with significant morbidity and mortality, particularly in patients with more impaired lung function or multiple comorbidities, such as cardiovascular disease or diabetes.6,7 Therefore, identifying predictive markers to screen high-risk populations is important.
Systemic inflammation causes the progression or worsens the outcomes of COPD.8 The complete blood count (CBC) can measure various components of inflammation, including the white blood cell (WBC) count, to assess the presence and severity of systemic inflammation. In patients with COPD, WBC may show increased/decreased neutrophil and monocyte counts, depending on the stage and severity of COPD.9,10 Additionally, the neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio, and monocyte/lymphocyte ratio (MLR) are composite inflammatory biomarkers that can be calculated using values obtained from CBC. These WBC-related biomarkers reflect the overall inflammation status of the body and are associated with the severity and prognosis of COPD.11–19 However, the association between the long-term prognosis, particularly the risk of AECOPD, and WBC differential count and WBC-derived inflammatory markers is poorly understood. Therefore, the aim of the present study was to evaluate the predictive value of WBC differential count and WBC-derived inflammatory biomarkers for the long-term occurrence of AECOPD in Korean patients with COPD.
Materials and Methods
Study Population
We screened 3478 patients with COPD registered in the Korean COPD Subtype Study (KOCOSS) cohort from 2012 to 2017 (Figure 1). The KOCOSS cohort is a prospective, multicenter observational cohort consisting of patients with COPD from 52 participating referral centers across Korea.20
Inclusion criteria of KOCOSS were: 1) Korean adults with COPD over 40 years of age; and 2) a ratio of forced expiratory volume in 1 s to forced vital capacity (FEV1/FVC) < 0.7 after bronchodilator use. After excluding patients without baseline CBC data (n = 478) and those without 3-year follow-up data for the occurrence of AECOPD (n = 2174), we included 826 patients with COPD.
Ethics
This study was conducted in accordance with the Declaration of Helsinki. All patients provided informed consent for the use of clinical data. Ethics approval was obtained from all medical institutions, including the Institutional Review Board of the Soonchunhyang University Seoul Hospital (2022-03-019).
Clinical Data Collection
At the time of enrollment, baseline data were collected from a self-reported questionnaire, including demographics, smoking status, body mass index (BMI), comorbidities including history of asthma, chronic respiratory symptoms such as cough or sputum lasting over 3 months, and previous history of exacerbations during the 1 year before enrollment. An abnormal finding on the baseline chest X-ray was reviewed. In addition, our study assessed all respiratory medications, including inhalers, using multiple selection at the time of registration.
To measure the quality of life in patients with COPD, St. George’s respiratory questionnaire (SGRQ), symptom scores from the COPD assessment test (CAT) and modified Medical Research Council (mMRC) dyspnea grade were obtained. Spirometry and body plethysmography were performed based on the European Respiratory Society (ERS)/American Thoracic Society (ATS) guideline.21,22 Diffusing capacity for carbon monoxide (DLco) was also measured using the single-breath method following the ERS/ATS guideline.23 The predicted percentage values were calculated using an equation developed for the Korean population.24,25 According to the 2023 Global Initiative for Chronic Obstructive Lung Disease guidelines (GOLD),1 patients were classified based on FEV1: GOLD 1, FEV1 ≥ 80% predicted; GOLD 2, FEV1 ≥ 50% and < 80% predicted; GOLD 3, FEV1 ≥ 30% and < 50% predicted; and GOLD 4, FEV1 < 30% predicted. A six-minute walk test (6MWT) was performed based on the ATS guidelines.26 Over 3 years, prospective clinical data were collected using a study design that followed-up participants at regular intervals of 1 year.
WBC Differential Count and Derived Parameters
At each participating center, the total WBC, neutrophil, lymphocyte, monocyte, eosinophil, and basophil counts were measured at the time of enrollment, with the majority of participants in a stable condition. Using the initial CBC test, the following WBC-derived composite parameters were calculated: NLR, derived neutrophil/lymphocyte ratio (dNLR, calculated as the absolute neutrophil count/WBC – absolute neutrophil count), neutrophil/monocyte ratio, platelet/lymphocyte ratio, MLR, and eosinophil/basophil ratio (EBR).
For patients with available follow-up CBC data at 1 (n = 385), 2 (n = 294), and 3 (n = 231) years, changes in WBC differential parameters were determined by calculating differences between baseline and follow-up CBC values for each patient.
Clinical Outcomes
The study protocol was designed to track the incidence and frequency of moderate to severe exacerbations over a 3-year period, starting from the time of enrollment. The occurrence of AECOPD was documented through self-reporting questionnaires and medical chart reviews conducted at yearly intervals. A moderate AECOPD was defined as a deterioration in symptoms, such as increased sputum production or worsened breathlessness, resulting in the administration of antibiotics or steroids during outpatient visits. A severe AECOPD, on the other hand, was characterized by a significant exacerbation of respiratory symptoms necessitating urgent medical attention or hospitalization. The primary outcome was the occurrence of AECOPD at 3 years, and the secondary outcome was the cumulative occurrence of AECOPD over the 3-year period.
Statistical Analysis
Continuous variables are expressed as mean ± standard deviation or median (interquartile range), while categorical variables are expressed as frequency (percentage). Since WBC derived parameters were skewed, they were log-transformed before analyses and treated as continuous variables. The inflammatory markers were analyzed as categorical variables by dividing them into higher and lower groups based on the median values. To analyze serial changes in inflammatory parameters, we categorized parameters that remained stable or increased during the follow-up compared to baseline as “increased” and used them in the analyses.
To compare the two groups, Student’s t-test or Mann–Whitney U-test were used for continuous variables and chi-square test or Fisher’s exact test for categorical variables. The cumulative incidence of AECOPD during the follow-up was estimated by using the Kaplan–Meier method. The binary logistic analysis was used to identify the risk factors of 3-year cumulative AECOPD, presented as odds ratio (OR) with 95% confidence interval (CI). The univariate and covariates-adjusted multivariable analyses (age, sex, smoking status, BMI, previous AECOPD history, FEV1, FVC, CAT total score, use of a long-acting muscarinic antagonist [LAMA], inhaled corticosteroid/long-acting beta-agonist combination [ICS/LABA]) were performed. Statistical analyses were conducted using SPSS software version 23.0 (IBM, Armonk, NY, USA). A p-value < 0.05 was considered to indicate statistical significance.
Results
Comparison of Clinical Parameters Between the AE and Non-AE Patients
We enrolled 826 patients, including 758 (91.8%) men and 68 (8.2%) women, with a mean age of 68.6 years. Of all patients, 90.9% were ever-smokers (Table 1). The most common comorbidity was asthma (36.9%), followed by hypertension (36.6%) and a history of tuberculosis (27.9%). Over the 3-year follow-up, 558 patients experienced moderate to severe AECOPD, with cumulative incidence rates of 47.6% at 12 months, 60.5% at 24 months, and 67.6% at 36 months (Figure 2a). The cumulative incidences of moderate AECOPD at 12, 24, and 36 months were 47.7%, 56.5%, and 63.2%, respectively (Figure 2b), while those of severe AECOPD were 13.1%, 20.2%, and 26.6%, respectively (Figure 2c).
 |
Table 1 Comparison of Baseline Characteristics Between Patients with and without 3-Year AECOPD |
Patients with AECOPD at 3 years had a higher rate of osteoporosis, chronic cough and sputum, emphysema on chest X-ray and previous history of AE in the past year than those without (Table 1). In addition, patients with AECOPD had impaired lung function, with lower pre- and post-bronchodilator FEV1, FVC and lower DLco than those without AECOPD. Patients with AECOPD also had lower distance in 6MWT, higher CAT total score, SGRQ score, and mMRC grade than those without AECOPD (Table 2). Patients with AECOPD were more likely to be treated with inhalers, including LAMA monotherapy, ICS/LABA, ICS/LABA/LAMA, and methylxanthine, than those without AECOPD (Table 3).
 |
Table 2 Comparison of Lung Function, Exercise Capacity, Life Quality Between Patients with and without 3-Year AECOPD |
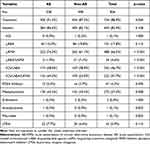 |
Table 3 Comparison of the Treatment Status Between Patients with and without 3-Year AECOPD |
Patients with AECOPD had higher WBC count, neutrophil counts and NLR than those without AECOPD. Conversely, hemoglobin levels were lower in patients with AECOPD than in those without AECOPD (Table 4).
 |
Table 4 Comparison of Laboratory Findings Between Patients with and without 3-Year AECOPD |
Baseline Risk Factors for 3-Year AECOPD
The univariate analysis revealed that both continuous and high WBC and neutrophil counts and continuous NLR were associated with the development of AECOPD at the 3-year follow-up (Table 5). However, in the covariate-adjusted multivariable models, only a higher neutrophil count was associated with the occurrence of AECOPD in patients with COPD (OR = 1.468; 95% CI: 1.024–2.104; p = 0.036).
 |
Table 5 Univariate and Multivariable Logistic Analysis for the Risk Factors of 3-Year AECOPD Among Baseline WBC |
The univariate analysis showed that both continuous and higher WBC and neutrophil counts, NLR, dNLR, and continuous MLR were associated with the 3-year cumulative AECOPD (Supplementary Table 1). However, in multivariable models adjusted for other covariates, only continuous WBC (OR = 2.366; 95% CI: 1.211–4.623; p = 0.012) and high neutrophil counts (OR = 1.703; 95% CI: 1.153–2.517; p = 0.008) were independently associated with the development of 3-year cumulative AECOPD.
Changes in Risk Factors for 3-Year AECOPD
A subgroup analysis was conducted to identify the risk factors for AECOPD in patients with CBC data available during 1 (n = 385), 2 (n = 294), and 3 (n = 231) years of follow-up (Table 6). In the univariate analysis, an increase in basophils during the first year was associated with the occurrence of AECOPD at 3 years. However, no significant factor was identified in patients with 1-year follow-up CBC data in the multivariable analysis. Among patients whose CBC data were available for 2 years, the univariate analysis showed that increased lymphocyte and reduced platelet counts and NLR were significantly associated with AECOPD. In the multivariable analysis, reduced platelet count (OR = 0.502; 95% CI: 0.280–0.902; p = 0.021) and NLR (OR = 0.535; 95% CI: 0.294–0.974; p = 0.041) remained significantly associated with the occurrence of AECOPD. In the univariate analysis including 3-year changes in CBC data, an increase in lymphocyte, eosinophil counts and EBR during the 3 years was associated with AECOPD. However, in the multivariable analysis after adjusting for other covariates, only increased eosinophil count (OR = 2.130; 95% CI: 1.027–4.416; p = 0.042) and EBR (OR = 3.276; 95% CI: 1.463–7.336; p = 0.004) were significantly associated with the occurrence of AECOPD.
 |
Table 6 Univariate and Multivariable Logistic Analysis for the Risk Factors of 3-Year AECOPD in WBC Changes |
In the univariate analysis, reduced platelet count over 1 year, reduced monocyte count and MLR over 2 years, and reduced NLR and dNLR over 3 years were associated with the development of 3-year cumulative AECOPD (Supplementary Table 2). However, after adjusting for covariates, only reduced platelet count (OR = 0.484; 95% CI: 0.262–0.896; p = 0.021) and MLR (OR = 0.525; 95% CI: 0.282–0.978; p = 0.042) for 1 year were significant risk factors for the development of cumulative AECOPD over 3 years.
Discussion
We investigated the predictive value of WBC differential count and its derived parameters for 3-year AECOPD in a large, multicenter Korean study. Our findings showed that patients with AECOPD at 3 years had a higher WBC differential count, particularly neutrophil count, and derived parameters compared to those without AECOPD. Among various WBC parameters, a higher neutrophil count was associated with an increased incidence of long-term AECOPD. Additionally, 3-year AECOPD was associated with high eosinophil count during the follow-up and reduced platelet count and NLR.
In the present study, an increased baseline neutrophil count was associated with the occurrence of 3-year AECOPD, consistent with a previous study demonstrating the link between the neutrophil and the prognosis of COPD.10 In a large population-based COPD registry from East Scotland (n = 7220), patients with a high blood neutrophil count (6000–15,000 cells/μL) had more impaired lung function and a higher average rate of AECOPD (2.3/year [higher] vs 1.3/year [normal], p < 0.001), including severe exacerbations (13% vs 5%, p < 0.001) in the year following the CBC measurement compared to those with a normal neutrophil count (2000–6000 cells/μL).10 Another Chinese study by Yan et al demonstrated that a high neutrophil count based on a median value (> 86%) was associated with an increased risk of severe AE (adjusted OR = 1.68; 95% CI:1.09–2.62) during a 1-year follow-up in a prospective COPD cohort (n=521).27 Moreover, NLR, a composite biomarker of neutrophils and lymphocytes, was effective in predicting AECOPD in several previous studies.28 Lee et al reported that baseline NLR was significantly associated with acute exacerbations at the 1-year follow-up (adjusted OR = 1.16; 95% CI: 1.04–1.29) in our cohort (n = 855).19 However, in the present study, NLR was associated with 3-year AECOPD in the univariate analysis but lost statistical significance after adjusting for other covariates in the multivariable analysis. These results suggest that neutrophils, rather than lymphocytes, may have a more significant impact on long-term AECOPD by reflecting the chronic systemic inflammatory status.
Possible mechanisms through which neutrophils contribute to long-term AECOPD are as follows: Elevated levels of neutrophils in the airways can cause chronic inflammation, leading to long-term exacerbations of COPD. A study by Day et al found an increased bronchoalveolar lavage median neutrophil count in frequent exacerbators (n=13, 9.4%) compared to infrequent exacerbators (n=17, 3.1%) in patients with COPD,29 which supports the role of airway neutrophils in AECOPD. Additionally, the release of proteases and oxidative stress by neutrophils can cause persistent damage to lung tissues, leading to AECOPD.30,31 The release of cytokines and proteases by neutrophils, such as neutrophil elastase, matrix metalloproteinase, and myeloperoxidase, can lead to airway remodeling,32 resulting in long-term changes in the airway structure and function, contributing to AECOPD.33 Furthermore, Yang et al found that increased sputum neutrophil proportions were associated with a higher risk of severe AE only in the presence of air trapping in patients with COPD.27 The process of tissue remodeling that occurs in response to high levels of airway neutrophil inflammation may involve repairing damaged tissue, as well as the loss and thickening of small airways. These changes can also contribute to the development of air trapping, which can lead to further damage to the lung structure and function.34 Day et al also showed that acinar ventilation heterogeneity, a surrogate parameter for small airway disease, was significantly higher in the frequent exacerbator group compared to the infrequent exacerbator group (p = 0.027).29 However, the mechanisms linking neutrophils and AECOPD in patients with COPD are poorly understood and require further research.
In the present study, elevated eosinophil count during the 3-year period was associated with the development of AECOPD at 3 years. The association between the eosinophil count and recurrence of AECOPD has been demonstrated in patients with AECOPD.35,36 However, the association between the eosinophil count and AECOPD in a stable patient remains controversial.37–40 A post-hoc analysis of 11 clinical trials (n = 22,125) revealed that the rate of annual exacerbation did not vary significantly with the eosinophil count (0.62 [≤ 150 cells/μL] vs 0.65 [151– 300 cells/μL] vs 0.67 [> 300 cells/μL]), regardless of the ICS use or previous AECOPD rate.37 Kerkhof et al also exhibited that a high baseline eosinophil count (≥ 450 cells/μL) might be a predictor for 1-year AECOPD only in ex-smokers (adjusted relative risk = 1.32; 95% CI: 1.15–1.51) in 8318 patients with stable COPD.38 However, another small retrospective study (n = 247) showed that a high blood eosinophil count (≥ 2%) was a significant risk factor for the occurrence of AECOPD during 12 months (covariates-adjusted OR = 2.98; 95% CI: 1.42–6.25).39 Eosinophil-associated proinflammatory factors have been detected in the airways and blood of COPD patients, implying a possible contribution of eosinophils to the development of AECOPD in these patients.41 However, a post-hoc analysis of the ECLIPSE study found that only 37.4% of patients with COPD had persistently elevated blood eosinophil counts (≥ 2% at baseline and 1, 2, and 3 years), while 49% had intermittent elevation.42 In the present study, an increased eosinophil count at 3 years was significantly associated with 3-year AECOPD, but an increased baseline eosinophil count was not. These findings suggest that sustained eosinophil inflammation is a factor predicting AECOPD, underscoring the significance of monitoring the eosinophil count as a potential biomarker for AECOPD.
Furthermore, reduced platelet count and NLR were associated with 3-year AECOPD in the present study. This is contrary to most previous studies, which have reported increased platelet count or NLR being associated with a poor prognosis of COPD.28,43 However, the present study had a relatively small sample size of patients with available CBC data during the 3-year follow-up (385 at 1 year, 294 at 2 years, and 231 at 3 years), which may have introduced potential bias. Therefore, these results should be interpreted cautiously, and further research with larger sample sizes and longer follow-up periods is required to validate these findings.
The present study has some limitations. First, the study design was retrospective. Therefore, the study was based on pre-existing data and limited by the accuracy and completeness of the recorded data. Consequently, only 826 of the 3478 patients registered in the cohort could be included. Notably, the reasons for patient dropout, which could include the possibility of mortality, remain unknown, potentially introducing selection bias. Second, the study was conducted at multiple centers, which may have introduced inter-center variability in patient selection and management. Thirdly, we collected several clinical data, such as comorbid conditions and medication history, via self-administered questionnaires, which may introduce biases as it relies on subjective patient responses rather than mandatory medical record reviews. Nonetheless, data were collected in a uniform format at each institution, and most included institutions were secondary or tertiary, with proper quality control of tests, including CBC. Finally, we could not establish causality between the identified factors and the occurrence of AECOPD. Further prospective studies are required to confirm these findings and explore the underlying mechanisms. Despite these limitations, the present study provided valuable insights into the predictive value of WBC differential count and derived parameters for the incidence of 3-year AECOPD in the Korean population.
Conclusion
We evaluated the predictive value of WBC differential count and its derived parameters for 3-year AECOPD in this large-scale, multicenter Korean study. Our findings suggest that a high WBC differential count, particularly neutrophil count, was associated with an increased incidence of long-term AECOPD. These results indicate that WBC differential count and WBC derived parameters may serve as useful predictive markers for AECOPD. Further prospective studies are required to confirm these results and explore the underlying mechanisms.
Abbreviations
COPD, chronic obstructive pulmonary disease; AECOPD, acute exacerbation of chronic obstructive pulmonary disease; AE, acute exacerbation; BMI, body mass index; GERD, gastroesophageal reflux disease; IQR, interquartile range; TB, tuberculosis; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; FEF25-75, forced expiratory flow between 25–75% of vital capacity; DLco, diffusing capacity for carbon monoxide; DL/VA, diffusing capacity for carbon monoxide/alveolar volume; Hb, hemoglobin; TLC, total lung capacity; VC, vital capacity; IC, inspiratory capacity; FRC, functional residual capacity; RV, residual volume; mMRC, modified Medical Research Council; CAT, COPD Assessment Test; SGRQ, St. George’s Respiratory Questionnaire; SpO2, oxygen saturation; ICS, inhaled corticosteroid; LABA, long-acting beta agonist; LAMA, a long-acting muscarinic antagonist; PDE4 inhibitor, phosphodiesterase-4 inhibitor; LTRA, leukotriene receptor antagonist; CBC, complete blood count; OR, odds ratio; CI, confidence interval; WBC, white blood cell; NLR, neutrophil/lymphocyte ratio; dNLR, derived neutrophil/lymphocyte ratio; MLR, monocyte/lymphocyte ratio; EBR, eosinophil/basophil ratio; KOCOSS, Korean COPD Subtype Study.
Data Sharing Statement
Data generated and/or analyzed during the study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
All patients signed an informed consent form for the use of clinical data, and ethics approval was obtained from all medical institutions, including the Institutional Review Board of the Soonchunhyang University Seoul Hospital (2022-03-019).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Soonchunhyang University Research Fund and the Research Program funded Korea National Institute of Health (Fund CODE 2016ER670100, 2016ER670101, 2016ER670102, 2018ER67100, 2018ER67101, 2018ER67102, 2021ER120500, 2021ER120501, and 2021ER120502).
Disclosure
The authors declare that they have no conflicts of interests.
References
1. Agustí A, Celli BR, Criner GJ, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med. 2023;207(7):819–837. doi:10.1164/rccm.202301-0106PP
2. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–458. doi:10.1016/s2213-2600(21)00511-7
3. Raherison C, Girodet P-O. Epidemiology of COPD. Eur Respir Rev. 2009;18(114):213–221. doi:10.1183/09059180.00003609
4. Kim V, Aaron SD. What is a COPD exacerbation? Current definitions, pitfalls, challenges and opportunities for improvement. Eur Respir J. 2018;52(5):1801261. doi:10.1183/13993003.01261-2018
5. Hogea S-P, Tudorache E, Fildan AP, Fira-Mladinescu O, Marc M, Oancea C. Risk factors of chronic obstructive pulmonary disease exacerbations. Clin Respir J. 2020;14(3):183–197. doi:10.1111/crj.13129
6. Choi J, Sim JK, Oh JY, et al. Prognostic marker for severe acute exacerbation of chronic obstructive pulmonary disease: analysis of diffusing capacity of the lung for carbon monoxide (DLCO) and forced expiratory volume in one second (FEV1). BMC Pulm Med. 2021;21(1):152. doi:10.1186/s12890-021-01519-1
7. Steer J, Gibson GJ, Bourke SC. Predicting outcomes following hospitalization for acute exacerbations of COPD. QJM. 2010;103(11):817–829. doi:10.1093/qjmed/hcq126
8. Oudijk EJD, Lammers JWJ, Koenderman L. Systemic inflammation in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(46 suppl):5s–13s. doi:10.1183/09031936.03.00004603a
9. Lin CH, Li YR, Lin PR, et al. Blood monocyte levels predict the risk of acute exacerbations of chronic obstructive pulmonary disease: a retrospective case-control study. Sci Rep. 2022;12(1):21057. doi:10.1038/s41598-022-25520-8
10. Lonergan M, Dicker AJ, Crichton ML, et al. Blood neutrophil counts are associated with exacerbation frequency and mortality in COPD. Respir Res. 2020;21(1):166. doi:10.1186/s12931-020-01436-7
11. El-Gazzar AG, Kamel MH, Elbahnasy OKM, El-Naggar ME-S. Prognostic value of platelet and neutrophil to lymphocyte ratio in COPD patients. Expert Rev Respir Med. 2020;14(1):111–116. doi:10.1080/17476348.2019.1675517
12. Luo Z, Zhang W, Chen L, Xu N. Prognostic value of neutrophil: lymphocyte and platelet: lymphocyte ratios for 28-day mortality of patients with AECOPD. Int J Gen Med. 2021;14:2839–2848. doi:10.2147/ijgm.S312045
13. Xiong W, Xu M, Zhao Y, Wu X, Pudasaini B, Liu JM. Can we predict the prognosis of COPD with a routine blood test? Int J Chron Obstruct Pulmon Dis. 2017;12:615–625. doi:10.2147/copd.S124041
14. Taylan M, Demir M, Kaya H, et al. Alterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patients. Clin Respir J. 2017;11(3):311–317. doi:10.1111/crj.12336
15. Aksoy E, Karakurt Z, Gungor S, et al. Neutrophil to lymphocyte ratio is a better indicator of COPD exacerbation severity in neutrophilic endotypes than eosinophilic endotypes. Int J Chron Obstruct Pulmon Dis. 2018;13:2721–2730. doi:10.2147/copd.S170353
16. Koo HK, Kang HK, Song P, Park HK, Lee SS, Jung H. Systemic white blood cell count as a biomarker associated with severity of chronic obstructive lung disease. Tuberc Respir Dis. 2017;80(3):304–310. doi:10.4046/trd.2017.80.3.304
17. Yao C, Liu X, Tang Z. Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2285–2290. doi:10.2147/copd.S141760
18. Zinellu A, Zinellu E, Mangoni AA, et al. Clinical significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute exacerbations of COPD: present and future. Eur Respir Rev. 2022;31(166):220095. doi:10.1183/16000617.0095-2022
19. Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. doi:10.1371/journal.pone.0156511
20. Lee JY, Chon GR, Rhee CK, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical center in Korea: the Korea COPD Subgroup Study Team Cohort. J Korean Med Sci. 2016;31(4):553–560. doi:10.3346/jkms.2016.31.4.553
21. Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. doi:10.1183/09031936.05.00035005
22. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
23. Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017;49(1). doi:10.1183/13993003.00016-2016
24. Park JO, Choi IS, Park KO. Normal predicted values of single-breath diffusing capacity of the lung in healthy nonsmoking adults. Korean J Intern Med. 1986;1(2):178–184. doi:10.3904/kjim.1986.1.2.178
25. Choi JK, Paek D, Lee JO. Normal Predictive Values of Spirometry in Korean Population. Tuberc Respir Dis. 2005;58(3):230–242. doi:10.4046/trd.2005.58.3.230
26. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi:10.1164/ajrccm.166.1.at1102
27. Yang H, Wen X, Wu F, et al. Inter-relationships among neutrophilic inflammation, air trapping and future exacerbation in COPD: an analysis of ECOPD study. BMJ Open Respir Res. 2023;10(1). doi:10.1136/bmjresp-2022-001597
28. Paliogiannis P, Fois AG, Sotgia S, et al. Neutrophil to lymphocyte ratio and clinical outcomes in COPD: recent evidence and future perspectives. Eur Respir Rev. 2018;27(147). doi:10.1183/16000617.0113-2017
29. Day K, Ostridge K, Conway J, et al. Interrelationships among small airways dysfunction, neutrophilic inflammation, and exacerbation frequency in COPD. Chest. 2021;159(4):1391–1399. doi:10.1016/j.chest.2020.11.018
30. Pandey KC, De S, Mishra PK. Role of proteases in chronic obstructive pulmonary disease. Front Pharmacol. 2017;8:512. doi:10.3389/fphar.2017.00512
31. Barnes PJ. Oxidative stress in chronic obstructive pulmonary disease. Antioxidants. 2022;11(5). doi:10.3390/antiox11050965
32. Wang Y, Xu J, Meng Y, Adcock IM, Yao X. Role of inflammatory cells in airway remodeling in COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:3341–3348. doi:10.2147/copd.S176122
33. Papakonstantinou E, Karakiulakis G, Batzios S, et al. Acute exacerbations of COPD are associated with significant activation of matrix metalloproteinase 9 irrespectively of airway obstruction, emphysema and infection. Respir Res. 2015;16(1):78. doi:10.1186/s12931-015-0240-4
34. Singh D. Small airway disease in patients with chronic obstructive pulmonary disease. Tuberc Respir Dis. 2017;80(4):317–324. doi:10.4046/trd.2017.0080
35. Bélanger M, Couillard S, Courteau J, et al. Eosinophil counts in first COPD hospitalizations: a comparison of health service utilization. Int J Chron Obstruct Pulmon Dis. 2018;13:3045–3054. doi:10.2147/copd.S170743
36. Cui Y, Zhan Z, Zeng Z, et al. Blood eosinophils and clinical outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease: a propensity score matching analysis of real-world data in China. Front Med. 2021;8:653777. doi:10.3389/fmed.2021.653777
37. Singh D, Wedzicha JA, Siddiqui S, et al. Blood eosinophils as a biomarker of future COPD exacerbation risk: pooled data from 11 clinical trials. Respir Res. 2020;21(1):240. doi:10.1186/s12931-020-01482-1
38. Kerkhof M, Sonnappa S, Postma DS, et al. Blood eosinophil count and exacerbation risk in patients with COPD. Eur Respir J. 2017;50(1):1700761. doi:10.1183/13993003.00761-2017
39. Chan MC, Yeung YC, Yu ELM, Yu WC. Blood eosinophil and risk of exacerbation in chronic obstructive pulmonary disease patients: a retrospective cohort analysis. Int J Chron Obstruct Pulmon Dis. 2020;15:2869–2877. doi:10.2147/copd.S268018
40. Juthong S, Kaenmuang P. Association between blood eosinophils with exacerbation and patient-reported outcomes in chronic obstructive pulmonary disease patients in an endemic area for parasitic infections: a prospective study. J Thorac Dis. 2020;12(9):4868–4876. doi:10.21037/jtd-19-4101
41. David B, Bafadhel M, Koenderman L, De Soyza A. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax. 2021;76(2):188–195. doi:10.1136/thoraxjnl-2020-215167
42. Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44(6):1697–1700. doi:10.1183/09031936.00162414
43. Mallah H, Ball S, Sekhon J, Parmar K, Nugent K. Platelets in chronic obstructive pulmonary disease: an update on pathophysiology and implications for antiplatelet therapy. Respir Med. 2020;171:106098. doi:10.1016/j.rmed.2020.106098
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


