Back to Journals » Journal of Pain Research » Volume 16
Predictive Factors Associated with Chronic Neck Pain in Patients with Cervical Degenerative Disease: A Retrospective Cohort Study
Authors Kang X , Qian M, Liu M, Xu H, Xu B
Received 18 July 2023
Accepted for publication 27 November 2023
Published 11 December 2023 Volume 2023:16 Pages 4229—4239
DOI https://doi.org/10.2147/JPR.S423144
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Alaa Abd-Elsayed
Xinjian Kang,1,2 Man Qian,3 Mingli Liu,2 Haiwei Xu,4 Baoshan Xu4
1Department of Orthopedics, Traditional Chinese Medicine Hospital of Qinhuangdao, Qinhuangdao, Hebei, People’s Republic of China; 2Tianjin Medical University, Graduate School, Tianjin, People’s Republic of China; 3Department of Refractive Surgery, Qinhuangdao Aier Ophthalmic Hospital, Qinhuangdao, Hebei, People’s Republic of China; 4Department of Minimally Invasive Spine Surgery, Tianjin Hospital, Tianjin, People’s Republic of China
Correspondence: Baoshan Xu, Department of Minimally Invasive Spine Surgery, Tianjin Hospital, No. 406 Jiefangnan Road, Hexi District, Tianjin, People’s Republic of China, Tel +86 13502028198, Fax +86- 22 -28241184, Email [email protected]
Purpose: To explore the predictive factors of neck pain (NP) in patients with cervical degenerative disease by retrospectively analyzing their occupational and demographic characteristics and to provide a valuable reference for preventing and treating chronic NP.
Patients and Methods: We retrospectively reviewed the occupational and demographic data of patients with cervical degenerative disease who had undergone anterior cervical surgery between June 2021 and December 2022 at our center. The patients were divided into NP and no-NP groups based on whether they had chronic NP before surgery. Relevant occupational and demographic data from all patients were statistically analyzed, and all variables were made categorical. Forward stepwise logistic regression models were constructed for preoperative chronic neck pain to explore the possible risk factors associated with chronic neck pain.
Results: The differences in smoking, being an office worker, BMI, and disease types between NP and no-NP groups were statistically significant. In contrast, there were no statistically significant in age, sex, academic level, duration, and degeneration grade between the two groups. Moreover, further logistic regression analysis indicated that smoking, being an office worker, having an abnormal BMI, and cervical spondylotic radiculopathy (CSR) were related to chronic neck pain.
Conclusion: The present study indicated that smoking, being an office worker, having an abnormal BMI, and CSR were predisposing risk factors for NP associated with cervical degenerative disease. Although intervertebral disc degeneration is the pathology basis of NP, the degeneration grade was not related to the occurrence of NP in our current study. Therefore, quitting smoking, avoiding sedentariness, and maintaining a normal BMI may prevent NP to some extent.
Keywords: discogenic pain, radiating pain, musculoskeletal disorder, intervertebral disc degeneration
Introduction
Neck pain (NP), similar to low back pain, is a common musculoskeletal disorder and the leading cause of disability worldwide, accounting for one of the top five chronic pain conditions.1 According to reports in the literature, its mean point, annual, and lifetime prevalence rates are 7.6%, 37.2%, and 48.5%, respectively.2 However, the exact pathogenesis is poorly understood. Various cervical disorders may cause it, such as neck muscle tension or strain, minor arthropathy, trauma, cervical disc herniation, abnormal spine curvature, and cervical degenerative disease.3
As an important component of the physiological structure of the cervical spine, the cervical intervertebral disc has been established as a main source of NP.4,5 NP originating from cervical intervertebral disc can be divided into two types:6 radiating and discogenic pain. Radiating pain is typically caused by spinal stenosis or cervical spondylotic radiculopathy. In contrast, discogenic pain results from internal intervertebral disc disorders alone, without disc herniation and cervical spondylosis. The concomitant symptoms of discogenic neck pain include neck stiffness, headache, unilateral or bilateral shoulder pain, non-radicular upper arm pain, ocular and vestibular dysfunction, and anterior chest wall pain.1 Although the exact etiology of the two types of NP may differ, degenerative changes in the intervertebral disc are a common pathological basis for both, with a reported incidence of 16–41%.2,7
Intervertebral disc degeneration (IVDD) results from multiple factors.8 Predisposing risk factors include aging, sex, genes, mechanical injury, smoking, nutrition, and environmental factors.9–11
Aging is one of the factors most closely related to IVDD. The cellular composition and microenvironment within the disc are altered with aging, such as a decline in the concentration of cells and proteoglycans in the nucleus, a decrease in the synthesis rate, and a diminished concentration of chondroitin sulfate.12,13 The degeneration will occur when the matrix is abnormal.
Genetic factors are important in determining the individual risk of developing disc degeneration and some specific types of diseases, which have been identified by a series of studies in twins. As a form of genetic inheritance, sex causes a different susceptibility to some specific diseases due to differences in genetic information. Women, particularly women with obesity, are more susceptible to IVDD and spinal diseases.14
As an important structure in the spine that transmits stress and connects adjacent vertebral bodies, the intervertebral disc is extremely sensitive to mechanical influences, and possible risk factors include sitting with prolonged neck flexion or with a protruded head posture, frequent flexion, sudden unexpected movements, and trauma. Sports-related spine injuries may also predispose individuals to IVDD.15 Therefore, some occupations and special movements that increase the spinal load can accelerate IVDD and result in chronic discogenic pain.16
As the largest blood-free supply tissue in the human body, it is important to maintain sufficient nutrient supply and metabolic balance for the intervertebral disc to keep its normal physiological function. Obesity, as a prevalent condition in both developed and developing countries, is the combined result of genetic and environmental factors. It indicates a metabolic disorders and is recognized as a systemic inflammatory state mediated by adipokines, which has been proved as a predisposing risk factor for IVDD.17
Moreover, smoking is another cause for IVDD and chronic spinal pain. The possible mechanism may be the excessive activation of mast cells (MCs) and subsequent protease release, which are key in smoking-associated diseases.18–21
IVDD is the pathological basis of NP, whether the factors associated with disc degeneration may also lead to the occurrence of NP. Even though the theory states so, it can often be found that many degenerated discs are asymptomatic in clinical practice. In contrast, several mild degenerative discs may lead to severe symptoms. Thus, the occurrence of NP is a very complex pathological process. Therefore, this study aimed to explore the predictive factors of NP in patients with cervical degenerative disease by retrospectively analyzing their occupational and demographic characteristics and to provide a valuable reference for preventing and treating chronic NP.
Materials and Methods
Patients
This study retrospectively reviewed the data of patients with cervical degenerative disease who had undergone anterior cervical surgery between June 2021 and December 2022 at our center for any of the following reasons: 1) not responding to appropriate conservative therapies; 2) having persistent radicular pain, progressive neurologic deficits, or motor weakness; or 3) showing signs of cord compression. Three types of diseases were included, namely, cervical spondylotic radiculopathy (CSR), cervical spondylotic myelopathy (CSM), and discogenic neck pain (DNP). The recruited patients with DNP had to undergo anterior cervical surgery as an alternative treatment for suffering refractory pain that failed to respond to conservative treatment.
The surgical procedures were either anterior cervical discectomy and fusion (ACDF) or anterior cervical corpectomy decompression and fusion (ACCF). The patients were divided into NP and no-NP groups based on the presence or absence of chronic NP before surgery.
Inclusion Criteria
The inclusion criteria were the presence of severe chronic NP before surgery (Visual Analog Scale [VAS] ≥70 mm) for the NP group and the absence of NP or only mild NP before surgery (VAS ≤30 mm) for the no-NP group.15
The exclusion criteria for both the NP and no-NP groups were: 1) mental disorders; 2) a history of cervical tuberculosis, infections, tumors, acute trauma, or any demonstrable congenital or developmental abnormalities of the cervical spine; and 3) incomplete medical data.
To guarantee an excellent surgical effect, the diagnosis of discogenic NP was determined by a positive response to an analgesic discography test.22 The details are as follows: the patient was placed in the supine position, a 22-G spinal needle was percutaneously punctured into the center of the disc via an anterolateral approach, guided by a C-armed X-wire machine, as judged from anteroposterior and lateral views. A small volume (0.3–0.5 mL) of 0.25% bupivacaine was injected. If there was no complaint of discomfort after lying supine for two hours, the patient was allowed to get up and move around without limiting cervical spine movement. Pain relief of ≥70% was regarded as positive. During the analgesic discography test, no contrast medium was used. If two discs were suspected to be affected, the second disc was tested after any effects on the first disc had ceased.
Relief percent was calculated using the following equation:
Parameter Evaluation
During the study, two experienced radiologists and two senior spine surgeons were invited to evaluate the degree of degeneration of the target discs on the preoperative magnetic resonance imaging (MRI; 3.0-T Siemens Magnetom Symphony; Siemens, Berlin, Germany). They evaluated using T2-weighted (T2W) sagittal MRI according to the Miyazaki disc degeneration grading system,23 as shown in Table 1. A detailed record was made, and the procedure was performed under double-blind conditions. The MRI scan (T2W1, repetition time: 2000 ms, and echo time: 90 ms) layer was 4 mm thick and 1 mm apart, and the matrix was 320×192. The scoring method was according to the Miyazaki intervertebral disc degeneration (IVDD) grading system (grades I–V; the higher the grade, the more severe the IVDD). The scores corresponded to the degree of IVDD. For example, grade 3 corresponded to 3 points and grade 4 to 4 points. The average of four scores determined by the two radiologists and two spine surgeons was regarded as the final score of disc degradation.
 |
Table 1 Miyazaki’s Grading System for Cervical Intervertebral Disc Degeneration |
The present study identified smokers based on the definition of smokers by Wu et al24 combined with the characteristics of smoking in China.25 The following inclusion criteria were applied: ≥20 cigarettes smoked daily and a smoking history of ≥5 years. In addition, we collected and statistically analyzed the data on the education level of all participants. The patients with a university education were considered to have a high level of education; otherwise, they were considered to have a low level of education.
Written informed consent was obtained from each patient before the study, and the study protocol was approved by the Ethics Committee of our Hospital (202303F). The study was conducted in accordance with relevant guidelines and regulations of the Declaration of Helsinki.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics (version 25.0; IBM Corp., Armonk, NY, USA). The differences in age, sex, education level, smoking, being an office worker, duration, Body Mass Index (BMI), and disease types between the two groups were tested using Pearson’s chi-squared test. The difference in degeneration grade between the two groups was tested using Rank-sum test. Statistical significance was set at P≤0.05, detailed in Table 2. Moreover, all variables were made categorical and assigned (as shown in Table 3), and forward stepwise logistic regression models were constructed for preoperative severe chronic NP.26 We used the presence or absence of severe neck pain before surgery as a dependent variable, and univariate logistic regression analysis was used to study the related factors, such as age, sex, education level, smoking, being an office worker, duration, BMI, degeneration grade, and disease type, as shown in Table 4. Subsequently, the variables were assessed as significant (P≤0.05) in univariate regression analysis were entered as independent variables in multivariate logistic regression analysis (as shown in Table 5), thereby establishing the regression model. For the independent variables, the lowest value in the Table 3 was taken as the reference group.
 |
Table 2 All Enumeration Data and Measurement Data of Participants in the Two Groups |
 |
Table 3 Variable Assignment Table |
 |
Table 4 Risk Factors Related to Chronic Neck Pain in 189 Patients: Univariate Logistic Regression Analysis |
 |
Table 5 Risk Factors Related to Chronic Neck Pain in 189 Patients: Multivariate Logistic Regression Analysis |
Results
Patients’ Occupational and Demographic Data
A total of 247 patients with cervical degenerative disease underwent anterior cervical surgery during this period. According to the inclusion criteria, 86 and 103 patients were recruited in the NP and no-NP groups, respectively. In addition, there were 55, 18, and 13 patients with cervical spondylotic radiculopathy, cervical spondylotic myelopathy, and discogenic pain in the NP group, respectively. In the no-NP group, 35 and 68 patients had cervical spondylotic radiculopathy and cervical spondylotic myelopathy, respectively. The NP group included 45 males and 41 females with a mean age of 64.7 (37–82) years. The mean duration was 13.6 (3–29) months. The involved segments in the NP group ranged from C3/4 to C6/7. The no-NP group included 57 males and 46 females, with a mean age of 61.2 (31–79) years. The mean duration was 11.4 (1–21) months. Similar to the NP group, the involved segments in the no-NP group ranged from C3/4 to C6/7.
The present study involved 128 and 175 intervertebral segments in the NP and no-NP groups, respectively. Detailed data of all the participants were collected by questionnaires and medical records.
Table 2 presents the comparison of all the enumeration and measurement data of participants in the NP and no-NP groups. Significant differences were observed between the smoking, being an office worker, having an abnormal BMI, and disease types in the two groups (Pearson’s chi-square test, P<0.001, =0.004, 0.002, and <0.001, respectively). However, there were no significant differences in age, sex, education level, and duration between the two groups (Pearson’s chi-square test, P=0.108, 0.679, 0.943, and 0.127 respectively). In addition, the difference in the degeneration grade between the NP group and the no-NP group was not statistically significant (Rank-sum test, P=0.104).
Furthermore, the original data from all the participants in both groups were analyzed using Origin Pro 2023 (The Ultimate Software for Graphing & Analysis, Origin Lab Corporation). The proportions of smoking, office workers, and abnormal BMI in the NP group were higher than those in the no-NP group, with statistically significant differences, the results are shown in Figure 1.
 |
Figure 1 Comparison of smoking, office workers, and abnormal BMI in the neck pain (NP) and no-NP groups. (A) = NP group, (B) = no-NP group; **P<0.01; ***P<0.001. |
Univariate Logistic Regression Analysis
A total of 189 training samples were performed analysis using univariate logistic regression analysis.
According to the specific content of the questionnaire and medical records, 9 variables that may related to the occurrence of NP were selected to conduct statistical analysis. They were age, sex, education level, smoking, being an office worker, duration, BMI, degeneration grade, and disease types. The statistical data are outlined in Table 4, that shows that the risk of smokers suffering from NP is 3.049 (1.672–5.559) times more than that of non-smokers. The risk for office workers is 2.341 (1.300–4.218) times more than that for non-office workers. The risk of suffering from NP in patients with abnormal BMI is 2.533 (1.400–4.583) times more than whose with normal BMI. And the risk for patients with CSM is 0.168 (0.086–0.329) times more than that for patients with CSR, in other words, the risk of suffering from NP in patients with CSR is more than 5 times than that of patients with CSM.
Multivariate Logistic Regression Analysis
Among all the 9 variables, 4 variables which show significant in the univariate logistic regression analysis were chosen as independent variable included in the multivariate logistic regression analysis and entered logistic regression equation. According to the results of analysis, it can be found that the maximum contribution for NP was BMI, followed by smoking and being an office worker, excepting CSR (Table 5). A p-value closer to 1 was considered to be more likely to occur in preoperative chronic neck pain; the less likely, the p-value was closer to 0.
Evaluation of the Predictive Model
The Chi-square value of Hosmer-Lemeshow test is 11.689, P=0.166 (P> 0.05), indicating that the model fit in Table 5 is good. The ROC curves (Figure 2) also indicate that.
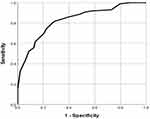 |
Figure 2 The ROC curves corresponding to the multivariate logistic regression analysis. The area under the curve is 0.829, 95% CI: (0.771–0.888), p=0.030. |
Discussion
Chronic neck pain, similar to low back pain, has become a severe public health problem worldwide.27,28 It is reported that various factors are related to the occurrence of neck pain. The current study also indicated that smoking, being an office worker, and having an abnormal BMI and CSR are predisposing risk factors related to neck pain. Although there is limited understanding of its pathogenesis, it is reported that a degenerative disc is a common source of neck pain with a reported prevalence between 16% to 41%.16 Therefore, the predisposing risk factors related to neck pain may work by resulting in IVDD.
Abnormal BMI as a manifestation of nutritional metabolic dysfunction, either obesity or marasmus, is not conducive for intervertebral disc to maintaining the normal physiological function. Obesity is an abnormal or excessive fat accumulation that presents a health risk,29 and obesity-related risk factors may cause changes in the disc microenvironment, enhancing cell apoptosis, autophagy, and matrix breakdown.18 The negative effects of obesity contain two aspects:1) Metabolic disturbance. Obese patients are susceptible to hyperlipidemia, which is the primary cause of atherosclerosis and artery occlusion.17 The intervertebral disc, the largest non-vascular tissue in the human body with insufficient blood supply, is sensitive to ischemia. Previous studies have reported that insufficient blood supply may lead to IVDD, and atherosclerosis could be a possible reason for the lack of blood supply.30–32 2) Mechanical overload. Although an increased BMI does not necessarily meet the diagnostic criteria for obesity (BMI ≥25 kg/m2, according to the Asian criteria (WHO Expert Consultation, 2004)), people with an increased BMI tend to be overweight and bring excessive spinal load which may accelerate the process of IVDD. What is more, marasmus also has adverse health effects, especially for spine stability. For emaciated people, the muscles and ligaments are less developed, and fail to provide enough tension to maintain the stability of the spine during flexion and extension activities, resulting in abnormal motion between the neighbor vertebral bodies, which may lead to disc degeneration. In the current study, the proportion of patients with abnormal BMI in the NP group was higher than that in the no-NP group, and the difference was statistically significant. In addition, the results of the logistic regression analysis showed abnormal BMI is related to NP, the partial regression coefficient is 0.957. Therefore, abnormal BMI might be a risk factor for chronic neck pain.
Smoking, as a global problem, is an established risk factor for human health. A series of related studies have indicated the negative effects of smoking on spinal diseases. Livshits et al33 reported that the chance of undergoing cervical spine surgery was greater in the smoking population compared to that in the non-smoking population (64.3% vs 37%, P<0.01). Battié et al10 studied IVDD in 20 male monozygotic twins and found that smokers had a higher average disc degeneration score (>18%) than nonsmokers. Wahlstrom et al34 reported that smokers with spinal degeneration had a longer average length of hospital stay than nonsmokers. Kim et al35 retrospectively analyzed that the improvement of neurological function in nonsmokers was better than that in smokers after ACDF. Moreover, studies on the relationship between smoking and IVDD have proven that they are closely related, and smoking has been identified as a risk factor for IVDD and discogenic pain.36,37 This is consistent with the results of the current study. In this study, the proportion of smokers in the NP group was statistically higher than that in the no-NP group, and further logistic regression analysis showed that smoking is related to NP, with the partial regression coefficient being 0.895. Therefore, smoking might be a risk factor for chronic neck pain.
Office workers or sedentary individuals are more prone to neck and low back pain.38–40 The prolonged sitting time and specific body postures, such as inappropriate neck or low back flexion or rotation,41 may increase the mechanical burden of the intervertebral disc, leading to mechanical damage. Moreover, workplace environmental factors such as temperature, humidity, and location of the computer monitor may be associated with IVDD and NP.42 In this study, we also drawn similar conclusion. The proportion of office workers in the NP group was significantly higher than that in the no-NP group, and further logistic regression analysis showed that being an office worker is related to NP, with a partial regression coefficient of 0.724.Hence, placing computer monitors directly in front of the users and maintaining an indoor temperature between 24–26 °C are recommended to reduce the incidence of NP by avoiding excessive flexion and relieving muscle tension of cervical spine.43–46
Cervical spondylosis is a common and frequently occurring disease in clinical practice. Among all the subtypes of cervical spondylosis, 40% of patients with CSM and about 26% of patients with CSR have to undergo surgical treatment due to severe neurological dysfunction and refractory symptoms.47,48 CSR usually combines with radiating neck pain due to the compression of cervical nerve roots.49 CSM represents the most common spinal cord disorder in adults and often develops progressive neurologic deficits and motor weakness, while concurrent neck and shoulder pain is relatively rare.50 This is consistent with the results of our current study. The univariate logistic regression analysis in the present study showed the risk of suffering from NP in patients with CSR is more than 5 times than of patients with CSM, and further multivariate logistic regression analysis showed that CSR is related to NP. Moreover, the prognosis for most patients with CSR is favorable.51 However, the effect of conservative interventions for most CSM is limited.52,53 Accordingly, surgical treatments are more likely to be selected for patients with CSM. These may be the possible reasons for the distributional difference of cervical disease types between the two groups in the current study; the proportion of CSR was significantly higher than CSM in the NP group, while the no-NP group had the opposite result.
Aging and Sex Aging has been seen as one of the most closely related factors of disc degeneration. It is reported that the incidence of disc degeneration among adults <30 years old is about 40%, and the incidence of disc degeneration in people >50 years old is >90%.54 The intervertebral disc is one of the earliest organs to degenerate with aging. The characteristic changes of IVDD present as different cellular and biochemical alterations, including degradation of the extracellular matrix, accumulation of cellular waste products, and increased expression of proinflammatory cytokines. These changes, particularly inflammatory reactions, are closely associated with chronic neck and low back pain.5,15,55 In this study, the average age of participants in the NP group was older than that in the no-NP group, but the difference was not statistically significant, and further logistic regression analysis did not show that age is related to NP. Additionally, because of the differences in genetic and physiological factors, being a female, particularly a female with obesity, increases the susceptibility to IVDD.14,17 Previous studies have reported that females have a higher prevalence of neck or low back pain, and are more susceptible to environmental risk factors than males due to less physical activity, lower bone mineral density, and their specific anatomical structure.56–58 However, the results of the present study did not show the association between sex and NP either. The possible reasons are as follows: 1) the sample size in this study was small, and the distribution of variables is narrow; 2) variables may not be normally distributed, which may bias the results at some extent.
Although IVDD is the primary cause of chronic neck and low back pain, this study did not show degeneration grade of intervertebral disc is related to NP. Dwyer et al59 reported that a greater degree of degeneration does not necessarily implicate a more severe discogenic pain. This is why many patients have significant disc degeneration but not any clinical symptoms. One of the previous studies from the first author also found no positive linear correlation between the degree of disc degeneration and NP. However, the conclusion was drawn from a cross-sectional cohort study, and the study’s method and limited sample size might have biased the results.
A series of studies have explored the possible risk factors related to chronic NP. However, most of them did not classify NP according to its source. Therefore, the conclusions drawn were not targeted. In the present study, patients with cervical degenerative diseases who underwent anterior cervical surgery were recruited and divided into NP and no-NP groups based on whether they suffered preoperative NP or not. Therefore, NP discussed in the current study was closely associated with degenerative cervical discs, including radiating and discogenic pain. According to the results of logistic regression analysis, abnormal BMI, smoking, being an office worker, and CSR were possible risk factors associated with chronic NP, while age, sex, duration, education level, and degeneration grade were not related. However, due to the complexity of the etiology for IVDD and chronic NP, studies with larger sample size and multi-center are also needed for in-depth studies.
Limitations
This study had several limitations. First, this was a retrospective cohort study, if it was a prospective randomized controlled study, the evidence level would be higher and more meaningful. Second, the sample size is small. A larger sample size and multi-center studies may be more convincing. In addition, the number of variables included in this study was limited. Some possible risk factors of NP, such as cervical curvature and Modic changes, were not included in the present research.
Conclusions
According to the results of the logistic regression analysis, having an abnormal BMI, smoking, being an office worker, and CSR are predisposing risk factors associated with chronic NP, while age, sex, duration, education level, and degeneration grade were not related to NP in the present study.
Abbreviations
ACCF, anterior cervical corpectomy decompression and fusion; ACDF, anterior cervical discectomy and fusion; BMI, body mass index; CSM, cervical spondylotic myelopathy; CSR, cervical spondylotic radiculopathy; IVDD, intervertebral disc degeneration; MRI, magnetic resonance imaging; NP, neck pain; T2W, T2-weighted; VAS, Visual Analog Scale.
Data Sharing Statement
The data used to support the findings of this study are included within the article.
Acknowledgments
The authors would like to thank Yongchao Li, Yongjin Li, and Yufei Yuan for their help in the preparation and submission of the manuscript. The authors would also like to thank Editage for English language editing.
Funding
This research received no external funding.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this article.
References
1. Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221.
2. Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.
3. Manchikanti L, Boswell MV, Singh V, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12(4):699–802.
4. Fujimoto K, Miyagi M, Ishikawa T, et al. Sensory and autonomic innervation of the cervical intervertebral disc in rats: the pathomechanics of chronic discogenic neck pain. Spine. 2012;37(16):1357–1362.
5. Yang L, Yang C, Pang X, et al. Mechanoreceptors in Diseased Cervical Intervertebral Disc and Vertigo. Spine. 2017;42(8):540–546.
6. Lotz JC, Ulrich JA. Innervation, inflammation, and hypermobility may characterize pathologic disc degeneration: review of animal model data. J Bone Joint Surg Am. 2006;88(Suppl 2):76–82.
7. Nilsen TI, Holtermann A, Mork PJ. Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: longitudinal data from the Nord-Trondelag Health Study. Am J Epidemiol. 2011;174(3):267–273.
8. Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine. 2006;31(18):2151–2161.
9. Cinotti G, Della Rocca C, Romeo S, Vittur F, Toffanin R, Trasimeni G. Degenerative changes of porcine intervertebral disc induced by vertebral endplate injuries. Spine. 2005;30(2):174–180.
10. Battié MC, Videman T. Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am. 2006;88 Suppl 2(Suppl 2):3–9. doi:10.2106/JBJS.E.01313
11. Yuan H-Y, Tang Y, Liang Y-X, et al. Matrix metalloproteinase-3 and vitamin d receptor genetic polymorphisms, and their interactions with occupational exposure in lumbar disc degeneration. J Occup Health. 2010;52(1):23–30. doi:10.1539/joh.L8149
12. Hadjipavlou AG, Tzermiadianos MN, Bogduk N, Zindrick MR. The pathophysiology of disc degeneration: a critical review. J Bone Joint Surg Br. 2008;90–B(10):1261–1270. doi:10.1302/0301-620X.90B10.20910
13. Burke JG, Watson RW, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br. 2002;84-B(2):196–201. doi:10.1302/0301-620X.84B2.0840196
14. Chen -H-H, Hsu H-T, Liao M-H, Teng M-S. Effects of Sex and Obesity on LEP Variant and Leptin Level Associations in Intervertebral Disc Degeneration. Int J Mol Sci. 2022;23(20):12275. doi:10.3390/ijms232012275
15. Wu B, Yang L, Peng B. Ingrowth of Nociceptive Receptors into Diseased Cervical Intervertebral Disc Is Associated with Discogenic Neck Pain. Pain Med. 2019;20(6):1072–1077. doi:10.1093/pm/pnz013
16. Peng B, DePalma MJ. Cervical disc degeneration and neck pain. J Pain Res. 2018;11:2853–2857. doi:10.2147/JPR.S180018
17. Sharma A. The role of adipokines in intervertebral disc degeneration. Med Sci. 2018;6(2):34.
18. Prieto-García A, Zheng D, Adachi R, et al. Mast cell restricted mouse and human tryptase·heparin complexes hinder thrombin-induced coagulation of plasma and the generation of fibrin by proteolytically destroying fibrinogen. J Biol Chem. 2012;287(11):7834–7844.
19. Liu G, Jarnicki AG, Paudel KR, et al. Adverse roles of mast cell chymase-1 in COPD. Eur Respir J. 2022;60(6):2101431.
20. Tiotiu A, Badi Y, Kermani NZ, et al. Association of Differential Mast Cell Activation with Granulocytic Inflammation in Severe Asthma. Am J Respir Crit Care Med. 2022;205(4):397–411.
21. Schanin J, Gebremeskel S, Korver W, et al. A monoclonal antibody to Siglec-8 suppresses non-allergic airway inflammation and inhibits IgE-independent mast cell activation. Mucosal Immunol. 2021;14(2):366–376.
22. Roth DA. Cervical analgesic discography. A new test for the definitive diagnosis of the painful-disk syndrome. JAMA. 1976;235(16):1713–1714.
23. Miyazaki M, Hong SW, Yoon SH, et al. Kinematic analysis of the relationship between the grade of disc degeneration and motion unit of the cervical spine [published correction appears in Spine. 2008 Apr 1;33(7):830]. Spine. 2008;33(2):187–193.
24. Wu HL, Ding WY, Shen Y, et al. Prevalence of vertebral endplate modic changes in degenerative lumbar scoliosis and its associated factors analysis. Spine. 2012;37(23):1958–1964.
25. Oda H, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y, Iwahashi M. Degeneration of intervertebral discs due to smoking: experimental assessment in a rat-smoking model. J Orthop Sci. 2004;9(2):135–141.
26. Anderson RP, Jin R, Grunkemeier GL. Understanding logistic regression analysis in clinical reports: an introduction. Ann Thorac Surg. 2003;75(3):753–757.
27. Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848.
28. Onyewu O, Manchikanti L, Falco FJ, et al. An update of the appraisal of the accuracy and utility of cervical discography in chronic neck pain. Pain Physician. 2012;15(6):E777.
29. Cannata F, Vadalà G, Ambrosio L, et al. Intervertebral disc degeneration: a focus on obesity and type 2 diabetes. Diabetes Metab Res Rev. 2020;36(1): e3224.
30. Altun I, Yuksel KZ. An experimental study on the effects of smoking in the perinatal period and during lactation on the intervertebral disks of newborns. World Neurosurg. 2017;99:1–5.
31. Benneker LM, Heini PF, Alini M, Anderson SE, Ito K. 2004 Young Investigator Award Winner: vertebral endplate marrow contact channel occlusions and intervertebral disc degeneration. Spine. 2005;30(2):167–173.
32. Kauppila LI, Tallroth K. Postmortem angiographic findings for arteries supplying the lumbar spine: their relationship to low-back symptoms. J Spinal Disord. 1993;6(2):124–129.
33. Livshits G, Cohen Z, Higla O, Yakovenko K. Familial history, age and smoking are important risk factors for disc degeneration disease in Arabic pedigrees. Eur J Epidemiol. 2001;17(7):643–651.
34. Wahlström J, Burström L, Nilsson T, Järvholm B. Risk factors for hospitalization due to lumbar disc disease. Spine. 2012;37(15):1334–1339.
35. Kim TH, Ha Y, Shin JJ, Cho YE, Lee JH, Cho WH. Signal intensity ratio on magnetic resonance imaging as a prognostic factor in patients with cervical compressive myelopathy. Medicine. 2016;95(39):e4649.
36. Ferreira PH, Beckenkamp P, Maher CG, Hopper JL, Ferreira ML. Nature or nurture in low back pain? Results of a systematic review of studies based on twin samples. Eur J Pain. 2013;17(7):957–971.
37. Goldberg MS, Scott SC, Mayo NE. A review of the association between cigarette smoking and the development of nonspecific back pain and related outcomes. Spine. 2000;25(8):995–1014.
38. Chiu TT, Lam PK. The prevalence of and risk factors for neck pain and upper limb pain among secondary school teachers in Hong Kong. J Occup Rehabil. 2007;17(1):19–32.
39. De Loose V, Burnotte F, Cagnie B, Stevens V, Van Tiggelen D. Prevalence and risk factors of neck pain in military office workers. Mil Med. 2008;173(5):474–479.
40. Erick PN, Smith DR. Low back pain among school teachers in Botswana, prevalence and risk factors. BMC Musculoskelet Disord. 2014;15:359.
41. Yue P, Liu F, Li L. Neck/shoulder pain and low back pain among school teachers in China, prevalence and risk factors. BMC Public Health. 2012;12:789.
42. Ye S, Jing Q, Wei C, Lu J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: a cross-sectional study. BMJ Open. 2017;7(4):e014914.
43. Pienimäki T, Karppinen J, Rintamäki H, et al. Prevalence of cold-related musculoskeletal pain according to self-reported threshold temperature among the Finnish adult population. Eur J Pain. 2014;18(2):288–298.
44. Burström L, Järvholm B, Nilsson T, Wahlström J. Back and neck pain due to working in a cold environment: a cross-sectional study of male construction workers. Int Arch Occup Environ Health. 2013;86(7):809–813.
45. Dovrat E, Katz-Leurer M. Cold exposure and low back pain in store workers in Israel. Am J Ind Med. 2007;50(8):626–631.
46. Fernandes ES, Russell FA, Alawi KM, et al. Environmental cold exposure increases blood flow and affects pain sensitivity in the knee joints of CFA-induced arthritic mice in a TRPA1-dependent manner. Arthritis Res Ther. 2016;18:7.
47. Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine. 2013;38(22 Suppl 1):S21–S36.
48. Lees F, Turner JW. Natural history and prognosis of cervical spondylosis. Br Med J. 1963;2(5373):1607–1610.
49. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015;28:E251–E259.
50. Iyer A, Azad TD, Tharin S. Cervical spondylotic myelopathy. Clin Spine Surg. 2016;29(10):408–414.
51. Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325–335.
52. Gok B, Sciubba DM, McLoughlin GS, et al. Surgical treatment of cervical spondylotic myelopathy with anterior compression: a review of 67 cases. J Neurosurg Spine. 2008;9(2):152–157.
53. Sampath P, Bendebba M, Davis JD, Ducker TB. Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine. 2000;25(6):670–676.
54. Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34(9):934–940.
55. Urban JP, Smith S, Fairbank JC. Nutrition of the intervertebral disc. Spine. 2004;29(23):2700–2709.
56. Briggs AM, Straker LM, Burnett AF, Wark JD. Chronic low back pain is associated with reduced vertebral bone mineral measures in community-dwelling adults. BMC Musculoskelet Disord. 2012;13:49.
57. Hiz O, Ediz L, Ercan S, Arslan M, Avcu S, Tekeoglu I. The relationship between chronic low back pain and bone mineral density in young and middle-aged males. Turk J Phys Med. 2012;58(4). doi:10.4274/tftr.37267
58. Muntner P, Gu D, Wildman RP, et al. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health. 2005;95(9):1631–1636.
59. Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine. 1990;15(6):453–457.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

