Back to Journals » Nature and Science of Sleep » Volume 14
Prediction of Mandibular Advancement Device Response Using CPAP Pressure in Different Polysomnographic Phenotypes
Authors Lee CF, Chen YJ, Huang WC, Hou JW, Liu YT, Shih TTF , Lee PL , Yu CJ
Received 30 November 2021
Accepted for publication 13 March 2022
Published 25 March 2022 Volume 2022:14 Pages 517—529
DOI https://doi.org/10.2147/NSS.S351027
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Video abstract presented by Chien-Feng Lee.
Views: 301
Chien-Feng Lee,1,* Yunn-Jy Chen,2,* Wen-Chi Huang,3 Jen-Wen Hou,4 Yu-Ting Liu,5 Tiffany Ting-Fang Shih,6 Pei-Lin Lee,7– 10 Chong-Jen Yu1,8,9
1Department of Internal Medicine, National Taiwan University Hospital Hsin-Chu Branch, Hsin-Chu, Taiwan; 2Department of Dentistry, School of Dentistry, National Taiwan University Hospital, Taipei, Taiwan; 3Department of Computer Science and Information Engineering, National Taiwan University, Taipei, Taiwan; 4Graduate Institute of Electronics Engineering, National Taiwan University, Taipei, Taiwan; 5MediaTek Inc., Hsinchu, Taiwan; 6Department of Radiology and Medical Imaging, National Taiwan University Hospital, Taipei, Taiwan; 7Center of Sleep Disorder, National Taiwan University Hospital, Taipei, Taiwan; 8Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan; 9School of Medicine, College of Medicine, National Taiwan University, Taipei, Taiwan; 10Center for Electronics Technology Integration, National Taiwan University, Taipei, Taiwan
*These authors contributed equally to this work
Correspondence: Pei-Lin Lee, Tel +886-2-2356-2755, Fax +886-2-2358-2867, Email [email protected]
Objective: Both continuous positive airway pressure (CPAP) pressure and polysomnographic phenotypes have been associated with mandibular advancement device (MAD) treatment response, but the precise relationship has not been fully elucidated. We hypothesized that utilizing CPAP pressure would predict the MAD response in treatment-naïve patients with moderate-severe obstructive sleep apnea (OSA), and the MAD response would be associated with two polysomnographic phenotypes, including sleep stage dependency and positional dependency.
Methods: OSA treatment-naïve patients with an apnea-hypopnea index (AHI) ≥ 15/h who declined CPAP treatment and received MAD treatment for 3– 6 months were enrolled. The MAD treatment response was defined as 1) residual AHI under MAD (AHIMAD) < 5/h and 2) AHIMAD < 10/h. Logistic regression was applied to identify the association between CPAP pressure and MAD treatment responders. The predictability of the MAD responder status utilizing CPAP pressure was assessed with the area under the receiver operating characteristic (AUROC).
Results: A total of 128 enrolled patients (AHI ≥ 30/h in 74.2%) were recruited, of whom 119 patients and 80 patients were included for analysis of sleep stage and positional dependency, respectively. REM-predominant OSA had lower AHI than stage-independent OSA, while the supine-predominant phenotype had lower anthropometrics than the nonpositional-dependent phenotype. The response rates for AHIMAD < 5/h and AHIMAD < 10/h were 25.8% and 48.4%, respectively. Lower anthropometrics, baseline AHI, and supine predominance were associated with the responder status, while CPAP pressure was an independent predictor. The AUROCs for the prediction of AHIMAD < 5/h and AHIMAD < 10/h responders were 0.635 and 0.664, respectively. Utilizing a CPAP level > 14 cmH2O as the cutoff to predict criterion 1 and 2 nonresponders, the sensitivity was 93.9% and 95.2%, respectively.
Conclusion: In treatment-naïve patients with moderate-severe OSA, the supine-predominant phenotype and lower CPAP pressure were associated with the MAD response, while the sleep stage dependency phenotype was not. Utilization of a CPAP level > 14 cmH2O could be a sensitive measure to identify nonresponders.
Keywords: continuous positive airway pressure, mandibular advancement device, polysomnography, phenotype, sleep apnea, obstructive
Introduction
Obstructive sleep apnea (OSA) is a common disease with a 9–38% prevalence in the general population.1 It is characterized by the recurrent collapse of the upper airway during sleep, resulting in chronic intermittent hypoxia and sleep fragmentation. Untreated OSA is associated with hypertension, cardiovascular mortality, motor vehicle accidents, diabetes mellitus, and impaired quality of life.2–4 Continuous positive airway pressure (CPAP) therapy is the standard treatment for moderate-severe OSA and can improve daytime sleepiness, quality of life, and blood pressure.5–9 However, the efficacy of CPAP is often offset by suboptimal adherence.10 Mandibular advancement device (MAD) treatment is an alternative for patients who refuse or cannot tolerate CPAP therapy. The response to MAD treatment is defined according to the residual apnea-hypopnea index (AHI) on MAD treatment (AHIMAD) and AHI reduction: criterion 1, AHIMAD <5/h with a reduction >50%; criterion 2, AHIMAD <10/h with a reduction >50%, and criterion 3, a reduction in AHI >50%. The response rates to the three criteria have been reported to be 48%, 64%, and 35%, respectively, which highlights the importance of patient selection.11,12 Therefore, a biomarker is needed to identify patients who would benefit from MAD treatment.
Factors associated with a favorable response to MAD treatment include younger age, female sex, lower AHI, body mass index (BMI) and neck circumference,11–15 craniofacial features (eg, angle between the anterior cranial base and mandibular plane),16 extent of mandibular advancement,17 and upper airway response (collapsibility, loop gain, arousal threshold, compensation, and ventilatory response to arousal).18 Few studies have linked polysomnographic phenotypes, including sleep stage dependency and positional dependency, to MAD treatment response. Three studies have shown that positional-predominant OSA was more likely to have a better response to MAD therapy than non-positional OSA,19–21 while one study showed the opposite findings.14 One study reported that rapid eye movement (REM)-predominant OSA was associated with a lower MAD treatment response,14 while another reported no association between sleep-stage dependency and MAD treatment response.22 The inconsistencies are partly related to differences in the definitions of sleep stage dependency, positional dependency and MAD type.14,15,19–22
Recent studies have reported that the CPAP pressure was associated with the MAD treatment response.23–26 Our previous study identified that higher BMI and higher CPAP pressure were associated with AHIMAD ≥15/h.27 Tsuiki et al reported that a fixed pressure ≥10.5 cmH2O could predict no response to MAD therapy across all three criteria in male Japanese patients adhering to CPAP treatment.26 Sutherland et al reported that a fixed pressure ≥13 cmH2O was predictive of criterion 1 or 2 nonresponders in treatment-naïve Caucasian patients.25 Additionally, Storesund et al reported that a maximum autoadjusting CPAP (APAP) level >12 cmH2O could predict criterion 1 and 2 nonresponders in Caucasian patients nonadherent to APAP.24 Moreover, Dort et al reported that CPAP level >9 cmH2O, obtained from both fixed pressure and APAP, could predict criterion 1 nonresponders in a variety of Caucasian patients, including those who were treatment naïve; had failed CPAP treatment; had an unsuccessful surgery; and were using a MAD as a temporary alternative.23 These inconsistencies in CPAP level cutoff values may be related to the heterogeneity of the participants, treatment prior to MAD treatment, and the method of determining the CPAP pressure.
To the best of our knowledge, no study has reported the association between MAD treatment response and CPAP pressure and the polysomnographic phenotype of sleep stage and positional dependency. Moreover, it is unclear whether the predictability of the MAD treatment response with CPAP pressure varies across different polysomnographic phenotypes. We hypothesized that the level of CPAP was predictive of the MAD treatment response independent of the polysomnographic phenotype (sleep stage dependency and positional dependency) in treatment-naïve patients with moderate-severe OSA. The present study aimed to test the association between CPAP pressure and MAD treatment responder status across different sleep stages and positional dependency phenotypes. We also tested the predictability of the MAD response utilizing CPAP pressure.
Methods
Study Setting
This retrospective study was conducted at the Center of Sleep Disorder of National Taiwan University Hospital (NTUH). The routine protocol for treating patients with moderate-severe OSA (AHI ≥15/h) has previously been reported.27 Briefly, patients underwent 2-week fixed-pressure CPAP, where therapeutic pressure was obtained by overnight manual titration. Patients who declined CPAP treatment were referred to an orthodontist for MAD treatment. Three to six months after MAD delivery, the patient underwent follow-up polysomnography (PSG) while on MAD to determine the response to MAD treatment.
Participants and Data Collection
Medical records of patients referred for suspected OSA from January 1, 2008, to December 31, 2017, were reviewed for eligibility. Patients who fulfilled all the following inclusion criteria were eligible for the study: 1) age 20–80 years; 2) diagnosed moderate-severe OSA; 3) no previous treatment for OSA; 3) CPAP titration to determine the therapeutic pressure; and 4) refusal of CPAP treatment and subsequent receipt of MAD treatment for 3–6 months. Patients were excluded if they fulfilled one of the following exclusion criteria: 1) failed CPAP titration; 2) residual AHI ≥ 5/h at a CPAP level of 20 cmH2O; 3) MAD treatment period < 3 months; and 4) refusal of follow-up PSG after MAD for 3–6 months (Figure S1).
Data extracted from collected medical records included demographics, anthropometrics [body mass index (BMI), neck and waist circumference], subjective sleepiness, PSG parameters, and CPAP pressure. All methods were carried out in compliance with the Declaration of Helsinki and the data remained confidential. The study protocol was approved by the Research Ethics Committee of NTUH (protocol number 20161218ORINA). Because it was a retrospective study, the need for consent from the participants was waived by the Research Ethics Committee.
Polysomnographic Phenotype
Full-night PSG (Embla N7000, Medcare Flaga, Reykjavik, Iceland) was performed in the sleep lab following the protocol as previously described.27 Apnea was defined as the absence of airflow for ≥ 10 sec, and hypopnea was defined as a 30% decrease in airflow for ≥ 10 sec associated with a ≥ 4% reduction in arterial oxygen saturation. The oxygen desaturation index was defined as the number of times that pulse oxygen saturation decreased by ≥ 4% per hour.28
The polysomnographic phenotypes in the present study included positional dependency and sleep stage dependency. Patients with a time in supine or nonsupine sleep <15 min were excluded from the analysis of positional dependency, while patients with a time in REM or NREM <15 min were excluded from the analysis of sleep stage dependency. Positional dependency was defined as the ratio of the AHI during supine sleep (AHIsupine) to the AHI during nonsupine sleep (AHInonsupine). Supine-predominant OSA was defined as an AHIsupine/AHInon-supine ratio ≥ 2, and nonpositional OSA was defined as an AHIsupine/AHInon-supine ratio < 2.
Sleep stage dependency was defined as the ratio of AHI during REM (AHIREM) to AHI during NREM (AHINREM). Because the definition of sleep stage dependency was inconsistent across previous reports, two definitions for the sleep stage phenotype were applied in the present study. First, REM-predominant OSA was defined as an AHIREM/AHINREM ratio ≥ 2, and NREM-predominant OSA was defined as an AHIREM/AHINREM ratio ≤ 0.5. Stage-independent OSA was defined as a ratio between 2 and 0.5.14,29,30 Second, REM-related OSA (AHIREM/AHINREM ratio ≥ 2) and NREM-related OSA (AHIREM/AHINREM ratio < 2) were defined.31–33
Determination of CPAP Pressure
The therapeutic pressure was determined by overnight manual titration using BiPAP SynchronyTM (Respironics Inc., Murrysville, PA, USA) following a published protocol.27 The manual titration started with the CPAP mode at a pressure of 4 cmH2O. The pressure was then increased in 1 cmH2O increments over 10 min to eliminate obstructive events, including apnea, hypopnea, and snoring, and to minimize electroencephalography arousals until 30 min had elapsed without any obstructive events. Optimal pressure was defined as the pressure at which the AHI was < 5/h for 15 min, including supine REM sleep. The choice of interface started with a nasal mask, which was changed to an oronasal mask if a significant mouth leak was detected.
MAD Treatment
The MAD used in the present study was a monobloc that was fabricated as previously described to achieve 75% of the maximum mandibular advancement, and the vertical opening was limited to 5 mm.27 The design of the MAD remained the same during the study period. MAD was delivered four weeks after taking a dental impression. The patients visited the clinic at the 1st, 3rd, 6th, and 12th months after MAD delivery, where the self-reported average nightly usage was recorded at every follow-up visit.
Outcomes
The outcome was the MAD treatment response, which was evaluated by reduction in the baseline AHI and residual AHI (AHIMAD) on the follow-up PSG. The response to MAD treatment was defined by two criteria: criterion 1, residual AHIMAD < 5/h with AHI reduction > 50%; criterion 2, AHIMAD < 10/h with AHI reduction > 50%.23,25,26
Data Analysis
Factors associated with positional dependency were determined by comparing the clinical features between supine-predominant and nonpositional-dependent OSA; between REM-predominant, NREM-predominant, and stage-independent OSA; and between REM-related and NREM-related OSA. Factors associated with MAD treatment response were determined by comparing the clinical features between the responders and nonresponders.
Correlations between clinical features, CPAP pressure, baseline AHI, and AHIMAD were evaluated using Spearman's correlation analysis. The association between CPAP pressure and MAD treatment response was determined with logistic regression. Multiple logistic regression was conducted with age, sex, BMI, baseline AHI, CPAP pressure, sleep stage dependency, positional dependency, and factors significant at the 0.1 level in univariate analysis entered into the regression model.
The ability of the CPAP pressure to predict the MAD treatment response was assessed using the area under the receiver operating characteristic curve (AUROC). In addition, the best cutoff CPAP level was based on sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), negative likelihood ratio (LR−), and accuracy.
Continuous variables are expressed as medians (interquartile ranges [IQRs]), and categorical variables are expressed as numbers (percentages). The Wilcoxon-Mann–Whitney U-test, chi-square test or Fisher’s exact test with Bonferroni correction, and the Kruskal–Wallis test with the Bonferroni post hoc method were used as appropriate. A two-tailed P value <0.05 was considered to be statistically significant. All statistical analyses were conducted using SPSS version 23 (SPSS, Chicago, IL, USA).
Data Availability Statement
The data of individual subjects that are not publicly available may be obtained from the corresponding author upon reasonable request.
Results
Clinical Features of the Participants
Figure S1 shows the recruitment flowchart. A total of 5796 patients with moderate-severe OSA aged 20–80 years were screened. A total of 4859 patients were newly diagnosed and had never been treated for OSA (treatment-naïve). Among the 1559 who underwent CPAP titration, 53 had titration failure, and 151 had a residual AHI > 5/h at a pressure of 20 cmH2O. Among the 1355 patients with a residual AHI<5/h, 144 received MAD treatment. A total of 128 patients who completed 3–6 months of MAD treatment and underwent follow-up PSG were recruited for the study.
Table 1 shows the clinical features of these 128 patients. The patients were middle-aged, predominantly male (82%), and overweight-obese with a median BMI of 26.8 kg/m2 (IQR, 24.2–28.6). The median baseline AHI was 38.9/h (IQR, 29.3–52.1), with an AHI ≥ 30/h observed in 74.2% of the patients. The median CPAP level was 9 cmH2O (IQR, 7–12), and the median AHIMAD was 10.2/h (IQR, 4.7–20.3). Compared to the male patients, female patients were older, had lower neck and waist circumferences, had more excessive daytime sleepiness (EDS), and had a higher AHIREM.
 |
Table 1 Comparisons of the 105 Male and 23 Female Enrolled Patients |
Polysomnographic Phenotype
Nine patients with time in REM < 15 mins were excluded from the analysis of the sleep stage dependency phenotype. Among the remaining 119 patients, stage independency accounted for 71.4%, while REM predominance and NREM predominance accounted for 16.8% and 11.8%, respectively. Patients with REM-predominant OSA tended to have a higher percentage of females and lower baseline AHI than sleep stage-independent patients. Patients with NREM-predominant OSA had a lower percentage of criterion 1 and 2 responders. Age, sex, anthropometrics, and CPAP pressure were similar in the three sleep-stage dependency phenotypes (Table 2). For the other definition of sleep stage dependency, 20 patients had REM-related OSA and 99 had NREM-related OSA, and REM-related OSA had a higher percentage of female patients and lower baseline AHI but a similar percentage of criterion 1 and 2 responders than NREM-related OSA (Table S1).
 |
Table 2 Comparison of Patients with Different Sleep Stage Dependency and Positional Dependency Phenotypes |
A total of 48 patients with supine sleep and nonsupine sleep < 15 mins were excluded from the analysis of the positional dependency phenotype. In the remaining 80 patients, supine-predominant and nonpositional OSA accounted for half each. Compared with the patients with nonpositional OSA, those with supine-predominant OSA were older, had lower neck and waist circumferences, and had a higher percentage of criterion 1 responders (Table 2).
Response to MAD Treatment
The percentages of criterion 1 and 2 responders were 25.8% and 48.4%, respectively. For criteria 1 and 2, responders had lower anthropometrics and lower CPAP pressure but a similar age and percentage of males compared with nonresponders. Compared with nonresponders, criterion 2 responders had a lower baseline AHI, lower percentage of severe OSA, and lower AHINREM, AHIsupine and AHInon-supine, while AHInon-supine was lower in criterion 1 responders. Regarding sleep stage dependency, stage-independent OSA was the most common phenotype in both responders and nonresponders for both criterion 1 and 2. For criterion 1 responders, there was a higher percentage of stage-independent and no NREM-predominant OSA. For criterion 1 responders, the percentage of supine-predominant OSA was higher than that of nonresponders (Table 3).
 |
Table 3 Comparison of Criterion 1 and 2 Responders and Nonresponders |
Factors Associated with the MAD Treatment Response
Spearman's correlation showed that the AHIMAD was positively correlated with BMI, neck and waist circumferences, baseline AHI, and CPAP pressure. CPAP pressure was correlated with BMI, neck circumference, and baseline AHI (Figure 1A). For patients included in the analysis of sleep stage dependency, AHINREM was correlated with both AHIMAD and CPAP pressure, while the AHIREM was not (Figure 1B). For patients included in the analysis of positional dependency, AHIsupine and AHInon-supine were correlated with AHIMAD, while AHInon-supine was correlated with CPAP pressure (Figure 1C).
Univariate analysis revealed that BMI, neck circumference, and baseline AHI were associated with CPAP, while age, sex, and waist circumference were not in all patients. Neither the sleep stage dependency nor positional dependency phenotype was associated with CPAP pressure (Table S2). Lower anthropometrics and CPAP pressure were associated with criterion 1 and 2 responders, while lower baseline AHI was associated with criterion 2 responders. Compared with stage-independent OSA, REM-predominant and NREM-predominant OSA has similar associations with responders. Compared with nonpositional OSA, supine-predominant OSA was associated with criterion 1 responders (Table S3).
Multivariable analysis was applied to identify the association between CPAP pressure and MAD treatment responders. The unadjusted model showed that lower CPAP pressure was associated with the MAD treatment response. For criterion 1 responders, the association was not observed after adjustment for BMI in either all groups or patients included for analysis of sleep stage dependency. However, for patients included for positional dependency, a lower CPAP pressure was associated with responder status, even with further adjustment for position dependency. For criterion 2, CPAP pressure was associated with responder status after full adjustment, including age, sex, BMI, baseline AHI, and sleep stage dependency or positional dependency (Table 4).
 |
Table 4 Multivariable Logistic Regression to Identify the Association Between CPAP and MAD Treatment Responder |
Prediction of MAD Responder Status with CPAP Pressure
Using CPAP pressure alone, the AUROC was 0.635 (95% CI, 0.519–0.751; P=0.027) and 0.664 (95% CI, 0.570–0.757; P=0.001) in predicting criterion 1 and 2 responders, respectively (Figure 2). To maximize the sensitivity in identifying patients who may benefit from MAD treatment, CPAP level >14 cmH2O was selected as a cutoff value to predict both criterion 1 and 2 nonresponders, in which the minimal pressure reached the highest sensitivity. The prediction model of criterion 1 nonresponders had a sensitivity of 93.9%, specificity of 13.7%, and accuracy of 34.4%. The prediction model of criterion 2 nonresponders had a sensitivity of 95.2%, specificity of 18.2%, and accuracy of 55.5% (Table 5).
 |
Table 5 Utilizing CPAP to Predict MAD Treatment Nonresponders with Criteria 1 and 2 According to Different Cutoff Values |
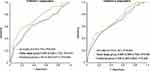 |
Figure 2 AUROC in the prediction of MAD responder status with CPAP pressure. |
Discussion
This study aimed to test the association between CPAP pressure and MAD treatment responders across different sleep stages and positional dependency phenotypes in treatment-naïve patients with moderate-severe OSA. Our results showed that CPAP pressure was independently associated with responder status independent of sleep stage and positional dependency. Utilizing CPAP level >14 cmH2O identified nonresponders to MAD treatment with a sensitivity of 93.9–95.2%. Moreover, supine-predominant OSA might be associated with the MAD treatment response.
The strength of our study included our recruitment of patients with moderate-severe OSA with AHI ≥ 30/h in 74.2%. In this population, CPAP is superior to MAD for AHI reduction, and MAD is an alternative treatment for those who refuse or cannot tolerate CPAP treatment. Hence, a parameter of high sensitivity may maximize the chance of identifying candidates for MAD treatment. Moreover, only patients whose time in supine sleep, nonsupine sleep, REM and NREM ≥ 15 min were included for analysis of sleep stage dependency and positional dependency, which enhanced the robustness of the phenotyping. Our results showed that CPAP pressure was a sensitive measure in identifying candidates for MAD treatment across different polysomnographic phenotypes.
In the present study, the response rates for criterion 1 and 2 were 25.8% and 48.4%, respectively. These rates were lower than the 53.8% and 69.2% reported in the study by Sutherland et al, who recruited 78 treatment-naïve Caucasian patients.25 It was also lower than the 35.6% and 64.4% reported by Storesund et al, who recruited 87 Caucasian patients with moderate-severe OSA who were CPAP non-adherent.24 This discrepancy may be related to the older age, higher baseline AHI, monoblock device use, longer duration of MAD treatment, and Asian ethnicity of our patients. Older age and higher baseline AHI have been associated with a poor response to MAD treatment,15 while Asian ethnicity has been associated with a higher craniofacial risk and higher AHI than BMI-matched Caucasians. These discrepancies may contribute to the lower response rate in the present study. Our response rate was similar to the result reported by Tsuiki et al. However, Tsuiki included patients who adhered to CPAP, whose upper airway may have less collapsibility and need a lower CPAP pressure. In contrast, we included treatment-naïve patients whose airway may have had higher collapsibility and who needed higher CPAP pressure to stent the airway. The difference in upper airway physiology was supported by the higher cutoff of CPAP level (14 cmH2O) in the present study than that (10.5 cmH2O) reported by Tsuiki et al.26
Supine position-related fallback of the mandible, tongue, and soft palate could compromise the upper airway during sleep and could be reversed by mandibular protrusion with MAD treatment. Our study revealed that supine-predominant OSA was associated with a higher criterion 1 response, which is in line with the study by Chung et al.21 Both studies excluded patients with inadequate nonsupine sleep time, which may enhance the robustness of the definition of positional dependency. Sutherland et al14 reported that patients with supine-predominant OSA had a lower response rate, which was in contrast to the findings of our and other studies.19–21 The higher BMI and lower percentage of supine-predominant OSA in the study by Sutherland et al may contribute to the paradoxical findings.
Very few studies have investigated the association between stage-dependent OSA and MAD treatment response. Our results showed that the response rate was similar between different sleep stage dependencies for two definitions, which is in line with the findings of the study by Nishio et al.22 Our finding is in contrast with that reported by Sutherland et al, who showed that REM-predominant OSA had a lower response rate than NREM-predominant and stage-independent OSA.14 A possible explanation for the discrepancy in the results is that participants included in the study by Sutherland had more elderly females, higher BMI, and lower AHI, which may contribute to a higher percentage of REM-predominant OSA and higher residual AHI at REM. Despite the difference in response rate, all three studies confirmed that sleep stage dependency was not associated with MAD treatment response.
There were several limitations to this study. First, it is a retrospective study with a small cohort consisting of a small number of each polysomnographic phenotype, which may underestimate the power of the study. However, despite the possibility of underestimation, our study still confirmed the association between MAD response, positional dependency and CPAP pressure. Such an association may be more significant in the larger cohort. Second, patients with residual AHI ≥ 5/h at a CPAP level of 20 cmH2O were excluded, and thus, our findings may not apply to patients treated with BPAP. Third, the MAD in the present study was a nontitratable monobloc with tongue backing. Even though a monobloc MAD has been reported to be noninferior to a titratable bibloc in reducing AHI,34,35 the CPAP pressure cutoff may be different between the two designs. Fourth, all participants were of Asian ethnicity recruited from a single-center hospital, and our findings need to be validated in a large-scale prospective study with a multiethnic population. Fifth, craniofacial features were not analyzed in the present study. However, craniofacial phenotyping has been demonstrated to have limited utility in enhancing models based on clinical variables alone,36 and there is no universal standard to evaluate craniofacial features.15 Sixth, the CPAP pressure in the present study was obtained by overnight manual titration, which may limit the generalizability of its implications. Further study to validate the predictability of MAD treatment response utilizing pressure obtained from APAP may promote feasibility.
In conclusion, in patients with moderate-severe OSA who were treatment-naïve, CPAP pressure may be a sensitive predictor for identifying candidates for MAD treatment, and the predictability was consistent across the different polysomnographic phenotypes. Further study with the CPAP pressure obtained from APAP in a large-scale and multiethnicity cohort to validate the findings of the present study is warranted.
Rationale
Mandibular advancement devices (MADs) are alternative treatments to continuous positive airway pressure (CPAP) for patients with moderate-severe obstructive sleep apnea (OSA) who cannot tolerate CPAP therapy. Both CPAP pressure and positional phenotype (supine vs nonsupine) have been associated with the response to MAD treatment. However, the interplay between CPAP, polysomnographic phenotype (sleep stage dependency, positional dependency), and MAD treatment response has not been fully elucidated.
Study Impact
In patients with moderate-severe OSA who were treatment-naïve, the response rates for residual AHI under MAD (AHIMAD) <5/h and AHIMAD <10/h were 25.8% and 48.4%, respectively. Supine dependency was associated with responders, while sleep stage dependency was not. CPAP pressure was an independent predictor, and utilization of CPAP level >14 cmH2O could be a sensitive measure for identifying nonresponders.
Acknowledgments
This study was sponsored by the National Scientific Council (NSC 102-2314-B002-099), the Ministry of Science and Technology of Taiwan (MOST 103-2314-B-002−139-MY3, 109-2314-B-002-252), National Taiwan University Hospital (NTUH 109-042, 108-S4331, 110-N5164, 107-19, 111-S0298, 111-X0033), National Taiwan University (NTU-EPR-104R8951-1; 105R8951-1; 106R880301), and Center for Electronic Technology Integration (NTU-107L900502, 108L900502, 109L900502) from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, and NTU-NTUH-MediaTek Innovative Medical Electronics Research Center. The work was performed in National Taiwan University Hospital.
Disclosure
All authors declare that they have no conflicts of interest in this work.
References
1. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002
2. Altaf QA, Dodson P, Ali A, et al. Obstructive sleep apnea and retinopathy in patients with type 2 diabetes. A longitudinal study. Am J Respir Crit Care Med. 2017;196(7):892–900. doi:10.1164/rccm.201701-0175OC
3. Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med. 2009;122(12):1122–1127. doi:10.1016/j.amjmed.2009.04.026
4. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi:10.1164/rccm.2109080
5. McDaid C, Duree KH, Griffin SC, et al. A systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Med Rev. 2009;13(6):427–436. doi:10.1016/j.smrv.2009.02.004
6. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111–119. doi:10.1093/sleep/34.1.111
7. Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90(1):47–112. doi:10.1152/physrev.00043.2008
8. Lin MT, Lai CL, Lee PL, et al. Timely diagnosis and treatment of sleep apnea reduce cardiovascular sequelae in patients with myocardial infarction. PLoS One. 2018;13(7):e0201493. doi:10.1371/journal.pone.0201493
9. Lin MT, Lin HH, Lee PL, et al. Beneficial effect of continuous positive airway pressure on lipid profiles in obstructive sleep apnea: a meta-analysis. Sleep Breath. 2015;19(3):809–817. doi:10.1007/s11325-014-1082-x
10. Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887–895. doi:10.1164/ajrccm/147.4.887
11. Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827. doi:10.5664/jcsm.4858
12. Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10(2):215–227. doi:10.5664/jcsm.3460
13. Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163(6):1457–1461. doi:10.1164/ajrccm.163.6.2004213
14. Sutherland K, Takaya H, Qian J, Petocz P, Ng AT, Cistulli PA. Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med. 2015;11(8):861–868. doi:10.5664/jcsm.4934
15. Chen H, Eckert DJ, van der Stelt PF, et al. Phenotypes of responders to mandibular advancement device therapy in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Med Rev. 2020;49:101229. doi:10.1016/j.smrv.2019.101229
16. Ng AT, Darendeliler MA, Petocz P, Cistulli PA. Cephalometry and prediction of oral appliance treatment outcome. Sleep Breath. 2012;16(1):47–58. doi:10.1007/s11325-011-0484-2
17. Walker-Engstrom ML, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A. A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath. 2003;7(3):119–130. doi:10.1007/s11325-003-0119-3
18. Op de Beeck S, Dieltjens M, Azarbarzin A, et al. Mandibular advancement device treatment efficacy is associated with polysomnographic endotypes. Ann Am Thorac Soc. 2021;18(3):511–518. doi:10.1513/AnnalsATS.202003-220OC
19. Yoshida K. Influence of sleep posture on response to oral appliance therapy for sleep apnea syndrome. Sleep. 2001;24(5):538–544. doi:10.1093/sleep/24.5.538
20. Lee CH, Jung HJ, Lee WH, et al. The effect of positional dependency on outcomes of treatment with a mandibular advancement device. Arch Otolaryngol Head Neck Surg. 2012;138(5):479–483. doi:10.1001/archoto.2012.452
21. Chung JW, Enciso R, Levendowski DJ, Morgan TD, Westbrook PR, Clark GT. Treatment outcomes of mandibular advancement devices in positional and nonpositional OSA patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(5):724–731. doi:10.1016/j.tripleo.2009.11.031
22. Nishio Y, Hoshino T, Murotani K, et al. Treatment outcome of oral appliance in patients with REM-related obstructive sleep apnea. Sleep Breath. 2020;24(4):1339–1347. doi:10.1007/s11325-019-01966-5
23. Dort L, Savard N, Dort E, Dort M, Dort J. Does CPAP pressure predict treatment outcome with oral appliances? J Dent Sleep Med. 2016;3(4):113–117. doi:10.15331/jdsm.6248
24. Storesund A, Johansson A, Bjorvatn B, Lehmann S. Oral appliance treatment outcome can be predicted by continuous positive airway pressure in moderate to severe obstructive sleep apnea. Sleep Breath. 2018;22(2):385–392. doi:10.1007/s11325-017-1578-2
25. Sutherland K, Phillips CL, Davies A, et al. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med. 2014;10(9):943–949. doi:10.5664/jcsm.4020
26. Tsuiki S, Kobayashi M, Namba K, et al. Optimal positive airway pressure predicts oral appliance response to sleep apnoea. Eur Respir J. 2010;35(5):1098–1105. doi:10.1183/09031936.00121608
27. Liu HW, Chen YJ, Lai YC, et al. Combining MAD and CPAP as an effective strategy for treating patients with severe sleep apnea intolerant to high-pressure PAP and unresponsive to MAD. PLoS One. 2017;12(10):e0187032. doi:10.1371/journal.pone.0187032
28. Iber C, Quan S. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications.
29. Joosten SA, Hamza K, Sands S, Turton A, Berger P, Hamilton G. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology. 2012;17(1):99–107. doi:10.1111/j.1440-1843.2011.02037.x
30. Joosten SA, O’Driscoll DM, Berger PJ, Hamilton GS. Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev. 2014;18(1):7–17. doi:10.1016/j.smrv.2013.01.005
31. Sakao S, Sakurai T, Yahaba M, et al. Features of REM-related sleep disordered breathing in the Japanese population. Intern Med. 2015;54(12):1481–1487. doi:10.2169/internalmedicine.54.4248
32. Conwell W, Patel B, Doeing D, et al. Prevalence, clinical features, and CPAP adherence in REM-related sleep-disordered breathing: a cross-sectional analysis of a large clinical population. Sleep Breath. 2012;16(2):519–526. doi:10.1007/s11325-011-0537-6
33. Hoshino T, Sasanabe R, Mano M, et al. Prevalence of rapid eye movement-related obstructive sleep apnea in adult narcolepsy. Intern Med. 2019;58(15):2151–2157. doi:10.2169/internalmedicine.2601-18
34. Bloch KE, Iseli A, Zhang JN, et al. A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med. 2000;162(1):246–251. doi:10.1164/ajrccm.162.1.9908112
35. Ishiyama H, Hasebe D, Sato K, et al. The efficacy of device designs (mono-block or bi-block) in oral appliance therapy for obstructive sleep apnea patients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2019;16(17):3182. doi:10.3390/ijerph16173182
36. Sutherland K, Chan ASL, Ngiam J, Dalci O, Darendeliler MA, Cistulli PA. Awake multimodal phenotyping for prediction of oral appliance treatment outcome. J Clin Sleep Med. 2018;14(11):1879–1887. doi:10.5664/jcsm.7484
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

