Back to Journals » Journal of Asthma and Allergy » Volume 15
Phenotypic Distinctions Between Omega-5-Gliadin Allergy and Peanut Allergy: Clinical Profile, Reaction Rates and Triggers, and Quality of Life
Authors Zubrinich CM , Puy RM, O'Hehir RE , Hew M
Received 19 September 2022
Accepted for publication 22 November 2022
Published 22 December 2022 Volume 2022:15 Pages 1823—1830
DOI https://doi.org/10.2147/JAA.S390125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Celia M Zubrinich,1,2 Robert M Puy,3 Robyn E O’Hehir,1,3 Mark Hew1,2
1Allergy, Asthma & Clinical Immunology, Alfred Health, Melbourne, Victoria, Australia; 2School of Public Health & Preventive Medicine, Monash University, Melbourne, Victoria, Australia; 3Allergy and Clinical Immunology Laboratory, Department of Immunology and Pathology, Central Clinical School, Monash University, Melbourne, Victoria, Australia
Correspondence: Celia M Zubrinich, Email [email protected]
Background: Different phenotypes of food allergy may exist, exhibiting distinct clinical features, and driven by different pathogenic mechanisms. We compared omega-5-gliadin (O5G) allergy to peanut allergy, focusing on clinical features, reaction rates and triggers, and quality of life (QOL).
Methods: We surveyed adults with O5G allergy and peanut allergy regarding their diagnosis, co-morbidities, allergic reactions, and QOL measured by the FAQLQ-AF.
Results: We received responses from 43/80 (54%) individuals with O5G allergy and 43/130 (33%) with peanut allergy. Compared to peanut allergic individuals, those with O5G allergy were older at age of onset (37.2 vs 2.5 years, p < 0.001), had fewer additional atopic conditions (0.88 vs 2.93, p < 0.001) or food allergies (0.15 vs 1.86, p < 0.001), and more frequent reactions before diagnosis (1.085 vs 0.29 per month, p < 0.05) Reaction rates improved in both groups following diagnosis. Reactions to peanut were more often triggered by accidental exposure (84% vs 26%, p < 0.001) and being away from home (65% vs 28%, p < 0.001), while reactions to O5G were more often due to deliberate ingestion (30% vs 9%, p < 0.05) or unexpected exercise (35% vs 2%, p < 0.001). Overall QOL score was similar between groups (4.2 in O5G allergy, 4.7 in peanut allergy, p = 0.12), but worse among women and those with additional food allergies.
Conclusion: Phenotypic differences between O5G and peanut allergy support the development of different clinical approaches and the possibility of targeting distinct pathogenic mechanisms for prevention and treatment. Quality of life was impaired to a similar degree between groups.
Keywords: omega-5-gliadin allergy, wheat allergy, peanut allergy, food allergy, anaphylaxis, wheat-dependent exercise-induced allergy, WDEIA, food-dependent exercise-induced allergy, FDEIA, quality of life, QOL, Australia
Introduction
IgE mediated food allergy occurs in 1–2% of adults,1,2 with significant impacts on health and behaviour for those individuals. It has been proposed that different phenotypes of food allergy exist, each exhibiting distinct clinical features, and underpinned by different endotypes of underlying pathogenic mechanisms.3,4 Improving our understanding of distinct food allergy phenotypes may provide pathogenic insights that are important for development of effective prevention strategies. It may also enable a personalized approach to practical management strategies, tailored to the particular disease and to the individual.
Key to the management of food allergy is dietary restriction, but this can sometimes be difficult to implement in practice. Patients need to exercise constant vigilance to avoid food allergens successfully, but also be prepared to manage an inadvertent exposure.5 Both requirements would be expected to impact the quality of life (QOL) of the affected individual. Validated tools to quantify QOL in food allergy are now available.6
Food-dependent exercise-induced allergy is a unique clinical syndrome in which allergic reactions, including anaphylaxis, can occur if a patient exercises within a few hours of ingesting a specific food to which they are sensitised. The requirement for the presence of a co-factor before an allergic episode can occur is, therefore, a different allergic phenotype, and in some cases results in considerable difficulty in recognising the correct diagnosis. We previously identified that individuals with Omega-5-gliadin (O5G) allergy contributing to food-dependent exercise-induced allergy (FDEIA) had unique clinical features.7 We hypothesize that this condition may be phenotypically different from peanut allergy – as an example of a more classic or conventional IgE mediated food allergy. We, therefore, undertook a comparison of patient cohorts with O5G allergy with peanut allergy, in terms of clinical features and presentation, reaction rates and triggers, and disease-specific QOL.
Methods
Our tertiary university academic centre, Alfred Health, in Melbourne, Victoria, Australia, provides allergy services for the surrounding metropolitan area and additionally draws referrals from the entire state of Victoria, Australia, providing approximately 6000 outpatient consultations per year. We invited two groups of patients, adults with peanut allergy and adults with O5G allergy, to participate in this study.
Adults with a diagnosis of O5G allergy were identified through a review of positive pathology results (ImmunoCAP® assay, Phadia, Uppsala, Sweden) between 1 November 2008 (when the O5G test first became available locally) and 31 December 2016. For comparison, peanut-allergic adults were identified from a database retained by our large clinical service. All patients had been assessed in our service as having confirmed food allergy according to the diagnostic group. Patients were sent a questionnaire regarding demographics and allergic comorbidities including other IgE mediated food allergies (Appendix 1). We surveyed the number of allergic reactions and time periods so that the rates of allergic reaction before and after diagnosis could be calculated. We determined management strategies that were undertaken by the individual. Individuals were asked for their assessment of factors contributing to allergic reactions that occurred after the diagnosis was known; the responses could be multiple for each individual.
To better understand the approaches chosen to manage O5G allergy specifically, we divided patients into two management groups. In recognition of possible combinations of diet and exercise strategies relevant to this condition, we defined a “stringent” management approach as one that required complete avoidance of wheat/gluten (‘avoiders”) and/or separation of food and exercise by a minimum of four hours (‘separators’). A “liberal” management approach involved neither of these approaches. This strategy is not of relevance in peanut allergy, so we did not measure it in this way.
We utilized an internationally validated disease-specific QOL instrument, FAQLQ-AF (food allergy quality of life questionnaire - adult form), which was administered to all participants and scored according to previously published methods.6 This tool includes questions about the impact of food allergy on lifestyle, relationships with others, eating out, and fear of allergic reactions. The results are presented as a total QOL score and also four component domains: allergen avoidance and dietary restrictions (AADR), risk of accidental exposure (RAE), food allergy-related health (FAH) and emotional impact (EI). The scores range from possible values of 1–7; a higher value indicates greater effects on QOL. We hypothesized that there would be greater impacts on QOL in O5G allergy, which is largely of adult-onset, and may have been associated with apparently unexplained allergic reactions if the diagnosis were not suspected at presentation.
We stated that responses would be de-identified, and thus the return of a completed questionnaire implied consent, in accordance with the Declaration of Helsinki. Ethics Committee approval was obtained for this study (Alfred Health REB No. 279/14). Comparisons were made by t-tests and one-way ANOVA. To assess the relationship between the various domains, bivariate Pearson’s correlation coefficients (r) were calculated. Statistics were calculated and graphics created using SPSS (Version 27).
The abstract of this paper was presented at the 32nd Annual Conference of the Australasian Society of Clinical Immunology and Allergy (ASCIA) in September 2022 in poster format with interim findings. The poster’s abstract was published in “Conference Poster Abstracts” in Internal Medicine Journal, October 2022, Volume 52 Issue S5 https://onlinelibrary.wiley.com/doi/full/10.1111/imj.47_15894.
Results
Participants
Between 1 November 2008 (when the O5G serum-specific IgE test first became available locally) and 31 December 2016, 80 individuals with O5G allergy were identified through a review of positive O5G results in our Adult Centre. Questionnaires were sent to all 80 identified patients between October 2014 and January 2017. Of these, 37 responded and six were “Returned-to Sender” (RTS). A second mail out to the remaining 37 yielded six further responses giving an overall response rate of 43/74 (58%). The cohort derivation has been described in detail, previously.7
For comparison, an initial 100 peanut-allergic adults were identified in reverse chronological order from a database of 300 retained by our large clinical service for adult patients dating from 2011 onwards. One hundred surveys were mailed out in June 2018 and 34 responses were received. A further 30 individuals were identified and mailed in June 2019 from whom an additional nine surveys were returned, coincidentally giving the same number of respondents for peanut allergy as for O5G allergy. Twelve questionnaires were “Returned-to Sender” resulting in a denominator of 118 and an overall response rate 43/118 (36.4%).
Clinical Characteristics (Table 1)
Onset of O5G allergy occurred predominantly in adulthood, while that of peanut allergy typically in childhood. Despite a shorter duration of allergic illness, individuals with O5G allergy were significantly older than those with peanut allergy. Men and women were equally represented.
 |
Table 1 Clinical Characteristics of Participants with Omega-5-Gliadin Allergy and Peanut Allergy |
The peanut allergy cohort exhibited higher rates of atopic diseases (eczema, asthma, additional food allergies) than the O5G allergy group (Table 1). They also had more concurrent food allergies than the O5G allergy group (1.86 vs 0.15 additional food allergies reported per person, p < 0.0001).
The majority of individuals in each group had experienced anaphylaxis (79% vs 88%, NS) and carried an epinephrine auto-injector (98% vs 91%, NS). A minority of individuals in each group had ever consulted with a dietitian (13/43 in each group, NS).
Reaction Rates Before and After Diagnosis
The peanut allergic patients reported a lower reaction frequency at baseline pre-diagnosis than the O5G allergic individuals (0.29 vs 1.085/month, p = 0.03) (Table 2). The reaction rate was significantly lower post-diagnosis in both groups. For peanut allergy it fell to 0.05/month (p = 0.001, compared to pre-diagnosis), and for O5G allergy it fell to 0.35/month (p = 0.012, compared to pre-diagnosis). Paired data were unavailable for 5 peanut allergic patients and 1 O5G allergic patient.
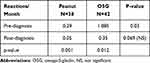 |
Table 2 Reaction Rates Before and After Diagnosis |
Triggers of Allergic Reactions
Reactions occurring in peanut allergy (compared with O5G allergy) were more often due to accidental exposure (84% vs 26%, p < 0.001) or while away from home (65% vs 28%, p < 0.001) (Table 3). Compared to peanut allergy, reactions occurred in O5G allergy more frequently due to deliberate ingestion of food allergen (9 vs 30%, p = 0.015) or unexpected exercise (2% vs 35%, p < 0.001).
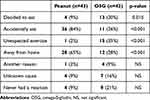 |
Table 3 Reported Triggers of Allergic Reactions by Food Allergen |
Quality of Life: Peanut vs O5G Allergy
The QOL score measured by FAQLQ-AF was not significantly different between the peanut allergy and O5G allergy groups (4.7± 1.27 vs 4.2 ±1.4, mean±SD, p = 0.12). Data are presented in Table 4.
 |
Table 4 FAQLQ-AF Scores (Total and Domains) by Food Allergen |
The four component domains of the FAQLQ-AF, Allergen avoidance and dietary restrictions (AADR), Risk of accidental exposure (RAE), Food allergy-related health (FAH) and Emotional Impact (EI) were compared. A higher value denotes greater effect on QOL. There was a greater impact on the Allergen Avoidance (AADR) domain of QOL in the peanut allergic group compared to O5G allergy (4.9 vs 4.2, P = 0.04). No other differences between the two groups were significant.
To assess the relationship between the various domains, bivariate Pearson’s correlation coefficients (r) were calculated. There were significant positive correlations between the various domains of the FAQLQ-AF; these ranged between r = 0.501 (AADR and FAH, p < 0.001) and r = 0.912 (FAQLQ-AF total score and EI, p < 0.001).
Additional Factors Affecting Quality of Life
The total QOL score (4.75 vs 4.06, p 0.018), as well as the Risk of accidental exposure domain (4.59 vs 3.82, p 0.016) and the Emotional impact domain (5.24 vs 4.16, p < 0.001), were significantly higher in women than in men (Table 5).
 |
Table 5 FAQLQ-AF Scores (Total and Domains) by Food Allergen and Sex |
The presence of additional food allergies, apart from peanut allergy or O5G allergy, negatively impacted the total FAQLQ-AF total score (4.7 vs 4.0, p < 0.019), and also reached significance in the Allergen avoidance and dietary restrictions domain (AADR) (4.8 vs 4.1, p = 0.045), and the Risk of accidental exposure domain (RAE) (4.6 vs 3.8, p = 0.013).
Total QOL, or QOL by domain, did not differ significantly whether or not anaphylaxis had ever occurred, whether there had been no reaction since diagnosis, whether there had been a dietitian consultation, by the number of additional food allergies, the number of atopic comorbidities, or how long the diagnosis had been present and age at questionnaire completion (data not shown).
Quality of Life in O5G Allergy – Stringent vs Liberal Strategies
To better understand the approaches chosen to manage O5G allergy specifically, we compared two management groups. We defined a “stringent” management approach as one that required complete avoidance of wheat/gluten (“avoiders”) or separation of food and exercise by a minimum of four hours (“separators”). A “liberal” management approach involved neither of these. Ten of 43 individuals adopted a “liberal” approach, the remainder were “stringent”. There were no differences in overall QOL or any of the domains between the two management groups (Table 6).
 |
Table 6 FAQLQ-AF Scores (Total and Domains) in O5G Allergy by Management Strategy |
Discussion
Our results suggest that O5G allergy and peanut allergy represent two distinct disease phenotypes. Peanut allergy presents predominantly in childhood and is associated with multiple atopic co-morbidities including other IgE mediated food allergies, while O5G allergy is almost exclusively of adult-onset, and associated with less atopic burden. Allergic reaction rates were higher in O5G allergy than in peanut allergy and tended to remain so even after definitive diagnosis and management advice were provided. Reactions in O5G allergy were often related to deliberate ingestion or unexpected exercise, whilst those associated with peanut allergy were more often triggered by accidental exposure and eating away from home. Despite these differences, QOL measures in both groups were generally similar, showing substantial impairment which was greater among women and those with additional food allergies.
Our findings are directly relevant to the search for definitive personalized treatments for food allergy. An accurate understanding of distinct food allergy phenotypes and aetiologies is needed to develop effective preventive measures for relevant pathogenic exposures. An understanding of QOL impact is needed to adequately determine the benefits (or otherwise) of interventions with food allergen-specific immunotherapy.
In our analysis, peanut allergy presented in a cohort of younger patients, almost all of whom had additional atopic co-morbidities. Substantial research has been directed toward understanding these risk factors, and such efforts have culminated in effective prevention8 and treatment9–12 strategies for peanut allergy. The presentation of O5G allergy later in life, with fewer atopic co-morbidities, hints at aetiological factors different to those in peanut allergy. Efforts to identify these factors may guide future personalized treatment and prevention for O5G allergy.
The rate of allergic reactions was higher in the O5G allergy group. The diagnosis of O5G allergy can be clinically challenging, given the need for the presence of a co-factor for reactions to occur. We previously reported that the median time from symptom onset to diagnosis was 2 years, with a range of 1 month to 30 years.7 Conversely, peanut allergy is usually readily apparent, allowing avoidance strategies to be implemented rapidly. These clinical factors may explain the differing rates of allergic reaction prior to diagnosis.
O5G and peanut allergy both require the presence of IgE to the allergen which can activate the FcεRI IgE receptor on effector cells and provoke an allergic reaction. For peanut allergy, the amount of peanut exposure (“eliciting dose”) may vary between individuals but once this level of exposure is reached, a clinical reaction is to be expected. However, in O5G allergy, the interactions between gluten dose threshold, the exercise or other co-factor threshold, and the time-interval between the two, mean that the occurrence of an allergic reaction is less predictable. The mechanism by which the cofactors promote development of an allergic reaction is incompletely understood.
One challenge in managing O5G allergy lies in attempting to predict the interactions between gluten dose, the exercise threshold, and the time-interval between the two in real life.14 We previously reported that individuals with O5G allergy receive varying advice regarding management, and they often choose an approach different to the advice given.7 The requirement for a co-factor to be present in most cases of allergic reaction in the O5G allergy groups allows some dietary flexibility, and some patients with O5G allergy continue to include wheat/gluten in their diet.13 Christensen et al demonstrated a lower threshold to reaction during oral gluten challenge in completely wheat-avoidant patients compared to patients who included wheat in their diet. This suggests that total avoidance may, over time, heighten wheat sensitivity and consequently the risk of a reaction.15 Hence, the optimal dietary approach to manage O5G allergy remains unclear. Conversely, total avoidance of peanut is unequivocally the recommended approach, unless some form of disease-modifying therapy is instituted. Accordingly, we found that the factors that led to an allergic reaction differed between O5G allergy and peanut allergy, with accidental exposure more likely in those with peanut allergy (accidentally eaten, eating away from home), and deliberate ingestion or inadvertent exertion more likely in those with O5G allergy.
Even when successful management of food allergy (predominantly by avoidance of allergen) results in an absence of reactions, there remain nonetheless profound effects of food allergy on day-to-day living. We chose the FAQLQ-AF, a food-specific QOL questionnaire with excellent construct validity, to measure QOL in our cohort.6 We had expected poorer QOL among patients with O5G allergy compared to patients with peanut allergy, but this was not the case. The uncertainties around diagnosis and management of O5G allergy do not appear to cause greater QOL impairment by this measure. The FAQLQ-AF was developed for use in “conventional” IgE mediated food allergy rather than specifically FDEIA. It does not include questions related to co-factors or their avoidance, and so it remains possible that this tool is not able to detect distinct effects on QOL from these two different phenotypes of food allergy.
There are limited data on QOL effects of food allergy on adults, and almost none in Australia. A paediatric study by Dunn Galvin et al16 demonstrated improvement in a parent-scored QOL measure at 12 months following completion of probiotic-peanut oral immunotherapy treatment, with no corresponding improvement in the placebo group. The only other study in O5G allergy17 reported a total FAQLQ-AF score of 4.7 in 28 individuals in Wuhan with O5G allergy, similar to our cohort. It is always possible that the impact of staple food allergies on QOL may vary according to region and culture, so our QOL results add important data to the literature.
Across peanut allergy and O5G allergy as a whole, we found that the presence of additional food allergies and female sex both affected QOL. Results from other studies have been mixed. A Swedish study demonstrated that the presence of other atopic conditions, but not food allergies alone, increased QOL impairment; there was no sex difference.18 The Dutch study reporting the development and validation of the FAQLQ-AF6 found a correlation between additional food allergies and QOL, again with no sex difference. An American study found greater effects on QOL in adults whose food allergy presented in childhood, compared to those with onset in adulthood.19
There was a wide range for QOL impacts among individuals. Using the FAQLQ-AF questionnaire, the lowest possible score is 1 and highest is 7; there were some individuals within each domain and for each food allergen who scored at, or very close to, each end of the spectrum. It appears likely that such heterogeneity reflects multiple competing factors relevant to the patients themselves.
Our study has several limitations. Participant numbers were relatively small. Selection bias was possible given incomplete response rates. Participant responses were not verified by file review. Our estimate of reaction rates was based on patient recall of timelines and events, when prospective assessment of validated allergic reactions would be preferable. QOL was assessed at a single time-point, and measurements in O5G and peanut allergy may not be generalizable to other food allergies.
Conclusion
Compared to peanut allergy, O5G allergy is predominantly of adult onset and associated with lower rates of atopic co-morbidities including additional food allergies. These phenotypic differences suggest the probability of distinct aetiologies and pathogeneses between the two conditions. Different reaction triggers between the two conditions also call for distinct approaches to clinical management. According to our data, Australian adults with allergies to two key staple foods experience significant impacts on QOL, especially among women and those with additional food allergies.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lyons SA, Burney PGJ, Ballmer-Weber BK, et al. Food allergy in adults: substantial variation in prevalence and causative foods across Europe. J Allergy Clin Immunol. 2019;7(6):1920–1928.e11.
2. Kamdar T, Peterson S, Lau C, Saltoun C, Gupta R, Bryce PJ. Clinical communications: prevalence and characteristics of adult onset food allergy. J Allergy Clin Immunol Pract. 2015;3(1):114–115. doi:10.1016/j.jaip.2014.07.007
3. Baker MG, Sampson HA. Phenotypes and endotypes of food allergy: a path to better understanding the pathogenesis and prognosis of food allergy. Ann Allergy Asthma Immunol. 2018;120(s3):245–253. PMID: 29378246. doi:10.1016/j.anai.2018.01.027
4. Deschildre A, Lejeune S, Cap M, et al. Food allergy phenotypes: the key to personalized therapy. Clin Exp Allergy. 2017;47(9):1125–1137. PMID: 28710890. doi:10.1111/cea.12984
5. Sicherer SH, Sampson HA. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141(1):41–58. doi:10.1016/j.jaci.2017.11.003
6. Flokstra-de Blok BM, van der Meulen GN, DunnGalvin A, et al. Development and validation of the food allergy quality of life questionnaire - adult form. Allergy. 2009;64(8):1209–1217. PMID: 19210345. doi:10.1111/j.1398-9995.2009.01968.x
7. Zubrinich C, Puy R, O’Hehir R, Hew M. Evaluation of diagnosis and management of omega-5-gliadin allergy: a retrospective survey. J Asthma Allergy. 2021;14:397–403. doi:10.2147/JAA.S304444
8. Du Toit G, Roberts G, Sayre PH, et al; LEAP Study Team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803–813.
9. Vickery BP, Vereda A, Casale TB, et al; PALISADE Group of Clinical Investigators. AR101 oral immunotherapy for peanut allergy. N Engl J Med. 2018;379(21):1991–2001. PMID: 30449234. doi:10.1056/NEJMoa1812856
10. Tang ML, Ponsonby AL, Orsini F, et al. Administration of a probiotic with peanut oral immunotherapy: a randomized trial. J Allergy Clin Immunol. 2015;135(3):737–44.e8. PMID: 25592987. doi:10.1016/j.jaci.2014.11.034
11. Prickett SR, Voskamp AL, Phan T, et al. Ara h 1 CD4+ T cell epitope-based peptides: candidates for a peanut allergy therapeutic. Clin Exp Allergy. 2013;43(6):684–697. PMID: 23711131; PMCID: PMC3709139. doi:10.1111/cea.12113
12. Jones SM, Sicherer SH, Burks AW, et al; Consortium of Food Allergy Research. Epicutaneous immunotherapy for the treatment of peanut allergy in children and young adults. J Allergy Clin Immunol. 2017;139(4):1242–1252.e9. PMID: 28091362; PMCID: PMC8609774. doi:10.1016/j.jaci.2016.08.017
13. Kennard L, Thomas I, Rutlowski K, et al. A multicenter evaluation of diagnosis and management of omega-5 gliadin allergy (also known as wheat-dependent exercise-induced anaphylaxis) in 132 adults. J Allergy Clin Immunol Pract. 2018;6(6):1892–1897. doi:10.1016/j.jaip.2018.02.013
14. Le TA, Kindi AM, Tan JA, et al. The clinical spectrum of omega-5-gliadin allergy. Intern Med J. 2016;46(6):710–716. doi:10.1111/imj.13091
15. Christensen MJ, Eller E, Mortz CG, Brockow K, Bindslev-Jensen C. Clinical and serological follow-up of patients with WDEIA. Clin Transl Allergy. 2019;9:26. doi:10.1186/s13601-019-0265-8
16. Dunn Galvin A, Lloyd M, Hsiao K-C, Tang MLK; PPOIT-001 study team. Long-term benefit of probiotic peanut oral immunotherapy on quality of life in a randomized trial. J Allergy Clin Immunol Pract. 2021;9(12):4493–4495.e1. doi:10.1016/j.jaip.2021.07.047
17. Chen H, Huang N, Li WJ, et al. Clinical and laboratory features, and quality of life assessment in wheat dependent exercise-induced anaphylaxis patients from central China. J Huazhong Univ Sci Technol Med Sci. 2016;36(3):410–415. doi:10.1007/s11596-016-1601-z
18. Jansson SA, Heibert-Arnlind M, Middelveld RJ, et al. Health-related quality of life, assessed with a disease-specific questionnaire, in Swedish adults suffering from well-diagnosed food allergy to staple foods. Clin Transl Allergy. 2013;1(3):21. doi:10.1186/2045-7022-3-21
19. Patel GB, Kellner ES, Clayton E, et al. Quality of life is lower in adults labeled with childhood-onset food allergy than in those with adult-onset food allergy. Ann Allergy Asthma Immunol. 2021;127(1):70–75.e2. PMID: 33753218; PMCID: PMC8483056. doi:10.1016/j.anai.2021.03.009
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
