Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Perceptions and Knowledge of Public Towards Emerging Human Monkeypox in Yemen: A Cross-Sectional Study
Authors Halboup AM , Alzoubi KH , Abu-Farha RK , Harun SN , Al-Mohamadi A , Battah MM , Jaber AAS , Alkubati S , Al-Ashwal FY
Received 27 September 2023
Accepted for publication 22 November 2023
Published 30 November 2023 Volume 2023:16 Pages 3689—3701
DOI https://doi.org/10.2147/JMDH.S442296
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdulsalam M Halboup,1,2 Karem H Alzoubi,3,4 Rana K Abu-Farha,5 Sabariah Noor Harun,2 Ahmed Al-Mohamadi,1 Mohammed M Battah,1,2 Ammar Ali Saleh Jaber,6 Sameer Alkubati,7,8 Fahmi Y Al-Ashwal1,9
1Department of Clinical Pharmacy and Pharmacy Practice, University of Science and Technology, Sana’a, Yemen; 2Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia; 3Department of Pharmacy Practice and Pharmacotherapeutics, College of Pharmacy, University of Sharjah, Sharjah, United Arab Emirates; 4Department of Clinical Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 5Department of Clinical Pharmacy and Therapeutics, Faculty of Pharmacy, Applied Science Private University, Amman, 11931, Jordan; 6Department of Clinical Pharmacy & Pharmacotherapeutics, Dubai Pharmacy College for Girls, Dubai, United Arab Emirates; 7Department of Nursing, Faculty of Medicine and Health Sciences, Hodeidah University, Hodeidah, Yemen; 8Department of Medical Surgical Nursing, College of Nursing, University of Hail, Hail, Saudi Arabia; 9Department of Clinical Pharmacy, College of Pharmacy, Al-Ayen University, Thi-Qar, Iraq
Correspondence: Abdulsalam M Halboup, Department of Clinical Pharmacy and Pharmacy Practice, University of Science and Technology, Sana’a, Yemen, Tel +967774960247, Email [email protected]
Background: The spread of monkeypox (mpox) worldwide poses a severe threat to human life. This virus leads to a disease with symptoms similar to smallpox in humans. To combat this threat, improving public knowledge and perception toward mpox is vital for public health preventive measures.
Methods: A cross-sectional survey was carried out in Yemen from December 2022 to March 2023 to investigate public perception and knowledge of mpox. Individuals were approached through social media platforms using a convenient sampling approach. Linear regression was used to determine the association between participants’ knowledge (dependent variable) and explanatory variables.
Results: A total of 853 individuals consented to take part in the study. A significant proportion of respondents had a low knowledge level (N=572, 67.06%). Most participants knew about the nature of the diseases (75%, n=641), transmission mode (78.1%, n=668), hand sanitizer preventive measures, and skin- related symptoms. However, only 20.8% (n= 178) knew that diarrhea is not a symptom, and 25.4% (n= 217) knew antibiotics are unnecessary for mpox management. A proportion of 57.7% (n=492) of the participants feared human mpox, and 47.7% (n= 407) thought it was a conspiracy. Most participants had a good perception of local and international health authorities controlling the disease. Age, education level, having a health-related certificate, and receiving a 2-dose vaccination for COVID-19 had statistically significant associations with mpox knowledge level (P < 0.05). Social media platforms were the most often used information source about mpox (78.3%, n= 668), followed by articles (41.1%, n=351).
Conclusion: The study reveals a low public knowledge about mpox in Yemen, emphasizing the need for targeted educational campaigns, especially via social media, to strengthen public health measures and disease control. Addressing Knowledge gaps and correcting misconceptions is crucial for improving preparedness and response to the disease.
Keywords: monkeypox virus, public knowledge, public perception, outbreak, Yemen
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Fikri has been published for this article.
Introduction
Human monkeypox (mpox) is a viral infection transmitted from animals to humans. The virus belongs to the Orthopoxvirus genus of the Poxviridae family, including the variola virus that causes smallpox.1 The disease is typically self-limited, but in rare cases, it can lead to severe illness and even death.2 The symptoms of mpox are similar to smallpox, such as fever, chills, headache, muscle aches, and a rash that begins on the face and spreads to other parts of the body.3–5 However, lymphadenopathy, which is the swelling of lymph nodes, is a characteristic feature of mpox but not smallpox.6
Although mpox is similar to smallpox, it is generally milder and has a lower mortality rate. In mild cases, the skin lesions are only limited to the extremities. However, in severe cases of mpox, skin lesions can spread to various body parts, including the mouth, cornea, and genitals. Such severe cases still occur, particularly in individuals with weakened immune systems or those with underlying health conditions. The incubation period ranges from 5 to 21 days, with symptoms persisting for up to four weeks.7–9
Transmission of mpox occurs through close contact with infected animals and person-to-person contact involving skin lesions, respiratory secretions, and contaminated objects. Additionally, the transmission of mpox from humans to dogs highlights the potential for infected individuals to pass the virus to susceptible animals, posing additional challenges in preventing transmission from humans to pets and vice versa.10,11 Moreover, maternal-fetal transmission is possible.12,13 Interestingly, men who have sex with men (MSM) experienced the highest prevalence during the recent outbreak.14
During the early days of May 2022, the sudden rise in mpox cases outside endemic regions, including Europe and North America prompted global health concerns,15 leading the Director-General of the World Health Organization (WHO) to declare a global mpox outbreak as a Public Health Emergency of International Concern on July 23, 2022.16 By November 18, 2022, there were 86,956 confirmed cases and 119 deaths across 110 countries, the majority (85,502 case) occurred in non-endemic countries.17 The mutations in the genome of the Mpox-2022 strains might have influenced their virulence and pathogenesis, leading to heightened transmission dynamics and the capacity to spread to non-endemic geographical regions.18,19
Effective control of mpox transmission relies heavily on public knowledge and compliance with preventive measures. Thus, improving public understanding of symptoms, transmission, and preventive measures is crucial.20,21
In Yemen, the fragile health system and political instability pose significant challenges to the implementation of the International Health Regulations during disease outbreaks.22 The strategic location, serves as the northern entrance to the Indian Ocean, connecting with African and Asian markets, exposes it to the potential spread of mpox.23 This vulnerability is amplified by the continuous arrival of migrants and refugees from the Horn of Africa, area where mpox is endemic.24
Despite of the current political instability, ongoing civil war, and fragile healthcare system in Yemen, it is imperative to assess public knowledge and perception of mpox. This assessment is critical since public engagement effective preventive measures is significantly influenced by their understanding and perception of the disease. Furthermore, gaining insight into the public’s knowledge and perception is essential for identifying gaps and implementing appropriate preventive measures against human mpox. Therefore, this study aimed to investigate the overall knowledge and perceptions of the general population in Yemen about human mpox.
Materials and Methods
Study Design and Participants
This cross-sectional study used a pre-validated online survey with slight modifications.25 The study was conducted in Arabic to guarantee that all participants could comprehended the questions. To achieve this, two investigators proficient in both English and Arabic performed a forward-backward translation of the survey to compare the Arabic version with the original English version. After resolving any disparities between the translations, the final Arabic version of the tool was prepared. Subsequently, the participants were invited to participate in the survey using social media platform. Inclusion criteria were Yemeni participants with access to social media platforms. Participation in the study was voluntary, and all respondents provided informed consent.
Sample Size Determination
The sample size was estimated using Daniel’s formula:26 n = P × (1-P) × z2/d2, where n is the sample size, z = 1.96 at 95% confidence level, d (0.05) is the margin of error, P (0.5) is a prevalence estimate. The minimum required sample size was 384 participants.
Study Tool
A pre-validated questionnaire was used, which underwent slight modification on some demographic variables to suit the study’s setting (Supplementary File). The questionnaire was created using Google Forms and included information regarding the research background, study objectives, confidentiality assertion, and voluntary participation. The questionnaire was divided into four sections. The first section gathered participants’ sociodemographic data and their past medical history. The second section evaluated participants’ fear of human mpox and their vaccination history. Respondent’s awareness of mpox and the source of their information was assessed in the third section. A 3-point Likert scale (no, yes, and do not know) was used for this section. Correct answers received a score of 1, while “I don’t know” or incorrect responses received a score of 0. The overall knowledge score was calculated out of 15. The fourth section evaluated participants’ perception of human mpox using a 5-point Likert scale, ranging from 5 (strongly agree) to 1 (strongly disagree). The overall knowledge score was classified into high (12–15, 80–100%), moderate (9–11, 60–79%), and low knowledge scores (0–8, ≤ 59.0%) using Bloom’s cut-off point.27
Data Collection
This study was conducted in Yemen from December to March 2023. Social media platforms (WhatsApp and Facebook) were employed for participants recruitment. The questionnaire hyperlink was shared, along with instructions outlining the study’s objectives, expected completion time, and anonymity assurance. Participants were encouraged to share the questionnaire within their social networks. Regular follow-up efforts throughout the data collection process were maintained to ensure a broad representation of various sectors and groups within Yemeni society.
At the first page of the study, a written participant consent statement was provided, stating that “Your participation in completing this questionnaire is highly appreciated”. If the participants were willing to proceed with the study, they provided their informed consent to volunteer by selecting “agree to participate” and completing the survey. If they were not willing, they chose “disagree to participate”.
Ethical approval was obtained from the ethical committee at the University of Science and Technology, Sana’a, Yemen (Ref. No.: EAC/UST239). This study complies with the Declaration of Helsinki.
Statistical Analysis
Data was downloaded from Google Forms as excel sheet then imported into IBM SPSS statistics version 27.0 (IBM Corp., Armonk, NY, USA) and subsequently coded and labeled. Categorical variables were presented as frequency and percentage. Normal distribution for continuous data was assessed using the Kolmogorov–Smirnov test. The overall knowledge of the participants about mpox exhibited a non-normally distributed pattern (P value ≤ 0.05). Therefore, it was displayed as median and interquartile range. Univariate and multivariate linear regressions were employed to assess the association between participants’ overall knowledge about human mpox and their sociodemographic data. Predictors with p-value < 0.25 in univariate linear regression were entered into multivariate linear regression. The absence of multicollinearity between independent variables was checked using the Pearson correlation and confirmed at r < 0.9. A p-value of < 0.05 was considered a significant difference.
Results
Participants’ Sociodemographic Data
In this study, 895 individuals were approached during the study period. Of them, 42 participants disagreed to provide their informed consent and did not fill out the survey. Thus, 853 participants agreed to participate and filled out the survey. As shown in Table 1, the respondents had a median age of 23 years (IQR= 7), and a significant portion of them were male (60.5%, n=516), university students (59.3%, n = 505). Most of the participants were not married (68%, n= 580), unemployed (72.1%, n= 615), and had less than 150,000 YR as a monthly income (78.5%, n = 670). The majority of the participants were from Sana’a (61.4%, n= 524), had no children (72.6%, n= 619), reported having no chronic disease (90.6%, n = 773), and had no health-related certificate (60.7%, n= 518).
 |
Table 1 Sociodemographic Data of the Participants (N=853) |
Participants’ Level of Fear of Human Mpox
Respondents’ awareness and fear of mpox transmission were reported in Table 2. Only 13.2% of the respondents claimed that cases of mpox infection were reported in Yemen. A proportion (47.7%, n= 407) of the participants thought there was a conspiracy surrounding human mpox transmission. Over half of the respondents (57.7%, n= 492) were afraid of mpox, and less than half (46.8%, n= 393) reported being afraid of visiting friends or family members due to human mpox. Additionally, 47.4% of the respondents (n= 404) feared traveling to certain countries due to the disease. The majority (72.3%, n = 617) suggested that health authorities launch a vaccination campaign against human mpox infection.
 |
Table 2 Public Awareness and Fear of Human Mpox Transmission (N = 853) |
Participants’ Knowledge About Human Mpox
The respondents’ knowledge about mpox infection was also analyzed and shown in Table 3. The overall median score of participants’ knowledge was 7 out of 15 and an interquartile range of 6. Based on the Bloom’s cut-off points, 572 (67.06%), 212 (24.85%), and 69 (8.09%) of the participants had low, moderate, and high knowledge levels, respectively. The majority of the respondents (75%, n=668) accurately identified that a virus causes the disease. Concerning disease transmission, the majority (78.1%, n=668) recognized that it could be spread from an infected person to others, while less than half (41.9%, n=385) knew it could be transmitted through a monkey bite. Additionally, over half of the respondents (55.6%, n=475) knew that the disease could affect both genders but not exclusively males.
 |
Table 3 Respondents’ Knowledge About Mpox Infection (N = 853) |
In terms of recognizing the symptoms of mpox, only a small proportion of participants (23.7%, n=203) were aware that it shares the same symptoms as smallpox. A higher percentage (34.9%, n=298) recognized that flu-like syndrome could be an early sign of the disease, while the majority recognized skin rash (63.4%, n=542) and vesicles on the skin (51.9%, n=444) as signs of human mpox. However, only 32.6% (n=279) knew that lymphadenopathy could be used to differentiate between smallpox and mpox. Regarding preventive measures, while 56.5% (n=483) recognized the importance of hand sanitizers and face masks, only 38.7% (n=331) correctly identified bodily fluids as the mode of transmission for mpox. Additionally, 25.8% (n=221) knew that childhood immunization does not protect against human mpox. Notably, only 20.8% (n=178) and 25.4% (n=217) of respondents knew that diarrhea is not a symptom of the disease and that antibiotics are ineffective in treating mpox, respectively.
Regarding mpox information sources, the majority of respondents (78.3%, n= 668) reported social media as the primary information source for mpox, followed by articles (41.1%, n=351) and family and friends (34.2%, n = 292). Healthcare professionals, on the other hand, were reported as being the least utilized source for information (25.6%, n =218), as shown in Figure 1.
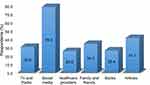 |
Figure 1 Source of Information about Mpox. |
Participants’ knowledge about human mpox was also analyzed and reported in Table 3. The overall median score of participants’ knowledge was low, with a median of 7 out of 15 and an interquartile range of 6. The majority of the participants (75%, n=668) correctly identified that the disease is caused by a virus. Concerning disease transmission, the majority (78.1%, n=668) recognized that it could be spread from an infected person to others, while less than half (41.9%, n=385) knew it could be transmitted through a monkey bite. Additionally, more than half of the participants (55.6%, n=475) knew that the disease could affect both genders but not exclusively males.
In terms of recognizing the symptoms of mpox, only a small proportion of participants (23.7%, n=203) were aware that it shares the same symptoms as smallpox. A higher percentage (34.9%, n=298) recognized that flu-like syndrome could be an early sign of the disease, while the majority recognized skin rash (63.4%, n=542) and vesicles on the skin (51.9%, n=444) as signs of human mpox. However, only 32.6% (n=279) knew that lymphadenopathy could be used to differentiate between smallpox and mpox. Regarding preventive measures, while 56.5% (n=483) recognized the importance of hand sanitizers and face masks, only 38.7% (n=331) correctly identified bodily fluids as the mode of transmission for mpox. Additionally, 25.8% (n=221) were aware that the vaccination received during childhood does not protect against human mpox. Finally, only 20.8% (n=178) and 25.4% (n=217) of respondents correctly identified that diarrhea is not a disease symptom and that antibiotics are ineffective in treating mpox, respectively.
Regarding the source of information about mpox, the majority of the respondents (78.3%, n= 668) reported social media as their primary source of information, followed by articles (41.1%, n=351), and family and friends (34.2%, n = 292). In contrast, healthcare providers were reported as the least frequently used source of information (25.6%, n =218), as shown in Figure 1.
Participants’ Perception Toward Human Mpox
Participants’ perceptions regarding human mpox were also examined and reported in Table 4. The majority of respondents (80.4%, n=686) agreed that global control of mpox is possible, while 51.1% (n=436) believed that the Yemeni Ministry of Health and the local population could control the disease locally. More than half (59.4%, n=507) of the participants believed that mpox would have socio-economic impacts similar to COVID-19, and most of them (82.3%, n=702) thought that the disease could put an additional burden on affected countries’ healthcare systems. Despite 77.5% (n=661) of participants expressing an interest in learning more about mpox, 64.8% (n=553) believed that traveling to a country with an mpox epidemic is dangerous. Furthermore, 85.5% (n=729) of the respondents recognized the importance of reporting mpox symptoms to local health authorities for disease prevention, and 85.1% (n=726) believed that the vaccine for mpox should be provided for free.
 |
Table 4 Perception About Human Mpox (N = 853) |
Factors Associated with Participants’ Knowledge of Mpox
The study also examined the relationship between socioeconomic factors and participants’ knowledge about mpox (Table 5). Univariate linear regression analysis showed that education level (Beta = 0.174, P < 0.001), marital status (Beta = 0.090, P = 0.009), having children (Beta = 0.109, P = 0.001), having a health certificate (Beta = 0.237, P < 0.001), age (Beta = −0.119, P < 0.001), and receiving two doses of COVID-19 vaccine (Beta = 0.139, P < 0.001) were significantly associated with participants’ knowledge about mpox. However, the multivariate linear regression analysis revealed that only education (Beta = 0.111, P= 0.001), having a health certificate (Beta = 0.237, P < 0.001), age (Beta = −0.104, P =0.034), and receiving two doses of COVID-19 vaccine (Beta = 0.088, P = 0.010) were significantly associated with respondents’ knowledge level of mpox.
 |
Table 5 Factors Associated with Participants’ Knowledge About Mpox |
Discussion
The human mpox outbreak has spread rapidly worldwide, with a spike in confirmed and suspected cases, which WHO regards as an emergency.28 This has necessitated empirical research to determine if different populations understand the implication of the disease. The majority of participants in this study were male, university students, unmarried, unemployed, earned <150,000, resided in Sana’a, had no children, had no chronic disease, and had no health-related certificate. This study found that the participants have a poor level of knowledge regarding the epidemiology of mpox in terms of the symptoms and transmission, even though this information is crucial to improving response to the high human mpox incidence.
In Yemen, the scenario of mpox is obscure, like the situation of COVID-19. This situation may be attributed to the ongoing war, closure of the airports, and political instability, so the spread of mpox in Yemen seems relatively mild or underreported. Therefore, only 13.2% of the current study participants reported cases in Yemen.29 A proportion of 47.7% of the participants in this study believed that mpox transmission is a conspiracy. This finding is expected since the emergence of frequent infectious diseases was associated with unusual conspiracy theories that could spread quicker than the actual disease due to the effect of different social media platforms and the political conflict we live in today.30,31 The same situation was encountered during the COVID-19 and Ebola outbreaks.32,33 Several studies from Arab countries, including Kuwait,34 Jordan,25,35 and Lebanon36 reported firm conspiracy beliefs regarding human mpox. Although the ideas in conspiracy theory seem harmless, its potential negative consequences have been reported, particularly regarding health-related decisions like vaccine hesitancy and a lack of trust in scientific and medical institutions.37,38 Also, those who believe in this theory tend not to take preventive measures.39 This study found that more than half of the respondents exhibited fear of mpox, and approximately half feared traveling to foreign countries or visiting other people to avoid contracting the disease. More than two-thirds of the respondents in the present study recommend that healthcare authorities start the vaccination campaign. This high proportion may reflect the anxiety and fear from the spread of mpox. Evidence from previous studies has shown that pandemics and epidemics often induce fear in society and lead to restrictions on their activities.40,41 In Iraqi Kurdistan42 and Jordan,25 there were reports of fear and anxiety related to the spread of mpox. However, in Saudi Arabia, human mpox was viewed as less concerning compared to COVID-19.43
In the present study, the majority of participants had a low level of knowledge. Knowledge of the public about human mpox was evaluated in different countries and reported similar findings. For instance, studies from Saudi Arabia, Jordan, and Italy revealed that the overall public knowledge regarding mpox was low, and over half of the participants had a poor knowledge level about the disease.25,44,45 Low knowledge about mpox is concerning because involving the public is vital for successfully implementing preventative measures to control and treat possible outbreaks. When comparing human mpox to other viral infections, it has been reported that individuals from Yemen have a good understanding of the COVID-19 nature and seasonal influenza virus, as well as their susceptibility to complications.46,47 In the current study, more than two-thirds of the respondents knew that the nature of the disease and an infected individual could transmit the disease to others. A similar finding was obtained from a study undertaken in Nigeria, showing that most participants were aware of the mpox causative pathogen and methods to prevent it. Nonetheless, most participants lacked awareness about how the disease is transmitted, its symptoms, complications, and the existence of a vaccine.20 The majority of individuals in this study accurately identified the skin-related symptoms of mpox, including skin rashes and vesicles. These results align with previous studies that also demonstrated high accuracy in recognizing skin-related symptoms.35,44 Their familiarity with these signs and symptoms may result from the visual learning approach they have gained through watching television and other visual social media. On the other hand, only less than a quarter of respondents correctly identified that diarrhea is not associated with human mpox. Also, a quarter of them correctly recognized that antibiotics are unnecessary to treat human mpox. Similar findings were also obtained among the public in Jordan25 and healthcare workers in Lebanon.36 The conflict of data regarding the use of antibiotics during the COVID-19 pandemic48 and the public perception of self-medication with antibiotics in the middle east49,50 could potentially influence participants’ knowledge of using antibiotics in the current study.
Regarding the association between the overall knowledge about mpox and the participants’ sociodemographic data, participants with younger age, higher education, or those who have a health certificate and those who had not received the COVID-19 vaccination, had higher knowledge scores. This outcome was predictable, as individuals with healthcare certificates are often highly educated, and those at a university level are typically younger and have not yet received the vaccination, which suggests that they are likely to be educated. These populations are expected to have reliable access to information, are engaged in reading scientific publications, and possess the skills to assess information resources and make informed decisions about their quality. Similar findings were also obtained in a recent survey conducted in Saudi Arabia and Lebanon, where participants with higher education levels or healthcare workers had a higher knowledge score about mpox.36,44 Also, a study conducted in Nigeria reported that occupation, education level, and age are the factors that have an impact on knowledge about mpox.20
In the current study, the social media platform emerged as the primary information source regarding human mpox. A similar finding was also reported from recent studies in Jordan,25 the Kurdistan region of Iraq,42 Saudi Arabia,44 and Philippines.51 The growing dependence on social media as a source of medical information is a concern. Health authorities need to acknowledge and tackle this issue as these platforms are not usually trustworthy sources for health-related information. The trend of relying on social media for health-related information was brought during the COVID-19 pandemic, when the lockdowns led many individuals to rely on social media and the internet for information.30 Therefore, it is essential to promote awareness among the public about the potential risks of relying solely on social media for health-related information and encourage the use of credible sources of information, such as healthcare providers and official government websites. The current study showed that reading articles was the second most frequent source of obtaining information about mpox. This finding may be explained by the fact that the majority of the respondents were university students, and they were familiar with this source of information.
In Yemen, healthcare system has confronted numerous challenges for more than a decade, including insufficient funding, substandard infrastructure, a shortage of qualified personnel, political instability, and conflicts. These obstacles have significantly impaired Yemen’s healthcare systems, resulting in suboptimal preparedness and response to newly emerging diseases, such as the current mpox outbreak. In a recent study conducted among healthcare workers in several countries in the middle east, including Yemen, revealed that the majority of healthcare professionals have a moderate knowledge about mpox virus.52 Therefore, Increased knowledge regarding mpox infections among healthcare workers is crucial. This can be addressed by incorporating information on emerging and re-emerging zoonoses into the routine professional continuing education for health professionals. Additionally, the integration of newly developed diagnostic methods, such as those utilizing deep learning, holds great promise for image-based diagnosis. This contributes significantly to the early and accurate detection of mpox skin lesions.53
The majority of respondents in the present study showed high levels of confidence in the ability of the general public and the local health authorities to control human mpox, even though it would negatively impact the economy. This confidence could have stemmed from the firsthand experience during the COVID-19 pandemic, where the World Health Organization (WHO) and health authorities have gained significant empowerment over the last three years.22,46 The study participants emphasized the importance of taking preventative measures to manage this outbreak, such as reporting symptoms to health authorities, avoiding traveling to epidemic countries, increasing knowledge, and getting vaccinated. In addition, recent studies reported similar findings.25,47
Study Strengths and Limitations
This study is the first to assess the perception and knowledge regarding mpox among the general population in Yemen. The outcomes of the present research could have considerable implications for formulating and implementing policies and intervention strategies aimed at preventing and managing emerging infectious diseases. The study revealed significant gaps in knowledge and the prevalence of unreliable sources of information that the majority of people in Yemen rely on for information about human mpox. These findings emphasize the need for awareness campaigns targeting the general population in Yemen to enhance their understanding of the disease and promote the use of reliable sources of information. However, the current study had several limitations, including the sampling approach, which may have provided unequal opportunities for participants and favored those with internet access. Additionally, the online survey was biased toward younger generations residing in Sana’a, which may not represent the entire Yemeni population. Furthermore, the current study was also vulnerable to desirability bias, whereby participants may have answered questions based on what they believed others expected of them.
Conclusion
The study revealed that the general public in Yemen had insufficient knowledge about the mpox disease, including its symptoms, preventive measures, and treatment with a good perception of local and international health authorities in controlling the emerging mpox. Individuals with younger ages, higher education, and those holding health certificates tended to have better knowledge, indicating that reliable information is essential for acquiring accurate knowledge. Furthermore, a significant proportion of the participants belief in conspiracy theories regarding mpox outbreaks. This widespread belief in conspiracy theories could have detrimental consequences, potentially impeding community efforts to implement effective preventive measures against human mpox. Social media is the primary source of information about human mpox among public. Therefore, there is an opportunity to use this platform for disseminating accurate information, mitigating the risk associated with conspiracy theory. The implementation of educational campaigns aimed at addressing knowledge gaps and correcting public misconceptions becomes crucial for enhancing preparedness and facilitating an efficient response to the disease. Future studies should address the limitations of this study when designing research on human mpox.
Acknowledgments
We are grateful to all individuals who have made valuable contributions to this study.
Disclosure
The authors report no conflicts of interest in this work
References
1. Smith GL, McFadden G. Smallpox: anything to declare? Nat Rev Immunol. 2002;2(7):521–527. doi:10.1038/nri845
2. Benites-Zapata VA, Ulloque-Badaracco JR, Alarcon-Braga EA, et al. Clinical features, hospitalisation and deaths associated with monkeypox: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob. 2022;21(1):36. doi:10.1186/s12941-022-00527-1
3. Shariq A, Rasheed Z, Abdulmonem WA. Human monkeypox: an update on knowledge and future implications. Int J Health Sci. 2022;16(4):1–2.
4. Liu Q, Fu L, Wang B, et al. Clinical Characteristics of Human Mpox (Monkeypox) in 2022: a Systematic Review and Meta-Analysis. Pathogens. 2023;12(1):146. doi:10.3390/pathogens12010146
5. Alshahrani NZ, Algethami MR, Alarifi AM, et al. Knowledge and Attitude Regarding Monkeypox Virus among Physicians in Saudi Arabia: a Cross-Sectional Study. Vaccines. 2022;10(12):2099. doi:10.3390/vaccines10122099
6. Jairoun AA, Al-Hemyari SS, Abdulla NM, et al. Awareness and preparedness of human monkeypox outbreak among university student: time to worry or one to ignore? J Infect Public Health. 2022;15(10):1065–1071. doi:10.1016/j.jiph.2022.08.015
7. McCollum AM, Damon IK. Human monkeypox. Clin Infect Dis. 2014;58(2):260–267. doi:10.1093/cid/cit703
8. Petersen E, Kantele A, Koopmans M, et al. Human Monkeypox: epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect Dis Clin North Am. 2019;33(4):1027–1043. doi:10.1016/j.idc.2019.03.001
9. Huhn GD, Bauer AM, Yorita K, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin Infect Dis. 2005;41(12):1742–1751. doi:10.1086/498115
10. Seang S, Burrel S, Todesco E, et al. Evidence of human-to-dog transmission of monkeypox virus. Lancet (London, England). 2022;400(10353):658–659. doi:10.1016/S0140-6736(22)01487-8
11. Mohapatra RK, Mishra S, Kandi V, et al. Monkeypox plays a similar role like SARS-CoV-2; intensive animal screening is crucial after the first human-to-dog transmission report - Correspondence. Int J Surg. 2022;106:106925. doi:10.1016/j.ijsu.2022.106925
12. Beeson A, Styczynski A, Hutson CL, et al. Mpox respiratory transmission: the state of the evidence. Lancet Microbe. 2023;4(4):e277–e283. doi:10.1016/S2666-5247(23)00034-4
13. Pan D, Nazareth J, Sze S, et al. Transmission of monkeypox/mpox virus: a narrative review of environmental, viral, host, and population factors in relation to the 2022 international outbreak. J Med Virol. 2023;95(2):e28534. doi:10.1002/jmv.28534
14. Petersen E, Zumla A, Hui D, et al. Vaccination for monkeypox prevention in persons with high-risk sexual behaviours to control on-going outbreak of monkeypox virus clade 3. Int J Infect Dis. 2022;122:569–571. doi:10.1016/j.ijid.2022.06.047
15. Girometti N, Byrne R, Bracchi M, et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis. 2022;22(9):1321–1328. doi:10.1016/S1473-3099(22)00411-X
16. Lancet T. Monkeypox: a global wake-up call. Lancet (London, England). 2022;400(10349):337. doi:10.1016/S0140-6736(22)01422-2
17. CDC. 2022 Mpox Outbreak Global Map. 2022; Available from: https://www.cdc.gov/poxvirus/mpox/response/2022/world-map.html.
18. Wang L, Shang J, Weng S, et al. Genomic annotation and molecular evolution of monkeypox virus outbreak in 2022. J Med Virol. 2023;95(1):e28036. doi:10.1002/jmv.28036
19. Mohapatra RK, Kandi V, Seidel V, et al. Monkeypox lineages amid the ongoing COVID-19 pandemic: a global public health concern - Correspondence. Int J Surg. 2022;107:106968. doi:10.1016/j.ijsu.2022.106968
20. Awoyomi OJ, Njoga EO, Jaja IF, et al. Mpox in Nigeria: perceptions and knowledge of the disease among critical stakeholders—Global public health consequences. PLoS One. 2023;18(3):e0283571. doi:10.1371/journal.pone.0283571
21. Lulli LG, Baldassarre A, Mucci N, Arcangeli G. Prevention, Risk Exposure, and Knowledge of Monkeypox in Occupational Settings: a Scoping Review. Trop Med Infect Dis. 2022;7(10):276. doi:10.3390/tropicalmed7100276
22. Dureab F, Al-Awlaqi S, Jahn A. COVID-19 in Yemen: preparedness measures in a fragile state. The Lancet Public Health. 2020;5(6):e311. doi:10.1016/S2468-2667(20)30101-8
23. Raga AA. The Bab el-Mandeb strait: geopolitical considerations of the strategic chokepoint. Ieee Es Opinion Paper. 2020.
24. McCollum AM, Shelus V, Hill A, et al. Epidemiology of Human Mpox - Worldwide, 2018-2021. MMWR Morb Mortal Wkly Rep. 2023;72(3):68–72. doi:10.15585/mmwr.mm7203a4
25. Abu-Farha RK, Alzoubi KH, Mukattash TL, Alkhawaldeh R, Barakat M, Thiab S. Public Knowledge and Perceptions about the Emerging Human Mpox in Jordan: a Cross-Sectional Study. Trop Med Infect Dis. 2023;8(1):41. doi:10.3390/tropicalmed8010041
26. Daniel WW, Cross CL. Biostatistics: A Foundation for Analysis in the Health Sciences. Wiley; 2018.
27. Suaidi MT, Wong PK, Mohd Tahir NA, Chua EW. Community pharmacists’ knowledge, attitude, and practice in providing self-care recommendations for the management of premenstrual syndrome. Medicina. 2020;56(4):181. doi:10.3390/medicina56040181
28. Meo SA, Jawaid SA. Human monkeypox: fifty-two years based analysis and updates. Pak J Med Sci. 2022;38(6):1416. doi:10.12669/pjms.38.6.6775
29. WHO. World faces big challenges over Covid, monkeypox and wars - WHO. 2023; Available from: https://www.bbc.com/news/health-61546199.amp.
30. Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. 2020;27(3). doi:10.1093/jtm/taaa031
31. Douglas KM, Uscinski JE, Sutton RM, et al. Understanding conspiracy theories. Polit Psychol. 2019;40(S1):3–35. doi:10.1111/pops.12568
32. Sell TK, Hosangadi D, Trotochaud M. Misinformation and the US Ebola communication crisis: analyzing the veracity and content of social media messages related to a fear-inducing infectious disease outbreak. BMC Public Health. 2020;20(1):1–10. doi:10.1186/s12889-020-08697-3
33. Sallam M, Dababseh D, Yaseen A, et al. Conspiracy beliefs are associated with lower knowledge and higher anxiety levels regarding COVID-19 among students at the University of Jordan. Int J Environ Res Public Health. 2020;17(14):4915. doi:10.3390/ijerph17144915
34. Alsanafi M, Al-Mahzoum K, Sallam M. Monkeypox Knowledge and Confidence in Diagnosis and Management with Evaluation of Emerging Virus Infection Conspiracies among Health Professionals in Kuwait. Pathogens. 2022;11(9):994. doi:10.3390/pathogens11090994
35. Sallam M, Al-Mahzoum K, Dardas LA, et al. Knowledge of human monkeypox and its relation to conspiracy beliefs among students in Jordanian health schools: filling the knowledge gap on emerging zoonotic viruses. Medicina. 2022;58(7):924. doi:10.3390/medicina58070924
36. Malaeb D, Sallam M, Salim NA, et al. Knowledge, Attitude and Conspiracy Beliefs of Healthcare Workers in Lebanon towards Monkeypox. Trop Med Infect Dis. 2023;8(2):81. doi:10.3390/tropicalmed8020081
37. Sallam M, Dababseh D, Eid H, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. doi:10.3390/vaccines9010042
38. van Mulukom V, Pummerer LJ, Alper S, et al. Antecedents and consequences of COVID-19 conspiracy beliefs: a systematic review. Soc Sci Med. 2022;301:114912. doi:10.1016/j.socscimed.2022.114912
39. Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Soc Sci Med. 2020;263:113356. doi:10.1016/j.socscimed.2020.113356
40. Shevlin M, McBride O, Murphy J, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6):e125. doi:10.1192/bjo.2020.109
41. Abuhammad S, Khabour OF, Alomari MA, Alzoubi KH. Depression, stress, anxiety among Jordanian people during COVID-19 pandemic: a survey-based study. Inform Med Unlocked. 2022;30:100936. doi:10.1016/j.imu.2022.100936
42. Ahmed SK, Abdulqadir SO, Omar RM, et al. Knowledge, Attitude and Worry in the Kurdistan Region of Iraq during the Mpox (Monkeypox) Outbreak in 2022: an Online Cross-Sectional Study. Vaccines. 2023;11(3):610. doi:10.3390/vaccines11030610
43. Temsah M-H, Aljamaan F, Alenezi S, et al. Monkeypox caused less worry than COVID-19 among the general population during the first month of the WHO Monkeypox alert: experience from Saudi Arabia. Travel Med Infect Dis. 2022;49:102426. doi:10.1016/j.tmaid.2022.102426
44. Alshahrani NZ, Alzahrani F, Alarifi AM, et al. Assessment of knowledge of monkeypox viral infection among the general population in Saudi Arabia. Pathogens. 2022;11(8):904. doi:10.3390/pathogens11080904
45. Gallè F, Bianco L, Da Molin G, et al. “Monkeypox: what Do You Know about That?” Italian Adults’ Awareness of a New Epidemic. Pathogens. 2022;11(11):1285. doi:10.3390/pathogens11111285
46. Halboup AM, Alzoubi KH, Khabour OF, et al. Public Perception Toward COVID-19 Disease Nature, Susceptibility to Complication, and Relationship to Influenza: a Cross-Sectional Study from Yemen. J Multidiscip Healthc. 2023;16:707–716. doi:10.2147/JMDH.S399405
47. Ahmed WS, Abu Farha R, Halboup AM, et al. Knowledge, attitudes, perceptions, and practice toward seasonal influenza and its vaccine: a cross-sectional study from a country of conflict. Front Public Health. 2023;11:1030391. doi:10.3389/fpubh.2023.1030391
48. Granata G, Schiavone F, Pipitone G, Taglietti F, Petrosillo N. Antibiotics Use in COVID-19 Patients: a Systematic Literature Review. J Clin Med. 2022;11(23):7207. doi:10.3390/jcm11237207
49. Jamhour A, El-Kheir A, Salameh P, Hanna PA, Mansour H. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control. 2017;45(4):384–388. doi:10.1016/j.ajic.2016.11.026
50. Ibrahim D, Halboup A. Self-medication Practice among Health Sciences Undergraduate Students in Sana’a City-Yemen. Int J Pharm Investigation. 2019;9(2):80–84. doi:10.5530/ijpi.2019.2.16
51. Berdida DJE. Population‐based survey of human monkeypox disease knowledge in the Philippines: an online cross‐sectional study. J Adv Nurs. 2023;79(7):2684–2694. doi:10.1111/jan.15635
52. Swed S, Alibrahim H, Bohsas H, et al. A multinational cross-sectional study on the awareness and concerns of healthcare providers toward monkeypox and the promotion of the monkeypox vaccination. Front Public Health. 2023;11:1153136. doi:10.3389/fpubh.2023.1153136
53. Pal M, Mahal A, Mohapatra RK, et al. Deep and Transfer Learning Approaches for Automated Early Detection of Monkeypox (Mpox) Alongside Other Similar Skin Lesions and Their Classification. ACS omega. 2023;8(35):31747–31757. doi:10.1021/acsomega.3c02784
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
