Back to Journals » Risk Management and Healthcare Policy » Volume 15
Patient and Staff Satisfaction and Experience While Transforming Health Center Systems
Authors Whelihan K , Modica C , Bay RC, Lewis JH
Received 24 May 2022
Accepted for publication 31 October 2022
Published 11 November 2022 Volume 2022:15 Pages 2115—2124
DOI https://doi.org/10.2147/RMHP.S375983
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Kate Whelihan,1 Cheryl Modica,2 R Curtis Bay,3 Joy H Lewis1
1Department of Public Health, A.T. Still University of Health Sciences, School of Osteopathic Medicine in Arizona, Mesa, AZ, USA; 2Quality Center, National Association of Community Health Centers, Bethesda, MD, USA; 3Department of Interdisciplinary Health Sciences, A.T. Still University of Health Sciences, Arizona School of Health Sciences, Mesa, AZ, USA
Correspondence: Joy H Lewis, 5850 E. Still Circle, Mesa, AZ, 85206, USA, Tel + 1 480 219 6000, Fax + 1 480 389 3661, Email [email protected]
Introduction: Patient satisfaction and experience are important measures of overall quality of care. In 2017, the National Association of Community Health Centers (NACHC) launched an initiative to facilitate changes across organizational systems within Federally Qualified Health Centers (FQHCs) with the goal of improving value-driven care.
Methods: NACHC worked with eight health centers, four in Georgia and four in Iowa, along with their state Primary Care Associations, to apply the Value Transformation Framework (VTF). This framework distills evidence-based practices into practical knowledge for goal-driven systems change. It provides actionable steps to help health centers reach value-driven goals of improved health outcomes, improved patient and staff experience, reduced costs, and improved equity (referred to as the Quintuple Aim goals). This paper reports on the patient and staff experience when applying VTF systems changes to improve colorectal cancer screening rates.
Results: Patient and staff satisfaction and experience remained highly rated even after extensive organizational changes were implemented as part of this project. Implementation of a systems-approach to organizational change, through application of the VTF, did not negatively impact patient or staff experiences.
Conclusion: Patient and staff satisfaction and experience were positive despite the application of the VTF and systems-wide organizational changes. These experience results were alongside improved cancer screening rates, as observed from full project results. Investigators are encouraged that the application of systems change using the VTF may result in the achievement of Quintuple Aim goals without disrupting the experience of patients and staff. Investigators recommend continued exploration of this transformation approach.
Keywords: Quadruple Aim, Quintuple Aim, healthcare experience, cancer screening, primary care, prevention, community health
Introduction
Enhancing patients’ healthcare experience requires that health centers attend to many areas within the overall care delivery system. The Quintuple Aim goals reinforce the importance of this multifaceted approach, with a focus on improved health outcomes, improved patient experience, improved staff experience, reduced costs, and improved equity. Originally established by the Institute for Healthcare Improvement as the Triple Aim,1 this concept was expanded to the Quadruple Aim with the addition of staff experience in 2014.2 Since the start of this project in 2017, the National Association of Community Health Centers (NACHC) adopted the Value Transformation Framework’s expanded focus on the Quintuple Aim with the addition of “equity” as a core goal and measure.
NACHC3 is the national membership organization for health centers that meet the Health Resources and Services Administration’s (HRSA) Health Center Program Requirements. NACHC works closely with health centers and their state and regional partners – primary care associations (PCAs) and health center controlled networks (HCCNs) – to deliver high-quality primary care services to communities in need. PCAs are state or regional membership organizations that offer training and technical assistance to safety-net providers. HCCNs are groups of health centers working together to support and enhance the use of health information technology to improve access and quality and lower costs.4–7
The Value Transformation Framework (VTF) was developed in response to an articulated need from health centers to gather, synthesize, and translate the expansive body of evidence around systems change into actionable steps health centers could readily implement.8 This need is even more critical as health centers transition from a volume-based to value-based model of care.
Health centers provide care to nearly 30 million patients at almost 14,000 delivery sites across nearly 1400 organizations. The majority of health center patients have incomes below the Federal Poverty Level and face social and environmental risk factors that affect their health.9 Despite the complexity of serving high-risk patients with disproportionate burdens of disease, health centers consistently provide quality care that meets or exceeds the performance of private practice primary care offices,10 at lower cost.11 It is estimated that health centers save the healthcare system $24 billion annually.11
Yet, health centers and their respective clinicians and staff—burdened with competing initiatives, rapidly changing technologies, and the demand for practice transformation—are experiencing increased burnout and decreased satisfaction.12–14 They need support in finding successful strategies to deliver better care at lower costs.15
In this project, NACHC aimed to transform health center systems and improve value, through application of the VTF conceptual model for systems change. In 2017, serving as the project lead, NACHC selected participant PCAs through a competitive application process. The PCAs then selected participant health center sites (hereafter “health center”). NACHC required that the PCA also serves as an HCCN or demonstrates a commitment to partner with a HCCN. The final selected organizations included four health centers each in Georgia and Iowa (Table 1).5
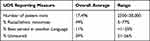 |
Table 1 Averaged Uniform Data Systems 2016 Population Measures for Participating Health Centers |
The Value Transformation Framework (VTF) is a conceptual model that organizes evidence-based strategies that can enhance the capabilities of a health center’s Infrastructure, Care Delivery, and People systems (known in the framework as “Domains”).8 The framework divides the Domains into 15 “Change Areas” (Figure 1). Change Areas focus on concrete interventions and recommended action steps, offered through step-by-step Action Guides and other tools that translate knowledge and evidence into practice. The VTF is designed to support health centers in the transition from a volume- to value-based model of care and achievement of improved health outcomes, improved patient and staff experiences, and lower costs. Equity, central to the Value Transformation Framework from its inception, was separately named as a goal beginning in 2019 – thus becoming the Quintuple Aim goals. While other improvement models exist, the VTF is unique as a clear, standardized model that federally qualified health centers can use as an actionable pathway to overall systems change that advances value.
 |
Figure 1 Graphic of the Value Transformation Framework (VTF). The VTF helps guide systems change in health centers by translating research and promising practices into manageable steps health centers can take to improve care and outcomes. At the core of the model is the health center and the patients it serves. Health centers’ complex systems are broken down into three manageable Domains: Infrastructure, Care Delivery, and People. Each Domain is divided into more detailed Change Areas, 15 in total (represented by the icons that encircle the 3 Domains). The Infrastructure Change Areas include: improvement strategy, health information technology, policy, payment and cost. The Care Delivery Change Areas include: population health management, patient-centered medical home, evidence-based care, care coordination and care management and social determinants of health. The People Change Areas include: patients, care teams, leadership, workforce and partnerships. The outer circle focuses on the goal of the VTF: to support health centers in making system changes by directing action in the 15 change areas and advancing toward value, defined as the Quintuple AIM (represented on the outer circle by: improved health outcomes, improved patient experience, improved staff experience, reduced cost and equity). The VTF was developed by the author, Modica.8 |
Through the lens of the VTF, this project focused on improving the Quintuple Aim goals, with a particular focus on colorectal cancer screening. It was hypothesized that by taking a systems approach to change through application of the VTF, health centers could not only increase the percentage of patients screened for colorectal cancer under the recommended guidelines but also improve performance in other clinical conditions and areas of systems change. Throughout this project, the participating health centers were guided through the areas of change with a focus on 10 evidence-based interventions.
NACHC combined the Value Transformation Framework, evidence-based colorectal cancer screening (CRCS) interventions, and a learning community model to drive health center system improvement. The Learning Community consisted of in-person training, networking opportunities, and regular calls by NACHC staff to provide ongoing project coaching, technical assistance, and support. A structured, yet flexible approach was necessary to provide actionable steps with the ability to perform them within the context of the center’s priorities.16
Members of this investigative team published the overall results of this project in a May 2019 report.16 The raw percentage of eligible patients screened for colorectal cancer increased from 33.2% in January 2017 to 46.5% in December 2017. This translates into an average increase of 3.3 (95% CI: 1.7, 5.0) eligible patients screened per month per health center over the year or 317 additional patients.
Methods
To determine if implementing changes associated with this systems transformation approach affects the experience of health center patients and staff, surveys were administered before, during, and after application of the VTF systems approach.
Investigators used two surveys to collect quantitative data for the evaluation of satisfaction and experience in relation to the implementation of the VTF’s systems approach to change. Drawing from approaches of other published healthcare satisfaction and experience surveys but recognizing the desire to measure elements specific to this project, the investigators developed tools to measure elements unique to the project. The surveys were reviewed by content experts and tested for face-validity. Consensus was reached by group discussion, and the final surveys were approved by the full project team.
Three data collection periods were defined for each survey, the first in March 2017 (baseline measure), the second in December 2017 (end of year one), and the last in December 2018 (end of year two). Each collection period lasted about two months.
Our analyses aimed to answer the following questions:
- Was implementation of the VTF’s systems approach to change associated with any changes in patient satisfaction with the health center or provider?
- Was implementation of the VTF’s systems approach to change associated with perceived changes to the patient visit experience or utilization of health center services and tools?
- Was implementation of the VTF’s systems approach to change associated with any changes in care team satisfaction or experience? Was implementation of the VTF’s systems approach to change associated with provider perceptions of changes in administrative performance?
This quality improvement project was submitted to the A.T. Still University (ATSU, Arizona) Institutional Review Board and deemed to not fall under the jurisdiction of the Board. All surveys were anonymous and did not collect any personally identifying information. Completion of the surveys was voluntary, and there were no consequences for those who chose not to complete the surveys.
Study Sample
Patients and staff of the participating health centers in Georgia and Iowa were the intended recipients of the experience surveys. Eight health centers participated in the first year of the project, and two survey collection periods (baseline and close of year one). Six of the centers continued in year two and participated in the third survey period (end of year two). For this paper, results will be presented reflecting the six health centers that participated in both years one and two of the project and all three survey periods.
Health center population size was determined using the publicly available health center data accessed via the Uniform Data System (UDS).5 Select data on patient demographics provided from each health center’s organizational profile can be found in (Table 2).
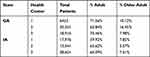 |
Table 2 Total Patients, Including the Percentage of Adults (18–64) and Older Adults (65 and Older), by Health Center |
Patient Survey
The patient survey included a total of 11 items designed to measure patient experience within three domains: satisfaction with health center, staff and visit experience, and utilization of health center services and tools. Patients were asked to base their responses on their experience at the health center over the prior 12-month period. A 5-point Likert scale was used, and responses were coded as Always (5), Often (4), Sometimes (3), Rarely (2), Never (1).
The patient survey was paper-based and available in both English and Spanish. Each participating health center was tasked with distributing the survey to adult patients visiting the health center during the three collection periods.
Staff Survey
The staff survey comprised 25 items developed to assess the following domains: individual level satisfaction and experience, organizational level satisfaction and experience, employment history, and demographics including age, gender, race, and ethnicity. A 5-point Likert scale included the responses: Strongly agree (5), Somewhat agree (4), Neither agree nor disagree (3), Somewhat disagree (2), Strongly disagree (1).
The survey was designed to be completed by health center staff online via the Qualtrics Research Platform. A unique electronic link was provided by investigators to project leaders at each health center and subsequently emailed to staff.
To preserve confidentiality, staff were provided with instructions for creating a personal identification number (PIN) to be entered at the start of each survey. This PIN was only used to link pre- and post-surveys and could not be used to identify any employee.
Analysis
Descriptive statistics (counts and percentages) were calculated to summarize survey responses for each item at each administration. Data were substantially skewed, so means (standard deviations) did not accurately convey the central tendency of the distribution or item variability. Medians (interquartile ranges) did not well convey the magnitude of respondent agreement with survey items or changes in scores across administrations. We chose to provide the percentage of respondents who “agreed” with each statement (endorsed “Always” or “Often” for patients or “Strongly agree” or “Somewhat agree” for staff). Kruskal–Wallis tests were used to evaluate changes in responses over time, based on the ordinal (Likert-type) response scale. Data were analyzed using the Statistical Package for Social Sciences (SPSS 27; IBM Corp., Armonk, NY). A p-value <0.05 (two-tailed) was considered statistically significant.
Results
The total number of patient and staff surveys collected by each health center is presented in (Table 3).
 |
Table 3 Response Counts by Health Center for Patient and Staff Experience Surveys During Each Collection Period |
Patient Survey Results
During the three collection periods, a total of 721, 632, and 389 patient surveys were collected, for a project total of 1742. Patient participants were not asked if they had previously completed the survey and no demographic information was collected.
The questions assessing patients’ satisfaction and their experience with the health center were rated highly and did not change significantly over time. For the survey item, I am satisfied with my experience at the health center, 91% of respondents endorsed “Always” or “Often” at each administration.
Patient agreement about whether staff had asked about cancer screening increased significantly during the three survey periods from 30.5% during survey period 1 to 33.3% at survey period 2 and to 48.7% at period survey 3 (Jonckheere–Terpstra test of trend, p < 0.001).
An additional category of the patient survey inquired if patients used or would use the optional health center services of an online patient portal and receipt of text message reminders. The percentage of patients using the health center’s online patient portal decreased from 21.9% at baseline to 15.1% at the third administration (p < 0.001). The percentage of patients who reported that they would like to receive text message reminders regarding health screenings remained stable at approximately 57%.
The full patient survey and the percentage agreement for each item are provided in Appendix A.
Staff Survey Results
A total of 374 staff surveys were collected with 128, 139, and 107 surveys received during the collection periods. Individual staff member responses could not be linked over time, due to inconsistencies in the use of the self-created PIN. However, staff members were asked to select the category, which best represented their job title from a provided list.
Clinical Providers and Clinical Staff consistently accounted for the greatest number of responses. Staff members in the Health Information Technology category accounted for the fewest number of responses. The job category proportions for each collection period are outlined in Table 4.
 |
Table 4 Percentage of Staff Survey Responses by Job Title per Survey Collection Period |
Health center staff rated items associated with individual level satisfaction and experience highly. None of the item scores changed significantly throughout the project. The highest scoring item was My work adds value to my health center’s ability to provide care with most staff indicating they “strongly agree”. The lowest scoring item was There are opportunities for career advancement within my health center, although more than half reported agreement.
The questions included in organizational level satisfaction and experience also scored highly, although measuring slightly lower than the individual level items. Most staff reported agreement with the following items: If I have ideas about how to improve systems or processes, I feel others will listen to me; I have been provided sufficient training to help me fulfill my specific role(s) as a member of my larger health center team; and At my health center, we all work together and support one another in getting work done.
For the items Overall, I am satisfied with my job and, I look forward to coming to work each day, staff remained in agreement over all measurement periods. The full staff survey and the percentage agreement score for each item are provided in Appendix B.
Discussion
Despite the addition of processes and changes in health center operations, both patient and staff satisfaction and experience remained highly rated throughout the project.
Significantly, these changes were also associated with improvements in performance of colorectal cancer screening.16
These findings support various recommendations for the use of multicomponent interventions in the pursuit of improved clinical care and patient outcomes.17–20 Satisfaction can remain high within the health center despite potential disruptions brought about through transformation efforts.
Patient Survey Discussion
Overall, patient satisfaction and experience remained highly rated at each health center throughout the project period. Together, the survey results indicate patient satisfaction and a positive patient experience and suggest that the additions to changes in organizational systems did not disrupt patient satisfaction or experience.
Responses to the survey items regarding patient portal use and text messaging preferences indicate use of these technologies is low. Reasons for not using the patient portal and opting out of text message reminders were not explored and could be incorporated into future surveys. Elucidating these patient preferences may identify better ways to keep patients up to date with recommended screenings and to connect patients with recommended services.
The inclusion criterion was an age over 18 years. A more targeted sample of established patients who meet the criteria for cancer screening may have produced different results. Additionally, as we could not control the local survey distribution process, the methods used for patient recruitment may have differed between health centers and could have impacted the number of surveys received.
The requirements a health center must meet to be certified as an FQHC21 and the demographics of patients typically served by health centers suggest that there could be a need for assistance with social factors that can affect health.22,23 Future patient surveys can assess the levels of need and perceived interest in receiving help in these areas, along with evaluations of the level of help provided.
Staff Survey Discussion
Throughout this project, health center staff also rated their job satisfaction and experience highly. Responses grouped by job category indicated improvements in ratings in all groups, except for those who work in Health Information Technology. This may be due to the low number of responses in this category but should be further explored.
Of note, the results showed upward trends for the item At my health center, screening and management of chronic disease (depression, obesity, high blood pressure, diabetes) are the responsibility of the entire care team and not just the medical provider. The improvements observed for this item can be used to demonstrate the success of the VTF in guiding successful systems change.
As shown in other published literature,24–26 results from patient surveys can also be used as an indicator of a positive staff experience and positive staff performance. The patient survey results from this project indicate that staff are performing well on the measured areas, including recommending cancer screenings and making the patient feel included when making care decisions. These patient survey results can be shared with staff to demonstrate high levels of patient satisfaction and experience even while managing a system transformation.
The limitations of this survey’s administration prevented the tracking of staff participants and the linking of their responses over time. Future projects should explore new ways to engage staff in survey participation and improved methods to ensure accurate participant tracking. Additionally, although staff satisfaction surveys are routinely administered by health centers and tracked over time, psychometric validation of these surveys has not been completed and thus there may be limitations in the survey sensitivity to change in attitudes and beliefs, particularly to subtle changes.
Conclusion
Changes in protocol and increases in job responsibilities that may take place as a part of transformation efforts are often associated with a decrease in job satisfaction, particularly during the period of change.27 The results of these surveys indicate that experience and satisfaction scores remained high for both patients and staff throughout the implementation of systems change through application of the Value Transformation Framework. Along with the improvement observed in the associated clinical measures, these survey results serve as further evidence that this framework may be effective in the pursuit of improving the elements of healthcare service associated with the Quintuple Aim.
A potential limitation is that both surveys were subject to the “ceiling effect”, allowing little room for improvement. Mean scores were high (more positive) from the start and therefore most increases in score were statistically insignificant. However, we view the overall results positively; as an indication that patients and staff highly rated their satisfaction and experience, despite system changes and the addition of processes and procedures.
Limitations in survey design prevent a full review of the association between application of the Value Transformation Framework and specific areas of patient and staff satisfaction and experience. Investigators must weigh the advantages and disadvantages of survey use while keeping in mind the intended outcome. Further, the surveys did not collect demographic information or information about specific social determinants of health. Future work should include more details in these areas to inform specific health center responses. Despite the production of imperfect data, the survey results of this project are still usable by the health center participants and others interested in pursuing application of this framework. More thorough evaluations might best be achieved through the regular distribution of verified experience surveys28–30 in addition to continual reporting of performance in clinical measures within recommended guidelines.
This project aimed to compile a holistic view of the potential effects of the interventions implemented on the satisfaction and experience of health center patients and staff. As one of the authors is designer and original author of the Value Transformation Framework,8 the importance of impartiality in viewing results is recognized and the need for continued study of patient and staff experience with implementation of the VTF. The survey results reported in this paper serve as snapshots in time that are encouraging, with no unintended consequences related to satisfaction or experience identified when a systems approach to change was undertaken through application of the Value Transformation Framework.
These results can be used to show that the implementation of the Value Transformation Framework in this project improved clinical outcomes without negatively impacting patient and staff satisfaction and experience. Therefore, the Value Transformation Framework may be a useful tool for other healthcare organizations initiating systems change and may be adaptable to a wide variety of areas for healthcare improvement.
Abbreviations
ATSU, A.T. Still University; CRCS, Colorectal Cancer Screening; FQHC, Federally Qualified Health Center; HCCN, Health Center Controlled Network; HRSA, Health Resources and Services Administration; NACHC, National Association of Community Health Centers; PCA, Primary Care Association; PIN, Personal Identification Number; QI, Quality Improvement; UDS, Unified Data Systems; VTF, Value Transformation Framework.
Ethics and Consent Statements
The Federal regulations 45 CFR 46.117c(1) Documentation of Informed Consent were met, which allow waiver of a signed consent if either:
- Only record linking the subject and the research would be the consent document and the principal risk would be potential harm resulting from a breach of confidentiality; or
- That the research presents no more than minimal risk of harm to subjects and involves no procedures for which written consent is normally required outside the research context.
The participants were not required to and did not provide informed consent because doing so would potentially have linked their identities to their responses. The intentionally anonymous surveys did not require names or signatures from any participants. The patient surveys were routinely collected as part of standard health center practice. There was no additional language added as the collection of these surveys is part of routine patient care. Review of the anonymous survey responses is part of the continued quality improvement process.
The staff surveys included the following language (adjusted for pre and post surveys):
The following survey is a project conducted by the National Association of Community Health Centers (NACHC) and A.T. Still University in Arizona (ATSU) as part of a Centers for Disease Control and Prevention (CDC) supported transformation project. The purpose of this survey is to gather input from health center employees regarding your work experience and satisfaction. Your participation in this survey is voluntary. Completing this survey should require approximately 5 minutes. We ask that you complete each question honestly and to the best of your ability. Your responses will be anonymous.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work. The authors thank the following health centers and primary care associations for their dedicated work in this project: Coastal Community Health Services, Brunswick, Georgia; Community Health Care Systems, Tennille, Georgia; East Georgia Healthcare Center, Swainsboro, Georgia; Community Health Centers of Southeastern Iowa, Burlington, Iowa; Eastern Iowa Health Center, Cedar Rapids, Iowa; Primary Health Care, Des Moines, Iowa; Georgia Primary Care Association, Decatur, Georgia; and Iowa Primary Care Association, Des Moines, Iowa.
Disclosure
R Curtis Bay reports grants from NACHC, during the conduct of the study. The authors reports no other conflicts of interest in this work.
References
1. Berwick DM, Nolan TW, Whittington J. The triple AIM: care, health, and cost. Health Aff. 2008;27(3):759–769. PMID: 18474969. doi:10.1377/hlthaff.27.3.759
2. Bodenheimer T, Sinsky C. From Triple to Quadruple AIM: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi:10.1370/afm.1713
3. About NACHC. National association of community health centers website. Available from; https://www.nachc.org/about/about-nachc/.
4. Health Resources and Services Administration website. About the health center program, what is a health center? Available from: https://bphc.hrsa.gov/about/what-is-a-health-center/index.html.
5. Health Center Program Data. Human resources and service administration website. Available from: https://bphc.hrsa.gov/uds/datacenter.aspx.
6. Primary Care Associations. Health resources and services administration website. Available from: https://bphc.hrsa.gov/qualityimprovement/strategicpartnerships/ncapca/associations.html.
7. Health Center Controlled Networks. Health resources and services administration website. Available from: https://bphc.hrsa.gov/program-opportunities/hccn.
8. Modica C. The value transformation framework: an approach to value-based care in federally qualified health center. J Healthc Qual. 2020;42(2):106–112. doi:10.1097/JHQ.0000000000000239
9. Health Center Program: Impact and Growth. Health resources and services administration website. Available from: https://bphc.hrsa.gov/about/healthcenterprogram/index.html.
10. Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43(2):142–149. doi:10.1016/j.amepre.2012.02.033
11. Ku L, Richard P, Dor A, Tan E, Shin P. Using primary care to Bend the curve: estimating the impact of a health center expansion on health care costs. Geiger Gibson/RCHN Community Health Foundation at the George Washington University. Policy Research Brief No. 14; 2009.
12. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi:10.1016/j.mayocp.2015.08.023
13. Friedberg MW, Reid RO, Timbie JW, et al. Federally qualified health center clinicians and staff increasingly dissatisfied with workplace conditions. Health Aff. 2017;36(8):1469–1475. doi:10.1377/hlthaff.2017.0205
14. Middaugh DJ. Can there really be joy at work? Medsurg Nurs. 2014;23(2):131–132.
15. Quinn MT, Gunter KE, Nocon RS, et al. Undergoing transformation to the patient centered medical home in safety net health centers: perspectives from the front lines. Ethn Dis. 2013;23(3):356–362.
16. Modica C, Lewis JH, Bay C. Colorectal cancer: applying the value transformation framework to increase the percent of patients receiving screening in federally qualified health centers. Prev Med Reps. 2019;15. doi:10.1016/j.pmedr.2019.100894
17. Nelson EC, Mohr JJ, Batalden PB, Plume SK. Improving health care, Part 1: the clinical value compass. Jt Comm J Qual Improv. 1996;22(4):243–258. PMID: 8743061. doi:10.1016/s1070-3241(16)30228-0
18. Crain AL, Solberg LI, Unützer J, et al. Designing and implementing research on a statewide quality improvement initiative: the DIAMOND study and initiative. Med Care. 2013;51(9):e58–e66. doi:10.1097/MLR.0b013e318249d8a4
19. Keuter K, Byrne E, Voell J, Larson E. Nurses’ job satisfaction and organizational climate in a dynamic work environment. Appl Nurs Res. 2000;13(1):46–49. doi:10.1016/S0897-1897(00)80018-X
20. Thornton RD, Nurse N, Snavely L, Hackett-Zahler S, Frank K. DiTomasso RA/ Influences on patient satisfaction in healthcare centers: a semi-quantitative study over 5 years. BMC Health Serv Res. 2017;17:361. doi:10.1186/s12913-017-2307-z
21. Federally Qualified Health Center. Medicare learning network, center for Medicaid and medicare services; 2021.
22. Shin S, Alvarez C, Sharac J, et al. A profile of community health center patients: implications for policy. Issue Brief of the Kaiser Commission on Medicaid and the Uninsured; 2013. Available from: https://www.kff.org/wp-content/uploads/2013/12/8536-profile-of-chc-patients.pdf.
23. Katz A, Chateau D, Enns JE, et al. Association of the social determinants of health with quality of primary care. Ann Fam Med. 2018;16(3):217–224. doi:10.1370/afm.2236
24. Molyneux J. Nurses’ job satisfaction linked to patient satisfaction. Am J Nurs. 2011;111:16. doi:10.1097/01.NAJ.0000398037.25162.fb
25. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–128. doi:10.1046/j.1525-1497.2000.02219.x
26. Palese A, Gonella S, Fontanive A, et al. The degree of satisfaction of in-hospital medical patients with nursing care and predictors of dissatisfaction: findings from a secondary analysis. Scand J Caring Sci. 2017;31:768–778. doi:10.1111/scs.12396
27. Kuokkanen L, Suominen T, Harkonen E, Kukkurainen ML, Doran D. Effects of organizational change on work-related empowerment, employee satisfaction, and motivation. Nurse Admin Q. 2009;33(2):116–124. doi:10.1097/NAQ.0b013e3181a10c86
28. Tantau C. Provider and staff satisfaction survey. tantau & associates. Chicago Park, California. made available for download through the institute for healthcare improvement. Available from: http://www.ihi.org/resources/Pages/Tools/ProviderandStaffSatisfactionSurvey.aspx.
29. Chang E, Cohen J, Koethe B, Smith K, Bir A. Measuring job satisfaction among healthcare staff in the United States: a confirmatory factor analysis of the Satisfaction of Employees in Health Care (SEHC) survey. Int J Health Care Qual Assur. 2017;29(2):262–268. doi:10.1093/intqhc/mzx012
30. Suhonen R, Leino-Kilpi H, Välimäki M, Kim HS. The patient satisfaction scale—An empirical investigation into the Finnish adaptation. J Eval Clin Pract. 2007;13:31–38. doi:10.1111/j.1365-2753.2006.00643.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
